Abstract
Urinary tract obstruction results in obstructive nephropathy and uropathy. It is the most frequent cause of renal failure in infants and children. In the past two decades, studies in transgenic models and humans have greatly enhanced our understanding of the genetic factors and developmental processes important in urinary tract obstruction. The emerging picture is that development of the urinary tract requires precise integration of a variety of progenitor cell populations of different embryonic origins. Such integration is controlled by an intricate signaling network that undergoes dynamic changes as the embryo develops. Most congenital forms of urinary tract obstruction result from the disruption of diverse factors and genetic pathways involved in these processes, especially in the morphogenesis of the urinary conduit or the functional aspects of the pyeloureteral peristaltic machinery.
Keywords: Urinary tract obstruction, genetic mutation, development, obstructive nephropathy, obstructive uropathy
Introduction
Urinary tract obstruction (UTO) can lead to hydroureter, hydronephrosis, and even renal failure (1-3). It is a condition that concerns both nephrologists and urologists. In a strict sense, UTO describes the presence of a physical blockage to urine flow. However, the word “obstruction” is also used to describe the failure of urine transport from the kidney to the ureter in the absence of physical blockage. In this review, we use the word “obstruction” to describe both physical obstruction of the urinary tract as well as functional obstruction (4, 5). There have been many comprehensive reviews on the pathological outcomes and treatment options for obstructive nephropathy and uropathy (2, 6-10). This review focuses on the recent advances in understanding the genetic and developmental causes of UTO, especially the congenital and hereditary forms.
Diverse Causes for UTO
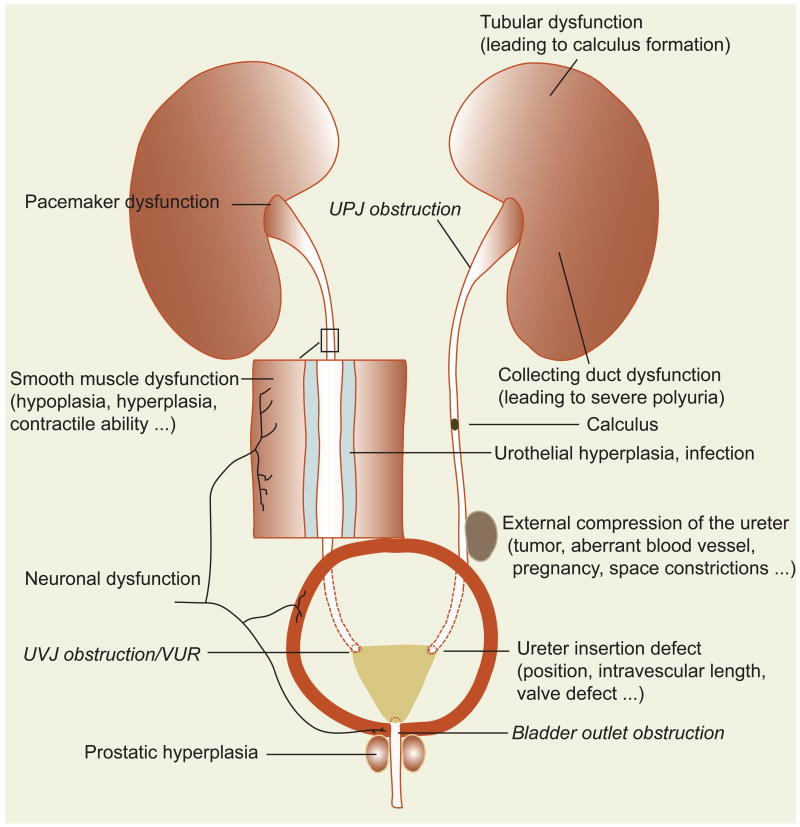
UTO is categorized by its location and/or cause (11) (Fig. 1). Obstruction at the junction between the ureter and the renal pelvis is called ureteropelvic junction (UPJ) obstruction presenting as hydronephrosis without obvious dilatation of the ureter. Urine blockage at the ureterovesical junction (UVJ) and the backflow of urine from the bladder to the ureter are described as UVJ obstruction and vesicoureteral reflux (VUR), respectively. Although VUR can occur along with other urinary tract anomalies, including anatomical obstruction of the urinary tract, UVR does not necessarily lead to upper urinary tract damage by itself. Interruption of urine flow from the bladder to the outside environment through the urethra is called bladder outlet obstruction. The presence of posterior urethral valves is the most common type of bladder outlet obstruction in male pediatric patients. Although not all of the terms described above directly describe the cause of the problem, the location of the urine flow interruption is taken into consideration in determining etiology. Obstruction can be caused by factors both within and outside the urinary system. Within the urinary system, developmental anomalies can result in anatomical blockage or stenosis of the urinary conduit, defective valves at UVJ, short intramural ureter, as well as fistulae between the ureter and surrounding structures. Since urine flow from the kidney to the bladder requires active pyeloureteral peristalsis, any developmental defects affecting the peristaltic machinery, including the pacemaker, the smooth muscle (SM), and the neuronal control, could potentially lead to functional obstruction. Hyperplasia of the urothelium and urinary tract infection (UTI) can block the ureteral lumen, causing obstruction. Renal dysfunction can also secondarily lead to urinary tract dysfunction and obstruction. For example, collecting duct defects can lead to severe polyuria that overwhelms the pyeloureteral peristaltic machinery, leading to functional obstruction. Renal tubular dysfunction can result in renal calculi and obstruction of the urine path. Factors outside the urinary system that can create spatial constraints for the urinary conduit can also lead to UTO. These include tumors, prostatic hypertrophy, aberrant vessel crossing, and pregnancy.
Figure 1. Causative factors for UTO.
UPJ, UVJ, and bladder outlet obstructions are in Italics as these terms describe the location but not the causes for the obstruction.
Besides the overt familial cases and transgenic models, strong genetic determinants were reported in UTO by a number of studies in seemingly sporadic cases (12-14). In one of these studies, Feather et al found a 30-50-fold increase in VUR incidence in first-degree relatives of probands with VUR, compared to the general population (13). Environmental factors can influence developmental defects in the urinary tract caused by genetic mutations, contributing to the variability of the urinary defects seen among patients or among animal models with the same genetic mutation.
Congenital UTO Originates from Anomalies in Metanephric Kidney Development
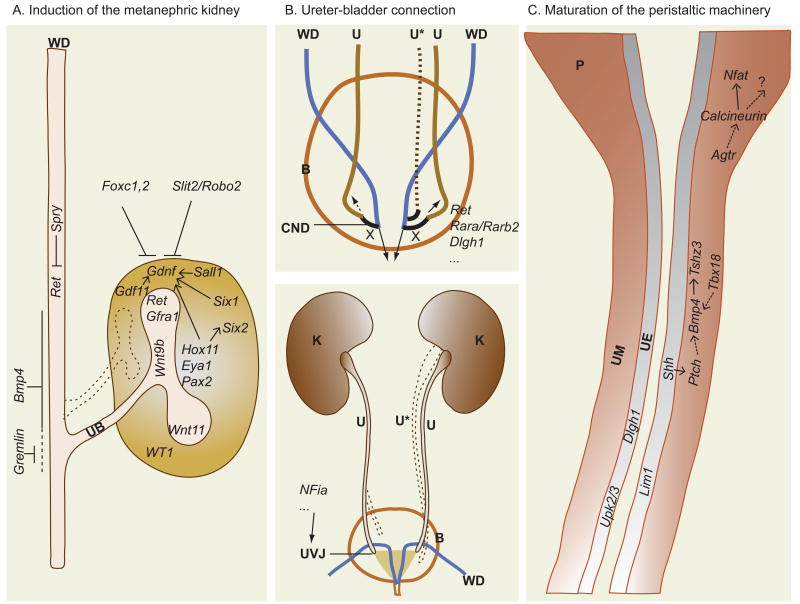
Congenital diseases originate from developmental errors and by definition, present at birth. In some cases, although the hallmarks of UTO, hydroureter and hydronephrosis may emerge at later postnatal stages, the cellular lesions and anatomical changes required for disease progression are already present at birth. In addition, hydronephrosis and hydroureter are frequently associated with a range of other kidney and urinary tract anomalies, including but not limited to, renal agenesis, renal hypoplasia, supernumerary ureters, ectopic ureters, horseshoe kidneys, pelvic kidneys, and others. Some of these defects directly cause UTO, while others reflect the commonality of defective critical developmental processes responsible for these defects. Although developmental errors in many areas may lead to UTO, three processes stand out as the most likely sources of such errors. These include the induction of the metanephric kidney, the establishment of the urinary conduit, and the maturation of the pyeloureteral peristaltic machinery (Fig. 2).
