Abstract
Purpose
This was a pilot project designed to assess the effect of individualized yoga treatment on eating disorder outcomes among adolescents receiving outpatient care for diagnosed eating disorders (Anorexia Nervosa, Bulimia Nervosa, Eating Disorder Not Otherwise Specified).
Methods
50 girls and 4 boys, aged 11–21 years were randomized to an 8 week trial of standard care versus individualized yoga plus standard care. 27 were randomized to standard care and 26 to yoga plus standard care (attrition: n = 4). Standard care (every other week physician/dietician appointments) was required to meet ethical guidelines. The control group was offered yoga after study completion as an incentive to maintain participation. Outcomes evaluated at baseline, end of trial, and one month follow-up included: Eating Disorder Examination (EDE), Body Mass Index (BMI), Beck Depression Inventory, State Trait Anxiety Inventory, and Food Preoccupation questionnaire.
Results
The yoga group demonstrated greater decreases in eating disordered symptoms. Specifically, the EDE scores decreased over time in the yoga group, while the control group showed some initial decline but then returned to baseline EDE levels at week 12. Food preoccupation was measured before and after each yoga session, and dropped significantly after all sessions. Both groups maintained current BMI levels and decreased in anxiety and depression over time.
Conclusions
Individualized yoga treatment decreased EDE scores at 12 weeks, and significantly reduced food preoccupation immediately following yoga sessions. Yoga treatment did not have a negative impact on BMI. Results suggest individualized yoga therapy holds promise as adjunctive therapy to standard care.
Background
Eating disorders are complicated medical conditions that are increasing in prevalence over time. Currently, approximately 1–5% of female adolescents are affected by eating disorders [1–6]. The Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) lists three main types of eating disorders: anorexia nervosa (AN), bulimia nervosa (BN) and eating disorder not otherwise specified (EDNOS) [5]. Medical prognosis is generally poor, with morbidity percentiles ranging between 10–20% [6–8]. Despite a wide range of treatments available, only about 50% of eating disorder (ED) patients fully recover, and of the remaining 50%, 20% are emaciated, and 25% are thin [9].
Anxiety and depression are common comorbid conditions in individuals with EDs, particularly anorexia nervosa. Anxiety rates are estimated to be 60.3% and 56.9% for individuals with AN and BN, respectively [10–11]. Approximately 50% of individuals with EDs have had a history of major depression and 20–40% of individuals with EDs experience concurrent depressive symptoms [12–14].
In addition to anxiety and depression, food preoccupation (FP) is included in most outcome measures of eating disorders and has been discussed in landmark studies investigating the impact of starvation on behavioral outcomes [15–19]. Current statistics on FP in EDs have yet to be provided. This study utilized a pilot version of a questionnaire derived from current measures to provide some indication of the qualitative impact of FP on EDs.
Individuals with EDs often attempt to control anxiety, depression and FP via exercise [20]. The substitution of yoga for more strenuous exercise may address health care provider concerns of the impact of exercise on weight loss while simultaneously reducing symptoms of anxiety, depression, and food preoccupation.
Yoga has been shown to be of preliminary use for anxiety, depression, and general ED symptoms [21–24]. The purpose of this study was to evaluate if yoga can decrease eating and psychological symptoms in adolescents with eating disorders.
Methods
Participants
All patients seeking standard care for an eating disorder at Seattle Children’s outpatient Adolescent Medicine Department received study fliers from medical staff if they met inclusion and exclusion criteria (n = 64). 10 patients declined participation. Inclusion criteria included the following: a) between 10–21 years of age, and b) met DSM-IV criteria for AN, BN and/or EDNOS. Exclusion criteria included: a) had a resting pulse less than 44 beats per minute, b) physical inability to participate in yoga as determined by the referring health care provider, and c) a co-morbid DSM-IV diagnosis of Psychotic disorder, Conversion disorder, Substance-Related Disorder, and/or an Axis II Disorder.
