Abstract
Background and objective
In Sweden, mortality from cardiovascular diseases (CVD) increased steadily during the 20th century and in the mid-1980s it was highest in the county of Västerbotten. Therefore, a community intervention programme was launched – the Västerbotten Intervention Programme (VIP) – with the aim of reducing morbidity and mortality from CVD and diabetes.
Design
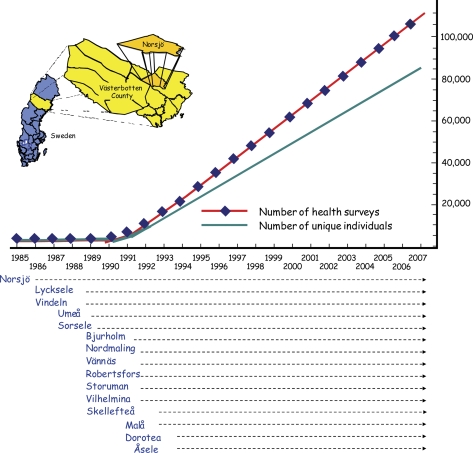
The VIP was first developed in the small municipality of Norsjö in 1985. Subsequently, it was successively implemented across the county and is now integrated into ordinary primary care routines. A population-based strategy directed towards the public is combined with a strategy to reach all middle-aged persons individually at ages 40, 50 and 60 years, by inviting them to participate in systematic risk factor screening and individual counselling about healthy lifestyle habits. Blood samples for research purposes are stored at the Umeå University Medical Biobank.
Results
Overall, 113,203 health examinations have been conducted in the VIP and 6,500–7,000 examinations take place each year. Almost 27,000 subjects have participated twice. Participation rates have ranged between 48 and 67%. A dropout rate analysis in 1998 indicated only a small social selection bias. Cross-sectional, nested case-control studies and prospective studies have been based on the VIP data. Linkages between the VIP and local, regional and national databases provide opportunities for interdisciplinary research, as well as national and international collaborations on a wide range of disease outcomes. A large number of publications are based on data that are collected in the VIP, many of which also use results from analysed stored blood samples. More than 20 PhD theses have been based primarily on the VIP data.
Conclusions
The concept of the VIP, established as a collaboration between politicians and health care providers on the one hand and primary care, functioning as the operating machinery, and the public on the other, forms the basis for effective implementation and endurance over time. After more than 20 years of the VIP, there is a large comprehensive population-based database, a stable organisation to conduct health surveys and collect data, and a solid structure to enable widespread multidisciplinary and scientific collaborations.
Keywords: prevention, community intervention, cardiovascular diseases, primary health care, health promotion, research methodology
In Sweden, mortality from cardiovascular diseases (CVD) gradually increased from the beginning of the 20th century until the 1960s, when this trend reached a plateau and then reversed in the mid-1980s. In the northern counties this transition was even more marked than in the country as a whole. Having constituted a negligible part of total mortality at the beginning of the 20th century, cardiovascular mortality increased more rapidly in the north starting in the early 1940s (1), becoming the leading cause of death in the 1970s and early 1980s. The county of Västerbotten showed the highest mortality from myocardial infarction with 720/100,000 inhabitants/year among 16 to 74-year-olds. By comparison, the county of Halland, located in southern Sweden, had the lowest myocardial infarction mortality with almost 200 fewer deaths per year (2). In the Västerbotten municipality of Norsjö, CVD mortality among men was even higher, and was three-fold that of women in the area. Among the general population there was a growing awareness of the threat of CVD.
During the 1970s, this pattern of mortality was observed and described in social medicine and epidemiological analyses (3–6). Scientific investigations and discussions among health policy makers and administrators led to a collaborative project between the Västerbotten County Council, SPRI (The Swedish Planning and Rationalization Institute for Health Services) and the Department of Social Medicine, Umeå University. The collaboration resulted in a report titled ‘Health problems in a county – a basis for health planning’ (7), based on the Swedish Causes of Death Register, the Register of Diagnoses in In-patient Care and Survey of Living Conditions (8). The new Health Care Act (9), provided an additional incentive for prevention initiatives. This legislation was adopted by the Swedish Parliament in 1982 and specified that, in addition to providing care, the County Council was also responsible for programmes to improve health. Subsequently, in 1984, the Västerbotten County Council decided to launch a community intervention programme – the Västerbotten Intervention Programme (VIP) – with the aim of reducing morbidity and mortality from CVD and diabetes (10). Initially, the intervention would be developed in a small municipality, Norsjö, where the programme would be evaluated and revised before successive implementation in the rest of the county.
Västerbotten County covers one eighth of Sweden, from the Gulf of Bothnia to the Scandinavian mountain chain, and has an area of 55,000 km2. The population is concentrated in the coast land and increased slightly from 245,000 in 1985 to 258,000 in 2007.
Setting: primary care in Sweden
Primary care has a long tradition in Sweden, dating back to the 17th century. District medical officers, who were often responsible for huge land areas, carried out inspections and reported to the authorities about health and diseases, lifestyle habits and sanitary and socioeconomic conditions in the population. The number of district medical officers increased gradually and at the turn of the 19th century there was at least one physician in each urban or rural district. In 1973, these district officers were replaced by family doctors working primarily in health care centres. Primary care centres often consist of 2–10 doctors collaborating and working together with district nurses, midwives, assistant nurses, physiotherapists, occupational therapists and administrative personnel. Primary care is financed by taxes and to a small extent by out-of-pocket payments, and is organised either by each county or by private care providers.
Primary prevention also has a long tradition in Sweden, with well-organised antenatal and child welfare clinics attended by almost all children and pregnant women in the country. The main area of responsibility for Swedish district nurses is prevention and public health with an emphasis on children and the elderly. Therefore, they have comprehensive knowledge about the population within the district they serve. Approximately 50% of the population attend their primary care centre each year and within a few years the majority are well-known by their family doctor and district nurse (11). However, no systematic prevention programmes have addressed the middle-aged population.
History of the VIP
Point of departure
The VIP, initially called the Norsjö Project, began in 1985. Descriptive analyses that showed high CVD mortality in Västerbotten as a whole, and in Norsjö in particular, were presented to leading physicians, politicians and administrators, social and health workers and the public. The discussions that followed created positive conditions for local initiatives and action by multiple sectors. A series of local meetings were held in Norsjö and the surrounding villages, and the public was invited to participate with regard to the contents of the VIP.
Alternative explanations for the high CVD mortality were put forward by the public, e.g. pollutants from the mining industry (12), however, a general understanding of the associations between risk factors and CVD gradually increased (13).
From the beginning, the Västerbotten model for prevention combined a population-based strategy directed towards the public with a strategy to reach all middle-aged persons individually by inviting them to participate in screening and health counselling conducted by their primary health care providers.
The population-oriented activities were co-ordinated within a framework of the intervention programme and consisted of many components. The intervention was tailored to local circumstances through involvement of the whole local community, from schools to homes for the elderly, public and private organisations, lay opinion leaders, politicians, voluntary organisations, industrial entrepreneurs and tradesmen. The process was integrated into everyday activities and aimed at health promotion (14). For example, schools and pre-schools developed more varied and healthier menus for school lunches, local associations organised health information meetings for their members and were supported in producing informational materials about various health issues. Educational materials were also produced for local study groups (studiecirkel), which focus on social life and local culture, health problems and health care, and food traditions and basic nutrition.
In agreement with the County Council, primary health centre staff assumed responsibility for inviting all inhabitants to participate in a comprehensive health survey every 10 years, at ages 30, 40, 50 and 60 years. The fundamental idea was that opportunities for intervention would be established at the local primary care centre, where systematic risk factor screening and individual counselling about healthy lifestyle habits could influence the risk of CVD at both population and individual levels.