Figure 2. Key developmental steps in which errors frequently lead to UTO.
A, Metanephric kidney Induction. WD: Wolffian duct. UB: Ureteric bud. B, Ureter-bladder connection. K: Kidney. U: Ureter; U*: Eectopic/supernumerary ureter (dotted lines); CND: Common nephric duct. B: Bladder. X: indicates that the CND undergoes apoptosis so that the ureter separates completely from the WD. The dotted arrow in the top panel indicates abnormal migration/positioning of the ureter that can result in abnormal insertion of the ureter into the bladder. In the bottom panel, the dotted lines connected to the right ureter depict the abnormal positioning of the ureter when the ureter insertion process is affected. The dotted lines on the left side depict the ectopic supernumerary ureter. Both diagrams in B represent the ventral views of the urinary system. C, Maturation of the pyeloureteral peristaltic machinery. P: Pelvis, UM: Ureteric mesenchyme; UE: Ureteric epithelium. Dotted arrows indicate potential regulation.
Metanephric Kidney Induction
Metanephric kidney induction occurs in the narrow strip of intermediate mesoderm (IM). In mammals, a pair of Wolffian ducts (WD, also known as mesonephric duct), connect the mesonephri (the transient embryonic kidney) to the urogenital sinus and serve as the anlage for the ureters and male reproductive ducts. During mid-gestation (at about E10.5 in mice, 28 days for human fetus), the ureteric bud (UB) emerges from the WD and invades the metanephric mesenchyme (MM) within the IM to initiate the development of the metanephric kidney (the definitive kidney). The reciprocal interactions between the UB and the MM drive the branching of the UB within the MM and the mesenchymal-epithelial transformation of the MM to form various nephron components. Anomalies in metanephric kidney induction may result in renal hypoplasia, renal agenesis, ectopic and supernumerary ureters, and a range of other defects. Some of these defects, especially ectopic ureter and supernumerary ureters, set the stage for UTO to occur. Since kidney induction was covered by a number of recent reviews, only aspects related to later UTO will be discussed in more details here.
Glial-derived neurotrophic factor (GDNF) is one of the most important factors expressed in the MM. GDNF, along with GDNF-family receptor α1 (GFRα1), activates the tyrosine kinase receptor RET (expressed in the WD) to promote the localized UB outgrowth. Null mutations in Gdnf, Ret, or Gfrα1 result in renal agenesis or severe dysplasia due to failure of UB outgrowth. The domain of Gdnf expression is tightly controlled to ensure that only one ureter will emerge from the WD at the correct position. A number of genes, including Sal-like gene 1 (Sall1), Sine oculis homeobox homolog 1 (Six1), Eyes-absent homolog 1 (Eya1), Paired-box 2 (Pax2), Growth and differentiation factor 11 (Gdf11), Hox11 genes, and others, directly or indirectly regulate the expression of Gdnf to ensure normal UB induction (15-22). Forkhead box protein c1/c2 (Foxc1/c2) and Slit homolog 2 (Slit2)/Roundabout homolog 2 (Robo2), however, suppress the expression of Gdnf in the region anterior to the MM. Disruption of these genes leads to the anterior expansion of the Gdnf expression domain and the formation of supernumerary and ectopic ureters (15, 16, 23, 24) (Fig. 2A). Both in vitro treatment of the cultured WD by GDNF or the transgenic expression of Gdnf in the WD can result in multiple ureters (25). However, renal agenesis in Gdnf-/- mice can be largely rescued by transgenic expression of Gdnf throughout WD (with no positional information for UB budding). This and other findings suggest the existence of redundant inductive signals for the localized induction of UB (25, 26). In particular, the Fibroblast growth factor (Fgf) signaling appears to have functions in both the UB and the MM during kidney induction and later development (27). Interruption of Fgf signaling in these embryonic structures can lead to a range of urinary tract anomalies, including UTO (28).
RET signaling in WD and UB appears to have a number of downstream pathways affecting metanephric development in different ways (29). While the null mutations and a mutation targeting a tyrosine linked to MAPK activation generally lead to renal agenesis, mutations targeting other tyrosine phosphorylation sites cause a range of congenital anomalies of the kidneys and the lower urinary tract, including supernumerary ureters, hydroureter, and hydronephrosis (29, 30). Furthermore, the tyrosine kinase inhibitor Sprouty 1 (SPRY1) suppresses RET activation in the WD, and is also important for ensuring the correct number and position of UB outgrowth (31, 32). Loss of Spry1 function leads to the development of supernumerary and obstructed ureters (31). Bone morphogenetic protein 4 (Bmp4) is expressed in the mesenchyme surrounding the WD and negatively regulates UB budding. Gremlin 1 (GREM1), an inhibitor of BMP signaling, is produced by MM to counter the BMP4 suppression and to promote UB budding. Therefore, inactivating mutations of Bmp4 and over-activation of Grem1 can both lead to the formation of supernumerary ureters that are frequently obstructed (33-35) (Fig. 2A).
Disruption of UB initiation and MM survival generally leads to renal agenesis, while anomalies in UB position and number create abnormal connections between the ureter and the bladder, leading to UTO (discussed in the next section). Different mutations of the same gene or even the exact same mutation can lead to different phenotypic and clinical presentations (even on two sides of the same individuals), underlying the intricate connection of these processes (36-38). The concurrence of renal agenesis/dysplasia and UTO in the same individuals and the variability of the disease presentation may seem enigmatic at first. Better understanding of the metanephric kidney development has provided more reasonable explanations for such phenomena. In a hypothetical example, a mutation affecting the timing and positioning of UB budding, may slow UB budding to a level that UB barely reaches the MM in time to prevent its apoptosis. Mispositioning of the UB then leads to ectopy and UTO. However, any additional factors, including intrinsic variations or random extrinsic disturbances, may delay the UB further, causing the failure of the UB to reach MM before its degeneration and leading to renal agenesis. Thus a quantitative difference (slower UB outgrowth, for example) may be translated into qualitative outcomes, leading to concurrence of seemingly distinct defects (renal agenesis or UTO) in affected individuals.
Establishment of the Urinary Conduit
Although defective kidney induction is the primary cause in many cases of congenital UTO, later remodeling of the lower urinary tract, especially the connection of the ureter to the bladder, also plays an important role in ensuring the proper layout of the urinary conduit system (36, 39-42). As development proceeds, the UB becomes the ureteric epithelium and the collecting duct system in the kidney (15, 16). The bladder, on the other hand, develops independently from the urogenital sinus of an endodermal origin. These two organs have to join precisely for completion of the urinary path. The complexity of this joining process and the demanding anti-reflux requirement near the junction are likely the reasons for the high incidence of VUR and UVJ obstruction.
The process of establishing the ureter-bladder connection has been redefined in unprecedented clarity and detail in a series of recent studies (36, 39, 41). These studies showed that the maturation of the ureter is a multi-step process. After emerging from the WD, the UB/ureter moves caudally along the common nephric duct (CND) toward the urogenital sinus (the future bladder). This is followed by lateral movement of the ureter toward its final insertion site away from the WD. Apoptosis of the CND eventually severs the link between the ureter and the WD (Fig. 2B). It appears that Ret has an additional site of action in the trigonal wedge area for the normal migration of the ureter. Ret expression in this area is itself regulated by Vitamin A through the RARA/RARB2 receptors. CND apoptosis is also dependent on Vitamin A. Disruption in Ret, Retinoic acid receptor alpha (Rara)/ Retinoic acid receptor beta 2 (Rarb2), and Aldehyde dehydrogenase 1 family, member A2 (Aldh1a2) (encodes an enzyme in retinoic acid synthesis) can lead to abnormal connection of the ureter to the bladder and UTO (36, 39). In some of these mice, the ureter connects to the reproductive tract as the normal separation of the ureter orifice from the WD is disrupted. A couple of studies have shown that the inactivation of Discs large homolog 1 (Dlgh1) causes hydronephrosis and hydroureter during embryonic development (43, 44). The study by Iizuka-Kogo et al found that the ureteral orifice of some of these mutants failed to migrate down the CND to reach the bladder and others have abnormally formed connections to the bladder, causing UTO in both cases (44). Additional functions of Dlgh1 in the differentiation and organization of the ureteral SM cells (SMCs) was indicated in another study by Mahoney et al and will be discussed in the next section on the maturation of the peristaltic machinery (43). Even a delayed separation of the ureter from the WD, as found in the Pax21Neu/+ mice (45), may cause reversible VUR, providing one possible explanation for pediatric VUR that resolves overtime. The intravesical section of the ureter is usually compressed by the surrounding bladder muscle. It appears that the intravesical ureter length can be affected by genetic mutations and is inversely correlated to the risk of reflux (46). In addition, inactivation of Nuclear factor I/A (NFIa) causes both UVJ and UPJ anomalies in murine models and humans, revealing the importance of this gene in the correct formation of these important junctions (47).