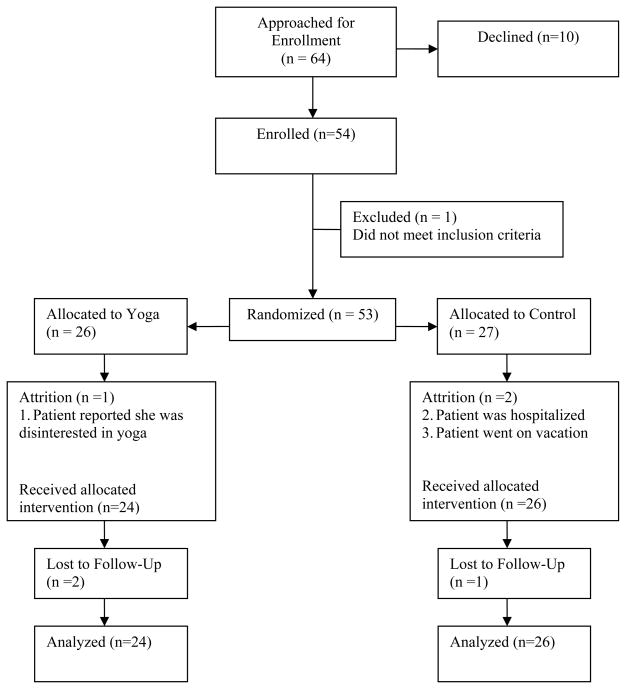
Fifty four adolescents (50 females and 4 males) with a DSM-IV diagnosis of AN, BN or EDNOS were recruited during active enrollment (February 2006-August 2006). Four participants were lost due to attrition (see Figure 1).
Figure 1.
Patient Flow.
Procedures
Interested adolescents and parents contacted study staff to schedule an in-person consent conference followed by completion of baseline measures. Informed consent (from parents/guardians) and assent (from adolescents) were obtained according to Seattle Children’s Institutional Review Board (IRB) protocols. Baseline measures included: a videotaped meal with a family member (30 minutes), an optional break (30 minutes), State Trait Anxiety Inventory and Beck Depression Inventory questionnaires (30 minutes), and the Eating Disorder Examination (1.5 hours).
Randomization to group assignment occurred after baseline measure completion. The randomization sequence was generated independently by biostatisticians at Seattle Children’s. Randomization was stratified according to eating disorder diagnosis (AN, BN or EDNOS). Participants were randomized to two treatment conditions using a stratified, permuted block scheme. The two conditions were: a) yoga or b) no yoga.
The initial phase of the study included no incentives for controls. All interested families declined participation when offered no compensation. When offered monetary compensation, families also declined. When offered the opportunity to receive yoga treatment after completion of the study, families participated and enrollment was completed in 7 months. All participants in the control group chose to complete individualized yoga treatment after the completion of the study.
All participants received standard medical care regardless of group assignment. This included appointments with a physician and dietician every other week. Weight, height, vital signs, body mass index (BMI), nutritional habits and menstrual status were monitored at these visits.
The research protocol was approved by the IRB at Seattle Children’s, and was funded by internal and external independent grants. All research practices were in compliance with the Health Insurance Portability and Accountability Act of 1996 (HIPAA).
Intervention
Participants received one hour of yoga semi-weekly for 8 consecutive weeks (1:1 instruction). Yoga was administered in clinical research rooms. Each room was carpeted and had minimal furniture or medical instruments. Room lights were dimmed to facilitate a less clinical atmosphere. Participants used the same instructor for all sessions. Instructors were certified in Viniyoga methodology by Yoga Alliance. Each instructor was a Registered Yoga Teacher at the 200 hour level (RYT-200). All instructors were trained at the same yoga studio by the same Experienced Registered Yoga Teacher, certified at the 500 hour level (E-RYT 500). Yoga sessions followed a yoga treatment manual. All yoga sessions were audio-taped. A random section of 20% of the audio recordings were assessed for inter-instructor reliability to the protocol.
Assessment
Assessments were completed for both yoga and no yoga group at three time points: baseline, post intervention (week 9), and at 1-month follow-up (week 12). Additionally, to examine possible mechanisms for the impact of yoga, food preoccupation was measured for both groups (the control group was offered yoga treatment after the conclusion of the study), before and after every yoga session by research assistants blind to group assignment.
Primary outcomes
Participants completed the Eating Disorder Examination (EDE), a standardized, semi-structured, diagnostic, clinical interview based on DSM-IV-TR criteria [25,26]. The EDE has long been considered the gold standard in the field of eating disorders based on validity, reliability, generalizabilty, and normative data [27]. It includes four subscales: restraint, eating concern, weight concern, and shape concern, which combine to form a global score. The EDE also includes physical measurements of height and weight. The EDE has been shown to have good internal consistency for each subscale and test–retest reliability and inter-rater reliability [26, 28–30].
Body Mass Index (BMI) was calculated by dividing weight (kg) by height2 (m2). Participants were weighed using a digital scale and a wall-mounted stadiometer. Shoes and excess layers of clothing were removed prior to acquiring weight, as patients were not weighed post voiding in a hospital gown. The calculated value was then compared with children of the same age and sex.