The VIP administrators had an open attitude towards the media, which resulted in a number of articles in the local and national press (13). The main participants in these articles were the authorities, including medical staff, and the focus was mainly on middle-aged men and individual lifestyle habits. Little space was given in the media to women, children and people of 60+. Collaborations with the local food production industry and merchants, as well as the National Food Administration in Sweden (Livsmedelsverket), resulted in a food labelling system for low-fat and high-fibre products. This system, known as ‘the green keyhole’, was introduced in Norsjö in 1987 and then further developed and introduced across the rest of Sweden (Fig. 1).
Fig. 1.
The green keyhole developed from a lattice-work heart pattern. The green keyhole designates a healthy food item.
Implementation throughout the rest of the county
Based on the experiences in Norsjö and how the model worked in practice, the VIP was gradually implemented throughout the county, starting in 1987. Since 1991, the programme has covered the entire middle-aged population (15) (Fig. 2). As part of a dissemination programme, various launch events were directed at the general population and introduced in each municipality. Among other things, this included public information meetings, activities in non-governmental organisations, and invitations to study groups and physical activities. Activities in the local community were most intense during the early years of the VIP, particularly in the pilot area of Norsjö. Initially, the VIP was characterised as a project, and health surveys could be discontinued for periods of time due to decisions at each health centre. This contributed to decreased participation rates, i.e. 48–57% during 1991–1995. In order to give priority to prevention efforts, the County Council decided to integrate the VIP into ordinary primary care routines in 1995. At the same time, it was also decided to omit individuals aged 30 due to low attendance rates and budgetary restrictions. Thereafter, participation rates increased and have remained at 66–67% since 2005. Between inception through 2007, a total of 86,242 individuals have participated with almost 27,000 participating twice. Overall, 113,203 health examinations have been conducted as part of the VIP and an additional 6,500–7,000 take place each year (Fig. 3). Distribution between sexes and educational groups is provided in (Table 1). Analysis of the dropout rate in 1998 showed marginal differences in social characteristics between participants and non-participants and indicate only a small social selection bias (16). Dropout analyses published in 2007 regarding longitudinal VIP studies showed that participants of younger age, with more cardiovascular risk markers, who were men or with higher education were less likely to return for a second health examination (39, 80). Overall, the effect of this should be complex because these characteristics are, to some extent, contradictive, as younger age and higher education is known to be associated with lower cardiovascular risk.
Fig. 2.
Cumulative number of individuals who participated in the Västerbotten Intervention Programme and the number of health surveys performed during the programme from 1985 to 2007. The start in Norsjö 1985 and subsequent implementation in all municipalities in the county until 1991 is demonstrated.
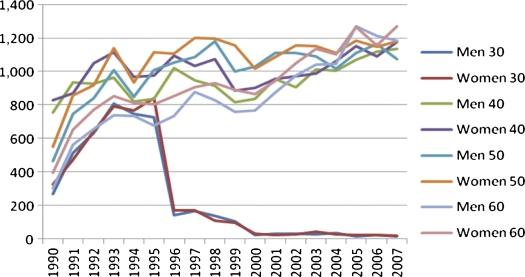
Fig. 3.
Number of Västerbotten Intervention Programme health examinations of men and women aged 30, 40, 50 and 60 years between 1990 and 2007. Total number: 54,568 men and 58,635 women.
Table 1.
Number of Västerbotten Intervention Programme health examinations of participants during three time periods from 1990 to 2007, with distribution by sex and educational group
| 1990–1995 | 1996–2001 | 2002–2007 | |
|---|---|---|---|
| Sex | |||
| Men | 17,390 (47.3) | 17,371 (48.2) | 19,644 (49) |
| Women | 19,378 (52.7) | 18,679 (51.8) | 20,458 (51) |
| Education | |||
| Basic | 10,556 (29.3) | 9,200 (25.7) | 6,887 (17.3) |
| Mid-level | 17,530 (48.7) | 17,818 (49.7) | 21,068 (52.9) |
| High | 7,927 (22) | 8,813 (24.6) | 11,869 (29.8) |
Design of the VIP
Procedures: the health survey, manual, decision support system, educational activities
The VIP manual
The VIP measurements and procedures follow a detailed manual that describes procedures and indications for extended examination or referrals and/or counselling regarding lifestyle modification.
Invitation to participants
Each year, all subjects who become 40, 50 or 60 years and who belong to the list for a specific primary care centre or live within the area for that centre, are identified by the County Council administrative staff, which has access to the national population register. This register is based on the individual civic numbers that identify all Swedes and include name, address and date of birth. This information is given to each health centre that, in turn, invites the participants to the health examination.
Measurements
Participants visit their health centre following an overnight fast. A list of procedures is given in Table 2. Height and weight in light clothing are measured and body mass index (BMI) in kilogram per square metre is calculated. Blood pressure is measured once with a mercury sphygmomanometer after 5 min rest with the subject in a supine position. An oral glucose tolerance test (OGTT) following WHO standards is done with a 75-g oral glucose load (17). Subjects with previously known diabetes mellitus or with fasting glucose exceeding the criterion for diabetes do not undergo OGTT. A Reflotron bench-top analyser (Roche Diagnostics) is used for the analyses of blood lipids; from 1985 to 2004 it was also used for plasma glucose values. Currently, a Hemocue bench-top analyser (Quest Diagnostics) is used for glucose values. For those identified as at increased risk, additional samples of blood are also sent to the clinical chemistry department at the nearest local hospital for more detailed analysis of blood lipids. Participants are invited to donate blood for research purposes and these samples are stored at –80°C at the Umeå University Medical Biobank (18). Reflotron and Hemocue analysers are regularly tested in a calibration scheme provided by EQUALIS, the External Quality Assurance in Laboratory Medicine in Sweden.
Table 2.
Overview of Västerbotten Intervention Programme procedures. Recommendations are that nurses and doctors (general practitioners, GP) use motivational interviewing (MI) when counselling lifestyle changes aimed at risk factor reduction. Doctors are encouraged to follow current guidelines regarding pharmacological treatments
| Risk indicator | Variable | Decision level | Recommendation |
|---|---|---|---|
| Overweight/obesity | Body mass index waist | ≥ 30 kg/m2a | MI |
| Men >102 cma, women >88 cma | |||
| Hypertension | Systolic, diastolic blood pressure, ongoing antihypertensive medicationa | ≥ 140/90a | Two follow-up visits to nurse then referral to GP if blood pressure remains elevated, MI |
| ≥ 130/80 for participants with diabetes | Referral to GP, MI | ||
| Dyslipidaemia | S-cholesterol | ≥ 7.5 mmol/L | Referral to GP, MI |
| Known CVD or diabetes and ≥ 3.5 mmol/La | Referral to GP, MI | ||
| >6.5 mmol/La | |||
| LDL-cholesterol | ≥ 6 mmol/L | Referral to GP, MI | |
| Triglycerides | ≥ 4 mmol/L | Referral to GP, MI | |
| Glucose regulation | Fasting plasma glucose (capillary) | Impaired fasting glucose (IFG): fasting plasma glucose 6.1–6.9 mmol/La | Follow up visit to nurse every second year, MI |
| 2 h plasma glucose | Impaired glucose tolerance (IGT): fasting plasma glucose <7.0 and 2 h plasma glucose 8.9–12.1 mmol/La | Follow up visit to nurse every second year, MI | |
| Diabetes: fasting plasma glucose ≥ 7.0 or/and 2 h plasma glucose ≥ 12.2 mmol/L | Referral to GP, MI | ||
| Metabolic syndromeb | Referral to GP, MI | ||
| Alcohol | CAGEc (four questions) | >2 yes answers of four | MI |
| AUDITc | Hazardous/harmful alcohol consumption: men 8–15 points, women 6–13 points | MI | |
| Alcohol abuse/dependence: men ≥ 16 points, women ≥ 14 points | |||
| Tobacco | Number of cigarettes smoked or boxes of snus consumed | >0 | MI |
aAdditional samples of blood are sent to the Department of Clinical Chemistry at the nearest local hospital for more detailed analysis of blood lipids including serum cholesterol, LDL-cholesterol, HDL-cholesterol and serum triglycerides.
bMetabolic syndrome defined as: diabetes or IFG or IGT plus two or more of the following: (1) body mass index ≥ 30 kg/m2 or waist circumference >102 cm for men or >88 cm for women; (2) blood pressure ≥ 140/90 or current use of antihypertensive medication; (3) triglycerides >2 mmol/L or HDL-cholesterol ≤1.0 mmol/L or current use of medication for dyslipidaemia.
