Abstract
OBJECTIVE
Exogenous administration of glucagon-like peptide-1 (GLP-1) or GLP-1 receptor agonists such as an exendin-4 has direct beneficial effects on the cardiovascular system. However, their effects on atherosclerogenesis have not been elucidated. The aim of this study was to investigate the effects of GLP-1 on accumulation of monocytes/macrophages on the vascular wall, one of the earliest steps in atherosclerogenesis.
RESEARCH DESIGN AND METHODS
After continuous infusion of low (300 pmol · kg−1 · day−1) or high (24 nmol · kg−1 · day−1) dose of exendin-4 in C57BL/6 or apolipoprotein E–deficient mice (apoE−/−), we evaluated monocyte adhesion to the endothelia of thoracic aorta and arteriosclerotic lesions around the aortic valve. The effects of exendin-4 were investigated in mouse macrophages and human monocytes.
RESULTS
Treatment with exendin-4 significantly inhibited monocytic adhesion in the aortas of C57BL/6 mice without affecting metabolic parameters. In apoE−/− mice, the same treatment reduced monocyte adhesion to the endothelium and suppressed atherosclerogenesis. In vitro treatment of mouse macrophages with exendin-4 suppressed lipopolysaccharide-induced mRNA expression of tumor necrosis factor-α and monocyte chemoattractant protein-1, and suppressed nuclear translocation of p65, a component of nuclear factor-κB. This effect was reversed by either MDL-12330A, a cAMP inhibitor or PKI14-22, a protein kinase A–specific inhibitor. In human monocytes, exendin-4 reduced the expression of CD11b.
CONCLUSIONS
Our data suggested that GLP-1 receptor agonists reduced monocyte/macrophage accumulation in the arterial wall by inhibiting the inflammatory response in macrophages, and that this effect may contribute to the attenuation of atherosclerotic lesion by exendin-4.
The glucagon-like peptide-1 (GLP-1) is a hormone secreted from the L-cells of the small intestine and stimulates glucose-dependent insulin response (1–3). In addition, GLP-1 has other effects that may improve the pathophysiology of the diabetic state, such as suppression of glucagon secretion (2), inhibition of gastrointestinal secretion and motility (4), and inhibition of food intake (5). Accordingly, enhancement of GLP-1 actions appears to have ideal profiles for the treatment of type 2 diabetes. However, a single administration of GLP-1 is not effective as a treatment for diabetes, because the protein is rapidly degraded by dipeptidyl peptidase-4. Thus, GLP-1 receptor agonists that are resistant to dipeptidyl peptidase-4, such as exendin-4, are currently being used for the treatment of type 2 diabetes.
Given that GLP-1 receptors are abundantly expressed in many cell types other than pancreatic islet cells, gastrointestinal cells, and neural cells, GLP-1 may play wider roles than expected. Because one of the major objectives of treatment of type 2 diabetes is to prevent cardiovascular diseases, several studies investigated the effects of GLP-1 on the cardiovascular system. With regard to the heart, exogenous administration of GLP-1 and exendin-4 has direct beneficial effects, such as improvement of left ventricular performance after myocardial infarction (6,7) and protection against ischemia (8,9). In cultured human vascular endothelial cells, one GLP-1 analog inhibited the expression of tumor necrosis factor-α (TNF-α) and hyperglycemic-mediated induction of expression of plasminogen activator inhibitor type-1 and vascular cell adhesion molecule-1 (VCAM-1) (10). In vascular endothelial cells, GLP-1 stimulates NO production, which may explain the vasodilatory effects in mesenteric arteries (11) and pulmonary artery rings (12). Indeed, it has been demonstrated that that GLP-1 ameliorates endothelial dysfunction in type 2 diabetic patients with established coronary artery disease without affecting whole-body glucose uptake (13). These data highlight the potential direct protective effects of GLP-1 on the progression of atherosclerosis. To our knowledge, however, there is little or no information on the effects of GLP-1 on atherosclerogenesis.
Atherosclerogenesis is a complex pathologic process associated with inflammatory reactions (14). Monocyte–endothelial cell interaction plays a crucial role in the formation of atheroma. Indeed, adhesion of circulating monocytes to the intimal endothelial cells is considered one of the earliest events in atherosclerogenesis (15). This process is mediated by interaction of adhesion molecules and their counterreceptors. The endothelially attached monocytes subsequently invade the vascular wall and play a central role in inflammation of the vascular wall. The latter process is mediated by several cytokines and chemokines secreted by proinflammatory macrophages. Thus, monocytes/macrophages play a pivotal role in atherosclerogenesis. At this stage, the effect of exendin-4 on the roles of monocytes/macrophages in atherosclerogenesis needs clarification.
The present study was designed to determine the effect of exendin-4 on atherosclerogenesis, with a special focus on accumulation of monocytes/macrophages in the vascular wall using en face immunohistochemistry of the endothelial surface in combination with confocal microscopy. The results indicated that exendin-4 directly suppressed the progression of atherosclerosis by downregulation of various inflammatory and adhesion molecules on monocytes/macrophages.
RESEARCH DESIGN AND METHODS
Animals.
The study protocol was approved by the Animal Care and Use Committee of Juntendo University. Male C57BL/6 mice (7 weeks old) were purchased from Oriental Yeast (Tokyo, Japan) and housed in specific pathogen–free barrier facilities at Juntendo University. Male apolipoprotein E–deficient (apoE−/−) mice (6 weeks old) were purchased from The Jackson Laboratory (Bar Harbor, ME) and housed in specific pathogen–free barrier facilities at the Institute of Nihon Bioresearch (Gifu, Japan). Mice were maintained under 12-h light/dark cycle, fed a standard rodent diet (from CLEA Japan at Nihon Bioresearch), and provided with water ad libitum, except where noted. Mice were treated with either high-dose (24 nmol · kg body wt−1 · day−1) or low-dose (300 pmol · kg body wt−1 · day−1) exendin-4 (Sigma-Aldrich, Tokyo, Japan), or with saline through a mini-osmotic pump (ALZEST, model 1004; DURECT, Cupertino, CA) that delivered the solution continuously for up to 28 days. At the age of 8 weeks, the osmotic pump was implanted under the skin of the back of each mouse after local anesthesia. The skin incision was closed with wound clip.
Preparation of cells and Western blotting analysis.
