Abstract
OBJECTIVE
To examine trends in the prevalence of diabetes among delivery hospitalizations in the U.S. and to describe the characteristics of these hospitalizations.
RESEARCH DESIGN AND METHODS
Hospital discharge data from 1994 through 2004 were obtained from the Nationwide Inpatient Sample. Diagnosis codes were selected for gestational diabetes mellitus (GDM), type 1 diabetes, type 2 diabetes, and unspecified diabetes. Rates of delivery hospitalization with diabetes were calculated per 100 deliveries.
RESULTS
Overall, an estimated 1,863,746 hospital delivery discharges contained a diabetes diagnosis, corresponding to a rate of 4.3 per 100 deliveries over the 11-year period. GDM accounted for the largest proportion of delivery hospitalizations with diabetes (84.7%), followed by type 1 (7%), type 2 (4.7%), and unspecified diabetes (3.6%). From 1994 to 2004, the rates for all diabetes, GDM, type 1 diabetes, and type 2 diabetes significantly increased overall and within each age-group (15–24, 25–34, and ≥35 years) (P < 0.05). The largest percent increase for all ages was among type 2 diabetes (367%). By age-group, the greatest percent increases for each diabetes type were among the two younger groups. Significant predictors of diabetes at delivery included age ≥35 years vs. 15–24 years (odds ratio 4.80 [95% CI 4.72–4.89]), urban versus rural location (1.14 [1.11–1.17]), and Medicaid/Medicare versus other payment sources (1.29 [1.26–1.32]).
CONCLUSIONS
Given the increasing prevalence of diabetes among delivery hospitalizations, particularly among younger women, it will be important to monitor trends in the pregnant population and target strategies to minimize risk for maternal/fetal complications.
Diabetes is the most frequent metabolic complication of pregnancy and is associated with an increased risk of maternal and neonatal morbidity (1,2). Most diabetes in pregnancy is gestational diabetes mellitus (GDM). Depending on the population, GDM affects up to 14% of pregnancies, although most commonly reported figures range from 2 to 5% (3,4). With the rapid rise of type 2 diabetes among women in general, it is expected that this condition will also affect pregnant women at an increasing rate.
A number of studies have reported increasing trends for pregestational diabetes, GDM, or both (5–7). The majority of these results, however, generally describe diabetes patterns at more localized levels in the U.S. Studies that have assessed diabetes trends in pregnancy at the national level have done so with a specific focus only on GDM, reporting marked increases in prevalence over the past 2 decades (8,9).
As a comparison to these previously reported numbers and for a more comprehensive assessment of diabetes in pregnancy in the U.S., the purpose of this analysis was to examine trends and characteristics of delivery hospitalizations with a recorded diabetes diagnosis of GDM, type 1 diabetes, and type 2 diabetes between 1994 and 2004 using the Healthcare Cost and Utilization Project (HCUP) Nationwide Inpatient Sample (NIS), a nationally representative sample of inpatient care. Given the rising background rates of type 2 diabetes, together with increases in risk factors for diabetes, which may be contributing to the trends in the general population, we expected that trends among pregnant women, particularly for GDM and type 2 diabetes, would also steadily increase, reflecting the patterns reported in localized studies.
RESEARCH DESIGN AND METHODS
We obtained data from the NIS, one of a family of research databases developed as part of the HCUP. It is sponsored by the Agency for Healthcare Research and Quality in partnership with public and private statewide data organizations to provide national estimates of inpatient care delivered in the U.S. (10). During annual data collection by HCUP, all community hospitals from participating states are stratified by rural/urban location, number of beds, geographic region, teaching status, and ownership. Within each stratum, a systematic random 20% sample of hospitals (∼1,000 hospitals) is drawn (11). The NIS includes all discharges from the sampled hospitals and can be used to produce nationwide estimates of inpatient care. It is the largest collection of all-payer inpatient care data in the U.S. and provides patient demographic and diagnostic/procedural data as well as facility information.