The trigone is a triangular muscular structure on the bladder floor important for the anti-reflux mechanism. It is believed to be critical in the control of the ureter position and the proper function of the ureteral valves. Traditional models described the origin of the trigone as the expansion of the CND. Recent findings, however, indicate that the trigone is not derived from the CND that undergoes apoptosis (39). Instead, the trigone develops from the intercalation of the bladder and the ureter SMCs with the bladder SMCs being the vast majority (41). The detailed mechanism of ureteral valve formation is still unclear. However, it appears that a transient membrane structure (Chwalla's membrane) seals the distal end of the ureter (48). It ruptures to allow urine flow after the ureter is properly inserted into the bladder. Although there is no evidence that the Chwalla's membrane contributes to the valves, its normal rupture and the development of the valves are likely temporally and spatially coordinated. Delayed rupture of the Chwalla's membrane could lead to UTO.
Maturation of the Pyeloureteral Peristaltic Machinery
The correct layout of the urinary conduit does not by itself guarantee uninterrupted urine flow. Urine transfer from the kidney to the bladder is an active process requiring well coordinated pyeloureteral peristalsis. Unidirectional peristalsis is believed to be initiated by the pacemaker cells. Although not very much is known about these cells, evidence suggests that they are likely specialized SMCs in the renal pelvis (49). The peristalsis itself is powered by the SMCs in the pelvis and ureter. SM defects have been frequently associated with UTO and the development of the ureteral SM will be discussed in more details below. Among other factors that may regulate peristalsis is neuronal control. The ureteral wall is highly innervated. Although neurological dysfunction can cause neurogenic bladder that loses the proper control of the expulsion of the stored urine from the bladder to the external environment through the urethra, the role of neuronal control of pyeloureteral peristalsis is less clear. Spontaneous peristalsis in the isolated or denervated pyeloureteral complexes retains characteristics similar to those observed in vivo and is not blocked by tetrodotoxin or other neuronal blockers (49, 50). In renal transplantation, donor kidney and ureter are surgically ligated to the recipient bladder. Effective peristalsis occurs shortly after surgery with no evidence of immediate reinnervation. These observations suggest that ureteral motility is largely a myogenic process, though the innervating nerves may have a modulatory role (49, 50).
While the ureteral epithelium is derived from the UB, the associated mesenchyme originates from the tailbud mesenchyme (40). The subdivision of the UB into the intra-renal colleting duct system and the ureter with its associated SM creates another junction within the urinary system where progenitors of distinct embryonic origins have to precisely integrate to form a functional structure. The complexity involved in such integration, similar in this regard to the situation at the UVJ, may increase the probability for errors to occur, leading to the high incidence of UPJ obstructions in humans and animal models. Bmp4, expressed in the tailbud mesenchyme, is essential for these cells to participate in the formation of the ureteral SM. Spatially restricted Bmp4 expression determines the site where UB is divided into the collecting duct system and the ureter (40). Thus, Bmp4 has an important role in regulating UB budding and in ureteric mesenchyme differentiation, both directly relevant to UTO when errors occur. T-box transcription factor 18 (Tbx18) is specifically expressed in the ureteric mesenchyme. Inactivation of Tbx18 leads to the loss of Bmp4 expression in the ureteral mesenchyme and defective differentiation of the mesenchymal cells into functional SMCs (42). If Bmp4 is indeed controlled by Tbx18, Tbx18 may be the key factor in the division of the UB into the collecting duct system and the ureter along the anterior and posterior axis (51).
Development of the ureteral mesenchyme is also regulated by the ureteral epithelium. Inactivation of Sonic hedgehog (Shh) in the urothelium leads to defective ureteral mesenchyme differentiation and hydroureter (52). Bmp4 expression is lost in these mutants, suggesting that Shh in the urothelium is required to sustain Bmp4 expression in the ureteral mesenchyme, presumably through the Shh receptor Ptch that is expressed in the periureteral mesenchyme. The transcription factor Teashirt zinc finger family member 3 (Tshz3) is expressed in the ureteric mesenchyme and its inactivation results in defective ureteral SM differentiation and hydronephrosis (53). Shh and Bmp4 expression appear normal in these mutants, suggesting that Tshz3 may function downstream of these factors for the regulation of SM differentiation. Dlgh1 is expressed more strongly in the epithelium than in the mesenchyme. Its inactivation results in a range of urogenital defects, including defective ureteral insertion into the bladder as discussed in the previous section (43, 44). In addition, Mahoney et al described the absence of a stromal cell layer between the urothelium and the SM as well as the misalignment of the muscle layers that affects peristalsis (43).
The Renin-Angiotensin system (RAS) is known to be involved in renal injury as a result of UTO. RAS, however, has a constructive role during urinary tract development (54, 55). Mutations in a number of RAS component genes cause congenital anomalies of the kidney and urinary tract (CAKUT), including UTO. Inactivation of Angiotensin II receptor, type 2 (Agtr2) results in CAKUT with partial penetrance (56, 57). Loss of Angiotensin II receptor, type 1a/b (Agtr1a/b) also results in pathological changes in the kidney resembling obstructive nephropathy (58, 59). Similar findings were reported in the study of mutant alleles of the other RAS components Angiotensin converting enzyme (Ace) (60) and Angiotensinogen (Agt) (61, 62). Although the broad effect of RAS in blood pressure control and regulation of the ability to concentrate urine may contribute to the observed renal pathological changes, evidence suggests that direct function of RAS in the ureteral SM differentiation plays an important role (58). Calcineurin, a calcium-dependent serine/threonine phosphatase, dephosphorylates the cytoplasmic Nuclear Factor of Activated T-cells (Nfat) transcription factors (among a number of its known substrates) and sends them into the nucleus to activate the transcription of the downstream genes. In our previous study, inactivation of Calcineurin in the metanephric and ureteric mesenchyme leads to the underdevelopment of the urinary tract SMs and results in dysfunction of the pyeloureteral peristaltic machinery (4). Our recent studies indicate that transgenic activation of Nfatc1 in the urinary tract also leads to severe developmental anomalies including hydroureters and hydronephrosis (Wang and Chen, unpublished results), emphasizing the importance of the Calcineurin-Nfat pathway in the regulation of the normal development of the urinary system. A number of studies suggest that RAS can induce activation of Calcineurin. It is likely that within the urinary system, RAS activates Calcineurin to induce Nfat-mediated transcription for proper urinary tract development and differentiation.
Other Developmental Defects Causing UTO
Besides the processes described above, UTO can also be caused by a variety of developmental anomalies. Inactivation of either Uroplakin II (UpkII) or Uroplakin III (UpkIII) causes defective plaque formation and hyperplasia of the urothelium (63, 64). These mutants have UTO possibly caused by urothelial hyperplasia blocking the urinary path, a situation similar to the dioxin-induced hydronephrosis (65). Interestingly, autoimmune antibodies against UpkIII and hydronephrosis were found in mice doubly homozygous for mutations in the following two genes: Fc receptor, IgG, low affinity IIb (Fcgr2b) and Programmed cell death 1 (Pdcd1) (66). Hydronephrosis was also observed in >50% of mice overexpressing Interleukin 9 (IL-9) (67). Autoimmune antibodies were again found in these mice, though the specificity of these antibodies was not well characterized. Linkage to human leukocyte antigen system (HLA) was reported in humans with UTO (68, 69). Whether autoimmunity plays a role in these patients is not known.
Besides factors that directly affect the cells and tissues in the urinary conduit, renal dysfunction can also cause UTO. Poorly controlled polyuria can lead to hydronephrosis in humans. This is also exemplified in the classical cph (Congenital progressive hydronephrosis) mutant mice. These mice have a single amino acid substitution in the water channel protein Aquaporin 2 (AQP2) that prevents its normal trafficking to the apical membrane for water absorption. The resulting polyuria overwhelms the pyeloureteral peristaltic machinery and leads to progressive hydronephrosis (70). Hydronephrosis is a common prenatal diagnosis that frequently resolves spontaneously (2). Since urine output is highly variable and influenced by multiple factors, it is conceivable that temporary polyuria may contribute to some of these spontaneously resolved hydronephrosis cases. Another example of renal dysfunction causing UTO is the Solute carrier family 7 member 9 (Slc7a9)-/- mice that have cystine urolithiasis, causing obstruction by blocking the ureteral lumen (71).