We prepared cell extracts from various samples. Livers and lungs were isolated from mice and snap-frozen in liquid nitrogen. Islets were isolated by a standard collagenase digestion method as described previously (16). Mouse aortic vascular endothelial cells were isolated and cultured as described previously (17). The cultured cells were verified as endothelial cells by positive immunostaining with anti–von Willebrand factor antibody (Dako, Carpinteria, CA) and negative immunostaining with anti–α-smooth muscle actin (Sigma-Aldrich). Mouse aortic vascular smooth muscle cells were isolated and cultured as described previously (18). The cultured cells were verified as smooth muscle cells by immunostaining using anti–α-smooth muscle actin. Peritoneal macrophages were harvested from the mice with cold PBS at 3 days after intraperitoneal injection of 3% thioglycolate media. The pooled macrophages from each mouse were cultured in RPMI 1640, supplemented with 0.2% FCS, 10 mmol/l HEPES, 1 mmol/l sodium pyruvate, 2 mmol/l l-glutamine, 100 units/ml penicillin, 100 μg/ml streptomycin, and 50 μmol/l 2-mercaptoethanol under 95% relative humidity and 5% CO2 at 37°C to allow cell adhesion. Nonadherent cells were removed by washing with PBS. Human peripheral blood mononuclear cells were isolated from whole blood collected from overnight-fasted healthy volunteers, with Mono-poly Resolving Medium (DS Pharma Biomedical, Osaka, Japan) after heparinization. Monocytes were isolated from peripheral blood mononuclear cells by positive selection using MACS CD14 microbeads (Miltenyi Biotec, Bergisch Gladbach, Germany). We confirmed that 95% of the isolated cells were CD14+ monocytes by flow cytometry analysis. Cells were cultured in RPMI 1640, supplemented with 2% FCS, 10 mmol/l HEPES, 1 mmol/l sodium pyruvate, 2 mmol/l l-glutamine, 100 units/ml penicillin, 100 μg/ml streptomycin, and 50 μmol/l 2-mercaptoethanol at 37°C under a humidified atmosphere with 5% CO2. THP-1 cells were cultured in cultured in RPMI 1640, supplemented with 10% FCS, 10 mmol/l HEPES, 1 mmol/l sodium pyruvate, 2 mmol/l l-glutamine, 100 units/ml penicillin, 100 μg/ml streptomycin, and 50 μmol/l 2-mercaptoethanol under 95% relative humidity and 5% CO2 at 37°C. Human umbilical vein endothelial cells (HUVECs) were cultured in 500-ml bottle of endothelial cell basal medium-2 and the following growth supplements: 0.2 ml hydrocortisone, 2 ml human fibroblast growth factor–basic, 0.5 ml vascular endothelial growth factor, 0.5 ml R3-IGF-1, 0.5 ml ascorbic acid, 0.5 ml heparin, 10 ml FBS, 0.5 ml human epidermal growth factor, and 0.5 ml GA-1000 (Cambrex BioScience Walkersville, Charles City, IA) under 95% relative humidity and 5% CO2 at 37°C. All samples were sonicated on ice and centrifuged at 15,000g at 4°C for 20 min. The supernatants were collected and Western blot analysis was performed using anti–GLP-1R antibody (ab3907; Abcam, Cambridge, U.K.) or rabbit anti–glyceraldehyde-3-phosphate dehydrogenase antibody (Cell Signaling Technology, Beverly, MA) as described previously (16).
IPGTT and insulin tolerance test.
The intraperitoneal glucose tolerance test (IPGTT) was performed at the age of 12 weeks (4 weeks after implantation of the osmotic pump). Briefly, 1.0 g/kg body wt glucose was injected intraperitoneally after overnight fasting. Blood glucose level was measured with a glucometer (One-Touch Ultra; Life Scan, Burnaby, Canada). Plasma insulin levels were measured using an ELISA kit (Morinaga, Kanagawa, Japan). The insulin tolerance test was performed at the age of 12 weeks with 0.75 units/kg body wt insulin (Humalin; Eli Lilly, Indianapolis, IN) after 6 h of fasting. Blood samples were collected from the retro-orbital venous plexus in awake mice to measure blood glucose and plasma insulin concentrations.
Immunohistochemistry.
After mice were killed by intraperitoneal injection of sodium pentobarbital (1 mg/kg; Abbott Laboratories), tissue preparation was performed by systemic perfusion with saline and 10% buffered formalin. Fixation was performed by immersion of the isolated thoracic aorta with 10% buffered formalin at 4°C. For en face immunohistochemistry of the endothelial surface, the thoracic aorta was cut open longitudinally along the ventral side with scissors and placed on a glass slide. Then immunohistochemistry was performed using anti-mouse Mac-2 monoclonal antibody (Dako, Cederlane, Burlington, ON, Canada). Next, each specimen was placed on a slide glass with the intimal side up, and covered with a coverslip. Specimens were viewed under a microscope (E800; Nikon, Tokyo, Japan) connected to an XYZ controller and a digital camera (Sony, Tokyo, Japan). To count the number of endothelium-adherent monocytes, we set a rectangular area with sides that were twice the length of the long and short diameters of the vessel opening of the intracostal arteries, respectively, and that were centered on the opening. The total number of Mac-2–immunopositive cells within the entire rectangular areas were counted in each aorta. The cell density in each area was then calculated as the cell count (determined by an examiner blinded to the treatment regimen) divided by the total area (19–21).
For fluorescent staining, the samples were embedded in optimal cutting temperature compound, then sectioned, air dried, and washed in PBS. After immersion in blocking solution of 10% goat serum in PBS for 30 min at room temperature, the sections were incubated overnight at 4°C in a humidified chamber for labeling with rabbit polyclonal anti-GLP1 receptor antibody (1:50, LS-A1205; MBL International, Woburn, MA), and rabbit anti–Mac-2 monoclonal antibody (1:200; Dako). The specimens were placed in the appropriate goat secondary antibody conjugated with Alexa Fluor Dyes (Invitrogen, Carlsbad, CA) and diluted 1:300 in PBS for 30 min at room temperature. The specimen was placed on a glass slide, DAPI-containing mounting medium (Vector Laboratories, Burlingame, CA) was added, and then the tissue was covered with a cover glass. Samples were viewed by confocal laser scanning microscopy (Fluoview FV1000; Olympus, Tokyo, Japan).
