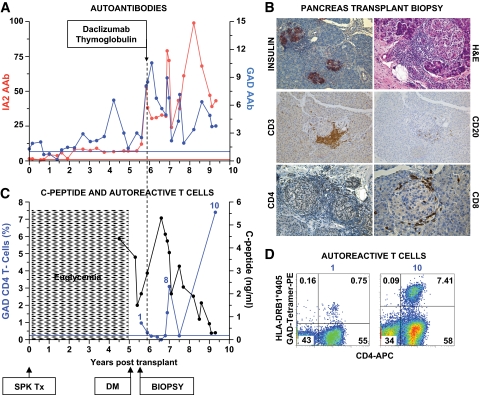
FIG. 1.
Clinical course, autoimmunity assessment, and biopsy in patient 1. Patient 1 was a 41-year-old Caucasian male [HLA A2/A3, B57/B60, DR4 (DRB1*0405)/DR6] who developed type 1 diabetes at age 7 years. He received an SPK transplant from an HLA A2/A30, B41/B60, DR4/DRX donor at age 32 years. The transplant reversed diabetes, but the patient returned to insulin dependence 5 years later, while kidney and exocrine pancreas allografts had normal function. A: Autoantibody levels before transplant and on follow-up. The patient had GAD and IA-2 autoantibodies before transplantation, which persisted despite immunosuppression, and titers increased on follow-up. Color-matched, horizontal lines represent the cutoff level for each autoantibody. For all autoantibodies, a value >1 denotes a positive result. B: Pancreas transplant biopsy stained as labeled, obtained ∼6 months after the recurrence of hyperglycemia. Insulitis and β-cell loss are shown. C: Serum C-peptide levels and % of GAD tetramer–positive T-cells in the CD4 T-cell population from the time of hyperglycemia recurrence. C-peptide was still detectable at diagnosis, confirming the function of residual β-cells observed at biopsy. Autoreactive T-cells were detected at the time of biopsy, ∼6 months after the recurrence of hyperglycemia on two samples, and again at several time points ∼1 year after treatment. The horizontal blue line represents the cutoff of the tetramer assay (0.25%). D: Flow cytometry plots demonstrating GAD-autoreactive CD4 T-cells. The numbers above the plots identify the same sample in C. Tetramer staining with irrelevant peptide was <0.1% (not shown). DM, diabetes; Tx, treatment. (A high-quality digital representation of this figure is available in the online issue.)