Secondary outcomes
Depression was assessed with the Beck Depression Inventory (BDI-II) [31]. The BDI-II is a 21-item self-report instrument used to assess depression in adults and adolescents (age 13 or older). The items on the BDI-II were derived from the diagnostic criteria for depression in the DSM-IV (1994) and are rated on a 4 point scale (0–3). The BDI has been shown to have good internal consistency and test–retest reliability and to be responsive to change in depressive symptoms [31].
Anxiety was assessed with the State Trait Anxiety Inventory (STAI), which consists of 40 items rated on a four-point Likert scale [32]. These items are divided into two scales: the A-state and A-trait scale, each of which consists of 20 items. State anxiety (A-state) refers to momentary anxiety and trait anxiety (A-trait) refers to a person’s overall, general, anxiety. Test-retest correlations from adolescent normative samples have shown good test-retest correlations and concurrent validity [32].
Food preoccupation (FP) is a key symptom in eating disorders. It is included in the EAT-40, EAT-26, EDI-II, and EDE [24, 16–18]. A measure solely focusing on FP has yet to be developed. Both versions of the EAT include a “bulimia and food preoccupation” subscale that includes true-false statements about FP (i.e. “I find myself too preoccupied with food”). The EDE includes a FP question, but not a FP subscale. Given the focus of the study on the use of yoga to decrease FP, a FP measure was needed. The EDE FP question was modified and used as a pilot measure. This question read: Right now, are you spending much time thinking about food, eating or calories? Is it interfering with your ability to concentrate? If so, how much is it interfering? Answers were rated on a 6-point Likert scale: (0) no impairment (no interference at all) (1) barely noticeable (it’s there in the back of my mind, but not consciously noticeable) (2) slight impairment (it’s present; gnawing) (3) minimal impairment (it’s present and pressing, but not consuming), (4) moderate impairment (it’s beginning to become consuming; I’m having trouble focusing) (5) significant impairment (it’s consuming my mind; it’s nearly unbearable), or (6) severe impairment (thinking of it every second; completely consuming; immobilizing). No psychometrics examining this question are currently available and it was not tested on healthy adolescents.
Data analysis
To examine the success of randomization procedures, chi square tests of independence and independent t-tests were used to evaluate categorical and continuous variables, respectively. There were no significant differences between the no yoga group and the yoga group on any of the variables described in this demographics section, indicating that random assignment was successful in evenly distributing third variables. As there were no significant differences, all participants are described in the preliminary analyses without respect to treatment group.
Missing data were managed in one of two ways. First, mean substitution was used to address occasional missing data points on scale items (in 2 individuals). Second, in cases with large amounts of data missing, such as full scale measures, individuals were dropped from those analyses (i.e. for outcome data points of 5 participants in the no yoga group, and for 6 participants in the yoga group).
Differences in outcomes were assessed using chi square analysis for categorical variables and one-way and mixed model analyses of variance for continuous variables. Pre/post quantitative data was examined using paired t-tests. All analyses were conducted using intent-to-treat. Partial eta squared was used as an estimate of effect size in interpreting ANOVA results. Cohen’s standards for the interpretation of partial eta squared effect size were used (1988): small (.01), medium (.06), and large (.14). Cohen’s d was used as an estimate of effect size in interpreting paired t tests. The standards are: small (.2), medium (.4), and large (.8).
Results
Preliminary analyses
All variables were normally distributed. At baseline, the mean age of the participants was 16.52 years (SD = 2.35; range = 11–21) and the mean length of eating disorder illness was 14.3 months (SD = 16.7; range = 0–45 months, with one outlier at 92 months). Over-exercising (daily participation in at least 2 organized sports, plus self initiated exercises, 5–7 days per week) was documented in 48% (n = 24) of the participants prior to the start of the study. According to chart review, 45% of participants (n = 23) had been hospitalized for their eating disorder prior to the start of the study. The majority of the sample was female (n = 46 [92%]), non-Hispanic (n = 47 [94%]), and white (n = 43 [86%]). Twenty nine participants (55%) had Anorexia Nervosa, nine (17%) had Bulimia, and fifteen (28%) had EDNOS.
In addition to study participation, many participants endorsed simultaneous treatment in other therapies and medication usage. Exploratory post-hoc analyses were conducted on participants endorsing the three forms of other treatment with sufficient sample size: Individual psychotherapy (n = 16), art therapy (n = 14), and SSRIs (n = 12). Independent t-tests comparing individuals using each of these treatments with those not using that particular treatment (e.g., those using art therapy vs. those not using art therapy) yielded no significant differences, indicating that none of these treatments had significant effects on outcome measures. Chi square tests of independence confirmed that individuals using these other forms of treatment were equally distributed across the yoga and no yoga groups, thus, there was no confounding of treatment type in the study.