Quantification of atherosclerotic lesions in the aortic sinus.
The heart and the aorta were flushed with normal saline followed by 10% buffered formalin as described previously (20). For quantitative analysis of arteriosclerotic lesions in the aortic sinus, the heart was cut in two halves and the top half was embedded in optimal cutting temperature compound, then cross-sectioned at 4-μm thickness at 50-μm interval with a cryostat. Twelve consecutive sections were taken sequentially from just above the aortic valve throughout the aortic sinus and allowed to dry at room temperature for 30 min. Sections were stained with oil red O staining as described above. Then, the images were captured with ImagePro Plus software. The mean lesion area of those 12 sections was calculated and expressed in square millimeters.
Ex vivo treatment of macrophages.
The isolated macrophages were washed once and then incubated with or without 0.03, 0.3, and 3 nmol/l exendin-4 or 10 μmol/l forskolin (an adenylate cyclase activator; Sigma-Aldrich) for 1 h, followed by incubation with or without lipopolysaccharide (LPS, 1 μg/ml; Sigma-Aldrich) for 1 h. To inhibit the exenatide signal, macrophages were incubated with 5 μmol/l MDL-12330A (Sigma-Aldrich), a specific adenylate cyclase inhibitor, and 10 μmol/l PKI14-22 (Sigma-Aldrich), a protein kinase A (PKA) inhibitor, for 30 min before adding exendin-4. Control macrophages were incubated with the vehicle (DMSO, final concentration <0.1%). After treatment, total RNA was prepared for further analysis. Nuclear protein extracts were isolated from peritoneal macrophages and the content of nuclear factor-κB (NF-κB) p65 was determined using a specific ELISA kit using the method recommended by the manufacturer (Imgenex, San Diego, CA) (22).
Isolation of tissue RNA and real-time quantitative RT-PCR.
Total RNA was extracted from peritoneal macrophages using the RNA easymicro Kit (Qiagen, Tokyo, Japan) and the instructions provided by the manufacturer. First-strand cDNA was synthesized using 1 μg of total RNA with oligo-dT primers and superscript reverse transcriptase (Invitrogen) as described previously (23). The resulting cDNAs were amplified using the SYBR Green PCR kit (Applied Biosystems, Foster City, CA). Quantitative PCR was performed with an ABI Prism 7700 sequence detection system (Perkin Elmer Life Sciences, Boston, MA). The relative abundances of mRNAs were calculated by the comparative cycle of threshold method with TATA box–binding protein for mice as the invariant control.
Flow cytometry.
After collection and stabilization for 6 h, monocytes were cultured in the presence or absence of different concentrations of exendin-4 for 24 h. The culture supernatants were removed and cells washed with PBS to remove nonadherent cells. Adherent monocytes were collected by scraping with a plastic policeman and pipetting. The Fc receptors were blocked by Clear Back (human Fc receptor blocking reagent; MBL, Nagoya, Japan) for 5 min at room temperature. Then the cells were stained with phycoerythrin–labeled antibodies to anti-human CD11b or the corresponding isotype control (nonspecific mouse IgG-phycoerythrin) (BD Biosciences, Cologne, Germany) and incubated at 4°C for 15 min. Flow cytometry was performed on a Becton Dickinson FACScan System. Data were expressed as mean fluorescence intensities, relative to the control.
Data analysis.
All data are presented as mean ± SEM. Differences among multiple groups were analyzed by one-way ANOVA. Bonferroni multiple comparison test was used for comparisons among multiple treatment groups and the control group. A P value less than 0.05 denoted the presence of a statistically significant difference.
RESULTS
GLP-1 receptor is abundantly expressed in monocytes/macrophages.
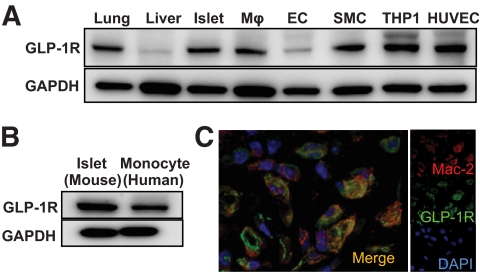
As a first step to elucidate the antiatherosclerotic effects of exendin-4, we first investigated the expression of GLP-1 receptor in cells associated with atherosclerogenesis. Similar to lung and pancreatic β-cells (24), mice peritoneal macrophages and vascular smooth muscle cells abundantly expressed GLP-1 receptor protein, and the expression level was higher than in freshly isolated endothelial cells. Similar to the expression level in macrophages, GLP-1 receptor was abundantly expressed in THP-1 cells, which are derived from human monocytes, and freshly isolated human monocytes. In contrast to the freshly isolated endothelial cells, abundant expression of GLP-1 receptor was detected in HUVECs (Fig. 1A and B). In addition, immunohistochemical staining showed GLP-1 receptor expression in cells that expressed Mac-2, a marker of macrophages located in the atherosclerotic lesions of the aortic valve of apoE−/− mice (Fig. 1C). These results may suggest that GLP-1 can directly act on monocytes or macrophages and affect the progression of atherosclerosis.
FIG. 1.
Expression of GLP-1 receptor on macrophages. A: Expression of GLP-1 receptor in murine lung and liver, isolated murine islets, isolated murine macrophages (Mϕs), cultured murine endothelial cells (ECs), cultured murine smooth muscle cells (SMCs), human monocyte derived line, THP-1 cells, and HUVECs. B: Expression of GLP-1 receptor in human monocytes from healthy subjects. C: Immunohistochemical staining of GLP-1 receptor (green) and Mac-2, a marker of macrophages (red) in atherosclerotic lesions of apoE−/− mice. (A high-quality digital representation of this figure is available in the online issue.)
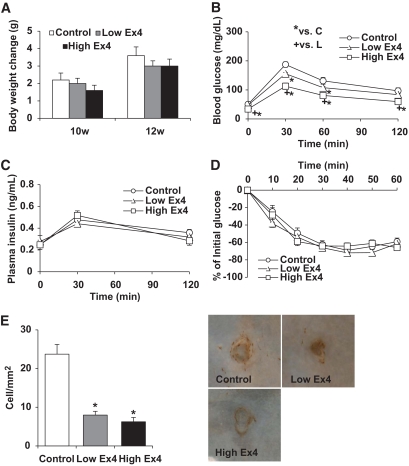
Exendin-4 reduces monocyte adhesion in C57BL/6 mice without affecting glucose tolerance.
