Abstract
OBJECTIVE
Adiponectin is one of several important metabolically active cytokines secreted from adipose tissue. Epidemiologic studies have associated low-circulating levels of this adipokine with multiple metabolic disorders including obesity, insulin resistance, type 2 diabetes, and cardiovascular disease. To investigate adiponectin-mediated changes in metabolism in vivo, we generated transgenic mice that specifically express the gene coding for human adiponectin in mouse macrophages using the human scavenger receptor A-I gene enhancer/promoter.
METHODS AND RESULTS
Using this transgenic mouse model, we found that adiponectin expression was associated with reduced whole-animal body and fat-pad weight and an improved lipid accumulation in macrophages when these transgenic mice were fed with a high-fat diet. Moreover, these macrophage Ad-TG mice exhibit enhanced whole-body glucose tolerance and insulin sensitivity with reduced proinflammatory cytokines, MCP-1 and TNF-a (both in the serum and in the metabolic active macrophage), adipose tissue, and skeletal muscle under the high-fat diet condition. Additional studies demonstrated that these macrophage adiponectin transgenic animals exhibit reduced macrophage foam cell formation in the arterial wall when these transgenic mice were crossed with an LDL receptor–deficient mouse model and were fed a high-fat diet.
CONCLUSIONS
These results suggest that adiponectin expressed in macrophages can physiologically modulate metabolic activities in vivo by improving metabolism in distal tissues. The use of macrophages as carriers for adiponectin, a molecule with antidiabetes, anti-inflammatory, and antiatherogenic properties, provides a novel and unique strategy for studying the mechanisms of adiponectin-mediated alterations in body metabolism in vivo.
The metabolic syndrome is an associated cluster of traits that include hyperinsulinemia, abnormal glucose tolerance, obesity, hypertension, and a dyslipidemia characterized by high triglycerides, low HDL cholesterol, and small-dense LDL particles leading to atherosclerosis. It is considered one of the main causes of mortality in the U.S. and in developing countries (1–3). Insulin resistance and hyperlipidemia have been linked to each of the traits, suggesting that these metabolic disorders and insulin resistance as well as hyperlipidemia are intimately related to one another. The diagnosis of the metabolic syndrome is a powerful risk factor for future development of type 2 diabetes and accelerated atherosclerosis resulting in heart attacks, stroke, and peripheral vascular disease.
Atherosclerosis is considered a chronic inflammatory disease and a disorder of lipid metabolism (4). The complex physiopathologic process is initiated by the formation of cholesterol-rich lesions in the arterial wall. The accumulation of cholesterol-rich lipoproteins in the artery wall results in the recruitment of circulating monocytes, their adhesion to the endothelium, and their differentiation into tissue macrophages. Macrophages play a crucial role in this process because they accumulate large amounts of lipid to form the foam cells that initiate the formation of the lesion and participate actively in the development of the atherosclerotic lesion. Because the transformation of macrophages into foam cells is a critical component of atherosclerotic lesion formation (5), the prevention or reversal of cholesterol accumulation or the production of inflammatory mediators in macrophage foam cells could result in protection from multiple pathological effects of atherosclerosis and other abnormal metabolic disorders.
Macrophages are a heterogeneous population of phagocytic cells found throughout the body that originate from the mononuclear phagocytic system (6). These are highly plastic cells that arise from circulating myeloid-derived blood monocytes that have entered target tissues and gained the phenotypic and functional attributes of their tissue of residence. Recent attention has focused on the potential role of macrophages in the process of metabolic diseases (7,8). It has been shown that in obesity, adipose tissue contains an increased number of resident macrophages and that, in some circumstances, macrophages can constitute up to 40% of the cell population within an adipose tissue depot (9,10); and macrophages are obviously a potential source of secreted proinflammatory factors to other tissues for insulin resistance. This correlative evidence has led to the concept that macrophages can directly influence other insulin target tissues and systemic insulin resistance. Furthermore, animal models have also been reported to evidence the causal role of the macrophage in leading to insulin resistance (11). When these animals were fed with a high-fat diet, the macrophage-specific inflammatory pathway knockout mice were relatively protected from glucose intolerance and hyperinsulinemia, and these results showed a global improvement in insulin sensitivity in all insulin-target tissues. These studies are consistent with the interpretation that the macrophage is an important, and potentially initiating, cell type in the process of inflammation-induced insulin resistance (12). To prevent macrophage infiltration into these insulin-target tissues will have beneficial effects on the inflammatory response and the abnormal metabolic state.
Adiponectin (also known as apM1, AdipoQ, Gbp28, and Acrp30) is an adipocytokine identified by screening adipose-specific genes in the human cDNA projects (13). Epidemiological evidence has indicated that circulating adiponectin levels are reduced in patients with insulin resistance, type 2 diabetes, obesity, or cardiovascular disease (14–16). When examined, low plasma adiponectin levels in these disease states are accompanied by reduced adiponectin gene expression in adipose tissue (17,18). There is also evidence that adiponectin gene polymorphisms may be associated with hypoadiponectinemia together with insulin resistance and type 2 diabetes (19). Therefore, low levels of adiponectin and adiponectin gene variation have been associated with obesity and insulin resistance. The metabolic effects and action mechanisms for adiponectin are less clear.
Adiponectin has been also shown to inhibit macrophage foam cell formation by downregulating scavenger receptor A (SR-A) expression and acyl-CoA: cholesterol-acyltransferase one (ACAT1) expression (20,21). It has been also reported that adiponectin may inhibit both the inflammatory process and atherogenesis by suppressing the migration of monocytes/macrophages and their transformation into macrophage foam cells in the vascular wall (20,22). These results suggest adiponectin's inhibitory role in macrophage foam cell formation from human monocyte-derived macrophages. Our recently published data have demonstrated that expression of adiponectin in human THP-1 macrophage cells can modulate multiple pathways of lipid metabolism and reduce macrophage foam cell formation (23). All of these data point to the anti-inflammatory and antiatherogenic role of adiponectin during atherosclerosis.
In current studies, we have generated an adiponectin macrophage-specific transgenic mouse model, and our results have shown that expression of adiponectin in mouse macrophages can significantly reduce cholesterol and triglyceride accumulation in these mouse macrophages and contribute to the reduction of macrophage foam cell formation in the atherosclerotic lesions when these macrophage modified transgenic animals are crossed with the LDL receptor (Ldlr)-deficient mouse model under a high-fat diet condition. Furthermore, the adiponectin-modified mouse macrophages also alter systemic metabolism in other metabolic active tissues with cell interactions either through infiltration or circulation by bloodstream, which influences the levels of inflammatory cytokines, monocyte chemoattractant protein (MCP)-1 and tumor necrosis factor (TNF)-α, and thus physiologically improves whole-body glucose tolerance and insulin sensitivity.