Questionnaire
The VIP participants are invited to complete a comprehensive questionnaire that covers socioeconomic and psychosocial conditions, self-rated health, personal health history and family history of CVD and diabetes, quality of life (19, 20), social network and support (21, 22), working conditions (23, 24), physical activity, alcohol problems (25, 26), tobacco consumption, eating habits and a food frequency questionnaire (27). Content areas of the VIP questionnaire are summarised in Table 3.
Table 3.
Overview of Västerbotten Intervention Programme questionnaire
| Area | Variables |
|---|---|
| Socioeconomic conditions | Marital/civil status |
| Housing conditions | |
| Educational level | |
| Occupation | |
| Employment | |
| Sick leave/pension | |
| Ethnicity | |
| Health | Self-reported health |
| Family history of myocardial infarction, stroke, diabetes | |
| Personal history of diabetes, myocardial infarction | |
| Current pharmacologic treatment | |
| Health-related quality of life | Göteborg Quality of Life Instrument |
| SF-36 | |
| Social support and network, work stress | ISSI (Interview Schedule for Social Interaction) |
| Karasek demand/control model | |
| Physical activity | Commuting activity |
| Physical activity at work | |
| Leisure activities | |
| Physical exercise | |
| Tobacco | Smoking habits |
| Use of Swedish moist snuff (snus) | |
| Alcohol | CAGE |
| AUDIT | |
| Sleeping habits | Daytime sleepiness, snoring, history of sleep apnoeas |
| Eating habits | Breakfast habits and daily meals, portion size, vegetarianism, dietary supplements |
| Food frequency questionnaire | 66 items, 8 alternatives from never to 4 times or more every day |
Individual counselling
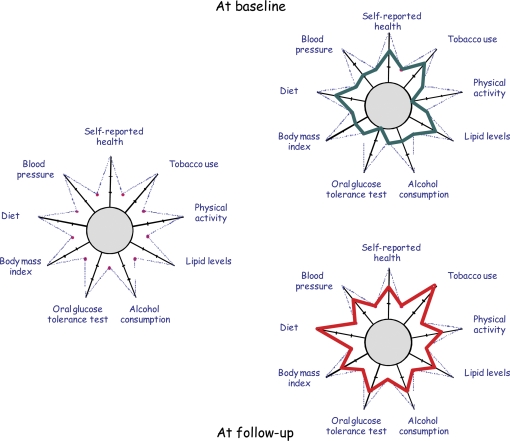
Each health survey concludes with information about the results of the examination and the questionnaire is reiterated to the participant. In the early years, this conversation was mainly unidirectional in nature, with nurses giving advice about adequate lifestyle changes with a focus on single risk indicators. Methodology has subsequently been developed to encourage a dialogue with the participant and provide a comprehensive approach to facilitate health promotion. To this end, in the late 1990s, family doctors and district nurses across the entire county were trained in the method of motivational interviewing (28). Motivational interviewing uses open questions, active listening and summaries, as a means of reinforcing lifestyle changes and aligning them with the individual's own conclusions and preferences regarding conceivable lifestyle changes. During the dialogue, a ‘star-profile’ is drawn that represents risk markers (Fig. 4); the more risk indicators, the smaller the points of the star. While none has a perfect nine-point star, this usefully illustrates the interrelationships between risk markers and behaviour, as well as options for health promotion.
Fig. 4.
The star-profile. Collection of data for blood pressure, body mass index (BMI), plasma glucose, blood lipids, level of physical activity, self-reported health, alcohol consumption (AUDIT) and tobacco habits are marked. Participants estimate their own dietary and eating habits. The example illustrates results at baseline and follow up.
Appropriate follow-up visits are recommended and depending on risk marker levels, participants are referred to their family doctor for further assessment. When needed, pharmacologic treatment is provided according to current guidelines. A significant methodological improvement was the implementation of EviBase in 2004: EviBase is a computerised decision support system. Measured values of height, weight, blood pressure, plasma glucose and lipids, as well as questionnaire data on smoking, history and a family history of CVD and medication are put into the system by the nurse. The output is an interpretation including a recommended action plan that follows the VIP manual and this is used in the discussion with the participant. This system was invented and developed by a general practitioner, Mats Persson (29).
Scientific board, updating procedures and the administrative system
From its inception, the VIP was supported by a scientific advisory group from Umeå University. The board represented internal medicine, social medicine, nutritional research, family medicine, pedagogy and epidemiology. This board determined the contents of the health examination and questionnaire, as well as the manual for management of results, e.g. cut-off values for recommended follow-up visits or referral to a physician. This advisory group was disbanded in 1995 when the VIP was integrated into daily primary care routines, and the County Council's Division for Research and Development (R&D) took responsibility for co-ordination of the VIP activities and annual training arrangements for personnel. In March 2005, a new scientific board was established, which is managed by the head of R&D and includes representatives with scientific and statistical competency, primary care expertise and is assisted by co-ordinating staff. Applications to use data from the VIP database for research purposes are evaluated and decided upon by this board. Decisions regarding material from the stored blood samples with corresponding VIP data are managed by the board of the Medical Biobank.
The VIP manual has been updated regularly according to current national and international guidelines (30). In 2003, metabolic syndrome was adopted as a tool to identify participants with a particularly high CVD risk. In the same year, measurement of waist circumference and the intermediate risk state of impaired fasting glucose (IFG) were also introduced. The questionnaire has gradually expanded, and the food frequency questionnaire has been modified and shortened. An additional questionnaire regarding health-related quality of life, the Short Form Health Survey (SF-36) (31), was included in 2003. In 2005, questions about sleep apnoea and snoring and the AUDIT questionnaire with questions on alcohol consumption (32) were added. Since September 2009, the use of Reflotrons has finished and all analyses of plasma lipids are now done with routine methods in the clinical chemistry department of the local hospital. From the same time point, blood pressure is measured twice with the subject sitting and after 5 min rest. The mean value for the two measurements is registered. Completed questionnaires have been optically read since 1993.
To promote follow-up activities, yearly data sheets are sent to each VIP nurse, which lists participants who fulfilled specific criteria during the previous year and require follow up, according to the VIP manual.
Funding of the VIP
All activities required to co-ordinate the health surveys in daily practice, including blood sampling, are managed by the County Council and funded by regional taxes. Primary care centres are paid 650 SEK (∼80 USD) for each completed VIP health survey. There are no contributions from national taxes or private funding. According to current legislation, the County Council owns and is responsible for holding and managing the primary VIP database.