Our analysis was conducted using NIS data from 1994 through 2004. Hospital discharge diagnoses were identified using the ICD-9-CM codes and diagnosis-related group (DRG) codes. The unit of analysis was the hospitalization of a female patient aged ≥15 years that resulted in a delivery as identified by a discharge ICD-9-CM code of V27.0–V27.9 and/or a DRG code of 370–375 listed anywhere on the discharge record. We identified hospitalizations with a diabetes diagnosis among the deliveries by the presence of ICD-9-CM codes for diabetes listed anywhere on the discharge record. GDM was identified by ICD-9-CM code 648.8X and type 1 and type 2 diabetes were identified by the appropriate 250.XX codes. Unspecified diabetes codes were defined as those that do not indicate type (790.29, 648.0–648.04, and 250–250.9). Where records were coded with two or more different diabetes code types, we constructed the following hierarchical coding scheme: if a type 1 code appeared alongside any other code(s) for diabetes, the type 1 code would supersede all others, and the discharge record would be categorized as type 1 diabetes. If any of the specific diabetes types were listed alongside an unspecified code, the more specific diabetes code type would supersede. If GDM and type 2 were listed together, that record would be categorized as type 2 diabetes. Discharge records with only unspecified diabetes codes were only included in analyses examining all diabetes.
All results were weighted estimates representing the total number of delivery hospitalizations from 1994 to 2004 in the U.S. Overall and age-specific rates of hospitalizations with any diabetes and by type were calculated per 100 deliveries. Because the sampling frame for the NIS changed over time, an alternate set of NIS discharge and hospital weights were used for the 1994–1997 dataset. These weights were calculated by HCUP in the same way as the weights for 1998 and later years of the NIS (12).
Demographic and hospital characteristics examined included maternal age, intended payer (Medicaid/Medicare, private insurance, and other types of payment), hospital location (rural/urban), geographic region (Northeast, Midwest, South, or West), mode of delivery (cesarean/vaginal), length of stay, hospital charges, and number of procedures and diagnoses. Because race is not uniformly collected by all states, we elected not to examine this variable because of the potential for systematic bias. ANOVA or χ2 and t tests were used to compare all categorical and continuous demographic and hospital variables between hospitalizations with any diabetes and no diabetes, and among each of the three diabetes types and the no diabetic group. P < 0.05 was considered significant. All charges were adjusted for inflation to 2004 dollar levels using the Consumer Price Index (13). Multivariate logistic regression was used to estimate odds ratios (ORs) and 95% CI of having an ICD-9-CM code for any diabetes and for each diabetes type in 2004 compared with that in 1994, as well as by age, urban/rural location, payer, and region. All analyses were conducted with SUDAAN (version 9; Research Triangle Institute, Research Triangle Park, NC) using survey methods that appropriately adjust for sampling weights. Because the NIS is a publicly available database that uses de-identified information, this analysis was exempt from internal review board approval.
RESULTS
Using delivery-related ICD-9-CM and DRG codes, there were 8,724,814 delivery hospitalization discharges available for analysis, 379,461 of which had a code for diabetes. Applying survey methods to adjust for sampling weights, there were an estimated 1,863,746 records with diabetes among 43,121,708 delivery discharges: an overall rate of 4.3 discharges with diabetes per 100 deliveries in the U.S. from 1994 to 2004. Among those with a code for GDM, the rate over this time period was 3.7 per 100 deliveries. Discharge records with a code for GDM accounted for the largest proportion of all delivery hospitalizations with diabetes (84.7%), followed by those with type 1 (7%), type 2 (4.7%), and unspecified (3.6%) diabetes.