These observations suggest that adiponectin can alter the important metabolic activities in other tissues through macrophage infiltration and circulation in addition to elevated adiponectin levels. Therefore, our studies provide new insights for investigating the mechanisms of metabolism and inflammatory response in vivo.
RESEARCH DESIGN AND METHODS
To generate the macrophage adiponectin transgenic (Ad-TG) mice, full-length cDNA encoding the human adiponectin gene with a V5 epitope tag fused at the 3′ end was subcloned into a plasmid vector containing the human SR-AI gene enhancer/promoter (5.0 kb) (kindly provided by Dr. Chris Glass, Department of Cellular and Molecular Medicine, University of California at San Diego). DNA fragments (8.5 kb) starting from the enhancer/promoter to human growth hormone tail were purified before they were microinjected into mouse embryos.
Transgenic animals were created by injections of the appropriate DNA fragments into the pronucleus of inbred C57BL/6 single-cell embryos at our Transgenic Animal/Embryonic Stem Cell Core at the University of Alabama at Birmingham (UAB). All of the conformed transgenic mice were backcrossed more than 10 generations into the C57BL/6J genetic background before being used for an experiment. To investigate the atherosclerotic lesion formation, the Ad-TG mice (Ad-TG) were crossed with the Ldlr-deficient mice (Ldlrtm1Her/J, category no. 002207; The Jackson Laboratories), a common model for cardiovascular research. The Ad-TG/Ldlr and control (wild type [WT/Ldlr]) mice were fed with a high-fat diet (60% kcal % fat) from the Research Diets Company (New Brunswick, NJ) for 6 months before the atherosclerotic lesion regions were measured and analyzed.
Wild-type and transgenic mice at 20 weeks of age but fed with the high-fat diet for 16 weeks were then killed and bled by cardiac puncture. Plasma was isolated by centrifugation at 12,000g for 10 min and stored at −80°C until analyses were performed.
All of these animals were housed in a specific pathogen-free facility with 12-h light/dark cycles and received a standard laboratory chow diet except for those undergoing the high-fat diet experiments. Only male mice were used for the experiments. All animal procedures were approved by the Institutional Animal Care and Use Committee of the Animal Resources Program at UAB.
Peritoneal macrophage isolation and culture.
Macrophages were isolated from the peritoneum of 20-week-old wild-type or transgenic mice after a priming injection with 2 ml of 3% thioglycollate to elicit macrophage accumulation. Five days after the injection, mice were anesthetized with isoflurane and injected peritoneally with 5 ml cold PBS with 10 mm EDTA. The PBS lavage containing the peritoneal macrophages was removed, and the process was repeated three times for each mouse. Macrophages from each mouse were cultured separately overnight in media (RPMI-1640) containing 10% FBS, after which nonadherent cells were removed by aspiration and the remaining, adherent cells were cultured an additional 6–7 days before they were used for the experiments.
Determination of cholesterol and triglyceride concentrations in mouse macrophages and plasma.
The concentrations of cholesterol and triglyceride in mouse macrophages and plasma were determined using enzymatic colorimetric assays (Wako, Richmond, VA) according to the manufacturer's protocols. The concentrations of cellular proteins from macrophages were measured with a protein assay kit from Bio-Rad (Hercules, CA).
Inflammatory cytokine expression in metabolic tissues and plasma concentration of cytokines and insulin.
To determine the expression level of genes coding for inflammatory cytokines, total RNA was extracted from wild-type and transgenic mouse adipose and skeletal muscle tissue using a commercially available TRIzol reagent from Invitrogen (Carlsbad, CA) according to the manufacturer's instructions. The quantitative real-time PCR analysis was performed using an Mx3000P Real-Time PCR System (Stratagene). Reactions were carried out in triplicate in a total volume of 20 μl using a Brilliant SYBR Green QPCR Master Mix (Stratagene). Quantification was calculated using the starting quantity of the cDNA of interest relative to that of 18S ribosomal cDNA in the same sample.
The plasma levels of MCP-1 and TNF-α were measured by ELISA Strips (Signosis, Sunnyvale, CA) according to the manufacturer's instructions. The insulin levels in mouse plasma were measured using an ultra-sensitive mouse insulin ELISA kit from Crystal Chem (Downers Grove, IL) according to the protocols from the manufacturer.
Glucose and insulin tolerance testing.
Glucose tolerance testing and insulin tolerance testing in adiponectin transgenic and control mice were performed as previously described (24). Mice were injected with glucose or insulin at 20 weeks of age after consuming the high-fat diet for 16 weeks. To determine glucose tolerance, animals were first fasted overnight and then given an intraperitoneal injection of glucose solution (100 g glucose/l; 10 μl/g body wt). Mouse tail blood drops were taken, and glucose concentration was determined at baseline (prior to injection) and at 30, 60, 90, 120, and 150 min postinjection using a HemoCue glucose 201 glucometer. To determine insulin tolerance, mice were fasted for 6 h the morning of the determination and then administered an intraperitoneal injection of insulin solution (1.5 units insulin/kg body wt). Glucose levels were measured in blood samples collected as above described for the glucose tolerance test.
Measurements of glucose metabolism in skeletal muscle.
Insulin-stimulated glucose uptake assays in skeletal muscle strips were performed as previously described (25). For measurement of glucose transport activity, the muscle strips were dissected from control wild-type and transgenic mice at 20 weeks of age, treated with insulin (100 nmol/l) for 30 min at 37°C, and then incubated with 3H-2-deoxyglucose for 3 min at 37°C before the reaction was stopped by incubation with 1 N NaOH at 70°C for 5 min. Aliquots of the supernatant were centrifuged and added to the scintillation mixtures and then counted for the isotope activities. In these glucose uptake experiments, the distribution space of radiolabeled l-glucose was used to correct for nonspecific carryover of radioactivity with the cells and uptake of hexose by simple diffusion as previously described (26).
Oil red O staining of tissue and tissue sections.
Mice were killed after being fed the high-fat diet for 6 months. The aortas were dissected and fixed in phosphate-buffered formaldehyde (10%), and lipid accumulating in the tissue was detected by staining with Oil red O (27). The percentage of Oil red O–positive tissue was quantitated in the excised aorta between the arch and the common iliac artery in stained en face preparations.
To quantitate lipid accumulation in tissue sections, the entire aorta was harvested and prepared with frozen tissue matrix (OCT) and frozen tissue was sectioned at a thickness of 5 μm with a Cryostat for a total of 300 μm through the aortic origin beginning at the base of the aortic valve. The tissue sections were first fixed in 10% formalin for 90 min and then washed thoroughly with distilled water. These tissue sections were then incubated with a working solution of Oil red O for 3 h before the examinations were started (27).
Western blot analysis.