To investigate the effect of GLP-1 receptor activation on atherosclerosis, C57BL/6 mice received continuous infusion of 300 pmol · kg−1 · day−1 (low dose) or 24 nmol · kg−1 · day−1 (high dose) exendin-4 for 28 days. During the treatment period, neither dose affected body weight (Fig. 2A). After the 24-day treatment, both doses of exendin-4 improved glucose tolerance without affecting insulin secretion (Fig. 2B and C). The results of the insulin tolerance test were similar in the two groups (Fig. 2D). Treatment with high-dose exendin-4, but not the low dose, slightly increased total cholesterol and HDL cholesterol compared with control group (Table 1). The density of monocytes that adhered to the endothelial cells of the thoracic aorta was markedly suppressed in both the low- and high-dose treatment groups, compared with control (Fig. 2E).
FIG. 2.
Exendin-4 reduced monocytic adhesion to the endothelium in C57BL/6 mice. A: Changes in body weight during treatment with exendin-4 in C57BL/6 mice (n = 6 each). B: Blood glucose concentrations during IPGTT after 24-day treatment with exendin-4 (n = 6 each). C: Plasma insulin levels during IPGTT after 24-day treatment with exendin-4 (n = 6 each). D: Results of insulin tolerance test in each group after 24-day treatment with exendin-4 (n = 6 each). E: The density of adherent Mac-2–positive cells on endothelial cells at branching areas in each group of mice after 28-day treatment (n = 6) with representative en face views of immunohistologic staining with Mac-2 antibody. Data are mean ± SEM. *P < 0.05 versus high-dose group, +P < 0.05 versus low-dose group. (A high-quality digital representation of this figure is available in the online issue.)
TABLE 1.
Results of laboratory tests in C57BL/6 mice and apoE−/− mice after 28-day treatment with exendin-4
| C57BL/6 |
ApoE−/− |
|||||
|---|---|---|---|---|---|---|
| Control | Low Ex4 | High Ex4 | Control | Low Ex4 | High Ex4 | |
| Total cholesterol (mg/dl) | 66.7 ± 2.6 | 70.5 ± 1.4 | 73.9 ± 2.2* | 522.3 ± 26.3 | 472.6 ± 22.8 | 437.2 ± 30.0* |
| LDL cholesterol (mg/dl) | 6.62 ± 0.42 | 6.33 ± 0.25 | 7.30 ± 0.59 | 136.5 ± 8.2 | 126.4 ± 7.5 | 138.4 ± 4.9 |
| HDL cholesterol (mg/dl) | 56.6 ± 2.0 | 61.0 ± 1.2 | 63.3 ± 1.5* | 16.9 ± 0.8 | 16.1 ± 1.0† | 19.0 ± 0.9 |
| TGs (mg/dl) | 42.9 ± 4.4 | 41.3 ± 3.3 | 37.6 ± 5.9 | 52.7 ± 4.2 | 54.7 ± 4.1 | 62.3 ± 4.2 |
| CM (mg/dl) | 5.95 ± 1.02 | 7.24 ± 1.13 | 4.35 ± 1.02 | 63.9 ± 4.4 | 61.6 ± 2.3 | 55.5 ± 4.2 |
| Sd-LDL (mg/dl) | 1.18 ± 0.07 | 1.16 ± 0.04 | 1.22 ± 0.09 | 27.0 ± 1.7 | 25.3 ± 1.7 | 29.2 ± 1.1 |
| A1C (%) | NA | NA | NA | 3.46 ± 0.20 | 3.64 ± 0.17 | 3.38 ± 0.12 |
Data are mean ± SE. Blood samples were collected from C57BL/6J mice (n = 6) and apoE−/− mice (n = 13 except for HbA1C, n = 6 for HbA1C) in the fasting state after 28-day treatment with exendin-4.
*P < 0.05 vs. control group.
†P < 0.05 for low Ex4 vs. high Ex4. Low Ex4, low-dose exendin-4; High Ex4, high-dose exendin-4; TG, triglycerides; CM, chylomicron; Sd-LDL, small, dense LDL; HbA1c, A1C; NA, not applicable.
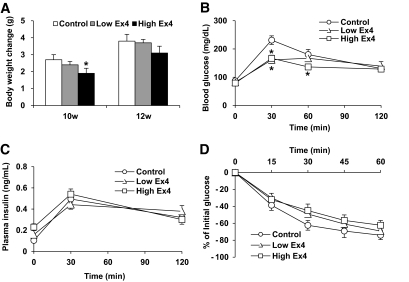
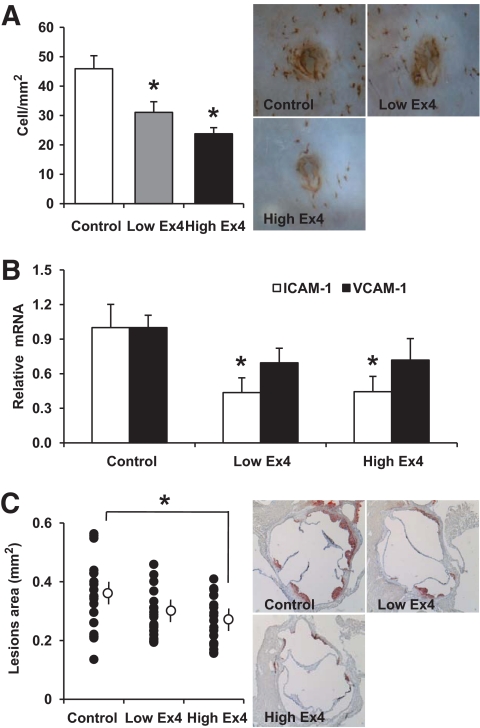
Exendin-4 reduces monocyte adhesion and atherosclerotic lesions in apoE−/− mice.