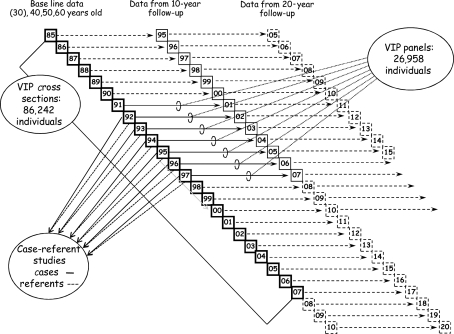
Scientific opportunities and potential
The construction of the VIP enables different types of study design (Fig. 5). Cross-sectional data comprising large amounts of information are used to investigate prevalence and trends in distribution of single markers or clusters of markers among the population or subpopulations over time. For example, biologic and psychosocial risk markers and lifestyle patterns can be studied (33–35). Shifts in risk marker distribution following societal changes or medical interventions may be demonstrated (36). Based on associations between exposure and outcome, new hypothesis can then be formulated and further studies planned.
Fig. 5.
Design of the Västerbotten Intervention Programme (VIP) and illustration of different study designs.
Nested case-control studies have the strength of prospective studies and are based on the well-defined VIP population that represents the more general middle-aged population. Associations may be evaluated at an individual level between baseline variables, including those analysed from stored blood samples, and a wide range of disease outcomes (37, 38). Results may then be used to suggest new hypotheses regarding causal links. Longitudinal observations from panel data are used to investigate incidence as well as associations between baseline variables and disease at follow up (39, 40). Supplementary studies based on quantitative data and adopting qualitative methodologies may deepen existing research questions (41).
Furthermore, linkages between the VIP and other local, regional and national databases provide opportunities for interdisciplinary research, investigation of various disease outcomes and assessment of further demographic and socioeconomic conditions (42) (Fig. 6). There are opportunities to compare Västerbotten and other parts of Sweden, as well as vast potential for consideration from a global perspective. Thus, linking the VIP data with other databases enables international research collaborations on a wide range of disease outcomes (43). It would also be possible to evaluate VIP interventions by comparing local and national data regarding CVD morbidity and mortality.
Fig. 6.
Potential links between the Västerbotten Intervention Programme database and local, regional and national registers.
A large number of publications are based on data collected in the VIP surveys. These may rely solely or to some degree on the VIP data and may or may not use results from analysed stored blood samples. This is exemplified in Table 4, which is a listing of selected theses defended at Umeå University.
Table 4.
Selection of theses defended at Umeå University using results that solely or to some degree are based on data from Västerbotten Intervention Programme, with or without analysis of stored blood samples from the Medical Biobank
| Author | Focus | Subject | Year | New series No. | Highlights |
|---|---|---|---|---|---|
| Rosén (66) | Public health planning | Epidemiology and Public Health | 1987 | 188 | Assesses the potential for using epidemiological data from available registers as a tool for planning. Community diagnoses to analyse local data and discuss the appropriateness of different intervention strategies. The case of a community-based intervention for cardiovascular disease (CVD) prevention in Norsjö, Västerbotten, is presented. |
| Brännström (13) | Social epidemiology | Epidemiology and Public Health | 1993 | 383 | Analyses participation processes and outcome patterns in a local health programme. Discusses considering age, gender and social differences in planning and evaluation of CVD prevention programmes. |
| Lindholm (67) | Health economics | Epidemiology and Public Health | 1996 | 449 | Addresses the health economic evaluation of community-based interventions for CVD prevention with special emphasis on the Västerbotten Intervention Programme. |
| Weinehall (15) | Community intervention and CVD prevention | Epidemiology and Public Health | 1997 | 531 | Evaluates VIP from a primary health care perspective. Individual attention provided by primary care promoted risk reduction and benefits to those with low education. |
| Lindahl (68) | Insulin resistance in CVD and diabetes | Medicine | 1998 | 552 | Determines the prevalence of the insulin resistance syndrome and impaired glucose tolerance. Proinsulin identified as a risk marker of acute myocardial infarction. The CV risk profile was improved by a behavioural intervention programmme. |
| Söderberg (69) | Leptin and CVD | Medicine | 1999 | 614 | Evaluates the role of leptin, in combination with obesity, in the link between insulin resistance syndrome (IRS) and CVD. |
| Rolandsson (70) | Autoimmune diabetes | Family Medicine | 2002 | 778 | Investigates auto-antibodies against pancreatic cell antigens in the population. Body mass index as effective as glucose values in predicting diabetes. Obesity suggested to be an accelerator of type 1 diabetes |
| Johansson (71) | Haemostatic factors predicting CVD | Medicine | 2002 | 815 | Evaluated haemostatic factors predicting stroke and myocardial infarction and concluded that, in addition to traditional cardiovascular risk factors, they carry predictive information on the risk of CVD. |
| Persson (72) | Hypertension drug treatment | Family Medicine | 2003 | 837 | Diagnosed hypertension is not controlled according to guidelines. This, as well as diabetes or untreated hypertension, increases the risk of stroke. A clinical decision support system was constructed that could reduce drug costs and enhance the quality of hypertension drug treatment. |
| Emmelin (73) | Self-rated health in CVD prevention | Epidemiology and Public Health | 2004 | 884 | Discusses the ethical platform of community interventions and suggests self-rated health as an unexplored indicator, potentially important for understanding the complexity of community interventions. |
| Karlsson (74) | Metabolic disturbances and shift work | Occupational Medicine | 2004 | 891 | Metabolic risk factors were associated with shift work. Shift work was associated with increased risk for coronary heart disease (CHD), diabetes and ischemic stroke, but not with increased total mortality. |
| Hultdin (75) | Homocysteine | Medical Chemistry | 2005 | 969 | Total plasma homocysteine levels and the main genetic determinant MTHFR are independent risk factors for first stroke but not ischemic stroke. Myocardial infarction does not increase homocysteine levels. |
| Thögersen (76) | Risk factors of myocardial infarction | Medicine | 2005 | 975 | Specific biomarkers related to fibrinolysis and lipoprotein systems may improve the prediction of a first myocardial infarction. A high creatinine value was associated with increased risk of first myocardial infarction. |
| Wiklund (77) | Genetic aspects of stroke | Medicine | 2005 | 999 | The genetic component in causation of stroke was investigated. PAI-1 genotype association with risk of future ischemic stroke. This interacted with the modifiable risk marker triglyceride level. |
| Berglin (78) | Rheumatoid arthritis | Medicine | 2006 | 1001 | Anti-CCP antibodies and IgA-RF are predictors of future RA and radiological progression. Therapeutic response decreases radiological progression and bone-loss as well as lowers the level of anti-CCP. |
| van Guelpen (79) | Folate in cancers and CVD | Medical Chemistry | 2006 | 1049 | A high folate status may reduce the risk of CVD. Increased folate and B12 levels might be associated with carcinogenesis. This may have implications for the debate concerning folate fortification of foods. |
| Nafziger (80) | Obesity prevention | Epidemiology and Public Health | 2006 | 1050 | BMI increases similarly in Sweden and the USA. More adult Swedes maintained weight in recent years. The proportion of weight-gaining adults with identified CVD risk factors is smaller than those without. Obesity prevention should target those usually considered low risk. |
| Norberg (81) | Early risk markers of type 2 diabetes | Family Medicine and Epidemiology | 2007 | 1077 | Common clinical markers are sufficient for identification of subjects at risk for type 2 diabetes (T2D). Psychosocial stress increases the risk for T2D in women. Snuff is an independent risk marker of obesity. |
| Krachler (82) | Diet and CVD | Medicine | 2007 | 1108 | Describes changes in dietary habits and their relative importance as risk factors for diabetes and CVD. Potential goals for interventions are suggested. |
| Johansson (83) | Prostate cancer epidemiology | Urology and Andrology | 2008 | 1165 | Genetic variations associated with risk of prostate cancer and with prostate-cancer-specific survival are evaluated. Further studies for confirmation are needed. |
| Wennberg (84) | Physical activity and coronary heart disease | Family Medicine | 2009 | 1245 | Active commuting reduces, but the use of snuff did not increase the risk of myocardial infarction. Haemostatic and inflammatory markers may enhance the predictive ability of established risk factors. |
| Stocks (85) | Metabolic factors and cancer | Urology and Andrology | 2009 | 1267 | Elevated blood glucose increases the risk of several cancers. Overweight and metabolic aberrations increase the risk of colorectal cancer in an additive way, but reduce the risk of incident prostate cancer, whereas overweight increases the risk of fatal prostate cancer. |
Discussion
The first CVD prevention trials were conducted in the 1960s using a clinical approach and focusing on single risk factors, in particular hypercholesterolemia and hypertension. High risk individuals were identified by means of screening procedures (often directed solely at men) conducted by medical staff and medical treatment was often advocated.