Mouse tissue was homogenized in tissue lysis buffer containing freshly added protease inhibitor cocktail (Sigma). Cell lysate proteins (25 μg protein) were separated by SDS-PAGE and then electrophoretically transferred onto nitrocellulose membranes and incubated overnight at 4°C with blocking solution (5% nonfat milk in Tris-buffered saline (TBS). The blocked membranes were separately incubated with the specific antibodies (1:5,000 dilutions with 1% nonfat milk in TBS) for 1 h at room temperature and washed three times with TBS buffer containing 0.1% Tween 20 for 15 min at room temperature with shaking. The secondary antibody conjugated to horseradish peroxidase (Santa Cruz Biotechnology) against the primary antibody was added, incubated, and washed as described above for the first antibody. Immunoreactive protein bands were detected using the Enhance Chemiluminescence Kit (New England Nuclear Life Science Products, Boston, MA).
Statistics.
Experimental results are reported as means ± SE. Statistical analyses were conducted using the unpaired Student's t test assuming unequal variance unless otherwise indicated. Significance was defined as P < 0.05.
RESULTS
Generation of the transgenic mouse model with adiponectin specifically expressed in macrophages.
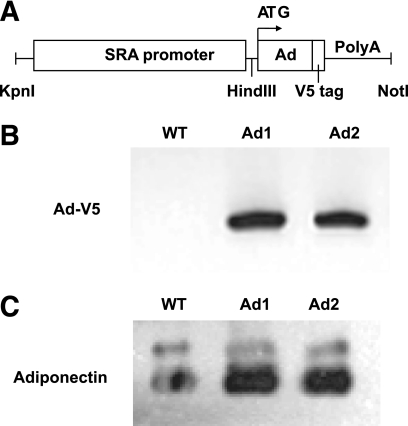
To investigate the functional roles of adiponectin in vivo, we generated adiponectin macrophage-specific transgenic mice expressing the human adiponectin gene (Ad-TG mice). Full-length cDNA encoding the human adiponectin gene with a V5 epitope tag fused at the 3′ end was subcloned into the plasmid DNA containing the human scavenger receptor A-I (SR-AI) gene enhancer/promoter (5.0 kb). DNA fragments (8.5 kb) starting from the enhancer/promoter to human growth hormone tail were purified before they were microinjected into mouse embryos (Fig. 1A). Transgenic animals were created by injections of the appropriate DNA fragments into the pronucleus of inbred C57BL/6 single-cell embryos. We identified the adiponectin transgene expression in mouse macrophages only from the transgenic animals by using a primer pair that amplified the junction sequence between the adiponectin gene and the V5 epitope tag (Fig. 1B). Adiponectin gene expression was not detected in other tissues isolated from the transgenic animals (data not shown). The levels of adiponectin protein in mouse plasma were also examined in control wild-type and transgenic mice at 6 weeks of age using an adiponectin antibody (Fig. 1C). Mice transgenic for the adiponectin gene had ∼2- to 4-fold (P < 0.01) elevated circulating adiponectin levels compared with those of control wild-type animals.
FIG. 1.
Macrophage Ad-TG mice and adiponectin expression. A: DNA construct for adiponectin macrophage-specific targeting with an SR-AI enhancer/promoter and growth hormone tail with poly A. B: Macrophages were isolated and collected from control wild-type (WT) and Ad-TG mice at 6 weeks of age, and adiponectin transgene expression was examined with RT-PCR analysis using a primer pair, which amplified the junction sequences between the adiponectin gene coding region and the V5 epitope tag. Ad1 and Ad2, macrophages from two different Ad-TG mouse lines. C: Adiponectin protein levels in plasma were examined in control wild-type and Ad-TG mice at 6 weeks of age by Western blot analyses with an adiponectin antibody against both human and mouse adiponectin. Each lane was loaded with 20 μl undiluted mouse plasma. SRA, scavenger receptor A.
Reduction of body weight and fat in Ad-TG mice fed the high-fat diet.
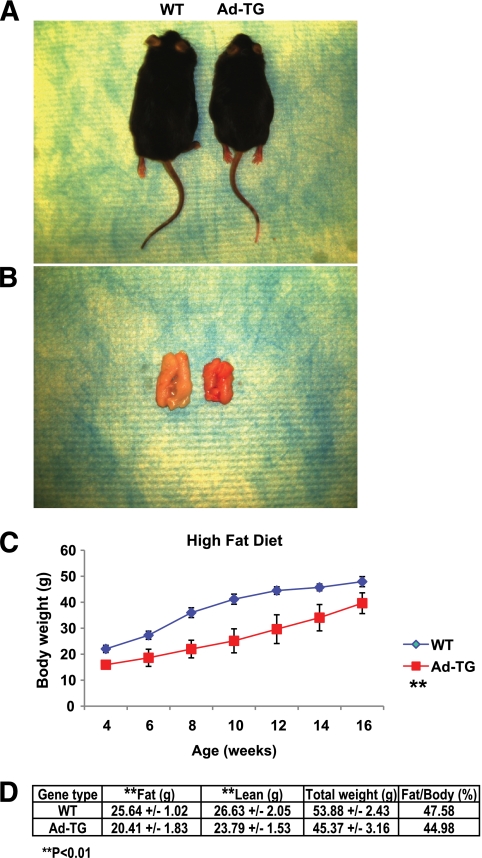
We first assessed whether growth and development were affected in Ad-TG mice compared with that in wild-type mice. There were no significant differences in reproduction, food consumption, or development between control and transgenic mice when these animals were fed chow or the high-fat diet (data not shown). However, the total body weights and visceral fat tissue masses in Ad-TG mice fed with the high-fat diet were significantly lower (P < 0.01) compared with those of control wild-type animals (Fig. 2A–C).
FIG. 2.
Decreased body weights in Ad-TG mice fed a high-fat diet. The weights of mouse bodies (A) and visceral fat pads (B) of control wild-type (WT) and Ad-TG mice fed a high-fat diet for 16 weeks and aged 20 weeks. C: Changes of body weights in wild-type and Ad-TG mice on a high-fat diet for 4–16 weeks. **P < 0.01 for all of the examined time points and n = 7 for each mouse group. D: Weights of whole body, fat, and lean muscle, as well as the percentage of fat mass to the whole-body weight in control wild-type (WT) and Ad-TG mice fed the high-fat diet for 20 weeks were determined using dual-energy X-ray absorptiometry. Weights of whole body, fat, and lean muscle were measured as grams with (± SEM), and the ratio of fat mass weight to whole-body weight was expressed as percent. n = 14 for each group of mice. **P < 0.01. (A high-quality digital representation of this figure is available in the online issue.)