To explore the role of GLP-1 receptor activation on the progression of atherosclerosis, we treated apoE−/− mice with low- or high-dose exendin-4. Treatment with high-dose exendin-4 modestly reduced body weight gain and glucose tolerance and decreased serum total cholesterol level without affecting LDL cholesterol level (Fig. 3, Table 1). On the other hand, treatment with low-dose exendin-4 only modestly reduced glucose level at 30 min after glucose injection without affecting other parameters investigated (Fig. 3, Table 1). The density of monocytes that adhered to endothelial cells of the thoracic aorta was significantly lower in the low- and high-dose groups than the control group (Fig. 4A). Quantification of mRNA expression in the thoracic aorta showed that exendin-4 treatment significantly downregulated intercellular adhesion molecule-1 (ICAM-1) and tended to downregulate VCAM-1 (Fig. 4B). In parallel with the decreased monocyte adhesion to endothelial cells, the oil red O–positive area at the aortic valve level was significantly reduced in the high-dose group compared with the control group (Fig. 4C). The area of the atherosclerotic lesions in the low-dose group also tended to be smaller than the control group, however the difference was not significant.
FIG. 3.
The metabolic effect of exendin-4 in apoE−/− mice. A: Changes in body weight during exendin-4 treatment in apoE−/− mice (n = 13). B: Blood glucose concentrations during IPGTT after 24-day treatment with exendin-4 (n = 6). C: Plasma insulin levels during IPGTT after 24-day treatment with exendin-4 (n = 6). D: Results of insulin tolerance test in each group after 24-day treatment with exendin-4 (n = 6). Data are mean ± SEM. *P < 0.01 versus high-dose group, +P < 0.01 versus low-dose group.
FIG. 4.
Exendin-4 reduced monocyte adhesion to the endothelium and atherosclerotic lesions in apoE−/− mice. A: En face immunohistochemical staining with Mac-2 antibody of the aorta of each group. The density of adherent Mac-2–positive cells on the endothelium at branching areas in each group of mice after 28-day treatment (n = 7) and representative en face views of immunohistologic staining with Mac-2 antibody. B: Aortas harvested from each group of mice after 28-day treatment were used for isolation of total RNA. The mRNA expression levels of ICAM-1 and VCAM-1 were determined by quantitative RT-PCR. Relative gene expression is displayed as the level of expression in the test mice relative to that in the control group (set at 1.0, n = 5–7). C: Representative histologic sections of the aortic sinuses stained with oil red O after 28-day treatment. The mean area of oil red O–positive lesions was determined (n = 20). Data are mean ± SEM. *P < 0.05 versus control group. (A high-quality digital representation of this figure is available in the online issue.)
Exendin-4 reduces the inflammatory response through cAMP signaling pathway in macrophages.
The data obtained from apoE−/− mice and C57BL/6 mice suggested that exendin-4 could have beneficial effects against atherosclerosis without affecting the metabolic parameters and that it could potentially prevent the progression of atherosclerosis by its direct action on the cells involved in atherosclerogenesis. The abundant expression of GLP-1 receptor in monocytes/macrophages and the inhibitory effects of exendin-4 on monocyte adhesion on endothelial cells encouraged us to investigate the effects of exendin-4 on the inflammatory response.
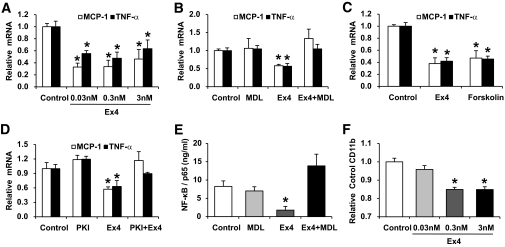
LPS is known to induce inflammatory response. Indeed, incubation with 1 μg/ml of LPS for 1 h induced ∼10-fold increases in the expression levels of TNF-α and monocyte chemoattractant protein-1 (MCP-1), a representative cytokine and a chemokine in isolated macrophages, respectively (data not shown). Thus, we investigated the effects of various concentrations of exendin-4 (0.03–3 nmol/l) in counteracting this response. Exendin-4 at all concentrations significantly suppressed LPS-induced increases in the expression levels of TNF-α and MCP-1 in macrophages (Fig. 5A). GLP-1 receptor is well-known Gs-protein–coupled receptor, thus the activation of GLP-1 receptor results in increased cAMP concentration due to activation of adenylate cyclase (25). To explore the mechanism of exendin-4–induced suppression of TNF-α and MCP-1 expression in macrophages, we preincubated peritoneal macrophages with MDL-12330A, a specific adenylyl cyclase inhibitor, or forskolin, an adenylyl cyclase activator. The addition of MDL-12330A completely suppressed the inhibitory effect of exendin-4 on the expression levels of TNF-α and MCP-1 (Fig. 5B). On the other hand, forskolin significantly suppressed LPS-induced TNF-α and MCP-1 expression in macrophages, and the levels of suppression by forskolin were similar to those of exendin-4 (Fig. 5C). These results suggest that the inhibitory effects of exendin-4 on the expression of TNF-α and MCP-1 are largely dependent on the activation of adenylate cyclase. Next, we investigated the downstream pathway of cAMP using PKI14-22, a specific PKA inhibitor. Similar to MDL-12330A, the inhibitory effect of exendin-4 was significantly reversed by PKI14-22 (Fig. 5D), suggesting the involvement of PKA in the anti-inflammatory effect of exendin-4.
FIG. 5.
Exendin-4 reduced the inflammatory response through cAMP signaling pathway in macrophages, and reduced the expression of CD11b in human monocytes. A: Peritoneal macrophages isolated from 8-week-old C57BL/6 mice were incubated with various concentrations of exendin-4 (0.03–3 nmol/l) for 1 h followed by treatment with LPS (1 μg/ml) for 1 h. Then, macrophages were used for isolation of total RNA. The mRNA expression levels of TNF-α and MCP-1 were determined by quantitative RT-PCR. Relative gene expression is displayed as the level of expression in peritoneal macrophages without the addition of exendin-4 set at 1.0 (n = 4–5). B: Peritoneal macrophages were preincubated with 5 μmol/l MDL-12330A for 30 min before the addition of 0.3 nmol/l exendin-4 and then incubated with LPS (1 μg/ml) for 1 h. Then, macrophages were used for isolation of total RNA (n = 4–6). C: Peritoneal macrophages were incubated with 0.3 nmol/l exendin-4 or 10 μmol/l forskolin for 1 h followed by LPS (1 μg/ml) for 1 h. Then, macrophages were used for isolation of total RNA (n = 4–5). D: Peritoneal macrophages were preincubated with 10 μmol/l PKI14-22 for 30 min before the addition of 0.3 nmol/l exendin-4 and then incubated with LPS (1 μg/ml) for 1 h. Then, macrophages were used for isolation of total RNA (n = 4–5). E: Peritoneal macrophages were preincubated with 5 μmol/l MDL-12330A for 30 min before the addition of 0.3 nmol/l exendin-4 and then incubated with LPS (1 μg/ml) for 1 h. Then, macrophages were used for isolation of nuclear protein extracts. The nuclear level of NF-κB p65 was determined by enzyme-linked immunosorbent assay (ELISA) (n = 3–4). F: Human monocytes isolated from healthy volunteers were incubated without or with various concentrations of exendin-4 (0.03–3 nmol/l) for 24 h. Then, the surface expression of CD11b was assessed by flow cytometry. Data are median fluorescence intensity relative to the control. *P < 0.05 versus the control group.