Summary
It is becoming clear that UTO can result from a wide variety of environmental causes or genetic mutations. Even the subtypes of UTO (such as UPJ obstruction, UVJ obstruction, etc) are heterogeneous and may have drastically different etiology. Kidney and urinary tract diseases frequently have ambiguous pathological presentations and require an understanding of the primary molecular and cellular defects to uncover the true nature of the condition. Although great progress has been made in understanding the genetic and developmental basis of UTO, to pinpoint the etiology in a given patient remains a great challenge. Further investigation is necessary to translate the knowledge gained in these studies into improvements in diagnosis and treatment.
Table 1. Genetic mutations causing congenital UTO.
The gene names follow the terminology in the original reference. Newer names are listed in the second column. The known or predicted function of the gene product is given in the brackets, if the full name does not already have a clear indication. In the genotypes, “T” stands for the transgene; “+” stands for a wild-type allele, “-” stands for a loss-of-function allele (presumed null); “flox” stands for the floxed allele; “lz” stands for the LacZ knock-in allele (usually a null allele for the endogenous gene). SM: Smooth muscle. SMC: Smooth muscle cell. UB: Ureteric bud. MM: Metanephric mesenchyme. VUR: Vesicoureteral reflux. UTO: Urinary tract obstruction. This is intended to be a representative list, instead of a complete list, both for animal models and for humans. This is especially true for cases with UTO as a minor component of a syndrome.
| Genes/Mutations | New gene names, Gene full names, & [Function] | Alleles and the corresponding urinary defects | Proposed or likely Mechanism | Ref |
|---|---|---|---|---|
| Ace | Angiotensin converting enzyme | Ace-/- mice: hydronephrosis, renal parenchymal atrophy. | Defective pyeloureteral peristalsis as a result of a ureter differentiation defect, a urine concentration defect/polyuria, or both. | (60) |
| Adamts-1 | A disintegrin-like &metallopeptidase with thrombospondin type 1 motif, 1 | Adamts-1-/- mice: UPJ obstruction, hydronephrosis, hydroureter, other urogenital defects. | Unclear. Excessive collagen deposit was found at UPJ. | (72) |
| Agt | Angiotensinogen | Agt-/- mice: hydronephrosis, renal parenchymal atrophy. | Defective pyeloureteral peristalsis. | (61, 62) |
| Agtr1a/b | Angiotensin II receptor, type 1 (1a & 1b) | Agtr1-/- (1a & 1b) mice: partial penetrance, hydronephrosis in older mutants, renal parenchymal atrophy. | Urinary SMC developmental Defect, renal pelvis development. | (58, 59) |
| Agtr2 | Angiotensin II receptor, type 2 | Agtr2-/- mice: limited incidence of hydronephrosis, megaureter, renal parenchymal atrophy. | Ectopic and duplicated UB. | (56, 57) |
| Aldh1a2 | Aldehyde dehydrogenase family 1 member A2 [encodes Raldh2, an enzyme in retinoic acid synthesis] | Aldh1a2-/- mice rescued by maternal retinoic acid: hydroureter & hydronephrosis | Defects in ureter maturation, especially the insertion of the ureter into the bladder. | (39) |
| Aqp2 | Aquaporin 2 [Water channel] | The cph mutants (Aqp2S256L/S256L) have polyuria and hydronephrosis. Other Aqp2 mutations also cause renal damage resembling obstructive nephropathy. | Polyuria overwhelms the pyeloureteral peristaltic machinery. | (70,73,74) |
| β-catenin | Same as Ctnnb1 [adherens junction protein, involved in Wnt signaling] | Hoxb7-CreT/+; β-catenin flox/flox mice: hydroureter & hydronephrosis. | Ectopic and supernumerary UB. | (37) |
| Bmp4 | Bone morphogenetic protein 4 | Bmp4+/- mice: hydronephrosis, hydroureter, other urinary tract defects. | Ectopic and supernumerary UB. | (33, 34) |
| Bmp5 | Bone morphogenetic protein 5 | short ear (Bmp5-/-) mice: Hydroureter & hydronephrosis. | Spatial constraints in the lower abdominal cavity affect urinary transfer. | (75, 76) |
| Calcineurin | Same as Ppp3c, protein phosphatase 3. [serine/threonine Protein phosphatase] | The Pax3-CreT/+; Cnb1flox/flox mice (with Calcineurin inactivation in the metanephric and ureteral mesenchyme): early postnatal hydronephrosis & hydroureter. | Pyeloureteral peristaltic defect, defect in urinary tract SMC development. | (4) |
| Dlgh1 | Same as Dlg1, Disk-large homolog 1 [scaffolding protein] | Dlgh1-/- mice: prenatal hydronephrosis, short ureter, and defects in the ureteral insertion into the bladder. | SM differentiation defect, ectopic UB. | (43, 44) |
| Fcgr2b & Pdcd1 | Fc receptor, IgG, low affinity IIb & Programmed cell death 1 [cell surface membrane protein of the immunoglobulin superfamily] | Some Fcgr2b-/-;Pdcd1-/- mice: hydronephrosis. | Autoimmune against UPKIIIa. | (66) |
| Fgfr2 | Fibroblast growth factor receptor 2 | Some Pax3-CreT/+; Fgfr2flox/flox mice have hydroureter. | Supernumerary UB, abnormal ureter connection | (28) |
| Foxc1/c2 | Forkhead box protein C1/C2 [transcription factor] | Foxc1-/- & Foxc1+/-,Foxc2+/- mice: duplex kidney, ureter duplication, hydroureter, hydronephrosis. | Ectopic and supernumerary UB. | (77) |
| Gata2 | GATA binding protein 2 [transcription factor] | Gata2-/- mice (with YAC rescue of hematopoietic defects): hydroureter, hydronephrosis. | Unclear. | (78) |
| Hoxa13 & Hoxd13 | Homeobox A13 and D13 [transcription factor] | Hoxa13+/-; Hoxd13-/- mice: UVJ obstruction, hydronephrosis, hydroureter, other urogenital defects. | Patterning defects. May have homeotic transformation. | (79) |
| Hspa4l | Heat shock protein 4 like [chaperone?] | Some Hspa4l-/- mice have genetic background-dependent hydronephrosis. | Unclear. | (80) |
| Id2 | Inhibitor of DNA binding 2 | Id2-/- and Id2+/- mice have hydronephrosis. | UPJ development. | (81) |
| Il-9 | Interleukin 9 | Overexpressing Il-9 by its own promoter in mice: hydronephrosis | Likely autoanitibodies against urinary tract components. | (67) |
| L1cam | L1 cell adhesion molecule | L1cam-/- mice: hydroureter & hydronephrosis. | Ectopic UB. | (82) |
| Lim1 | Same as Lhx1 – Lim homeobox protein 1 [transcription factor] | Hoxb7-CreT/+; Lim1lz/flox mice (with Lim1 deletion in the UB derivatives): hydroureter & hydronephrosis. | Ureter differentiation. | |
| Limp-2 (Lgp85) | Same as Scarb2 [scavenger receptor] | Limp-2-/- mice: kidney and ureter duplication, UPJ obstruction, hydroureter, and hydronephrosis. | Ectopic and supernumerary UB. | (83) |
| Lx (luxate) | Unknown | Some Lx+/- and -/- mice: hydroureter, hydronephrosis, horseshoe kidney. | Crossing vessels suspected (84). New results point to early metanephric patterning defects (Unpublished results from our laboratory). | (84) |
| Megabladder | Unknown | Mutants have hydronephrosis, hydronephrosis, megabladder | Bladder SM development. | (85) |
| Nfia | Nuclear factor I/A [transcription factor] | Nfia+/- and Nfia-/- mice: VUR, hydronephrosis & hydroureter. Human NFIA+/- patients have similar defects. | Abnormal development of the UPJ and UVJ. | (47) |