A second approach was launched in the 1970s, based on experiences from these early prevention trials and a recognition that most CVD cases occur in the large part of the population with only modestly increased levels of several risk factors. Examples of programmes are the North Karelia Project, the Stanford Five City Multifactor Risk Intervention Project and the Minnesota Heart Health Program, which were centrally administered on a large scale and combined population and high-risk approaches with a focus on traditional major CVD risk factors.
The VIP belongs to a third generation of prevention programmes, introduced in the 1980s, which build on existing local structures, are small scale, action oriented and combine a broad low-risk population and high-risk individual strategies. They include biomedical risk factors and psychosocial and socioeconomic living conditions. The information and dialogue that conclude each health survey complement activities in the local community to form a population-based intervention. In the VIP, primary care continuously promotes prevention efforts in a stable, well-established and familiar structure within the local community. This enables endurance and sustainability in a way that a research project is seldom able to achieve. Opportunities to detect participants at high CVD risk and subsequently implement secondary prevention measures add extra value to these efforts.
The simple strategy is to offer a health examination and accompanying dialogue with a VIP nurse to every middle-aged Västerbotten inhabitant every 10 years. In fact, to undergo a health survey at regular intervals, comparable to mandated Swedish motor vehicle inspections, was originally suggested by an elderly Norsjö resident (44). By the end of 2007, more than 86,000 (51% women) individuals had participated in the VIP and almost 27,000 (53% women) had done so twice. The pioneer Norsjö group is now in their third round of examinations. The potential for the spread of positive attitudes and improved health literacy cannot be fully estimated despite the fact that each participant knows that there will be a follow-up survey after 10 years, which may reinforce willingness to develop healthy habits (45). Evaluations in Norsjö show that local activities, the health survey and counselling, local information papers and the food labelling system were regarded as being the most influential motivators for individuals to make healthy lifestyle changes (44). Indeed, 2007 data from the National Institute of Public Health reveal that the population in Västerbotten County in 2007 reported healthier lifestyle habits as well as better self-reported health among men compared with other counties (46).
The 10-year evaluation of the VIP showed that reductions in cholesterol and blood pressure levels were significantly greater in the Norsjö area as compared to a reference area in Northern Sweden, and that the health gap between the socially privileged and less privileged had narrowed (47). Similar results were also reported from similar intervention programmes in the South of Sweden (48). More recently, Denmark's Ebeltoft Health Promotion Project has provided further support for this idea through a randomised controlled trial, which indicated high participation rates for general health screenings and consultations in family practices to address CVD risk. These interventions resulted in reduced CVD risk and increased life expectancy without any negative long-term psychological reactions or increased health care contacts compared to the control group (49). Evaluations showed cost effectiveness in life years gained (50), and the need for health professionals to be aware of an individual's willingness or potential to achieve suggested lifestyle changes (51).
Strengths and weaknesses of the VIP
The combination of low-risk population and high-risk individual strategies creates opportunities for active participation and intervention by the general population. Evaluations show that the primary health care strategy accelerates risk factor reduction that has been achieved by the population-oriented strategy (15). Swedish district nurses possess credibility and are highly respected among the population, and the fact that the VIP participants meet a district nurse generates a good grounding for health promotion. This also contributes to the longevity of the VIP and its high participation rates. A further strength is the use of motivational interviewing for the health survey, counselling and follow up. Moreover, the link from survey participation to care is rapid and made as reassuring as possible, since high-risk participants are referred to their usual family doctor for evaluation and medical treatment. Additional value can be found in the integration of the VIP data with ordinary case records, so that the former are available to and useful for physicians in consultations not directly connected to the VIP.
The VIP data also have obvious added values for planning and resource allocation by health care providers and managers. The scientific board, which supervises and updates the procedures and health survey manual, and the County Council co-ordinating staff ensure that the VIP operates according to current scientific evidence.
Low participation rates, around 50%, at the beginning of the 1990s mirrored both the independent role of the health centres and their different prioritisation strategies. The extent of individual VIP nurses to be the driving force for the VIP may also contribute to differences between health centres regarding participation rates. This was handled by the authority, the County Council, by the decision to integrate the VIP in prescribed routines and to pay only for completed health examinations. This political determination from the very start of the VIP, to give priority to prevention, probably contributes to the longevity of the VIP not being dependent on local enthusiasts. Indeed, the questioning of the VIP has been and is still obvious among some health care staff, not least among doctors, but to a much lesser degree during recent years. The need for support, not only from politicians and the VIP administration, but also from the local leader at each health centre and among all professionals is important for the functioning of the VIP.
Evaluation of complex interventions
In 1997, the Swedish Council on Technology Assessment in Health Care conducted a systematic review of community prevention programmes launched in the 1970s and 1980s (52). Only eight programmes fulfilled the evaluation criteria: targeting multiple risk factors, including a reference population, and outcomes reported and published as changes in CVD risk factors or disease. The North Karelia Project (53) and the large American trials, i.e. the Stanford Five City project (54), the Minnesota Heart Health Program (55) and the Pawtucket Heart Health Program (56), were included. The review concluded that no reliable effects could be demonstrated in a reduction of risk factor levels or morbidity within the intervention areas beyond those in society as a whole. However, local health care providers did not play a leading part in the above-mentioned US interventions and therefore the 1997 Swedish evaluation concluded that it would be difficult to estimate possible consequences if primary care played a crucial role (52). Experiences from the three US projects indicated that active participation by community health professionals would have strengthened these projects (57), and although not a driving force, the North Karelia project demonstrated the potential of primary care in prevention. The VIP, belonging to the third generation of intervention programmes, should therefore not be dismissed based on evaluations that apply methods designed for evaluation of randomised clinical trials and that have failed to show effects in earlier prevention programmes.
Due to different types of dilution bias, it is argued that intermediate outcomes (e.g. risk factor levels rather than morbidity and mortality) should be used for evaluation of community interventions (58). A more multidisciplinary, problem-oriented strategy to evaluate community interventions that use longitudinal analyses and several methods to identify critical points from baseline to a follow-up outcome is also proposed (44, 59, 60). The VIP fulfils criteria for complex interventions (61, 62) and therefore its evaluation demands research that aims to understand the process of implementing and maintaining the VIP, evaluation of feasibility, methodology and effects of health counselling from both provider and participant perspectives. As the development of CVD and diabetes spans decades, long-term follow up is necessary for evaluations of morbidity and mortality outcomes (63–65). Obviously, the evaluation of the intervention in the VIP and the VIP as a long-term activity is still a challenge and much work remains to be done.