Although NF-κB is a major regulator of the expression of TNF-α and MCP-1, vasoactive intestinal peptide and pituitary adenylate cyclase–activating polypeptide are known to inhibit NF-κB–dependent gene activation by activation of PKA in cultured monocytic cell line THP-1 (26). Thus, we investigated the effect of exendin-4 on LPS-induced nuclear translocation of NF-κB p65 in macrophages. Without any stimulation, nuclear NF-κB p65 was not detected in peritoneal macrophages, however, stimulation with LPS robustly induced nuclear translocation of NF-κB p65 (data not shown). Such translocation was markedly suppressed by exendin-4, and this inhibitory effect was completely abolished by MDL-12330A (Fig. 5E). These results indicate that exendin-4 inhibits nuclear translocation of NF-κB p65 by activating cAMP, in parallel with the expression of TNF-α and MCP-1.
Finally, we investigated the effect of exendin-4 on human monocytes. As stated above, exendin-4 attenuated the expression of ICAM-1 in apoE−/− mice. Thus, we investigated the effects of exendin-4 on their counterreceptors, CD11b, in isolated human peripheral monocytes. Exposure to 0.3 and 3 nmol/l, but not 0.03 nmol/l, exendin-4 for 24 h significantly reduced the surface expression of CD11b, as assessed by flow cytometry (Fig. 5F). These results suggest that activation of the GLP-1 receptor has the antiatherogenic effects on human circulating monocytes.
DISCUSSION
In the present study, we provide evidence that exendin-4, a GLP-1 receptor agonist, prevents the progression of atherosclerosis in apoE−/− mice without major effects on metabolic parameters. Our data suggest that exendin-4 markedly reduced the accumulation of monocytes/macrophages in the vascular wall at least in part by suppressing the inflammatory response in macrophages through the activation of the cAMP/PKA pathway.
The results showed that the exendin-4 decreased monocyte adhesion to endothelial cells in two nondiabetic mice, C57BL6 and apoE−/− mice. In both mouse strains, exendin-4 reduced glucose level during IPGTT, however, because the two strains are nondiabetic, the effect of exendin-4 on glucose level should play only a minor effect on its antiatherosclerogenetic properties.
In this study, we confirmed the expression of GLP-1 receptor in endothelial cells, smooth muscle cells, macrophages, and monocytes. Because these cells play critical roles in the progression of atherosclerosis, GLP-1 receptor activation in these cells may be involved in atherosclerogenesis. Indeed, several groups reported the beneficial effects of GLP-1 receptor activation on endothelial cells (10–13). On the other hand, we confirmed in the present study the direct anti-inflammatory effect of GLP-1 on monocytes/macrophages. Indeed, treatment with exendin-4 at concentrations observed during treatment of humans (27,28) reduced the expression of inflammatory mediators TNF-α and MCP-1 in activated macrophages. TNF-α and MCP-1 are among the important cytokines and chemokines whose atherogenic effect has been established. Both TNF-α– and MCP-1–deficient mice have significantly reduced atherosclerotic lesions (29,30). Furthermore, forced expression of TNF-α and MCP-1 in leukocytes promotes advanced atherosclerotic lesions (29,31). Thus, in addition to the effect of GLP-1 on endothelial cells, its effect on monocytes/macrophages may also have a major impact on the attenuation of atherosclerosis.
It was reported previously that the main effects of GLP-1 are mediated through the activation of adenylate cyclase and the production of cAMP (25). Using adenylate cyclase inhibitor and activator, we also demonstrated in this study that stimulation of cAMP by exendin-4 is critical for the attenuated production of proinflammatory mediators from macrophages. This result is consistent with previous studies in which increased intracellular levels of cAMP inhibited TNF-α production and its transcription in macrophage (32–34). These data suggest that exendin-4 regulates inflammatory response of macrophages via the cAMP/PKA pathway, which inhibits proinflammatory cytokine production as reported recently (35,36). Our results showed that PKA activation and inhibition of NF-κB p65 translocation mediate overexpression of inflammatory cytokines by increased cAMP level elicited by GLP-1 receptor activation.
The adhesion of circulating monocytes to the intimal endothelial cells is thought to be one of the earliest events in the complex pathologic process of atherosclerogenesis (14,15). This can be mediated by the interaction of specific adhesion molecules on vascular endothelial cells with their integrin counterreceptors on monocytes. CD11b is an important adhesion molecule on monocytes. Activation of monocytes by cytokines, chemokines, hypercholesterolemia, and hyperglycemia leads to increased expression of this integrin, and increased monocyte expression of CD11b correlates with adhesion of these cells to the endothelium in patients with hypercholesterolemia (37). Our results showed a potential suppressive effect of exendin-4 on the surface expression of CD11b on human monocytes. On the other hand, we demonstrated that exendin-4 decreased the expression of ICAM-1, which interacts with CD11b on monocytes in apoE−/− mice. These effects may contribute at least in part to the reduced monocyte adhesion to the endothelium in vivo. However, additional experiments are required to clarify the mechanism of exendin-4–induced inhibition of CD11b expression.
In conclusion, our data suggest that GLP-1 receptor activation significantly reduced the accumulation of monocytes/macrophages in the vascular wall and eventually inhibited atherosclerogenesis by regulating inflammation in macrophages via the cAMP/PKA pathway and the integrin-related gene expression on monocytes. These unique effects of GLP-1 receptor activation may help design new therapies for cardiovascular disease in patients with type 2 diabetes.
ACKNOWLEDGMENTS
We thank Naoko Daimaru, Eriko Magoshi, and Kiyomi Nakamura for the excellent technical assistance.