| Nkcc2 | Same as Slc12a1-solute carrier family 12, member 1 [Sodium-potassium-chloride cotransporter] | Nkcc2-/- mice: polyuria and hydronephrosis of varying severity. | Possibly by polyuria overwhelming the pyeloureteral peristaltic machinery. | (86) |
| Pax2 | Paired box gene 2 [transcription factor] | Pax21Neu/+ mice: VUR. Other human and mouse mutant alleles also cause VUR in addition to renal agenesis. | Delay in urinary tract maturation in the Pax21Neu/+ mice. | (45) |
| Rara/Rarb2 | Retinoic acid receptor, alpha/retinoic acid receptor beta 2 | Rara-/-;Rarb2-/- mice have hydronephrosis, hydroureter, VUR. | Defective differentiation of the MM. | (63) |
| Renin | Same as Ren1 [an enzyme in the rennin-angiotension system] | Renin-/- mice: hydronephrosis, renal parenchymal atrophy. | Possibly by polyuria. It is also possible that the mutation disrupts SM differentiation. | (87) |
| Ret | Ret proto-oncogene [Gdnf receptor] | Ret-/- mice: renal agenesis, hydronephrosis, hydroureter, VUR. | UB initiation defect, ureter maturation defect. | (36, 88, 89) |
| Mice carrying Ret alleles with specific mutation of the keytyrosines: CAKUT. | Ectopic and supernumerary UB. | (29) | ||
| Mice overexpressing Ret in UB: VUR. | Ureter maturation defect. | (90) | ||
| Robo2 | Roundabout homolog 2 [SLIT2 receptor] | Robo2-/- mice and human patients carrying ROBO2 mutations/variants have VUR. | Ectopic and supernumerary UB. | (24, 91, 92) |
| Romk | Same as Kcnj1, potassium inwardly-rectifying channel, subfamily J, member 1 | Romk-/- mice: hydronephrosis, water and electrolyte balance problem. | Unclear. | (93) |
| Shh | Sonic hedgehog [secreted signaling molecule] | Hoxb7-CreT/+; Shhflox/flox mice (Shh-/- in UB derivatives): hydroureter & hydronephrosis. | Mesenchymal proliferation, SMC differentiation. | (52) |
| Slc7a9 | Solute carrier family 7 member 9 [cationic amino acid transporter] | Slc7a9-/- mice: cystine urolithiasis and hydroureter. | Urolithiasis blocks urine flow. Not strictly “congenital”. | (71) |
| Slit2 | Slit homolog 2 [ROBO2 ligand] | Slit2-/- mice: hydroureter and hydronephrosis. | Ectopic and supernumerary UB. | (24) |
| Smad4 | MAD homolog 4 [Tgfβ signal transducer] | Bmp7-CreT/+; Smad4flox/flox mice: hydronephrosis, | Defective MM differentiation. | (94) |
| Spry1 | Sprouty homolog 1 [RTK/ERK antagonist] | Spry1-/- mice: hydroureter and hydronephrosis. | Ectopic and supernumerary UB. | (31) |
| Spry2 | Sprouty homolog 2 [RTK/ERK antagonist] | Spry2-/- mice: renal agenesis, Hydroureter and hydronephrosis. | Ectopic and supernumerary UB. | (95) |
| Tbx18 | T-box transcription factor 18 | Tbx18-/- mice: hydronephrosis, hydroureter, and short ureters. | Ureteral SM defects due to ureteric mesenchyme differentiation anomalies. | (42) |
| Tensin | Same as Tns1 [actin-binding protein] | Tensin-/- mice: cystic and hydronephrotic kidney at a few months of age. | Unclear, cell-cell, cell matrix interaction? | (96) |
| Tshz3 | Teashirt zinc finger family member 3 [transcription factor] | Tshz3-/- mice: hydronephrosis and hydronephrosis. | Defects in ureteral SM differentiation. | (53) |
| UpkII | Uroplakin II [Glycolsylated Transmembrane protein] | UpkII-/- mice: hydronephrosis, hydroureter, VUR. | Urothelial hyperplasia may block the urinary path. Alternatively, the urothelium defects may affect SM development. | (63) |
| UpkIII | Uroplakin III [Glycolsylated Transmembrane protein] | UpkIII-/- mice: hydronephrosis, hydroureter, VUR. | Urothelial hyperplasia may block the urinary path. Alternatively, the urothelium defects may affect SM development. | (64) |
Acknowledgments
The author wishes to thank Drs. Helen Liapis and Matthew Coussens for critical reading of the manuscript. F.C. has been supported in part by a NIH grant (DK067386) and the George M. O'Brien Washington University Center for Kidney Disease Research (NIHP30DK079333).
References
- 1.Chevalier RL, Peters CA. Congenital urinary tract obstruction. Proceedings of the State-Of-The-Art Strategic Planning Workshop-National Institutes of Health; Bethesda, Maryland, USA. 11-12 March 2002; 2003. [DOI] [PubMed] [Google Scholar]; Pediatr Nephrol. 18:576–606. doi: 10.1007/s00467-003-1074-8. [DOI] [PubMed] [Google Scholar]
- 2.Chevalier RL. Molecular and cellular pathophysiology of obstructive nephropathy. Pediatr Nephrol. 1999;13:612–619. doi: 10.1007/s004670050756. [DOI] [PubMed] [Google Scholar]
- 3.Chevalier RL. Pathophysiology of obstructive nephropathy in the newborn. Semin Nephrol. 1998;18:585–593. [PubMed] [Google Scholar]
- 4.Chang CP, McDill BW, Neilson JR, Joist HE, Epstein JA, Crabtree GR, Chen F. Calcineurin is required in urinary tract mesenchyme for the development of the pyeloureteral peristaltic machinery. J Clin Invest. 2004;113:1051–1058. doi: 10.1172/JCI20049. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mendelsohn C. Functional obstruction: the renal pelvis rules. J Clin Invest. 2004;113:957–959. doi: 10.1172/JCI21402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bascands JL, Schanstra JP. Obstructive nephropathy: insights from genetically engineered animals. Kidney Int. 2005;68:925–937. doi: 10.1111/j.1523-1755.2005.00486.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Chevalier RL. Promise for gene therapy in obstructive nephropathy. Kidney Int. 2004;66:1709–1710. doi: 10.1111/j.1523-1755.2004.00984.x. [DOI] [PubMed] [Google Scholar]
- 8.Peters CA. Congenital obstructive nephropathy: is the fog lifting? Kidney Int. 2005;67:371–372. doi: 10.1111/j.1523-1755.2005.00124.x. [DOI] [PubMed] [Google Scholar]
- 9.Liapis H. Biology of congenital obstructive nephropathy. Nephron Exp Nephrol. 2003;93:e87–91. doi: 10.1159/000069554. [DOI] [PubMed] [Google Scholar]
- 10.Klahr S, Morrissey J. Obstructive nephropathy and renal fibrosis. Am J Physiol Renal Physiol. 2002;283:F861–875. doi: 10.1152/ajprenal.00362.2001. [DOI] [PubMed] [Google Scholar]
- 11.Chevalier RL. Obstructive uropathy: state of the art. Pediatr Med Chir. 2002;24:95–97. [PubMed] [Google Scholar]
- 12.Kenda RB, Kenig T, Budihna N. Detecting vesico-ureteral reflux in asymptomatic siblings of children with reflux by direct radionuclide cystography. Eur J Pediatr. 1991;150:735–737. doi: 10.1007/BF01958768. [DOI] [PubMed] [Google Scholar]
- 13.Feather SA, Malcolm S, Woolf AS, Wright V, Blaydon D, Reid CJ, Flinter FA, Proesmans W, Devriendt K, Carter J, et al. Primary, nonsyndromic vesicoureteric reflux and its nephropathy is genetically heterogeneous, with a locus on chromosome 1. Am J Hum Genet. 2000;66:1420–1425. doi: 10.1086/302864. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Queisser-Luft A, Stolz G, Wiesel A, Schlaefer K, Spranger J. Malformations in newborn: results based on 30,940 infants and fetuses from the Mainz congenital birth defect monitoring system (1990-1998) Arch Gynecol Obstet. 2002;266:163–167. doi: 10.1007/s00404-001-0265-4. [DOI] [PubMed] [Google Scholar]
- 15.Schedl A. Renal abnormalities and their developmental origin. Nature Reviews genetics. 2007;8:791–802. doi: 10.1038/nrg2205. [DOI] [PubMed] [Google Scholar]
- 16.Dressler GR. The cellular basis of kidney development. Annu Rev Cell Dev Biol. 2006;22:509–529. doi: 10.1146/annurev.cellbio.22.010305.104340. [DOI] [PubMed] [Google Scholar]