As the FP measure had not been previously validated, correlations between Global EDE scores and the FP measure were examined. FP was significantly positively correlated with Global EDE scores in all but two of 96 instances; both exceptions were positive and marginally significant (ps < .1). These findings provide some evidence for concurrent validity of the measure.
Primary analyses
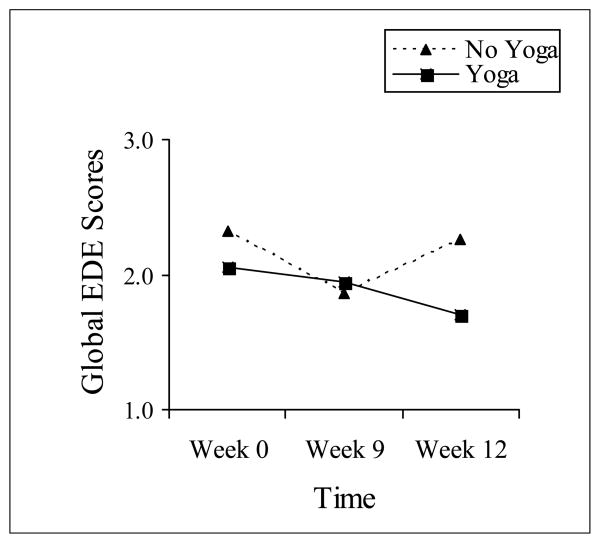
Table 1 presents the means and standard deviations of the EDE scores for both treatment groups at each assessment point. To test the hypothesis that eating disorder psychopathology would improve over time if the participant received yoga treatment, a 2 (Group- No Yoga vs. Yoga) × 3 (Time- Week 0, 9, 12) mixed model analysis of variance (ANOVA) was performed on participants’ EDE global scores. The results showed support for the hypothesis, with a significant interaction of Group by Time, F(2, 35) = 3.26, p = .05, η2 = .16. Planned comparisons revealed that the two groups’ scores declined between Weeks 0 and 9, but the yoga group’s scores continued to trend downward through follow-up at Week 12, t(21) = 1.74, p =.09. The no yoga group’s scores went in the opposite direction at the follow-up, significantly increasing between Weeks 9 and 12, t(15) = 2.67, p =.02. The overall main effects of Group and Time were non-significant (ps = .59 and .12, respectively). See Figure 2.
Table 1.
Eating Disorder Examination Scores by Group and Time
| Yoga | No Yoga | ||||
|---|---|---|---|---|---|
| EDE score | Time | M | SD | M | SD |
| Global | Week 0 | 2.06 | 1.31 | 2.32 | 1.57 |
| Week 9 | 1.94 | 1.50 | 1.86 | 1.61 | |
| Week 12 | 1.70 | 1.29 | 2.26 | 1.61 | |
| Weight Concern | Week 0 | 2.71 | 1.68 | 2.64 | 1.76 |
| Week 9 | 2.54 | 1.95 | 2.26 | 1.88 | |
| Week 12 | 2.41 | 1.83 | 2.59 | 1.97 | |
| Shape Concern | Week 0 | 2.22 | 1.46 | 2.35 | 1.60 |
| Week 9 | 2.13 | 1.75 | 1.88 | 1.72 | |
| Week 12 | 1.91 | 1.30 | 2.48 | 1.80 | |
| Eating Concern | Week 0 | 1.31 | 1.41 | 1.58 | 1.71 |
| Week 9 | 1.44 | 1.53 | 1.31 | 1.48 | |
| Week 12 | 1.10 | 1.27 | 1.47 | 1.37 | |
| Restraint | Week 0 | 2.01 | 1.64 | 2.69 | 1.70 |
| Week 9 | 1.66 | 1.37 | 2.02 | 1.81 | |
| Week 12 | 1.40 | 1.40 | 2.49 | 1.87 | |
Adult norms (N=337): restraint subscale mean: .79, SD of .97; eating concern subscale mean: .20, SD of .51; weight concern subscale mean: 1.00, SD .87; shape concern subscale mean: 1.14, SD of .98 [27]
Figure 2.