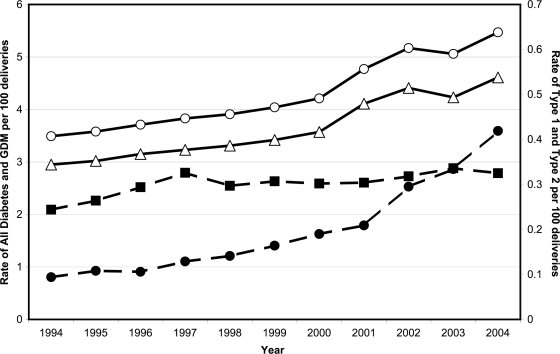
Trends in all diabetes types combined and in each of the specific types among delivery hospitalizations are presented in Fig. 1. All types significantly increased from 1994 to 2004. Rates and the percent change over time for each diabetes type are presented in Table 1 by age-group and for three selected years (first, midpoint, and last). The rates for all diabetes as well as for GDM, type 1 diabetes, and type 2 diabetes significantly increased in all of the three age-groups throughout the length of the study period. The largest percent increase overall occurred among those deliveries coded with type 2 diabetes (367%); the lowest percent increase was observed among those coded with type 1 diabetes (33%). The highest rates of diabetes overall and by type for all years combined were found among those aged >35 years. When percent change from 1994 to 2004 was examined, however, the greatest increases were observed among the younger age-groups (25–34 years and 15–24 years) for all three subtypes.
Figure 1.
Trends for all diabetes (○), GDM (▵), type 1 diabetes (■), and type 2 diabetes (●) among delivery hospitalizations in the U.S., 1994–2004.
Table 1.
Yearly and overall rates of delivery hospitalizations with diabetes in the U.S. by type, 1994–2004
| n * | Overall rate† | 1994 | 1999 | 2004 | % change‡ | |
|---|---|---|---|---|---|---|
| All diabetes | ||||||
| Age (years) | ||||||
| 15–24 | 317,457 | 2.06 | 1.72 | 1.93 | 2.50 | 45.3 |
| 25–34 | 1,058,087 | 4.84 | 3.91 | 4.61 | 6.08 | 55.5 |
| ≥35 | 488,203 | 8.37 | 7.03 | 7.71 | 10.29 | 46.4 |
| All ages (crude) | 1,863,746 | 4.32 | 3.49 | 4.04 | 5.47 | 56.3 |
| GDM | ||||||
| Age (years) | ||||||
| 15–24 | 257,255 | 1.67 | 1.37 | 1.54 | 2.02 | 47.4 |
| 25–34 | 901,570 | 4.12 | 3.34 | 3.93 | 5.16 | 54.5 |
| ≥35 | 419,879 | 7.20 | 6.06 | 6.70 | 8.79 | 45.0 |
| All ages (crude) | 1,578,703 | 3.66 | 2.95 | 3.42 | 4.61 | 56.2 |
| Type 1 diabetes | ||||||
| Age (years) | ||||||
| 15–24 | 32,813 | 0.21 | 0.17 | 0.23 | 0.24 | 42.4 |
| 25–34 | 71,570 | 0.33 | 0.27 | 0.34 | 0.35 | 28.1 |
| ≥35 | 25,917 | 0.44 | 0.36 | 0.41 | 0.45 | 24.2 |
| All ages (crude) | 130,300 | 0.30 | 0.24 | 0.31 | 0.33 | 33.2 |
| Type 2 diabetes | ||||||
| Age (years) | ||||||
| 15–24 | 14,026 | 0.09 | 0.05 | 0.07 | 0.18 | 260.0 |
| 25–34 | 48,248 | 0.22 | 0.09 | 0.18 | 0.45 | 388.0 |
| ≥35 | 25,203 | 0.43 | 0.24 | 0.34 | 0.84 | 250.0 |
| All ages (crude) | 87,477 | 0.20 | 0.09 | 0.16 | 0.42 | 366.7 |
Data are expressed as rates per 100 deliveries. P values for all trends from 1994 to 2004 were significant at P < 0.05.
*n represents estimated number of delivery hospitalizations with a diabetes diagnosis.
†Indicates overall rate from 1994 through 2004.
‡Indicates rate change from 1994 to 2004.
Demographic and hospital characteristics of delivery hospitalizations by diabetes type are presented in Table 2. Delivery hospitalizations with any diabetes versus no diabetes comprised individuals who were older, delivered in an urban versus rural hospital, and had a cesarean delivery. Hospitalizations with any diabetes also had a greater number of diagnoses on record, longer lengths of stay, and higher hospital charges, even after stratification by mode of delivery. In a comparison by diabetes type, those with type 2 diabetes were the oldest, had the highest frequency of delivery in an urban hospital, and had the highest frequency of Medicaid/Medicare as the primary payer. The highest proportions of cesarean deliveries were observed among the groups with type 1 diabetes, followed by type 2 diabetes. The type 1 deliveries also had the longest lengths of stay and the highest total hospital charges, even after stratification by mode of delivery.