Implications from the VIP
The concept of the VIP, established as a collaboration between politicians and health care providers on the one side and primary care and the public on the other, forms the basis for effective implementation and endurance over time. A core component in the VIP is the active involvement of primary care, which functions as the operating machinery. The VIP data have the potential to explore disease outcomes from several perspectives, beyond the current mapping of risk markers or protective (salutogenic) factors, socioeconomic conditions, lifestyle habits and their possible associations with CVD risk markers and diabetes. The VIP may also provide data to evaluate the predictive validity of risk markers and the requirements for successful intervention. In this way, the VIP may contribute to the development of prevention methods. Blood samples stored in the Medical Biobank enable investigation of a wide range of diseases in prospective case-referent and panel studies, including cancers, neurological, inflammatory and infectious diseases, and others, in addition to CVD and diabetes.
Comprehensive demographic data and causes-of-death statistics have been collected in Sweden since the 18th century. Census data now also include information on socioeconomic conditions (e.g. education, housing, occupation and income, employment and unemployment, migration, sick leave and parental leave). There are many other registers (e.g. a register linking generations, a twin register, medical birth registration, the collection of health data in child and maternal welfare clinics, dental care, somatic and psychiatric diagnoses for hospital inpatients and outpatients). Furthermore, an increasing number of national registers are built on diagnoses, e.g. cancers, myocardial infarction, stroke or diabetes. Every Swedish citizen has a unique civic number facilitating record linkage and comprehensive analyses of dropout frequencies and distributions of non-participation. The VIP provides extensive opportunities to link local, regional and national registers and databases in order to explore a wide range of scientific questions (Fig. 6). Most research projects that are based on the VIP data, with or without accompanying data from samples in the Medical Biobank, would be impossible to carry out if they had to be organised or financed by individual research groups.
Conclusion
After more than 20 years of the VIP, there is a large, comprehensive, population-based database, a stable organisation to conduct health surveys and collect data, established expectations among middle-aged citizens to be regularly offered a VIP examination, and a solid structure to enable widespread multidisciplinary and international scientific collaboration. The value of the VIP in this respect is steadily increasing and should not be underestimated.
Conflict of interest and funding
The authors have not received any funding or benefits from industry to conduct this study.
References
- 1.Weinehall L. The emerging epidemic of cardiovascular disease. Scand J Public Health Suppl. 2003;61:5–8. doi: 10.1080/14034950310001450. [DOI] [PubMed] [Google Scholar]
- 2.Socialstyrelsen. Statistical databases – cause of death statistics [updated 2007] 2007. Available from: http://www.socialstyrelsen.se/Statistik/statistik_amne/dodsorsaker/index.htmp [cited 16 October 2007]
- 3.Granvik M. Community structure and mortality in the County of Västerbotten (in Swedish); Department of Social Medicine, Umeå University. Report No. 28, Umeå; 1978. [Google Scholar]
- 4.Eriksson CG, Granvik M, Kindblad I, Lindgren G, Nystrom L, Rosen M, et al. Health problems in a Swedish county – what can we learn from official sources? Soc Sci Med [C] 1981;15:143–51. doi: 10.1016/0160-7995(81)90029-0. [DOI] [PubMed] [Google Scholar]
- 5.Wall S, Rosen M, Nystrom L. The Swedish mortality pattern: a basis for health planning? Int J Epidemiol. 1985;14:285–92. doi: 10.1093/ije/14.2.285. [DOI] [PubMed] [Google Scholar]
- 6.Nystrom L, Rosen M, Wall S. Why are diabetes, stomach cancer and circulatory diseases more common in Northern Sweden? Scand J Prim Health Care. 1986;4:5–12. doi: 10.3109/02813438609013963. [DOI] [PubMed] [Google Scholar]
- 7.Umeå: Västerbotten County Council, Umeå University; 1984. Health problems in Västerbotten – a new agenda for planning? [in Swedish]: Stockholm: Spri; Umeå. [Google Scholar]
- 8.Statistical databases [database on the Internet] Available from: http://www.socialstyrelsen.se/english/statisticaldatabases [cited 16 October 2007]
- 9.Hälso- och Sjukvårdslag. 1982: 763 [Act on Health Care] 1982.
- 10.Västerbottensprojektet 1985–94, en länsaktion för att förebygga hjärt-kärlsjukdom och diabetes. Bilaga till Förvaltningsutskottets protokoll. 1984. Umeå.
- 11.Koutis AD, Isacsson A, Lindholm LH, Lionis CD, Svenninger K, Fioretos M. Use of primary health care in Spili, Crete, and in Dalby, Sweden. Scand J Prim Health Care. 1991;9:297–302. doi: 10.3109/02813439109018536. [DOI] [PubMed] [Google Scholar]
- 12.Brannstrom I, Emmelin M, Dahlgren L, Johansson M, Wall S. Co-operation, participation and conflicts faced in public health – lessons learned from a long-term prevention programme in Sweden. Health Educ Res. 1994;9:317–29. doi: 10.1093/her/9.3.317. [DOI] [PubMed] [Google Scholar]
- 13.Brännstrom I. PhD thesis, Umeå University. 1993. Community participation and social patterning in cardiovascular disease intervention. [Google Scholar]
- 14.Brannstrom I, Rosen M, Wall S, Weinehall L. Local health planning and intervention – the case of a Swedish municipality. Scand J Prim Health Care Suppl. 1988;1:57–64. [PubMed] [Google Scholar]
- 15.Weinehall L. PhD thesis, Umeå University. 1997. Partnership for health. On the role of primary health care in a community intervention programme. [Google Scholar]
- 16.Weinehall L, Hallgren CG, Westman G, Janlert U, Wall S. Reduction of selection bias in primary prevention of cardiovascular disease through involvement of primary health care. Scand J Prim Health Care. 1998;16:171–6. doi: 10.1080/028134398750003133. [DOI] [PubMed] [Google Scholar]
- 17.WHO. Definition and diagnosis of diabetes mellitus and intermediate hyperglycemia. [updated 2006] 2006. Geneva. Available from: http://whqlibdoc.who.int/publications/2006/9241594934_eng.pdf [cited 16 October 2007]
- 18.Lenner P, Hallmans G, Weinehall L, Stenling R. Population-based biological test bank. New possibilities for epidemiologic cancer research. Lakartidningen. 1991;88:4447–9. [PubMed] [Google Scholar]
- 19.Tibblin G, Tibblin B, Peciva S, Kullman S, Svardsudd K. The Goteborg quality of life instrument' – an assessment of well-being and symptoms among men born 1913 and 1923. Methods and validity. Scand J Prim Health Care Suppl. 1990;1:33–8. [PubMed] [Google Scholar]
- 20.Sullivan M, Karlsson J, Bengtsson C, Furunes B, Lapidus L, Lissner L. The Goteborg quality of life instrument' – a psychometric evaluation of assessments of symptoms and well-being among women in a general population. Scand J Prim Health Care. 1993;11:267–75. doi: 10.3109/02813439308994842. [DOI] [PubMed] [Google Scholar]
- 21.Henderson S, Duncan-Jones P, Byrne DG, Scott R. Measuring social relationships. The interview schedule for social interaction. Psychol Med. 1980;10:723–34. doi: 10.1017/s003329170005501x. [DOI] [PubMed] [Google Scholar]