Global EDE Scores by Group and Time
The participants’ four EDE subscale scores were then examined individually, to determine what subscales were contributing to the significant interaction of Group and Time in the Global score. A series of 2 (Group) × 3 (Time) mixed model ANOVAs showed no significant effects; the interactions closest to approach significance were for Weight Concern scores, F(2, 35) = 2.79, p = .08, η2 = .14, and Shape Concern scores, F(2, 35) = 2.07, p = .14, η2 = .11. Both of these subscales followed the pattern seen in the Global scores. See Table 1 for means and standard deviations.
Secondary analyses
Scores on the BDI and STAI were examined as dependent variables in another series of 2 (Group) × 3 (Time) mixed model ANOVAs. The pattern of results on these measures was highly similar. There were significant main effects of time, such that over the study participants decreased in depression, F(2, 31) = 5.29, p = .01, η2 = .26, state anxiety, F(2, 35) = 4.28, p = .02, η2 = .2, and trait anxiety, F(2, 35) = 10.92, p = < .001, η2 = .38. There were no main effects of group and no significant interactions on these outcome measures (all ps > .3); essentially, participants improved over time in both groups. See Table 2 for descriptive statistics.
Table 2.
Depression, Anxiety, and BMI scores by Group and Time
| Yoga | No Yoga | ||||
|---|---|---|---|---|---|
| Outcome Measure | Time | M | SD | M | SD |
| Depression | Week 0 | 22.44 | 12.57 | 22.19 | 11.77 |
| Week 9 | 17.22 | 12.16 | 17.19 | 11.05 | |
| Week 12 | 16.61 | 12.62 | 17.75 | 12.72 | |
| State Anxiety | Week 0 | 42.24 | 11.47 | 45.00 | 13.64 |
| Week 9 | 41.05 | 14.66 | 40.00 | 12.42 | |
| Week 12 | 35.86 | 12.60 | 39.47 | 12.91 | |
| Trait Anxiety | Week 0 | 49.57 | 12.90 | 53.24 | 11.90 |
| Week 9 | 47.90 | 12.28 | 48.65 | 14.38 | |
| Week 12 | 43.81 | 12.04 | 47.29 | 13.56 | |
| BMI | Week 0 | 19.51 | 3.01 | 18.88 | 2.32 |
| Week 9 | 19.86 | 3.77 | 19.18 | 2.10 | |
| Week 12 | 20.01 | 3.54 | 19.38 | 2.26 | |
BDI-II cutoff scores indicated by BDI-II manual: 0–13 (minimal), 14–19 (mild), 20–28 (moderate), and 29–63 (severe).
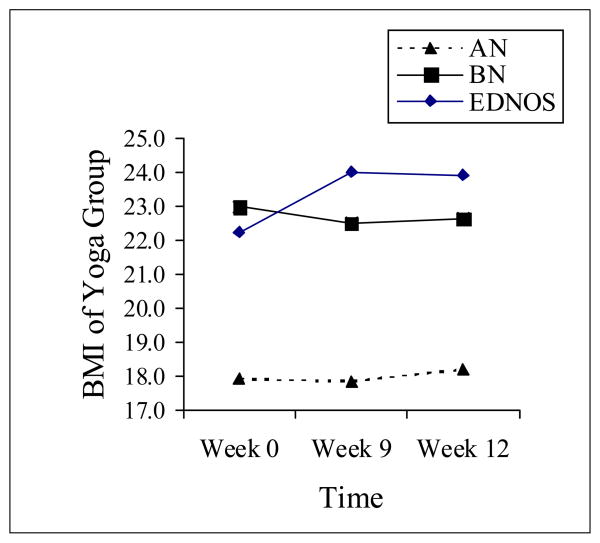
For BMI, data were analyzed by group and time and also by diagnosis in a 2 (Group) × 3 (Time) × 3 (Diagnosis) mixed model ANOVA, as treatment goals for weight outcomes differ by diagnosis. Both the no yoga and yoga groups improved over time, but not significantly so, F(2,62) = 1.28, p = .28. There was a significant main effect of group, such that the yoga group had somewhat higher overall BMI at all time points than the no yoga group, F(1,31) = 4.83, p = .04, η2 = .14. There was a significant main effect of diagnosis, such that the BN and EDNOS participants had significantly higher BMIs than the AN group at all time points, F(1,31) = 9.90, p < .001, η2 = .39. There were no other significant main effects or interactions, indicating that the yoga treatment did not adversely affect BMI over time. This was true for all three diagnostic categories. See Figure 3 for the yoga group’s data, and Table 2 for descriptive statistics on BMI in both groups. BMI increased or stayed the same in 62.2% of the sample at the 12 week followup. In the remainder of the sample, only 17.7% had BMI losses of greater than .5 points.
Figure 3.