Table 2.
Demographic and hospital characteristics of delivery hospitalizations by diabetes type in the U.S., 1994–2004
| All diabetes | GDM | Type 1 diabetes | Type 2 diabetes | No diabetes | |
|---|---|---|---|---|---|
| n | 1,863,746 | 1,578,703 | 130,300 | 87,477 | 41,257,962 |
| Age (years) (%)* | |||||
| 15–24 | 17.0 | 16.3 | 25.2 | 16.0 | 36.6 |
| 25–34 | 56.8 | 57.1 | 54.9 | 55.2 | 50.5 |
| ≥35 | 26.2 | 26.6 | 19.9 | 28.8 | 13.0 |
| Hospital location (%)* | |||||
| Rural | 10.6 | 10.7 | 9.6 | 9.0 | 13.3 |
| Urban | 89.4 | 89.3 | 90.4 | 91.0 | 86.7 |
| Primary expected payer (%)* | |||||
| Medicaid/Medicare | 34.1 | 33.1 | 37.9 | 43.3 | 36.7 |
| Other (i.e., self-pay) | 5.5 | 5.5 | 4.8 | 5.1 | 6.7 |
| Private | 60.5 | 61.4 | 57.3 | 51.6 | 56.6 |
| Region of hospital (%)† | |||||
| Northeast | 17.9 | 18.5 | 15.2 | 12.3 | 17.5 |
| Midwest | 21.4 | 21.4 | 23.7 | 18.6 | 22.7 |
| South | 35.9 | 35.1 | 39.4 | 41.5 | 35.0 |
| West | 24.7 | 25.0 | 21.8 | 27.6 | 24.8 |
| Mode of delivery (%)* | |||||
| Vaginal | 60.1 | 62.5 | 41.6 | 49.0 | 76.9 |
| Cesarean | 39.9 | 37.5 | 58.4 | 51.0 | 23.1 |
| No. of procedures | 2.3 ± 0.01 | 2.3 ± 0.01 | 2.3 ± 0.02 | 2.3 ± 0.03 | 2.1 ± 0.01 |
| No. of diagnoses* | 5.2 ± 0.02 | 5.0 ± 0.02 | 6.6 ± 0.03 | 6.7 ± 0.04 | 3.6 ± 0.01 |
| Length of stay (days)* | 3.1 ± 0.02 | 3.0 ± 0.01 | 4.4 ± 0.05 | 3.7 ± 0.04 | 2.4 ± 0.01 |
| Vaginal deliveries | 2.4 ± 0.01 | 2.3 ± 0.01 | 3.3 ± 0.05 | 2.8 ± 0.04 | 2.0 ± 0.01 |
| Cesarean deliveries | 4.3 ± 0.03 | 4.1 ± 0.03 | 5.2 ± 0.07 | 4.5 ± 0.05 | 3.7 ± 0.01 |
| Charges (U.S. $)*‡ | 8,876 ± 103 | 8,488 ± 100 | 11,811 ± 161 | 10,938 ± 193 | 6,635 ± 62 |
| Vaginal deliveries | 6,658 ± 71 | 6,468 ± 71 | 8,833 ± 153 | 8,071 ± 157 | 5,417 ± 51 |
| Cesarean deliveries | 12,184 ± 156 | 11,830 ± 154 | 13,922 ± 208 | 13,632 ± 249 | 10,678 ± 103 |
Data are % or means ± SEM.
*P < 0.001 between the diabetes and no diabetes groups (χ2 and t tests) and between the no diabetes group and the four diabetes types (χ2 test and ANOVA).
†Based on U.S. Census regions.
‡All charges adjusted for 2004 U.S. dollars.