To confirm these data, we conducted mouse whole-body dual-energy X-ray absorptiometry analyses (Fig. 2D) in control wild-type and Ad-TG mice fed with the high-fat diet for 16 weeks (20 weeks of age). As shown by the data presented in Fig. 2D, whole-body fat accumulation relative to the whole-body weight was significantly reduced (45 vs. 48%; P < 0.01) in transgenic mice compared with control mice—in agreement with the data observed in Fig. 2A–C.
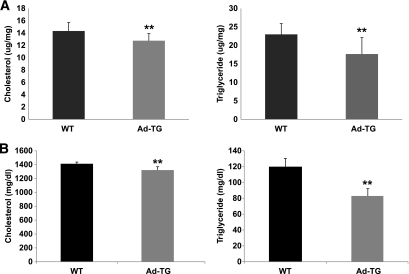
Decreased macrophage lipid accumulation, macrophage infiltration, and proinflammatory cytokine expression/secretion in Ad-TG mice.
To investigate the effect of tissue-specific adiponectin expression on macrophage metabolism, mouse peritoneal macrophages were isolated from 20-week-old control and transgenic mice and the cellular contents of cholesterol and triglyceride were determined (Fig. 3A). Both cholesterol and triglyceride levels were significantly reduced (P < 0.01) in macrophages from Ad-TG mice compared with those from the control mouse macrophages. Similarly, plasma cholesterol and triglyceride levels were significantly reduced in transgenic compared with control mice (P < 0.01) (Fig. 3B).
FIG. 3.
Decreased lipid accumulation in Ad-TG mouse macrophage and plasma. A: Mouse macrophages from 20-week-old control wild-type (WT) and Ad-TG mice fed the high-fat diet were isolated and cultured for 1 week. Cellular accumulation of cholesterol and triglycerides was assessed in the wild-type and Ad-TG macrophages using enzymatic colorimetric kits from Wako Company. Cellular lipid mass was normalized using cellular protein levels, which were determined using a protein analysis kit from the Bio-Rad. B: Mouse plasmas from 20-week-old control wild-type (WT) and Ad-TG mice fed with the high-fat diet were analyzed using enzymatic colorimetric kits from Wako Company. Means ± SE from three separate experiments with triplicate samples (n = 9 for each group) were examined. **P < 0.01.
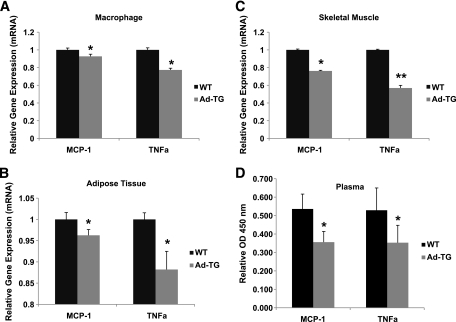
We also examined the impact of adiponectin expression in macrophages from transgenic mice on MCP-1 and TNF-α gene expression in macrophage, adipose tissue, and skeletal muscle, as well as plasma levels of these proinflammatory cytokines in animals fed the high-fat diet. The expression of the adiponectin gene in Ad-TG mouse macrophages led to a reduced expression of both the MCP-1 and TNF-α genes in macrophages and adipose and skeletal muscle tissues compared with those cells or tissues from the control animals (Fig. 4A–C). Similarly, the plasma concentrations of MCP-1 and TNF-α were significantly reduced in transgenic compared with those in control mice (Fig. 4D). Thus, the expression and secretion of adiponectin in mouse macrophages resulted in favorable changes not only in macrophage lipid metabolism but also in the expression of proinflammatory cytokines in macrophage, adipose tissue, and skeletal muscle in vivo.
FIG. 4.
Decreased proinflammatory cytokines in Ad-TG mice. Control wild-type (WT) and Ad-TG mice were fed with the high-fat diet for 20 weeks, and mouse macrophages (A), adipose tissues (B), and skeletal muscle tissues (C) were dissected. Total RNA was isolated from these tissues, cDNAs were synthesized, and quantitative PCR was performed with MCP-1 and TNF-α gene primers. D: Control wild-type and Ad-TG mice fed the high-fat diet for 20 weeks were killed and bled by cardiac puncture, and mouse plasma was collected to analyze the MCP-1 and TNF-α levels. Mean ± SE from three separate experiments with triplicate samples (n = 9 for each group) are presented. *P < 0.05; **P < 0.01.
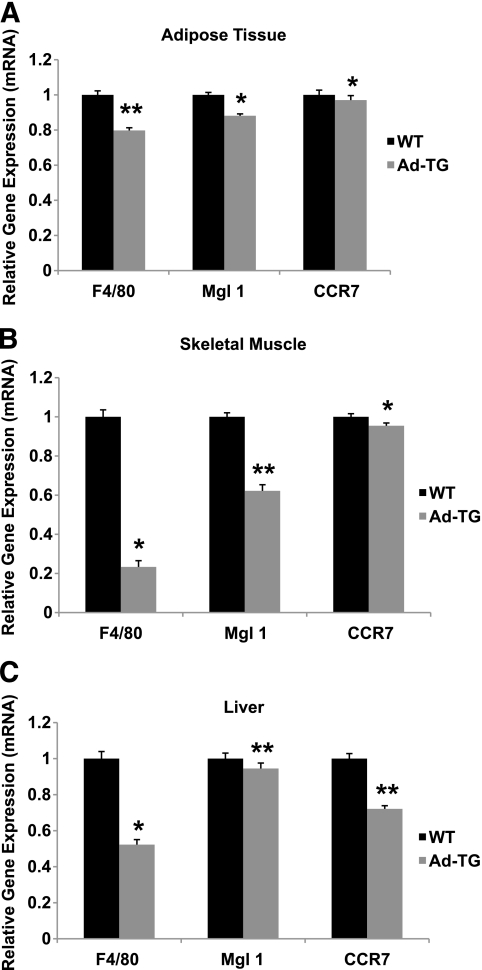
To further investigate whether these reduced proinflammatory cytokines from the metabolic active tissues of Ad-TG mice was due to the decreased macrophage filtrations in these tissues, we next examined the macrophage accumulation by detecting macrophage-specific F4/80, macrophage galactose N-acetyl-galactosamine–specific lectin 1 (MglI, a marker for an alternatively activated macrophage [M2a] phenotype), and chemokine receptor 7 (CCR7, a marker for the classically activated macrophage [M1] phenotype) gene expression in adipose, skeletal muscle, and liver tissues (Fig. 5A–C). The percentage of these macrophage-specific gene-expressing cells in these active metabolic tissues was markedly lower than that of control wild-type animals. Especially, the F4/80 gene, a marker specific for mature macrophages associated with “crown-like structure” in mice fed a high-fat diet, was significantly decreased in the three active metabolic tissues from Ad-TG mice.
FIG. 5.