- 17.Kreidberg JA, Sariola H, Loring JM, Maeda M, Pelletier J, Housman D, Jaenisch R. WT-1 is required for early kidney development. Cell. 1993;74:679–691. doi: 10.1016/0092-8674(93)90515-r. [DOI] [PubMed] [Google Scholar]
- 18.Xu PX, Adams J, Peters H, Brown MC, Heaney S, Maas R. Eya1-deficient mice lack ears and kidneys and show abnormal apoptosis of organ primordia. Nat Genet. 1999;23:113–117. doi: 10.1038/12722. [DOI] [PubMed] [Google Scholar]
- 19.Wellik DM, Hawkes PJ, Capecchi MR. Hox11 paralogous genes are essential for metanephric kidney induction. Genes Dev. 2002;16:1423–1432. doi: 10.1101/gad.993302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu PX, Zheng W, Huang L, Maire P, Laclef C, Silvius D. Six1 is required for the early organogenesis of mammalian kidney. Development. 2003;130:3085–3094. doi: 10.1242/dev.00536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nishinakamura R, Matsumoto Y, Nakao K, Nakamura K, Sato A, Copeland NG, Gilbert DJ, Jenkins NA, Scully S, Lacey DL, et al. Murine homolog of SALL1 is essential for ureteric bud invasion in kidney development. Development. 2001;128:3105–3115. doi: 10.1242/dev.128.16.3105. [DOI] [PubMed] [Google Scholar]
- 22.Sajithlal G, Zou D, Silvius D, Xu PX. Eya 1 acts as a critical regulator for specifying the metanephric mesenchyme. Dev Biol. 2005;284:323–336. doi: 10.1016/j.ydbio.2005.05.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wilm B, James RG, Schultheiss TM, Hogan BL. The forkhead genes, Foxc1 and Foxc2, regulate paraxial versus intermediate mesoderm cell fate. Dev Biol. 2004;271:176–189. doi: 10.1016/j.ydbio.2004.03.034. [DOI] [PubMed] [Google Scholar]
- 24.Grieshammer U, Le M, Plump AS, Wang F, Tessier-Lavigne M, Martin GR. SLIT2-mediated ROBO2 signaling restricts kidney induction to a single site. Dev Cell. 2004;6:709–717. doi: 10.1016/s1534-5807(04)00108-x. [DOI] [PubMed] [Google Scholar]
- 25.Shakya R, Jho EH, Kotka P, Wu Z, Kholodilov N, Burke R, D'Agati V, Costantini F. The role of GDNF in patterning the excretory system. Dev Biol. 2005;283:70–84. doi: 10.1016/j.ydbio.2005.04.008. [DOI] [PubMed] [Google Scholar]
- 26.Maeshima A, Sakurai H, Choi Y, Kitamura S, Vaughn DA, Tee JB, Nigam SK. Glial cell-derived neurotrophic factor independent ureteric bud outgrowth from the Wolffian duct. J Am Soc Nephrol. 2007;18:3147–3155. doi: 10.1681/ASN.2007060642. [DOI] [PubMed] [Google Scholar]
- 27.Bates CM. Role of fibroblast growth factor receptor signaling in kidney development. Pediatr Nephrol. 2007;22:343–349. doi: 10.1007/s00467-006-0239-7. [DOI] [PubMed] [Google Scholar]
- 28.Hains D, Sims-Lucas S, Kish K, Saha M, McHugh K, Bates CM. Role of fibroblast growth factor receptor 2 in kidney mesenchyme. Pediatr Res. 2008 doi: 10.1203/PDR.0b013e318187cc12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jain S, Encinas M, Johnson EM, Jr, Milbrandt J. Critical and distinct roles for key RET tyrosine docking sites in renal development. Genes Dev. 2006;20:321–333. doi: 10.1101/gad.1387206. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Costantini F, Shakya R. GDNF/Ret signaling and the development of the kidney. Bioessays. 2006;28:117–127. doi: 10.1002/bies.20357. [DOI] [PubMed] [Google Scholar]
- 31.Basson MA, Akbulut S, Watson-Johnson J, Simon R, Carroll TJ, Shakya R, Gross I, Martin GR, Lufkin T, McMahon AP, et al. Sprouty1 is a critical regulator of GDNF/RET-mediated kidney induction. Dev Cell. 2005;8:229–239. doi: 10.1016/j.devcel.2004.12.004. [DOI] [PubMed] [Google Scholar]
- 32.Basson MA, Watson-Johnson J, Shakya R, Akbulut S, Hyink D, Costantini FD, Wilson PD, Mason IJ, Licht JD. Branching morphogenesis of the ureteric epithelium during kidney development is coordinated by the opposing functions of GDNF and Sprouty1. Dev Biol. 2006;299:466–477. doi: 10.1016/j.ydbio.2006.08.051. [DOI] [PubMed] [Google Scholar]
- 33.Dunn NR, Winnier GE, Hargett LK, Schrick JJ, Fogo AB, Hogan BL. Haploinsufficient phenotypes in Bmp4 heterozygous null mice and modification by mutations in Gli3 and Alx4. Dev Biol. 1997;188:235–247. doi: 10.1006/dbio.1997.8664. [DOI] [PubMed] [Google Scholar]
- 34.Miyazaki Y, Oshima K, Fogo A, Hogan BL, Ichikawa I. Bone morphogenetic protein 4 regulates the budding site and elongation of the mouse ureter. J Clin Invest. 2000;105:863–873. doi: 10.1172/JCI8256. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Michos O, Panman L, Vintersten K, Beier K, Zeller R, Zuniga A. Gremlin-mediated BMP antagonism induces the epithelial-mesenchymal feedback signaling controlling metanephric kidney and limb organogenesis. Development. 2004;131:3401–3410. doi: 10.1242/dev.01251. [DOI] [PubMed] [Google Scholar]
- 36.Batourina E, Choi C, Paragas N, Bello N, Hensle T, Costantini FD, Schuchardt A, Bacallao RL, Mendelsohn CL. Distal ureter morphogenesis depends on epithelial cell remodeling mediated by vitamin A and Ret. Nat Genet. 2002;32:109–115. doi: 10.1038/ng952. [DOI] [PubMed] [Google Scholar]
- 37.Marose TD, Merkel CE, McMahon AP, Carroll TJ. Beta-catenin is necessary to keep cells of ureteric bud/Wolffian duct epithelium in a precursor state. Dev Biol. 2008;314:112–126. doi: 10.1016/j.ydbio.2007.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Murer L, Benetti E, Artifoni L. Embryology and genetics of primary vesico-ureteric reflux and associated renal dysplasia. Pediatr Nephrol. 2007;22:788–797. doi: 10.1007/s00467-006-0390-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Batourina E, Tsai S, Lambert S, Sprenkle P, Viana R, Dutta S, Hensle T, Wang F, Niederreither K, McMahon AP, et al. Apoptosis induced by vitamin A signaling is crucial for connecting the ureters to the bladder. Nat Genet. 2005;37:1082–1089. doi: 10.1038/ng1645. [DOI] [PubMed] [Google Scholar]
- 40.Brenner-Anantharam A, Cebrian C, Guillaume R, Hurtado R, Sun TT, Herzlinger D. Tailbud-derived mesenchyme promotes urinary tract segmentation via BMP4 signaling. Development. 2007;134:1967–1975. doi: 10.1242/dev.004234. [DOI] [PubMed] [Google Scholar]
- 41.Viana R, Batourina E, Huang H, Dressler GR, Kobayashi A, Behringer RR, Shapiro E, Hensle T, Lambert S, Mendelsohn C. The development of the bladder trigone, the center of the anti-reflux mechanism. Development. 2007;134:3763–3769. doi: 10.1242/dev.011270. [DOI] [PubMed] [Google Scholar]
- 42.Airik R, Bussen M, Singh MK, Petry M, Kispert A. Tbx18 regulates the development of the ureteral mesenchyme. J Clin Invest. 2006;116:663–674. doi: 10.1172/JCI26027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Mahoney ZX, Sammut B, Xavier RJ, Cunningham J, Go G, Brim KL, Stappenbeck TS, Miner JH, Swat W. Discs-large homolog 1 regulates smooth muscle orientation in the mouse ureter. Proc Natl Acad Sci U S A. 2006;103:19872–19877. doi: 10.1073/pnas.0609326103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Iizuka-Kogo A, Ishidao T, Akiyama T, Senda T. Abnormal development of urogenital organs in Dlgh1-deficient mice. Development. 2007;134:1799–1807. doi: 10.1242/dev.02830. [DOI] [PubMed] [Google Scholar]