Table 3 presents the adjusted odds of a diabetes diagnosis among the delivery hospitalizations. Delivery hospitalizations in 2004 were 1.5 times more likely to have a diabetes-related ICD-9-CM code compared with those in 1994 even after adjustment for age, location, payer, and geographic region. Other significant predictors of having a diabetes code at delivery included age ≥35 years vs. 15–24 years (OR 4.80 [95% CI 4.72–4.89]), urban versus rural location (1.14 [1.11–1.17]), Medicaid/Medicare versus other payment sources (1.29 [1.26–1.32]), and southern geographic region (1.10 [1.06–1.14]). The same predictors also remained significant for each diabetes type.
Table 3.
Adjusted odds of diabetes by select characteristics of delivery hospitalizations, 1994–2004
| ORs (95% CI) |
||||
|---|---|---|---|---|
| All diabetes | GDM | Type 1 diabetes | Type 2 diabetes | |
| Year | ||||
| 2004 | 1.52 (1.44–1.61) | 1.51 (1.42–1.61) | 1.28 (1.12–1.46) | 4.09 (2.92–5.71) |
| 1994 | 1.00 | 1.00 | 1.00 | 1.00 |
| Age, categorized (years) | ||||
| 15–24 | 1.00 | 1.00 | 1.00 | 1.00 |
| 25–34 | 2.64 (2.61–2.68) | 2.73 (2.69–2.76) | 1.69 (1.63–1.75) | 3.08 (2.93–3.25) |
| ≥35 | 4.80 (4.72–4.89) | 4.95 (4.86–5.04) | 2.35 (2.24–2.46) | 6.32 (5.95–6.72) |
| Hospital location | ||||
| Rural | 1.00 | 1.00 | 1.00 | 1.00 |
| Urban | 1.14 (1.11–1.17) | 1.12 (1.09–1.16) | 1.40 (1.31–1.50) | 1.39 (1.26–1.54) |
| Primary expected payer | ||||
| Medicaid/Medicare | 1.29 (1.26–1.32) | 1.24 (1.21–1.28) | 1.30 (1.25–1.36) | 1.94 (1.81–2.08) |
| Other (i.e., self pay) | 0.94 (0.90–0.97) | 0.95 (0.91–0.98) | 0.79 (0.73–0.86) | 1.08 (0.97–1.20) |
| Private | 1.00 | 1.00 | 1.00 | 1.00 |
| Region of hospital† | ||||
| Northeast | 0.99 (0.94–1.04) | 1.00 (0.95–1.06) | 0.98 (0.89–1.07) | 0.64 (0.56–0.74) |
| Midwest | 1.02 (0.98–1.06) | 1.00 (0.96–1.04) | 1.28 (1.18–1.39) | 0.87 (0.76–0.99) |
| South | 1.10 (1.06–1.14) | 1.06 (1.01–1.10) | 1.36 (1.26–1.46) | 1.15 (1.02–1.30) |
| West | 1.00 | 1.00 | 1.00 | 1.00 |
Data are ORs (95% CI). *Adjusted for all other characteristics in the table.
†Based on U.S. Census regions.
CONCLUSIONS
The most common national figures reported for GDM lie between 2 and 5%, whereas pregestational diabetes is said to affect ∼1% of all pregnancies (2,4). Other population-based investigations have also found increasing trends in GDM, consistent with our own findings (5,6,8,9). With respect to trends for type 1 and type 2 diabetes among pregnant women, no other studies, to our knowledge, have documented national trends in pregestational diabetes, which we observed to increase throughout the length of the study period.
As expected, we found that older maternal age was an independent predictor of any diabetes among delivery hospitalizations. This association likely contributed to the observed increase in the overall rate of diabetes as the proportion of U.S. births to older women also increased (14). Nonetheless, we found that diabetes rates among delivery hospitalizations increased for all ages, most sharply among the younger age-groups, noted for all three diabetes types. Other studies have documented similar findings, highlighting concerns about the rise of diabetes among younger women, a group previously thought to be at lower risk (7,8). Additional factors that may be contributing to increases include improvements in screening and detection, as well as the rising prevalence of diabetes risk factors, such as obesity, poor diet, and inactivity, which are likely contributing to trends specifically in GDM and type 2 diabetes (15).