No potential conflicts of interest relevant to this article were reported.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Greig NH, Holloway HW, De Ore KA, Jani D, Wang Y, Zhou J, Garant MJ, Egan JM: Once daily injection of exendin-4 to diabetic mice achieves long-term beneficial effects on blood glucose concentrations. Diabetologia 1999; 42: 45– 50 [DOI] [PubMed] [Google Scholar]
- 2.Kolterman OG, Buse JB, Fineman MS, Gaines E, Heintz S, Bicsak TA, Taylor K, Kim D, Aisporna M, Wang Y, Baron AD: Synthetic exendin-4 (exenatide) significantly reduces postprandial and fasting plasma glucose in subjects with type 2 diabetes. J Clin Endocrinol Metab 2003; 88: 3082– 3089 [DOI] [PubMed] [Google Scholar]
- 3.Parkes DG, Pittner R, Jodka C, Smith P, Young A: Insulinotropic actions of exendin-4 and glucagon-like peptide-1 in vivo and in vitro. Metabolism 2001; 50: 583– 589 [DOI] [PubMed] [Google Scholar]
- 4.Dupré J, Behme MT, McDonald TJ: Exendin-4 normalized postcibal glycemic excursions in type 1 diabetes. J Clin Endocrinol Metab 2004; 89: 3469– 3473 [DOI] [PubMed] [Google Scholar]
- 5.Szayna M, Doyle ME, Betkey JA, Holloway HW, Spencer RG, Greig NH, Egan JM: Exendin-4 decelerates food intake, weight gain, and fat deposition in Zucker rats. Endocrinology 2000; 141: 1936– 1941 [DOI] [PubMed] [Google Scholar]
- 6.Nikolaidis LA, Mankad S, Sokos GG, Miske G, Shah A, Elahi D, Shannon RP: Effects of glucagon-like peptide-1 in patients with acute myocardial infarction and left ventricular dysfunction after successful reperfusion. Circulation 2004; 109: 962– 965 [DOI] [PubMed] [Google Scholar]
- 7.Noyan-Ashraf MH, Momen MA, Ban K, Sadi AM, Zhou YQ, Riazi AM, Baggio LL, Henkelman RM, Husain M, Drucker DJ: GLP-1R agonist liraglutide activates cytoprotective pathways and improves outcomes after experimental myocardial infarction in mice. Diabetes 2009; 58: 975– 983 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bose AK, Mocanu MM, Carr RD, Brand CL, Yellon DM: Glucagon-like peptide 1 can directly protect the heart against ischemia/reperfusion injury. Diabetes 2005; 54: 146– 151 [DOI] [PubMed] [Google Scholar]
- 9.Nikolaidis LA, Elahi D, Hentosz T, Doverspike A, Huerbin R, Zourelias L, Stolarski C, Shen YT, Shannon RP: Recombinant glucagon-like peptide-1 increases myocardial glucose uptake and improves left ventricular performance in conscious dogs with pacing-induced dilated cardiomyopathy. Circulation 2004; 110: 955– 961 [DOI] [PubMed] [Google Scholar]
- 10.Liu H, Dear AE, Knudsen LB, Simpson RW: A long-acting glucagon-like peptide-1 analogue attenuates induction of plasminogen activator inhibitor type-1 and vascular adhesion molecules. J Endocrinol 2009; 201: 59– 66 [DOI] [PubMed] [Google Scholar]
- 11.Ban K, Noyan-Ashraf MH, Hoefer J, Bolz SS, Drucker DJ, Husain M: Cardioprotective and vasodilatory actions of glucagon-like peptide 1 receptor are mediated through both glucagon-like peptide 1 receptor-dependent and -independent pathways. Circulation 2008; 117: 2340– 2350 [DOI] [PubMed] [Google Scholar]
- 12.Richter G, Feddersen O, Wagner U, Barth P, Göke R, Göke B: GLP-1 stimulates secretion of macromolecules from airways and relaxes pulmonary artery. Am J Physiol 1993; 265: L374– L381 [DOI] [PubMed] [Google Scholar]
- 13.Nyström T, Gutniak MK, Zhang Q, Zhang F, Holst JJ, Ahrén B, Sjöholm A: Effects of glucagon-like peptide-1 on endothelial function in type 2 diabetes patients with stable coronary artery disease. Am J Physiol Endocrinol Metab 2004; 287: E1209– E1215 [DOI] [PubMed] [Google Scholar]
- 14.Ross R: Atherosclerosis: an inflammatory disease. N Engl J Med 1999; 340: 115– 126 [DOI] [PubMed] [Google Scholar]
- 15.Cybulsky MI, Iiyama K, Li H, Zhu S, Chen M, Iiyama M, Davis V, Gutierrez-Ramos JC, Connelly PW, Milstone DS: A major role for VCAM-1, but not ICAM-1, in early atherosclerosis. J Clin Invest 2001; 107: 1255– 1262 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Ebato C, Uchida T, Arakawa M, Komatsu M, Ueno T, Komiya K, Azuma K, Hirose T, Tanaka K, Kominami E, Kawamori R, Fujitani Y, Watada H: Autophagy is important in islet homeostasis and compensatory increase of beta cell mass in response to high-fat diet. Cell Metab 2008; 8: 325– 332 [DOI] [PubMed] [Google Scholar]
- 17.Kobayashi M, Inoue K, Warabi E, Minami T, Kodama T: A simple method of isolating mouse aortic endothelial cells. J Atheroscler Thromb 2005; 12: 138– 142 [DOI] [PubMed] [Google Scholar]
- 18.Nomiyama T, Nakamachi T, Gizard F, Heywood EB, Jones KL, Ohkura N, Kawamori R, Conneely OM, Bruemmer D: The NR4A orphan nuclear receptor NOR1 is induced by platelet-derived growth factor and mediates vascular smooth muscle cell proliferation. J Biol Chem 2006; 281: 33467– 33476 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Azuma K, Watada H, Niihashi M, Otsuka A, Sato F, Kawasumi M, Shimada S, Tanaka Y, Kawamori R, Mitsumata M: A new en face method is useful to quantitate endothelial damage in vivo. Biochem Biophys Res Commun 2003; 309: 384– 390 [DOI] [PubMed] [Google Scholar]