BMI of Yoga Group by Diagnosis and Time
Participants were assessed on food preoccupation before and after each of 16 yoga sessions. For this analysis, data for the yoga group and the no yoga group (who completed yoga after the study was over) were combined. Participants in both groups completed the same measures before and after yoga sessions and there were no significant differences between groups in any of the session means to indicate they should be considered separately. Paired t-tests revealed highly significant differences (ps < .01) from pre-test to post-test in all 16 sessions, such that participants indicated less food preoccupation after doing yoga. Seven sessions had pre-post differences in the medium effect size range according to Cohen’s criteria (.4 < d < .8), and the other nine sessions had large effect sizes (d > .8).
Discussion
This pilot study is one of the first to give support to yoga as an effective adjunctive treatment to improve eating disorder symptoms. The results showed differences in outcomes for the yoga and no yoga groups over time in eating psychopathology, with yoga decreasing Global EDE scores while the no yoga group’s EDE scores decreased but then returned to baseline levels after 12 weeks. The trends in participants’ scores on the Weight and Shape Concern subscales appeared responsible for the overall pattern of findings in the Global EDE scores, more so than the Restraint and Eating Concern subscales. One hypothesis for this trend is that food preoccupation may be reduced by focusing attention on yoga poses. Participants frequently endorsed this qualitatively after yoga sessions, commenting “This is the only hour in my week when I don’t think about my weight.”
BMI scores remained stable for both groups. Yoga did not decrease weight in patients with AN, and rapid weight fluctuations were not noted for patients with BN. Many physicians are concerned about caloric expenditure in ED patients, so BMI maintenance in combination with yoga therapy is reassuring. There were no interactive effects of BMI with the yoga treatment, indicating that yoga was equally safe for patients with any of the three diagnoses.
Both groups significantly improved in anxiety and depression scores over time, possibly as a result of the standard care they were receiving. Food preoccupation scores decreased from pre-test to post-test after all yoga sessions. Given the strength of the food preoccupation effects, it is hypothesized that yoga may function as an acute intervention. Giles (1986) suggested that yoga might be useful before and after meals to help reduce food preoccupation [33]. Research investigating Giles’ theory seems feasible based on these preliminary results. Data gained from videotaped meals is being analyzed to provide further evidence for this hypothesis. While the long term effects of yoga are not known, the apparent short term symptom relief from yoga may improve the quality of life during treatment for adolescents with EDs.
Despite promising results, our study has several limitations. First, results may not generalize to inpatient or community samples. Second, although some support for the concurrent validity of the FP measure was provided, normative data is needed. Third, the limited sample of participants within each diagnostic subgroup reduced statistical power to differentiate treatment effects by diagnosis. Finally, as with any repeated measures design, repetitive testing may increase scores for participants positively as they anticipate questions and form answers ahead of time.
Future studies should: (a) utilize a larger sample size to examine yoga benefits by eating disorder subgroup; (b) utilize biological measures of physical arousal; (c) examine the acute versus long term effects of yoga; (d) examine the specific effects of yoga as compared to other relaxation strategies; (e) examine the long term outcomes of adjunctive yoga interventions on weight restoration and bone health.
Acknowledgments
The following acknowledgements include everyone who contributed significantly to the work aforementioned:
Appreciation is expressed to Jay Uomoto, PhD, who provided review and analysis of study design, and Melissa Parks, BA, and Shannon Albert, BA, who completed data entry and coding. We would also like to thank Whole Life Yoga studio for providing consultation and yoga instructors.
Funding
This publication was made possible by a generous gift from Newman’s Own, the Complementary Alternative Medicine Grant, and by Grant Number UL1 RR025014-1 from the National Center for Research Resources (NCRR), a component of the National Institutes of Health (NIH). Its contents are solely the responsibility of the authors and do not necessarily represent the official view of NCRR or NIH.
Footnotes
Individual Contributions:
Dr. Carei designed the trial, wrote the study protocol, obtained institutional approval, implemented the protocol, completed statistical analysis, and contributed significantly to the authorship of this paper.
Dr. Fyfe-Johnson implemented the study protocol, provided oversight of integrated treatments, oversaw data entry and coding, and contributed significantly to the authorship of this paper.
Dr. Collette Breuner directed recruitment, facilitated institutional approval, oversaw ethical and research code compliance, and critically reviewed and edited this paper.
Dr. Marshall provided oversight for study design and statistical methods, provided intellectual and academic feedback, and collaborated on the writing of this paper.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Tiffany Rain Carei, Department of Adolescent Medicine, Seattle Children’s, 4800 Sandpoint Way NE, Seattle, WA 98105, (425) 971-5760, Fax: (206) 987-3959.