With respect to type 1 diabetes, no clear trends have been previously established among adults. Pregnant women with pregestational diabetes have a much greater risk of maternal and fetal complications, including preeclampsia and congenital abnormalities than nondiabetic women (2). Not surprisingly, in our study, hospitalizations coded with type 1 diabetes had the highest rates of cesarean delivery, the longest lengths of stay, and the highest total charges even after stratification by mode of delivery. Rising rates of type 1 diabetes, especially among the youngest groups, are a concern because of the potential for increased future burden of severe obstetric complications as these women age and become pregnant again.
As with type 1 diabetes, outcomes of type 2 diabetic pregnancies are also marked by an increased risk for fetal malformation and intrauterine death, as well as other obstetric complications (2). Although pregnancies with pregestational diabetes have more adverse outcomes than those with GDM, perhaps the greatest significance of GDM is the increased risk of future development of type 2 diabetes that it confers (15). As GDM prevalence increases, the number of women who enter subsequent pregnancies with pregestational diabetes, as well as the number of women who carry an increased lifetime risk of developing type 2 diabetes, is likely to increase.
Another factor that could have influenced diabetes trends in our study is changes to screening recommendations and diagnostic criteria that occurred during the study time frame. In 1997, an expert committee of the American Diabetes Association issued a report modifying the diagnostic criteria for diabetes, which resulted in the use of a fasting plasma glucose test of ≥126 mg/dl, rather than 140 mg/dl as the preferred tool and cutoff to diagnose type 2 diabetes (16). The anticipated result of this modification was that an additional 2 million cases of diabetes would be diagnosed, many of which would be identified in younger individuals and as “early” type 2 diabetes (17). Another modification that occurred in 2000 was the American Diabetes Association's adoption of the Carpenter and Coustan criteria for the diagnosis of GDM via the 75-g or 100-g oral glucose tolerance test (18). Although use of the more conservative 1979 National Diabetes Data Group criteria was still supported by the American College of Obstetricians and Gynecologists, adoption of the Carpenter and Coustan criteria may have partially contributed to the increased detection of additional cases of GDM, particularly after 2000.
In addition to increased maternal age, we also demonstrated urban location to be significantly associated with all diabetes types. There is evidence of urban/rural disparities in diabetes prevalence, but contrary to our results, rural areas appear to carry a greater burden of the disease (19). Reduced access to care in rural areas with the potential for underdiagnosis, together with our inability to adjust for potential drivers of urban/rural differences, including race and socioeconomic factors, may in part explain the associations we found with urban location.
We also demonstrated payer status, specifically Medicaid/Medicare, to be a significant predictor of a diagnosis of diabetes. Previous studies of other health outcomes using administrative data have used payer status as a crude proxy for socioeconomic status (SES) in the absence of other more commonly used markers (20,21). Since enrollment in Medicaid is contingent on meeting low-income thresholds and because low SES is a well-documented risk factor for diabetes, this may partly explain the association we found between diabetes and Medicaid/Medicare payer status. Limitations, nevertheless, are present when using payer status as an SES marker, and thus results are interpreted with caution.
Finally, we also documented an association between southern region and a diabetes diagnosis at delivery for all types. According to national diabetes estimates, the U.S. South has the highest prevalence estimates in the country (15). Similarly, obesity, a major risk factor for both GDM and type 2 diabetes, is also more pronounced in the South (22). Regional disparities may also be a reflection of differences in screening, as well as differences in race, SES, and lifestyle factors, which, analogous to differences in urban/rural estimates, may account for the association found with region. Less clear, however, is an explanation for the regional differences that we also observed with type 1 diabetes. Some hypotheses have suggested that excess weight may accelerate development of type 1 diabetes, which could partly explain increasing trends (23). Regional differences in obesity may also be reflected in the association with type 1 diabetes; however, because this hypothesis has not been thoroughly tested, explanations for the regional differences in type 1 diabetes remain unclear.