- 45.Murawski IJ, Myburgh DB, Favor J, Gupta IR. Vesico-ureteric reflux and urinary tract development in the Pax2 1Neu+/- mouse. Am J Physiol Renal Physiol. 2007;293:F1736–1745. doi: 10.1152/ajprenal.00221.2007. [DOI] [PubMed] [Google Scholar]
- 46.Murawski IJ, Gupta IR. Vesicoureteric reflux and renal malformations: a developmental problem. Clin Genet. 2006;69:105–117. doi: 10.1111/j.1399-0004.2005.00562.x. [DOI] [PubMed] [Google Scholar]
- 47.Lu W, Quintero-Rivera F, Fan Y, Alkuraya FS, Donovan DJ, Xi Q, Turbe-Doan A, Li QG, Campbell CG, Shanske AL, et al. NFIA haploinsufficiency is associated with a CNS malformation syndrome and urinary tract defects. PLoS Genet. 2007;3:e80. doi: 10.1371/journal.pgen.0030080. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Alcaraz A, Vinaixa F, Tejedo-Mateu A, Fores MM, Gotzens V, Mestres CA, Oliveira J, Carretero P. Obstruction and recanalization of the ureter during embryonic development. J Urol. 1991;145:410–416. doi: 10.1016/s0022-5347(17)38354-4. [DOI] [PubMed] [Google Scholar]
- 49.Santicioli P, Maggi CA. Myogenic and neurogenic factors in the control of pyeloureteral motility and ureteral peristalsis. Pharmacological Reviews. 1998;50:683–721. [PubMed] [Google Scholar]
- 50.DiBona GF, Kopp UC. Neural control of renal function. Physiol Rev. 1997;77:75–197. doi: 10.1152/physrev.1997.77.1.75. [DOI] [PubMed] [Google Scholar]
- 51.Mendelsohn C. Going in circles: conserved mechanisms control radial patterning in the urinary and digestive tracts. J Clin Invest. 2006;116:635–637. doi: 10.1172/JCI27985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Yu J, Carroll TJ, McMahon AP. Sonic hedgehog regulates proliferation and differentiation of mesenchymal cells in the mouse metanephric kidney. Development. 2002;129:5301–5312. doi: 10.1242/dev.129.22.5301. [DOI] [PubMed] [Google Scholar]
- 53.Caubit X, Lye CM, Martin E, Core N, Long DA, Vola C, Jenkins D, Garratt AN, Skaer H, Woolf AS, et al. Teashirt 3 is necessary for ureteral smooth muscle differentiation downstream of SHH and BMP4. Development. 2008;135:3301–3310. doi: 10.1242/dev.022442. [DOI] [PubMed] [Google Scholar]
- 54.Fujinaka H, Miyazaki Y, Matsusaka T, Yoshida H, Fogo AB, Inagami T, Ichikawa I. Salutary role for angiotensin in partial urinary tract obstruction. Kidney Int. 2000;58:2018–2027. doi: 10.1111/j.1523-1755.2000.00374.x. [DOI] [PubMed] [Google Scholar]
- 55.Yosypiv IV, El-Dahr SS. Role of the renin-angiotensin system in the development of the ureteric bud and renal collecting system. Pediatr Nephrol. 2005;20:1219–1229. doi: 10.1007/s00467-005-1944-3. [DOI] [PubMed] [Google Scholar]
- 56.Oshima K, Miyazaki Y, Brock JW, 3rd, Adams MC, Ichikawa I, Pope JCt. Angiotensin type II receptor expression and ureteral budding. J Urol. 2001;166:1848–1852. [PubMed] [Google Scholar]
- 57.Nishimura H, Yerkes E, Hohenfellner K, Miyazaki Y, Ma J, Hunley TE, Yoshida H, Ichiki T, Threadgill D, Phillips JA, 3rd, et al. Role of the angiotensin type 2 receptor gene in congenital anomalies of the kidney and urinary tract, CAKUT, of mice and men.PG - 1-10. Mol Cell. 1999;3 doi: 10.1016/s1097-2765(00)80169-0. [DOI] [PubMed] [Google Scholar]
- 58.Miyazaki Y, Tsuchida S, Nishimura H, Pope JCt, Harris RC, McKanna JM, Inagami T, Hogan BL, Fogo A, Ichikawa I. Angiotensin induces the urinary peristaltic machinery during the perinatal period. J Clin Invest. 1998;102:1489–1497. doi: 10.1172/JCI4401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Oliverio MI, Kim HS, Ito M, Le T, Audoly L, Best CF, Hiller S, Kluckman K, Maeda N, Smithies O, et al. Reduced growth, abnormal kidney structure, and type 2 (AT2) angiotensin receptor-mediated blood pressure regulation in mice lacking both AT1A and AT1B receptors for angiotensin II. Proc Natl Acad Sci U S A. 1998;95:15496–15501. doi: 10.1073/pnas.95.26.15496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Esther CR, Jr, Howard TE, Marino EM, Goddard JM, Capecchi MR, Bernstein KE. Mice lacking angiotensin-converting enzyme have low blood pressure, renal pathology, and reduced male fertility. Lab Invest. 1996;74:953–965. [PubMed] [Google Scholar]
- 61.Niimura F, Labosky PA, Kakuchi J, Okubo S, Yoshida H, Oikawa T, Ichiki T, Naftilan AJ, Fogo A, Inagami T, et al. Gene targeting in mice reveals a requirement for angiotensin in the development and maintenance of kidney morphology and growth factor regulation. J Clin Invest. 1995;96:2947–2954. doi: 10.1172/JCI118366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Nagata M, Tanimoto K, Fukamizu A, Kon Y, Sugiyama F, Yagami K, Murakami K, Watanabe T. Nephrogenesis and renovascular development in angiotensinogen-deficient mice. Lab Invest. 1996;75:745–753. [PubMed] [Google Scholar]
- 63.Kong XT, Deng FM, Hu P, Liang FX, Zhou G, Auerbach AB, Genieser N, Nelson PK, Robbins ES, Shapiro E, et al. Roles of uroplakins in plaque formation, umbrella cell enlargement, and urinary tract diseases. J Cell Biol. 2004;167:1195–1204. doi: 10.1083/jcb.200406025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Hu P, Deng FM, Liang FX, Hu CM, Auerbach AB, Shapiro E, Wu XR, Kachar B, Sun TT. Ablation of uroplakin III gene results in small urothelial plaques, urothelial leakage, and vesicoureteral reflux. J Cell Biol. 2000;151:961–972. doi: 10.1083/jcb.151.5.961. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Abbott BD, Birnbaum LS, Pratt RM. TCDD-induced hyperplasia of the ureteral epithelium produces hydronephrosis in murine fetuses. Teratology. 1987;35:329–334. doi: 10.1002/tera.1420350307. [DOI] [PubMed] [Google Scholar]
- 66.Okazaki T, Otaka Y, Wang J, Hiai H, Takai T, Ravetch JV, Honjo T. Hydronephrosis associated with antiurothelial and antinuclear autoantibodies in BALB/c-Fcgr2b-/-Pdcd1-/- mice. J Exp Med. 2005;202:1643–1648. doi: 10.1084/jem.20051984. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Lauder AJ, Jolin HE, Smith P, van den Berg JG, Jones A, Wisden W, Smith KG, Dasvarma A, Fallon PG, McKenzie AN. Lymphomagenesis, hydronephrosis, and autoantibodies result from dysregulation of IL-9 and are differentially dependent on Th2 cytokines. J Immunol. 2004;173:113–122. doi: 10.4049/jimmunol.173.1.113. [DOI] [PubMed] [Google Scholar]
- 68.Izquierdo L, Porteous M, Paramo PG, Connor JM. Evidence for genetic heterogeneity in hereditary hydronephrosis caused by pelvi-ureteric junction obstruction, with one locus assigned to chromosome 6p. Hum Genet. 1992;89:557–560. doi: 10.1007/BF00219184. [DOI] [PubMed] [Google Scholar]
- 69.Mackintosh P, Almarhoos G, Heath DA. HLA linkage with familial vesicoureteral reflux and familial pelvi-ureteric junction obstruction. Tissue Antigens. 1989;34:185–189. doi: 10.1111/j.1399-0039.1989.tb01735.x. [DOI] [PubMed] [Google Scholar]
- 70.McDill BW, Li SZ, Kovach PA, Ding L, Chen F. Congenital progressive hydronephrosis (cph) is caused by an S256L mutation in aquaporin-2 that affects its phosphorylation and apical membrane accumulation. Proc Natl Acad Sci U S A. 2006;103:6952–6957. doi: 10.1073/pnas.0602087103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Feliubadalo L, Arbones ML, Manas S, Chillaron J, Visa J, Rodes M, Rousaud F, Zorzano A, Palacin M, Nunes V. Slc7a9-deficient mice develop cystinuria non-I and cystine urolithiasis. Hum Mol Genet. 2003;12:2097–2108. doi: 10.1093/hmg/ddg228. [DOI] [PubMed] [Google Scholar]