Reduced macrophage accumulation in Ad-TG mice. Control wild-type (WT) and Ad-TG mice were fed with the high-fat diet for 20 weeks; and adipose tissue (A), skeletal muscle (B), and liver (C) were dissected. Total RNA was isolated from these tissues, cDNAs were synthesized, and quantitative PCR was performed with F4/80, MglI, and CCR7 gene primers. Means ± SE from three separate experiments with triplicate samples (n = 9 for each group) are presented. *P < 0.05; **P < 0.01.
Improved glucose tolerance and insulin sensitivity in Ad-TG mice.
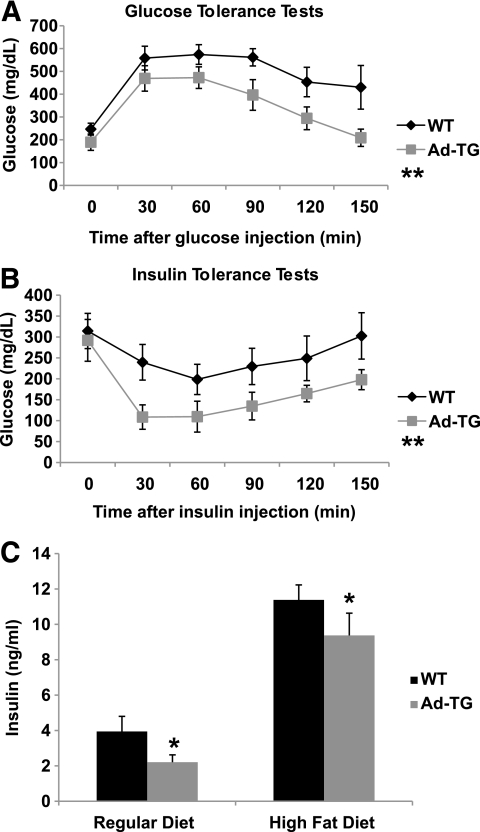
To investigate systemic insulin sensitivity in vivo, we performed glucose tolerance and insulin tolerance tests in the control and transgenic mice fed the high-fat diet for 16 weeks. Plasma glucose levels were consistently higher (P < 0.01) at baseline and during the glucose tolerance tests in control wild-type animals compared with levels in transgenic mice (Fig. 6A). As shown in Fig. 6B, plasma glucose levels were also consistently higher (P < 0.01) in control wild-type mice when insulin was injected for the insulin tolerance tests compared with levels in transgenic mice. Plasma insulin levels at baseline in transgenic mice fed either regular chow or the high-fat diet were significantly lower (P < 0.05) than the insulin levels in wild-type mice (Fig. 6C). Thus, selective, specific expression of adiponectin in mouse macrophages influences systemic metabolism in distal tissues as demonstrated by significantly reduced hyperglycemia and improved insulin sensitivity.
FIG. 6.
Glucose tolerance tests, insulin tolerance tests, and measurement of insulin levels in plasma. A: Glucose tolerance tests were performed on control wild-type (WT) and Ad-TG mice fed with the high-fat diet for 16 weeks. Experiments were performed in fasting overnight male mice. Glucose solutions were injected into the peritoneal cavity at a dose of 1.0 ml/kg (1 mol/l solution). Blood was collected via tail vein at the indicated time points. Glucose concentration in plasma was measured using a glucometer (Precision); n = 6 in each group of mice. B: Insulin tolerance tests were performed on control wild-type and Ad-TG mice under the high-fat diet condition for 16 weeks. Experiments were conducted similarly to the methodology described above for the glucose tolerance tests, with fasting 6 h before the injections and insulin solutions were injected into peritoneal cavity at a dose of 0.5 units/kg. Blood was collected via tail vein at the indicated time points, and glucose levels were measured; n = 6 in each group of animals. C: Insulin levels in plasmas from control wild-type and Ad-TG mice fed either with a regular diet or the high-fat diet at 20 weeks of age were measured using an ultrasensitive mouse insulin ELISA kit. Error bars represent ± SEM. *P < 0.05; **P < 0.01.
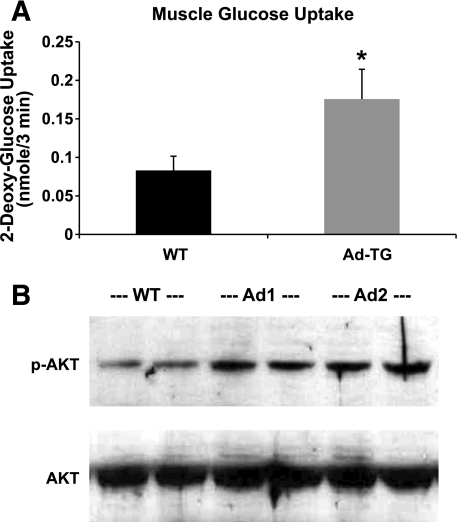
Glucose uptake and insulin-signaling pathway in mouse skeletal muscle.
To further investigate the role of adiponectin in glucose homeostasis, we assessed insulin-stimulated glucose transport activity in skeletal muscle tissues from both control wild-type and Ad-TG mice fed the high-fat diet for 16 weeks (Fig. 7A). Insulin-augmented glucose uptake in skeletal muscle from Ad-TG mice was significantly increased, by 47% (P < 0.05), compared with the levels in wild-type mice. These results indicated that macrophage adiponectin expression can significantly enhance insulin-stimulated glucose transport capacity in skeletal muscle, suggesting a novel role of macrophage adiponectin in improving insulin sensitivity in this target tissue. Thus, the expression and secretion of adiponectin from macrophages transgenic for the adiponectin gene resulted in favorable changes in vivo in insulin-stimulated glucose transport in skeletal muscle—further demonstrating the beneficial effects of macrophage-produced adiponectin on glucose metabolism in distal tissues of this transgenic mouse model.
FIG. 7.
Enhanced glucose uptake and insulin signaling in skeletal muscle from Ad-TG mice. A: Insulin-stimulated glucose uptake assays, in muscle strips containing samples from control wild-type (WT) and Ad-TG mice at 20 weeks of age on the high-fat diet for 16 weeks, were performed in vitro. For measurement of glucose-transport activity, the muscle strips were treated with insulin (100 nmol/l) for 30 min at 37°C and then treated with 3H-2-deoxyglucose for 3 min at 37°C before treatment with 1 N NaOH at 70°C for 5 min; the aliquots of the supernatant were centrifuged and added to the scintillation mixtures and then counted for the isotope activities. Results represent the means ± SE from three separate experiments with five to six mice per group of mice. *P < 0.05 for comparison of insulin-stimulated control wild-type and insulin-stimulated Ad-TG mice. B: Dissected skeletal muscle strips, from control wild-type or Ad-TG (two subtypes: Ad1 and Ad2) mice fed for 16 weeks with the high-fat diet, were treated with 100 nmol/l insulin for 30 min, and the total proteins were extracted for immunoblot analyses using antibodies against phosphorylated Akt (p-AKT) (serine 473) or total Akt. Results represent one of the three separate experiments.