Amber L. Fyfe-Johnson, Department of Adolescent Medicine, Seattle Children’s.
Cora Collette Breuner, Department of Adolescent Medicine, Seattle Children’s.
Margaret A. Marshall, Department of Psychology, Seattle Pacific University.
References
- 1.Golden NH, Katzman DK, Kreipe RE, et al. Eating Disorders in Adolescents: position Paper of the Society for Adolescent Medicine. J Adolesc Health. 2003;33:496–503. doi: 10.1016/s1054-139x(03)00326-4. [DOI] [PubMed] [Google Scholar]
- 2.Fisher M, Golden NH, Katzman DK, et al. Eating disorders in adolescents: a background paper. J Adolesc Health. 1995;16:420–37. doi: 10.1016/1054-139X(95)00069-5. [DOI] [PubMed] [Google Scholar]
- 3.Croll J, Neumark-Sztainer D, Sotry M, et al. Prevalence and risk and protective factors related to disordered eating behaviors among adolescent: Relationship to gender and ethnicity. J Adolesc Health. 2002;31:166–75. doi: 10.1016/s1054-139x(02)00368-3. [DOI] [PubMed] [Google Scholar]
- 4.Leichner P. Disordered eating attitudes among Canadian teenagers. CMAJ. 2002;166:707–8. [PMC free article] [PubMed] [Google Scholar]
- 5.American Psychiatric Association. Diagnostic and Statistical Manual for Mental Disorders. 4. Washington, DC: APA Press; 1994. [Google Scholar]
- 6.National Institute of Mental Health. National Comorbidity Survey (NCS) and National Comorbidity Survey Replication (NCS-R) [Accessed December, 2008];Collaborative Psychiatric Epidemiology Surveys. Available at http://www.icpsr.umich.edu/CPS.
- 7.Steinhausen HC, Boyadjieva S, Grigoroiu-Serbanescu M, et al. The outcome of adolescent eating disorders: findings from an international collaborative study. Eur Child Adolesc Psychiatry. 2003;12(Suppl 1):91–8. doi: 10.1007/s00787-003-1112-x. [DOI] [PubMed] [Google Scholar]
- 8.Steinhausen HC, Seidel R, Winkler Metzke C. Evaluation of treatment and intermediate and long-term outcome of adolescent eating disorders. Psych Med. 2000;30:1089–1098. doi: 10.1017/s0033291799002354. [DOI] [PubMed] [Google Scholar]
- 9.Speranza M, Loas G, Wallier J, et al. Predictive value of alexithymia in patients with eating disorders: a 3-year prospective study. J Psychosom Res. 2007;63(4):365–71. doi: 10.1016/j.jpsychores.2007.03.008. [DOI] [PubMed] [Google Scholar]
- 10.Bulik CM, Sullivan PF, Carter FA, et al. Lifetime anxiety disorders in women with bulimia nervosa. Compr Psychiatry. 1996;37(5):368–74. doi: 10.1016/s0010-440x(96)90019-x. [DOI] [PubMed] [Google Scholar]
- 11.Bulik CM, Sullivan PF, Fear JL, et al. Eating disorders and antecedent anxiety disorders: a controlled study. Acta Psychiatr Scand. 1997;96(2):101–7. doi: 10.1111/j.1600-0447.1997.tb09913.x. [DOI] [PubMed] [Google Scholar]
- 12.Smith C, Steiner H. Psychopathology in Anorexia Nervosa and Depression. J Am Acad Child Adolesc Psychiatry. 1992;31(5):841–3. doi: 10.1097/00004583-199209000-00009. [DOI] [PubMed] [Google Scholar]
- 13.Herpertz-Dahlmann BM, Remschmidt H. Depression in anorexia nervosa at follow-up. Int J Eat Disord. 1993;14(2):163–9. doi: 10.1002/1098-108x(199309)14:2<163::aid-eat2260140206>3.0.co;2-y. [DOI] [PubMed] [Google Scholar]
- 14.Herpertz-Dahlmann BM, Wewetzer C, Remschmidt H. The predictive value of depression in anorexia nervosa. Results of a seven-year follow-up study. Acta Psychiatr Scand. 1995;91(2):114–9. doi: 10.1111/j.1600-0447.1995.tb09750.x. [DOI] [PubMed] [Google Scholar]
- 15.Keys A, Brožek J, Henschel A, et al. The Biology of Human Starvation. Vol. 2. London: University of Minnesota Press; 1950. pp. 767–819. [Google Scholar]