- 22.Unden AL, Orth-Gomer K. Development of a social support instrument for use in population surveys. Soc Sci Med. 1989;29:1387–92. doi: 10.1016/0277-9536(89)90240-2. [DOI] [PubMed] [Google Scholar]
- 23.Karasek R, Theorell T. Healthy work: stress, productivity, and the reconstruction of working life. New York: Basic Books; 1990. [Google Scholar]
- 24.Theorell T, Perski A, Akerstedt T, Sigala F, Ahlberg-Hulten G, Svensson J, et al. Changes in job strain in relation to changes in physiological state. A longitudinal study. Scand J Work Environ Health. 1988;14:189–96. doi: 10.5271/sjweh.1932. [DOI] [PubMed] [Google Scholar]
- 25.Aertgeerts B, Buntinx F, Kester A. The value of the CAGE in screening for alcohol abuse and alcohol dependence in general clinical populations: a diagnostic meta-analysis. J Clin Epidemiol. 2004;57:30–9. doi: 10.1016/S0895-4356(03)00254-3. [DOI] [PubMed] [Google Scholar]
- 26.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. 2nd ed. Geneva: WHO; 2001. AUDIT, the alcohol use disorders identification test: guidelines for use in primary care. Document No WHO/MSD/MSB/01.6a. [Google Scholar]
- 27.Johansson I, Hallmans G, Wikman A, Biessy C, Riboli E, Kaaks R. Validation and calibration of food-frequency questionnaire measurements in the Northern Sweden Health and Disease cohort. Public Health Nutr. 2002;5:487–96. doi: 10.1079/phn2001315. [DOI] [PubMed] [Google Scholar]
- 28.Miller WR. Motivational interviewing: research, practice, and puzzles. Addict Behav. 1996;21:835–42. doi: 10.1016/0306-4603(96)00044-5. [DOI] [PubMed] [Google Scholar]
- 29.Persson M, Tegman J, Bohlin J. EviBase VHU. 2004. Available from: http://www.inlinedss.se [cited 12 May 2008]
- 30.Umeå: Västerbotten County Council; 2004. Manual 2004, Västerbotten Intervention Program. [Google Scholar]
- 31.Sullivan M, Karlsson J, Ware JE., Jr The Swedish SF-36 Health Survey–I. Evaluation of data quality, scaling assumptions, reliability and construct validity across general populations in Sweden. Soc Sci Med. 1995;41:1349–58. doi: 10.1016/0277-9536(95)00125-q. [DOI] [PubMed] [Google Scholar]
- 32.Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol Use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption – II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- 33.Lindahl B, Weinehall L, Asplund K, Hallmans G. Screening for impaired glucose tolerance. Results from a population-based study in 21,057 individuals. Diabetes Care. 1999;22:1988–92. doi: 10.2337/diacare.22.12.1988. [DOI] [PubMed] [Google Scholar]
- 34.Weinehall L, Ohgren B, Persson M, Stegmayr B, Boman K, Hallmans G, et al. High remaining risk in poorly treated hypertension: the ‘rule of halves’ still exists. J Hypertens. 2002;20:2081–8. doi: 10.1097/00004872-200210000-00029. [DOI] [PubMed] [Google Scholar]
- 35.Krachler B, Eliasson M, Stenlund H, Johansson I, Hallmans G, Lindahl B. Reported food intake and distribution of body fat: a repeated cross-sectional study. Nutr J. 2006;5:34. doi: 10.1186/1475-2891-5-34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Fharm E, Rolandsson O, Weinehall L. Guidelines improve general trend of lowered cholesterol levels in type 2 diabetes patients in spite of low adherence. Scand J Public Health. 2008;36:69–75. doi: 10.1177/1403494807085374. [DOI] [PubMed] [Google Scholar]
- 37.Soderberg S, Stegmayr B, Stenlund H, Sjostrom LG, Agren A, Johansson L, et al. Leptin, but not adiponectin, predicts stroke in males. J Intern Med. 2004;256:128–36. doi: 10.1111/j.1365-2796.2004.01351.x. [DOI] [PubMed] [Google Scholar]
- 38.Norberg M, Eriksson JW, Lindahl B, Andersson C, Rolandsson O, Stenlund H, et al. A combination of HbA1c, fasting glucose and BMI is effective in screening for individuals at risk of future type 2 diabetes: OGTT is not needed. J Intern Med. 2006;260:263–71. doi: 10.1111/j.1365-2796.2006.01689.x. [DOI] [PubMed] [Google Scholar]
- 39.Norberg M, Stenlund H, Lindahl B, Andersson C, Weinehall L, Hallmans G, et al. Components of metabolic syndrome predicting diabetes: no role of inflammation or dyslipidemia. Obesity (Silver Spring) 2007;15:1875–85. doi: 10.1038/oby.2007.222. [DOI] [PubMed] [Google Scholar]
- 40.Nafziger AN, Lindvall K, Norberg M, Stenlund H, Wall S, Jenkins PL, et al. Who is maintaining weight in a middle-aged population in Sweden? A longitudinal analysis over 10 years. BMC Public Health. 2007;7:108. doi: 10.1186/1471-2458-7-108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Emmelin M, Weinehall L, Stenlund H, Wall S, Dahlgren L. To be seen, confirmed and involved – a ten year follow-up of perceived health and cardiovascular risk factors in a Swedish community intervention programme. BMC Public Health. 2007;7:190. doi: 10.1186/1471-2458-7-190. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Stattin P, Bjor O, Ferrari P, Lukanova A, Lenner P, Lindahl B, et al. Prospective study of hyperglycemia and cancer risk. Diabetes Care. 2007;30:561–7. doi: 10.2337/dc06-0922. [DOI] [PubMed] [Google Scholar]
- 43.Hallmans G, Agren A, Johansson G, Johansson A, Stegmayr B, Jansson JH, et al. Cardiovascular disease and diabetes in the Northern Sweden Health and Disease Study Cohort – evaluation of risk factors and their interactions. Scand J Public Health Suppl. 2003;61:18–24. doi: 10.1080/14034950310001432. [DOI] [PubMed] [Google Scholar]
- 44.Weinehall L, Janlert U, Asplund K, Wall S. Public health work needs new evaluation models. Primary care projects are more effective than large scale campaigns. Lakartidningen. 1998;95:3812–6. [PubMed] [Google Scholar]
- 45.Coulter A, Ellins J. Effectiveness of strategies for informing, educating, and involving patients. BMJ. 2007;335:24–27. doi: 10.1136/bmj.39246.581169.80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.The National Survey of Public Health. Swedish National Institute of Public Health [updated 2008] 2008. Available from: http://www.fhi.se/templates/Page__13444.aspx [cited 15 April 2009]
- 47.Weinehall L, Hellsten G, Boman K, Hallmans G, Asplund K, Wall S. Can a sustainable community intervention reduce the health gap? – 10-year evaluation of a Swedish community intervention program for the prevention of cardiovascular disease. Scand J Public Health Suppl. 2001;56:59–68. [PubMed] [Google Scholar]
- 48.Lingfors H, Lindstrom K, Persson LG, Bengtsson C, Lissner L. Lifestyle changes after a health dialogue. Results from the Live for Life health promotion programme. Scand J Prim Health Care. 2003;21:248–52. doi: 10.1080/02813430310003282. [DOI] [PubMed] [Google Scholar]
- 49.Lauritzen T, Jensen MS, Thomsen JL, Christensen B, Engberg M. Health tests and health consultations reduced cardiovascular risk without psychological strain, increased healthcare utilization or increased costs. An overview of the results from a 5-year randomized trial in primary care. The Ebeltoft Health Promotion Project (EHPP) Scand J Public Health. 2008;36:650–61. doi: 10.1177/1403494807090165. [DOI] [PubMed] [Google Scholar]
- 50.Rasmussen SR, Thomsen JL, Kilsmark J, Hvenegaard A, Engberg M, Lauritzen T, et al. Preventive health screenings and health consultations in primary care increase life expectancy without increasing costs. Scand J Public Health. 2007;35:365–72. doi: 10.1080/14034940701219642. [DOI] [PubMed] [Google Scholar]