We next asked whether macrophage adiponectin expression would also affect insulin signaling in the skeletal muscle. Akt phosphorylation was assessed under insulin-stimulated conditions in skeletal muscle tissues from control and Ad-TG mice fed the high-fat diet for 16 weeks (Fig. 7B). Serine phosphorylation of Akt (serine 473) was enhanced with insulin stimulation in the Ad-TG mouse skeletal muscles compared with those from the wild-type animals.
Decrease of macrophage foam cell formation in atherosclerotic lesions of Ad-TG mice.
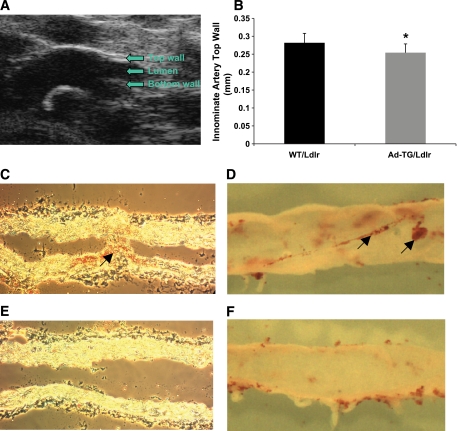
Since macrophages play a crucial role in atherosclerosis as a result of their potential to accumulate large amounts of lipid and to form the foam cells that are the hallmark of the atherosclerotic lesion, we determined whether adiponectin expression by macrophages could modify macrophage lipid homeostasis and reduce the lipid accumulation in this cell type that is characteristic of foam cell formation and of mouse atherosclerotic lesions in vivo. We first crossed mice transgenic for the human adiponectin gene with Ldlr-deficient mice, which is a common mouse model for cardiovascular research. We then fed the Ad-TG/Ldlr and the control WT/Ldlr mice with the high-fat diet for 6 months to enable the development of atherosclerotic lesions in arterial vessels.
We first quantitated the extent of atherosclerosis in this mouse model by measuring the thickness of the innominate artery wall in atherosclerotic lesions of the control and double-crossed Ad-TG mice using an in vivo imaging system (Vevo 770 μ-ultrasound system; VisualSonics company) (Fig. 8A). Quantification of these real-time physiological data showed reduced atheroaclerosis (reduced artery wall thickness) in Ad-TG/Ldlr mice compared with that in control animals (Fig. 8B).
FIG. 8.
Analysis of mouse arterial vessels and atherosclerotic lesions. A: the image indicates how to measure the top wall, lumen, and bottom wall of an innominate artery using a Vevo 770 μ-ultrasound in vivo imaging system for the atherosclerotic lesion area. B: The thickness of the innominate artery top walls in the atherosclerotic lesion areas from control WT-Ldlr (n = 11) and Ad-TG/Ldlr (n = 10) mice fed with the high-fat diet for 6 months were measured and analyzed with an S-Mode Protocol with a Vevo 770 μ-ultrasound imaging system. Error bars represent ±SEM. *P < 0.05. C and D: Control WT/Ldlr mice fed with the high-fat diet for 6 months were analyzed using Oil red O staining for 24 h for lipid-loaded foam cells (one arrow) in tissue longitudal section (C) and fatty strips (two arrows) in en face artery dissection (D). E and F: tissue longitudal section (E) and en face artery dissection (F) of arterial vessels from Ad-TG/Ldlr mice fed with the high-fat diet for 6 months. (A high-quality digital representation of this figure is available in the online issue.)
To confirm the results of the in vivo imaging analysis, the control and Ag-TG animals were also killed to enable examination of the arteries using histological analysis and en face artery dissection. Serial 5-μm-thickness cross-sections were then generated from the aortic origin beginning at the base of the aortic valve. The tissue sections and en face artery dissection were stained with the Oil red O solution (Fig. 8C–F) as previously described (27). Tissue morphological analysis of the artery sections revealed significantly increased Oil red O staining material in the arterial vessels from control mice (Fig. 8C and D) compared with arterial vessels from Ad-TG/Ldlr mice (Fig. 8E and F). These data suggest that fewer foam cells were formed in the arterial vessels from Ad-TG/Ldlr mice than those from the control WT-Ldlr animals.
DISCUSSION
Adiponectin is naturally expressed and secreted exclusively from adipocytes, and adiponectin expression is undetectable in macrophages. To investigate the mechanisms of adiponectin-mediated alterations of whole-body metabolism in vivo, we developed a mouse model in which the adiponectin gene was specifically expressed in macrophages using a human SR-AI enhancer/promoter. Our studies have shown that adiponectin expression in vivo by macrophages made transgenic for the human adiponectin gene can significantly decrease cholesterol and triglyceride accumulation in the macrophages. This altered macrophage metabolism presumably results either from reduced lipid uptake into the cells or from enhanced HDL cholesterol–mediate efflux, as we described previously in human THP-1 macrophages (23). Furthermore, the adiponectin-modified macrophages infiltrate or circulate into other metabolically active tissues such as adipose and skeletal muscle tissues, and there they can influence favorable changes in multiple metabolic pathways in these tissues. As demonstrated by our present data, macrophage-produced adiponectin can effect favorable alternations in proinflammatory cytokine release, glucose uptake, and the insulin-signaling pathway. Because macrophages in the arterial wall may be converted to the cholesterol-laden foam cells during atherogenesis, we crossed our macrophage Ad-TG mouse with the Ldlr-deficient mouse, a standard animal model for atherosclerosis. Our data clearly showed that macrophage foam cell formation in atherosclerotic lesions was significantly reduced in this double-crossed mouse model. These results suggest that adiponectin plays an important role in whole-body metabolism by modulating inflammatory and metabolic signaling pathways, by improving glucose tolerance and insulin resistance, and by reducing atherogenesis, which are typical characteristics of the metabolic syndrome.
We demonstrated previously that when adiponectin was overexpressed in mouse 3T3-L1 adipocytes, insulin-stimulated glucose uptake was increased in these fat cells (28). Similar results were also reported when adiponectin was overexpressed in vivo in adipose tissue of ob/ob mice, which are leptin deficient and have abnormal glucose and insulin levels. These ob/ob Ad-TG mice showed normalized glucose and insulin levels, with an improvement in insulin sensitivity even though they were morbidly obese with significantly higher levels of adipose tissue than their ob/ob littermates. Therefore, modestly increasing the levels of circulating adiponectin in these transgenic mice completely rescued the diabetic phenotype in ob/ob mice (29). Interestingly, our transgenic mouse model with macrophages expressing adiponectin not only showed improved insulin sensitivity and inflammation in skeletal muscle and adipose tissues but fat mass, macrophage and plasma lipid accumulation, and foam cell formation was also favorably reduced resulting from the adiponectin expressed in mouse macrophage cells. Thus, using macrophages as the carriers for in vivo delivery of adiponectin, which is an antidiabetic, anti-inflammatory and antiatherogenic cytokine, may provide a novel, unique strategy to develop a new therapeutic application for the treatment of human metabolic syndrome.