- 20.Mita T, Otsuka A, Azuma K, Uchida T, Ogihara T, Fujitani Y, Hirose T, Mitsumata M, Kawamori R, Watada H: Swings in blood glucose levels accelerate atherogenesis in apolipoprotein E-deficient mice. Biochem Biophys Res Commun 2007; 358: 679– 685 [DOI] [PubMed] [Google Scholar]
- 21.Yamada H, Yoshida M, Nakano Y, Suganami T, Satoh N, Mita T, Azuma K, Itoh M, Yamamoto Y, Kamei Y, Horie M, Watada H, Ogawa Y: In vivo and in vitro inhibition of monocyte adhesion to endothelial cells and endothelial adhesion molecules by eicosapentaenoic acid. Arterioscler Thromb Vasc Biol 2008; 28: 2173– 2179 [DOI] [PubMed] [Google Scholar]
- 22.Delgado M, Gonzalez-Rey E, Ganea D: The neuropeptide vasoactive intestinal peptide generates tolerogenic dendritic cells. J Immunol 2005; 175: 7311– 7324 [DOI] [PubMed] [Google Scholar]
- 23.Kumashiro N, Tamura Y, Uchida T, Ogihara T, Fujitani Y, Hirose T, Mochizuki H, Kawamori R, Watada H: Impact of oxidative stress and peroxisome proliferator-activated receptor gamma coactivator-1alpha in hepatic insulin resistance. Diabetes 2008; 57: 2083– 2091 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Baggio LL, Drucker DJ: Biology of incretins: GLP-1 and GIP. Gastroenterology 2007; 132: 2131– 2157 [DOI] [PubMed] [Google Scholar]
- 25.Brubaker PL, Drucker DJ: Minireview: glucagon-like peptides regulate cell proliferation and apoptosis in the pancreas, gut, and central nervous system. Endocrinology 2004; 145: 2653– 2659 [DOI] [PubMed] [Google Scholar]
- 26.Delgado M, Ganea D: Vasoactive intestinal peptide and pituitary adenylate cyclase-activating polypeptide inhibit nuclear factor-kappa B-dependent gene activation at multiple levels in the human monocytic cell line THP-1. J Biol Chem 2001; 276: 369– 380 [DOI] [PubMed] [Google Scholar]
- 27.Gedulin BR, Smith P, Prickett KS, Tryon M, Barnhill S, Reynolds J, Nielsen LL, Parkes DG, Young AA: Dose-response for glycaemic and metabolic changes 28 days after single injection of long-acting release exenatide in diabetic fatty Zucker rats. Diabetologia 2005; 48: 1380– 1385 [DOI] [PubMed] [Google Scholar]
- 28.Kolterman OG, Kim DD, Shen L, Ruggles JA, Nielsen LL, Fineman MS, Baron AD: Pharmacokinetics, pharmacodynamics, and safety of exenatide in patients with type 2 diabetes mellitus. Am J Health Syst Pharm 2005; 62: 173– 181 [DOI] [PubMed] [Google Scholar]
- 29.Brånén L, Hovgaard L, Nitulescu M, Bengtsson E, Nilsson J, Jovinge S: Inhibition of tumor necrosis factor-alpha reduces atherosclerosis in apolipoprotein E knockout mice. Arterioscler Thromb Vasc Biol 2004; 24: 2137– 2142 [DOI] [PubMed] [Google Scholar]
- 30.Gu L, Okada Y, Clinton SK, Gerard C, Sukhova GK, Libby P, Rollins BJ: Absence of monocyte chemoattractant protein-1 reduces atherosclerosis in low density lipoprotein receptor-deficient mice. Mol Cell 1998; 2: 275– 281 [DOI] [PubMed] [Google Scholar]
- 31.Aiello RJ, Bourassa PA, Lindsey S, Weng W, Natoli E, Rollins BJ, Milos PM: Monocyte chemoattractant protein-1 accelerates atherosclerosis in apolipoprotein E-deficient mice. Arterioscler Thromb Vasc Biol 1999; 19: 1518– 1525 [DOI] [PubMed] [Google Scholar]
- 32.Izeboud CA, Monshouwer M, van Miert AS, Witkamp RF: The beta-adrenoceptor agonist clenbuterol is a potent inhibitor of the LPS-induced production of TNF-alpha and IL-6 in vitro and in vivo. Inflamm Res 1999; 48: 497– 502 [DOI] [PubMed] [Google Scholar]
- 33.Chong YH, Shin SA, Lee HJ, Kang JH, Suh YH: Molecular mechanisms underlying cyclic AMP inhibition of macrophage dependent TNF-alpha production and neurotoxicity in response to amyloidogenic C-terminal fragment of Alzheimer's amyloid precursor protein. J Neuroimmunol 2002; 133: 160– 174 [DOI] [PubMed] [Google Scholar]
- 34.Shames BD, McIntyre RC, Jr, Bensard DD, Pulido EJ, Selzman CH, Reznikov LL, Harken AH, Meng X: Suppression of tumor necrosis factor alpha production by cAMP in human monocytes: dissociation with mRNA level and independent of interleukin-10. J Surg Res 2001; 99: 187– 193 [DOI] [PubMed] [Google Scholar]
- 35.Aronoff DM, Canetti C, Serezani CH, Luo M, Peters-Golden M: Cutting edge: macrophage inhibition by cyclic AMP (cAMP): differential roles of protein kinase A and exchange protein directly activated by cAMP-1. J Immunol 2005; 174: 595– 599 [DOI] [PubMed] [Google Scholar]
- 36.Mogi C, Tobo M, Tomura H, Murata N, He XD, Sato K, Kimura T, Ishizuka T, Sasaki T, Sato T, Kihara Y, Ishii S, Harada A, Okajima F: Involvement of proton-sensing TDAG8 in extracellular acidification-induced inhibition of proinflammatory cytokine production in peritoneal macrophages. J Immunol 2009; 182: 3243– 3251 [DOI] [PubMed] [Google Scholar]
- 37.Weber C, Erl W, Weber KS, Weber PC: HMG-CoA reductase inhibitors decrease CD11b expression and CD11b-dependent adhesion of monocytes to endothelium and reduce increased adhesiveness of monocytes isolated from patients with hypercholesterolemia. J Am Coll Cardiol 1997; 30: 1212– 1217 [DOI] [PubMed] [Google Scholar]