- 16.Garner D, Garfinkel P. Handbook of Treatment for Eating Disorders. 2. New York: Guilford (EDE); [Google Scholar]
- 17.Garner DM, Garfinkel PE. The Eating Attitudes Test: an index of the symptoms of anorexia nervosa. Psychol Med. 1979;9(2):273–9. doi: 10.1017/s0033291700030762. [DOI] [PubMed] [Google Scholar]
- 18.Garner DM, Olmsted MP, Bohr Y, et al. The eating attitudes test: psychometric features and clinical correlates. Psychol Med. 1982;12(4):871–8. doi: 10.1017/s0033291700049163. [DOI] [PubMed] [Google Scholar]
- 19.Garner DM, Olmstead MP, Polivy J. Development and validation of a multidimensional eating disorder inventory for anorexia nervosa and bulimia. Int J Eat Disord. 1983;2(2):15–34. [Google Scholar]
- 20.Thien V, Thomas A, Markin D, et al. Pilot study of a graded exercise program for the treatment of anorexia nervosa. Int J Eat Disord. 2000;28(1):101–6. doi: 10.1002/(sici)1098-108x(200007)28:1<101::aid-eat12>3.0.co;2-v. [DOI] [PubMed] [Google Scholar]
- 21.Mishra M, Kumar Sinha R. Effect of yogic practices on depression and anxiety. Journal of Projective Psychology & Mental Health. 2001;8(1):23–27. [Google Scholar]
- 22.Sahasi G, Mohan D, Kacker C, Sahasi G, Mohan D, Kacker Chitra. Effectiveness of Yogic Techniques in the management of anxiety. Journal of Personality and Clinical Studies. 1989;5(1):51–55. [Google Scholar]
- 23.Pilkington K, Kirkwood G, Rampes H, et al. Yoga for depression: the research evidence. J Affect Disord. 2005;89(1–3):13–24. doi: 10.1016/j.jad.2005.08.013. [DOI] [PubMed] [Google Scholar]
- 24.Mitchell KS, Mazzeo SE, Rausch SM, et al. Innovative interventions for disordered eating: evaluating dissonance-based and yoga interventions. Int J Eat Disord. 2007;40(2):120–8. doi: 10.1002/eat.20282. [DOI] [PubMed] [Google Scholar]
- 25.Fairburn CG, Cooper Z. Eating Disorder Examination. In: Fairburn CG, Cooper Z, editors. Binge eating: Nature, assessment, and treatment. 12. New York: Guildford Press; 1993. pp. 317–360. [Google Scholar]
- 26.Cooper Z, Fairburn C. The Eating Disorder Examination: a semi-structured interview for the assessment of the specific psychopathology of eating disorders. Int J Eat Disord. 1987;6(1):1–8. [Google Scholar]
- 27.Guest T. Using the Eating Disorder Examination of the Assessment of Bulimia and Anorexia: issues of Reliability and Validity. Social Work in Health Care. 2000;31(4):71–83. doi: 10.1300/J010v31n04_05. [DOI] [PubMed] [Google Scholar]
- 28.Rizvi SL, Peterson CB, Crow SJ, et al. Test-retest reliability of the eating disorder examination. Int J Eat Disord. 2000;28(3):311–6. doi: 10.1002/1098-108x(200011)28:3<311::aid-eat8>3.0.co;2-k. [DOI] [PubMed] [Google Scholar]
- 29.Cooper Z, Cooper PJ, Fairburn CG. The validity of the eating disorder examination and its subscales. Br J Psychiatry. 1989;154:807–12. doi: 10.1192/bjp.154.6.807. [DOI] [PubMed] [Google Scholar]
- 30.Gross J, Rosen JC, Leitenberg, et al. Validity of the eating attitudes test and the eating disorders inventory in bulimia nervosa. J Consult Clin Psychol. 1986;54(6):875–6. doi: 10.1037//0022-006x.54.6.875. [DOI] [PubMed] [Google Scholar]
- 31.Beck AT, Steer RA, Brown GK. Beck Depression Inventory Manual. 2. New York: Harcourt Brace & Company; 1996. [Google Scholar]
- 32.Spielberger CD, Gorsuch RL, Lushene R, et al. State-Trait Anxiety Inventory for Adults. Redwood City, CA: Mind Garden, Inc; 1983. [Google Scholar]
- 33.Giles G. Anorexia nervosa and bulimia: an activity-oriented approach. Am J Occup Ther. 1985;39(8):510–7. doi: 10.5014/ajot.39.8.510. [DOI] [PubMed] [Google Scholar]