It has recently been reported that in an Ad-TG mouse model, adiponectin specifically expressed in liver and macrophage infiltration in adipose tissue was reduced (30). Interestingly, in our macrophage Ad-TG animals, we did not observe a significant change for macrophage subtypes (e.g., from M1 to M2) in adipose, skeletal muscle, or liver tissues even though all of the macrophage infiltration in these tissues was reduced. This may result in altered metabolism in these active metabolic tissues since the infiltrated macrophages also exhibit reduced inflammatory cytokine secretion. Similar to the results reported from studies of liver Ad-TG mice, the expression levels of adiponectin receptors in skeletal muscle and adipose tissues were not significantly altered (data not shown).
Although adiponectin is a specific adipokine expressed and secreted physiologically only from the adipocytes, our results show that adiponectin from the modified macrophages can also exert powerful anti-inflammatory and antiatherogenic effects on whole-body metabolism. Thiazolidenediones, which are antidiabetic drugs, have been shown to increase adiponectin expression and plasma concentrations in obese type 2 diabetic patients (31,32); consistent with these reports, our current data have further demonstrated that the increased adiponectin concentrations from macrophages link to the decreased proinflammatory cytokines in the metabolic active cells/tissues as well as plasma.
The molecular basis of the cell/tissue interactions among adiponectin-expressing macrophages and other metabolic active tissues is still not fully understood. It is not clear how the macrophage-produced adiponectin directly influences productions of proinflammatory cytokines in macrophages or adipose and skeletal muscle tissues. It is not clear whether these favorable changes result from the secretion of other anti-inflammatory molecules from the adiponectin-modified macrophages or the reduced lipid accumulation and inflammatory response in thee macrophages result in reduced negative impact when the macrophages reside in other tissues or circulate inside other tissues via circulation system. Clearly, additional studies are required, and the potential for other cellular or molecular physiological effects among these metabolically active tissues should be further pursed in the future. Our macrophage Ad-TG mouse model provides an excellent research system for investigating and evaluating the potential role of these physiological mechanisms in vivo. Our current results from these unique mouse models also provide new insight into the prevention and therapy of metabolic syndrome in humans.
ACKNOWLEDGMENTS
We are grateful to the UAB Diabetes Research and Training Center for providing outstanding core services (supported by NIH 1P60DK0797626-01). This work was supported by grants from the National Institutes of Health (PO1-HL55782 and DK-38764), the Merit Review Program of the Medical Research Service of the Department of Veterans Affairs to (W.T.G. and R.L.K.), and the American Diabetes Association (1-07-RA-49) (to Y.F.).
No potential conflicts of interest relevant to this article were reported.
We thank Dr. Chris Glass (University of California, San Diego, San Diego, CA) for kindly providing the plasmid vector containing the SR-AI enhancer/promoter.
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
REFERENCES
- 1.Reaven GM: Role of insulin resistance in human disease. Diabetes 1988; 37: 1595– 1606 [DOI] [PubMed] [Google Scholar]
- 2.Reaven GM: Insulin resistance, hyperinsulinemia, hypertriglyceridemia, and hypertension. Diabetes Care 1991; 14: 195– 202 [DOI] [PubMed] [Google Scholar]
- 3.DeFronzo RA, Ferrannini E: Insulin resistance: a multifaceted syndrome responsible for NIDDM, obesity, hypertension, dyslipidemia, and atherosclerotic cardiovascular disease. Diabetes Care 1991; 14: 173– 194 [DOI] [PubMed] [Google Scholar]
- 4.Lusis A: Atherosclerosis. Nature 2000; 407: 233– 241 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Ross R: The pathogenesis of atherosclerosis: a perspective for the 1990s. Nature 1993; 362: 801– 809 [DOI] [PubMed] [Google Scholar]
- 6.Mantovani A, Sica A, Locati M: Macrophage polarization comes of age. Immunity 2005; 23: 344– 346 [DOI] [PubMed] [Google Scholar]
- 7.Bouloumie A, Curat CA, Sengenes C, Lolmede K, Miranville A, Busse R: Role of macrophage tissue infiltration in metabolic diseases. Curr Opin Clin Nutr Metab Care 2005; 8: 347– 354 [DOI] [PubMed] [Google Scholar]
- 8.Kanda H, Tateya S, Tamori Y, Kotani K, Hiasa K, Kitazawa R, Kitazawa S, Miyachi H, Maeda S, Egashira K, Kasuga M: MCP-1 contributes to macrophage infiltration into adipose tissue, insulin resistance, and hepatic steatosis in obesity. J Clin Invest 2006; 116: 1494– 1505 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Weisberg SP, McCann D, Desai M, Rosenbaum M, Leibel RL, Ferrante AW: Obesity is associated with macrophage accumulation in adipose tissue. J Clin Invest 2003; 112: 1796– 1808 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, Sole J, Nichols A, Ross JS, Tartaglia LA, Chen H: Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest 2003; 112: 1821– 1830 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Arkan MC, Hevener AL, Greten FR, Maeda S, Li Z-W, Long JM, Wynshaw-Boris A, Poli G, Olefsky J, Karin M: IKK-beta links inflammation to obesity-induced insulin resistance. Nat Med 2005; 11: 191– 198 [DOI] [PubMed] [Google Scholar]
- 12.Nguyen MTA, Favelyukis S, Nguyen AK, Reichart D, Scott PA, Jenn A, Liu-Bryan R, Glass CK, Neels JG, Olefsky JM: A subpopulation of macrophages infiltrates hypertrophic adipose tissue and is activated by free fatty acids via Toll-like receptors 2 and 4 and JNK-dependent pathways. J Biol Chem 2007; 282: 35279– 35292 [DOI] [PubMed] [Google Scholar]