- 72.Shindo T, Kurihara H, Kuno K, Yokoyama H, Wada T, Kurihara Y, Imai T, Wang Y, Ogata M, Nishimatsu H, et al. ADAMTS-1: a metalloproteinase-disintegrin essential for normal growth, fertility, and organ morphology and function. J Clin Invest. 2000;105:1345–1352. doi: 10.1172/JCI8635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Yang B, Gillespie A, Carlson EJ, Epstein CJ, Verkman AS. Neonatal mortality in an aquaporin-2 knock-in mouse model of recessive nephrogenic diabetes insipidus. J Biol Chem. 2001;276:2775–2779. doi: 10.1074/jbc.M008216200. [DOI] [PubMed] [Google Scholar]
- 74.Lloyd DJ, Hall FW, Tarantino LM, Gekakis N. Diabetes Insipidus in Mice with a Mutation in Aquaporin-2. PLoS Genet. 2005;1:e20. doi: 10.1371/journal.pgen.0010020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Green M. Further morphological effects of the short ear gene in the house mouse. J Morphol. 1951;88:1–22. doi: 10.1002/jmor.1050880102. [DOI] [PubMed] [Google Scholar]
- 76.King JA, Marker PC, Seung KJ, Kingsley DM. BMP5 and the molecular, skeletal, and soft-tissue alterations in short ear mice. Dev Biol. 1994;166:112–122. doi: 10.1006/dbio.1994.1300. [DOI] [PubMed] [Google Scholar]
- 77.Kume T, Deng K, Hogan BL. Murine forkhead/winged helix genes Foxc1 (Mf1) and Foxc2 (Mfh1) are required for the early organogenesis of the kidney and urinary tract. Development. 2000;127:1387–1395. doi: 10.1242/dev.127.7.1387. [DOI] [PubMed] [Google Scholar]
- 78.Zhou Y, Lim KC, Onodera K, Takahashi S, Ohta J, Minegishi N, Tsai FY, Orkin SH, Yamamoto M, Engel JD. Rescue of the embryonic lethal hematopoietic defect reveals a critical role for GATA-2 in urogenital development. EMBO J. 1998;17:6689–6700. doi: 10.1093/emboj/17.22.6689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Warot X, Fromental-Ramain C, Fraulob V, Chambon P, Dolle P. Gene dosage-dependent effects of the Hoxa-13 and Hoxd-13 mutations on morphogenesis of the terminal parts of the digestive and urogenital tracts. Development. 1997;124:4781–4791. doi: 10.1242/dev.124.23.4781. [DOI] [PubMed] [Google Scholar]
- 80.Held T, Paprotta I, Khulan J, Hemmerlein B, Binder L, Wolf S, Schubert S, Meinhardt A, Engel W, Adham IM. Hspa4l-deficient mice display increased incidence of male infertility and hydronephrosis development. Mol Cell Biol. 2006;26:8099–8108. doi: 10.1128/MCB.01332-06. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Aoki Y, Mori S, Kitajima K, Yokoyama O, Kanamaru H, Okada K, Yokota Y. Id2 haploinsufficiency in mice leads to congenital hydronephrosis resembling that in humans. Genes Cells. 2004;9:1287–1296. doi: 10.1111/j.1365-2443.2004.00805.x. [DOI] [PubMed] [Google Scholar]
- 82.Debiec H, Kutsche M, Schachner M, Ronco P. Abnormal renal phenotype in L1 knockout mice: a novel cause of CAKUT. Nephrol Dial Transplant. 2002;17 9:42–44. doi: 10.1093/ndt/17.suppl_9.42. [DOI] [PubMed] [Google Scholar]
- 83.Gamp AC, Tanaka Y, Lullmann-Rauch R, Wittke D, D'Hooge R, De Deyn PP, Moser T, Maier H, Hartmann D, Reiss K, et al. LIMP-2/LGP85 deficiency causes ureteric pelvic junction obstruction, deafness and peripheral neuropathy in mice. Hum Mol Genet. 2003;12:631–646. [PubMed] [Google Scholar]
- 84.Carter T. The Genetics of Luxate Mice III. Horseshoe Kidney, Hydronephrosis and Lumbar Reduction. Journal of Genetics. 1953;51:441–457. [Google Scholar]
- 85.Singh S, Robinson M, Nahi F, Coley B, Robinson ML, Bates CM, Kornacker K, McHugh KM. Identification of a unique transgenic mouse line that develops megabladder, obstructive uropathy, and renal dysfunction. J Am Soc Nephrol. 2007;18:461–471. doi: 10.1681/ASN.2006040405. [DOI] [PubMed] [Google Scholar]
- 86.Takahashi N, Chernavvsky DR, Gomez RA, Igarashi P, Gitelman HJ, Smithies O. Uncompensated polyuria in a mouse model of Bartter's syndrome. Proc Natl Acad Sci U S A. 2000;97:5434–5439. doi: 10.1073/pnas.090091297. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Takahashi N, Lopez ML, Cowhig JE, Jr, Taylor MA, Hatada T, Riggs E, Lee G, Gomez RA, Kim HS, Smithies O. Ren1c homozygous null mice are hypotensive and polyuric, but heterozygotes are indistinguishable from wild-type. J Am Soc Nephrol. 2005;16:125–132. doi: 10.1681/ASN.2004060490. [DOI] [PubMed] [Google Scholar]
- 88.Vega QC, Worby CA, Lechner MS, Dixon JE, Dressler GR. Glial cell line-derived neurotrophic factor activates the receptor tyrosine kinase RET and promotes kidney morphogenesis. Proc Natl Acad Sci U S A. 1996;93:10657–10661. doi: 10.1073/pnas.93.20.10657. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Sainio K, Suvanto P, Davies J, Wartiovaara J, Wartiovaara K, Saarma M, Arumae U, Meng X, Lindahl M, Pachnis V, et al. Glial-cell-line-derived neurotrophic factor is required for bud initiation from ureteric epithelium. Development. 1997;124:4077–4087. doi: 10.1242/dev.124.20.4077. [DOI] [PubMed] [Google Scholar]
- 90.Yu OH, Murawski IJ, Myburgh DB, Gupta IR. Overexpression of RET leads to vesicoureteric reflux in mice. Am J Physiol Renal Physiol. 2004;287:F1123–1130. doi: 10.1152/ajprenal.00444.2003. [DOI] [PubMed] [Google Scholar]
- 91.Lu W, van Eerde AM, Fan X, Quintero-Rivera F, Kulkarni S, Ferguson H, Kim HG, Fan Y, Xi Q, Li QG, et al. Disruption of ROBO2 is associated with urinary tract anomalies and confers risk of vesicoureteral reflux. Am J Hum Genet. 2007;80:616–632. doi: 10.1086/512735. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Bertoli-Avella AM, Conte ML, Punzo F, de Graaf BM, Lama G, La Manna A, Polito C, Grassia C, Nobili B, Rambaldi PF, et al. ROBO2 gene variants are associated with familial vesicoureteral reflux. J Am Soc Nephrol. 2008;19:825–831. doi: 10.1681/ASN.2007060692. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Lorenz JN, Baird NR, Judd LM, Noonan WT, Andringa A, Doetschman T, Manning PA, Liu LH, Miller ML, Shull GE. Impaired renal NaCl absorption in mice lacking the ROMK potassium channel, a model for type II Bartter's syndrome. J Biol Chem. 2002;277:37871–37880. doi: 10.1074/jbc.M205627200. [DOI] [PubMed] [Google Scholar]
- 94.Oxburgh L, Chu GC, Michael SK, Robertson EJ. TGFbeta superfamily signals are required for morphogenesis of the kidney mesenchyme progenitor population. Development. 2004;131:4593–4605. doi: 10.1242/dev.01324. [DOI] [PubMed] [Google Scholar]
- 95.Chi L, Zhang S, Lin Y, Prunskaite-Hyyrylainen R, Vuolteenaho R, Itaranta P, Vainio S. Sprouty proteins regulate ureteric branching by coordinating reciprocal epithelial Wnt11, mesenchymal Gdnf and stromal Fgf7 signalling during kidney development. Development. 2004;131:3345–3356. doi: 10.1242/dev.01200. [DOI] [PubMed] [Google Scholar]
- 96.Lo SH, Yu QC, Degenstein L, Chen LB, Fuchs E. Progressive kidney degeneration in mice lacking tensin. J Cell Biol. 1997;136:1349–1361. doi: 10.1083/jcb.136.6.1349. [DOI] [PMC free article] [PubMed] [Google Scholar]