- 51.Bach Nielsen KD, Dyhr L, Lauritzen T, Malterud K. Long-term impact of elevated cardiovascular risk detected by screening. A qualitative interview study. Scand J Prim Health Care. 2005;23:233–8. doi: 10.1080/02813430500336245. [DOI] [PubMed] [Google Scholar]
- 52.Lundvall O, Asplund K, Cohen D, Emmelin M, Eriksson C, Janlert U, et al. Stockholm: The Swedish Council on Technology Assessment in Health Care SBU; 1997. Community intervention programs to prevent cardiovascular disease – a systematic review. Report No. 134. [Google Scholar]
- 53.Puska P, Tuomilehto J, Nissinen A, Salonen JT, Vartiainen E, Pietinen P, et al. The North Karelia project: 15 years of community-based prevention of coronary heart disease. Ann Med. 1989;21:169–73. doi: 10.3109/07853898909149928. [DOI] [PubMed] [Google Scholar]
- 54.Fortmann SP, Flora JA, Winkleby MA, Schooler C, Taylor CB, Farquhar JW. Community intervention trials: reflections on the Stanford Five-City Project experience. Am J Epidemiol. 1995;142:576–86. doi: 10.1093/oxfordjournals.aje.a117678. [DOI] [PubMed] [Google Scholar]
- 55.Luepker RV, Murray DM, Jacobs DR, Jr, Mittelmark MB, Bracht N, Carlaw R, et al. Community education for cardiovascular disease prevention: risk factor changes in the Minnesota Heart Health Program. Am J Public Health. 1994;84:1383–93. doi: 10.2105/ajph.84.9.1383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Carleton RA, Lasater TM, Assaf AR, Feldman HA, McKinlay S. The Pawtucket Heart Health Program: community changes in cardiovascular risk factors and projected disease risk. Am J Public Health. 1995;85:777–85. doi: 10.2105/ajph.85.6.777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Mittelmark MB, Hunt MK, Heath GW, Schmid TL. Realistic outcomes: lessons from community-based research and demonstration programs for the prevention of cardiovascular diseases. J Public Health Policy. 1993;14:437–62. [PubMed] [Google Scholar]
- 58.Lindholm L, Rosen M. What is the ‘golden standard’ for assessing population-based interventions? – problems of dilution bias. J Epidemiol Community Health. 2000;54:617–22. doi: 10.1136/jech.54.8.617. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Brannstrom IA, Persson LÅM, Wall SI. Towards a framework for outcome assessment of health intervention. Conceptual and methodological considerations. Eur J Public Health. 1994;4:125–30. [Google Scholar]
- 60.Wall S, Weinehall L. Public health work is improvement without impairment. Lakartidningen. 1998;95:3807–8. 11. [PubMed] [Google Scholar]
- 61.Black N. Why we need observational studies to evaluate the effectiveness of health care. BMJ. 1996;312:1215–8. doi: 10.1136/bmj.312.7040.1215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Campbell M, Fitzpatrick R, Haines A, Kinmonth AL, Sandercock P, Spiegelhalter D, et al. Framework for design and evaluation of complex interventions to improve health. BMJ. 2000;321:694–6. doi: 10.1136/bmj.321.7262.694. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Campbell NC, Murray E, Darbyshire J, Emery J, Farmer A, Griffiths F, et al. Designing and evaluating complex interventions to improve health care. BMJ. 2007;334:455–9. doi: 10.1136/bmj.39108.379965.BE. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.von Elm E, Altman DG, Egger M, Pocock SJ, Gotzsche PC, Vandenbroucke JP. Strengthening the reporting of observational studies in epidemiology (STROBE) statement: guidelines for reporting observational studies. BMJ. 2007;335:806–8. doi: 10.1136/bmj.39335.541782.AD. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Craig P, Dieppe P, Macintyre S, Michie S, Nazareth I, Petticrew M. Developing and evaluating complex interventions: the new Medical Research Council guidance. BMJ. 2008;337:a1655. doi: 10.1136/bmj.a1655. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Rosén M. PhD thesis, Umeå University. 1987. Epidemiology and planning for health: with special reference to regional epidemiology and the use of health registers. [Google Scholar]
- 67.Lindholm L. PhD thesis, Umeå University. 1996. Health economic evaluation of community-based cardiovascular disease prevention: some theoretical aspects and empirical results. [Google Scholar]
- 68.Lindahl B. PhD thesis, Umeå University. 1998. Lifestyle and health. On the role of the insulin resistance syndrome in cardiovascular disease and diabetes. The effects of lifestyle intervention. [Google Scholar]
- 69.Söderberg S. PhD thesis, Umeå University. 1999. Leptin – a risk marker for cardiovascular disease. [Google Scholar]
- 70.Rolandsson O. PhD thesis, Umeå University. 2002. Islet beta cell autoimmunity. An epidemiological and experimental study. [Google Scholar]
- 71.Johansson L. PhD thesis, Umeå University. 2002. Hemostatic factors in cardiovascular disease with special reference to stroke. [Google Scholar]
- 72.Persson M. PhD thesis, Umeå University. 2003. Bring hypertension guidelines into play. Guidelinebased decision support system for drug treatment of hypertension and epidemiological aspects of hypertension guidelines. [Google Scholar]
- 73.Emmelin M. PhD thesis, Umeå University. 2004. Self-rated health in public health evaluation. [Google Scholar]
- 74.Karlsson B. PhD thesis, Umeå University. 2004. Metabolic disturbances in shift workers. [Google Scholar]
- 75.Hultdin J. PhD thesis, Umeå University. 2005. Homocysteine in cardiovascular disease with special reference to longitudinal changes. [Google Scholar]
- 76.Thögersen A. PhD thesis, Umeå University. 2005. Risk markers for first myocardial infarction. [Google Scholar]
- 77.Wiklund P. PhD thesis, Umeå University. 2005. Genetic aspects of stroke: association and linkage studies in a northern Swedish population. [Google Scholar]
- 78.Berglin E. PhD thesis, Umeå University. 2006. Predictors of disease onset and progression in early rheumatoid arthritis: a clinical, laboratory and radiological study. [Google Scholar]
- 79.van Guelpen B. PhD thesis, Umeå University. 2006. Folate in cancer and cardiovascular disease: prospective studies from the population-based northern Sweden health and disease study. [Google Scholar]
- 80.Nafziger A. PhD thesis, Umeå University. 2006. A population perspective on obesity prevention: lessons learned from Sweden and the US. [Google Scholar]
- 81.Norberg M. PhD thesis, Umeå University. 2007. Identifying risk of type 2 diabetes: epidemiologic perspectives from biomarkers to lifestyle. [Google Scholar]
- 82.Krachler B. PhD thesis, Umeå University. 2007. Diet and cardiometabolic disease: dietary trends and the impact of diet on diabetes and cardiovascular disease. [Google Scholar]
- 83.Johansson M. PhD thesis, Umeå University. 2008. Prostate cancer aetiology: epidemiological studies of IGF- and one-carbon metabolism pathways. [Google Scholar]
- 84.Wennberg P. PhD thesis, Umeå University. 2009. Beyond the established risk factors of myocardial infarction. Lifestyle factors and novel biomarkers. [Google Scholar]
- 85.Stocks T. PhD thesis, Umeå University. 2009. Metabolic factors and cancer risk: prospective studies on prostate cancer, colorectal cancer, and cancer overall. [Google Scholar]