- 13.Scherer PE, Williams S, Fogliano M, Baldini G, Lodish HF: A novel serum protein similar to C1q, produced exclusively in adipocytes. J Biol Chem 1995; 270: 26746– 26749 [DOI] [PubMed] [Google Scholar]
- 14.Arita Y, Kihara S, Ouchi N, Takahashi M, Maeda K, Miyagawa J, Hotta K, Shimomura I, Nakamura T, Miyaoka K, Kuriyama H, Nishida M, Yamashita S, Okubo K, Matsubara K, Muraguchi M, Ohmoto Y, Funahashi T, Matsuzawa Y: Paradoxical decrease of an adipose-specific protein, adiponectin, in obesity. Biochem Biophys Res Commun 1999; 257: 79– 83 [DOI] [PubMed] [Google Scholar]
- 15.Lindsay RS, Funahashi T, Hanson RL, Matsuzawa Y, Tanaka S, Tataranni PA, Knowler WC, Krakoff J: Adiponectin and development of type 2 diabetes in the Pima Indian population. Lancet 2002; 360: 57– 58 [DOI] [PubMed] [Google Scholar]
- 16.Lindsay RS, Funahashi T, Krakoff J, Matsuzawa Y, Tanaka S, Kobes S, Bennett PH, Tataranni PA, Knowler WC, Hanson RL: Genome-wide linkage analysis of serum adiponectin in the Pima Indian population. Diabetes 2003; 52: 2419– 2425 [DOI] [PubMed] [Google Scholar]
- 17.Hotta K, Funahashi T, Bodkin NL, Ortmeyer HK, Arita Y, Hansen BC, Matsuzawa Y: Circulating concentrations of the adipocyte protein adiponectin are decreased in parallel with reduced insulin sensitivity during the progression to type 2 diabetes in rhesus monkeys. Diabetes 2001; 50: 1126– 1133 [DOI] [PubMed] [Google Scholar]
- 18.Weyer C, Funahashi T, Tanaka S, Hotta K, Matsuzawa Y, Pratley RE, Tataranni PA: Hypoadiponectinemia in obesity and type 2 diabetes: close association with insulin resistance and hyperinsulinemia. J Clin Endocrinol Metab 2001; 86: 1930– 1935 [DOI] [PubMed] [Google Scholar]
- 19.Menzaghi C, Trischitta V, Doria A: Genetic influences of adiponectin on insulin resistance, type 2 diabetes, and cardiovascular disease. Diabetes 2007; 56: 1198– 1209 [DOI] [PubMed] [Google Scholar]
- 20.Ouchi N, Kihara S, Arita Y, Nishida M, Matsuyama A, Okamoto Y, Ishigami M, Kuriyama H, Kishida K, Nishizawa H, Hotta K, Muraguchi M, Ohmoto Y, Yamashita S, Funahashi T, Matsuzawa Y: Adipocyte-derived plasma protein, adiponectin, suppresses lipid accumulation and class A scavenger receptor expression in human monocyte-derived macrophages. Circulation 2001; 103: 1057– 1063 [DOI] [PubMed] [Google Scholar]
- 21.Furukawa K, Hori M, Ouchi N, Kihara S, Funahashi T, Matsuzawa Y, Miyazaki A, Nakayama H, Horiuchi S: Adiponectin down-regulates acyl-coenzyme A: cholesterol acyltransferase-1 in cultured human monocyte-derived macrophages. Biochem and Biophy Res Commun 2004; 317: 831– 836 [DOI] [PubMed] [Google Scholar]
- 22.Ouchi N, Kihara S, Funahashi T, Matsuzawa Y, Walsh K: Obesity, adiponectin and vascular inflammatory disease. Curr Opin Lipidol 2003; 14: 561– 566 [DOI] [PubMed] [Google Scholar]
- 23.Tian L, Luo N, Klein RL, Chung BH, Garvey WT, Fu Y: Adiponectin reduces lipid accumulation in macrophage foam cells. Atherosclerosis 2009; 202: 152– 161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Maeda K, Cao H, Kono K, Gorgun CZ, Furuhash M, Uysal KT, Cao Q, Atsumi G, Malone H, Krishnan B, Minokoshi Y, Kahn BB, Parker PA, Hotamisligil GS: Adipocyte/macrophage fatty acid binding proteins control integrated metabolic responses in obesity and diabetes. Cell Metabolism 2005; 1: 107– 119 [DOI] [PubMed] [Google Scholar]
- 25.Wredenberg A, Freyer C, Sandström ME, Katz A, Wibom R, Westerblad H, Larsson NG: Respiratory chain dysfunction in skeletal muscle does not cause insulin resistance. Biochem Biophysi Resea Comm 2006; 350: 202– 207 [DOI] [PubMed] [Google Scholar]
- 26.Garvey WT, Maianu L, Zhu J-H, Brechtel-Hook G, Wallace P, Baron AD: Evidence for defects in the trafficking and translocation of GLUT4 glucose transporters in skeletal muscle as a cause of human insulin resistance. J Clin Invest 1998; 101: 2377– 2386 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ramirez-Zacarias JL, Castro-Munozledo F, Kuri-Harcuch W: Quantitation of adipose conversion and triglycerides by staining intracytoplasmic lipids with Oil red O. Histochemistry 1992; 97: 493– 497 [DOI] [PubMed] [Google Scholar]
- 28.Fu Y, Luo N, Klein RL, Garvey WT: Adiponectin promotes adipocyte differentiation, Insulin sensitivity, and lipid accumulation. J Lipid Res 2005; 46: 1369– 1379 [DOI] [PubMed] [Google Scholar]
- 29.Kim JY, van de Wall E, Laplante M, Azzara A, Trujillo ME, Hofmann SM, Schraw T, Durand JL, Li H, Li G, Jelicks LA, Mehler MF, Hui DY, Deshaies Y, Shulman GI, Schwartz GJ, Scherer PE: Obesity-associated improvements in metabolic profile through expansion of adipose tissue. J Clin Invest 2007; 117: 2621– 2637 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Otabe S, Yuan X, Fukutani T, Wada N, Hashinaga T, Nakayama H, Hirota N, Kojima M, Yamada K: Overexpression of human adiponectin in transgenic mice results in suppression of fat accumulation and prevention of premature death by high-calorie diet. Am J Physiol Endocrinol Metab 2007; 293: 210– 218 [DOI] [PubMed] [Google Scholar]
- 31.Ghanim H, Dhindsa S, Aljada A, Chaudhuri A, Viswanathan P, Dandona P: Low-dose rosiglitazone exerts an antiinflammatory effect with an increase in adiponectin independently of free fatty acid fall and insulin sensitization in obese type 2 diabetics. J Clin Endocrinol Metab 2006; 91: 3553– 3558 [DOI] [PubMed] [Google Scholar]
- 32.Ghanim H, Garg R, Aljada A, Mohanty P, Kumbkarni Y, Assian E, Hamouda W, Dandona P: Suppression of nuclear factor-B and stimulation of inhibitor B by troglitazone: evidence for an anti-inflammatory effect and a potential antiatherosclerotic effect in the obese. J Clin Endocrinol Metab 2001; 86: 1306– 1312 [DOI] [PubMed] [Google Scholar]