There are some limitations with this analysis. First, record identification with diabetes was based on discharge ICD-9-CM codes without knowledge of the criteria used to make the diagnosis. In general, studies that use ICD-9-CM codes to describe disease trends may suffer from bias, depending on the validity of the code for the condition being examined. A previous study that evaluated ICD-9-CM codes in hospital discharge data for use in obstetric research reported high positive predictive values (96%) and moderate sensitivity (64%) for the full spectrum of diabetes codes (24). Similar results were reported in another study that assessed the validity of hospital discharge data for identifying diabetes-complicated births (25). This result suggests the potential for underestimation rather than overreporting in our numbers but would not deter from our conclusions regarding the impact of diabetes among pregnant women in the U.S. Similarly, because of the nature of the data, we also cannot rule out improvement in reporting quality over time as a partial explanation for the temporal increases. Population-based studies of laboratory-based diagnoses of GDM over similar time intervals, however, also documented increasing trends similar to what we report (5,6).
Second, because race is not consistently reported by all states in the NIS dataset, we elected to exclude any examination by race. To the extent that sampling and race reporting varied throughout the study period, interpretation of trends may be affected as it would with any unmeasured covariate (e.g., obesity). Previous studies of diabetes trends in pregnancy with more reliable race data, however, also demonstrated findings consistent with our own, even after adjustment for race (5,6). As a result, although we cannot rule out the contribution of a possible shift in the racial distribution over time to overall increases in diabetes in pregnancy in the U.S., our results nevertheless remain consistent with those of previous studies that were able to account for race.
We report increasing trends in all diabetes types among all age-groups from a sample of delivery hospitalizations in the U.S. from 1994 to 2004. Overall trends were largely driven by those with a diagnosis for GDM, although the sharpest rate increases were found among those with type 2. Most concerning was the identification of a group of relatively young women who have an increased lifetime risk of future development of type 2 diabetes and obstetric complications with subsequent pregnancies. Given the potential for maternal and perinatal morbidity and mortality associated with diabetes, it will be important to monitor trends among the pregnant population to target prevention strategies to minimize both these risks and the anticipated burden on the health care system.
Acknowledgments
No potential conflicts of interest relevant to this article were reported.
Parts of this study were presented in poster form at the 41st annual meeting of the Society for Epidemiologic Research, Chicago, Illinois, 24–27 June 2008.
Footnotes
The findings and conclusions are those of the authors and do not necessarily represent those of the Centers for Disease Control and Prevention.
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Schaefer-Graf UM, Buchanan TA, Xiang A, Songster G, Montoro M, Kjos SL. Patterns of congenital anomalies and relationship to initial maternal fasting glucose levels in pregnancies complicated by type 2 and gestational diabetes. Am J Obstet Gynecol 2000;182:313–320 [DOI] [PubMed] [Google Scholar]
- 2. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists. Number 60, March 2005. Pregestational diabetes mellitus. Obstet Gynecol 2005;105:675–685 [DOI] [PubMed] [Google Scholar]
- 3. Coustan DR. Gestational diabetes. In Diabetes in America. 2nd ed. National Diabetes Data Group. Bethesda, MD, National Institute of Diabetes and Digestive and Kidney Diseases, 1995, p. 703–717 (NIH publ. no. 95–1468) [Google Scholar]
- 4. American College of Obstetricians and Gynecologists. ACOG Practice Bulletin. Clinical management guidelines for obstetrician-gynecologists. Number 30, September 2001. Gestational diabetes. Obstet Gynecol 2001;98:525–538 [PubMed] [Google Scholar]
- 5. Ferrara A, Kahn HS, Quesenberry CP, Riley C, Hedderson MM. An increase in the incidence of gestational diabetes mellitus: Northern California, 1991–2000. Obstet Gynecol 2004;103:526–533 [DOI] [PubMed] [Google Scholar]
- 6. Dabelea D, Snell-Bergeon JK, Hartsfield CL, Bischoff KJ, Hamman RF, McDuffie RS. Increasing prevalence of gestational diabetes mellitus (GDM) over time and by birth cohort: Kaiser Permanente of Colorado GDM Screening Program. Diabetes Care 2005;28:579–584 [DOI] [PubMed] [Google Scholar]
- 7. Lawrence JM, Contreras R, Chen W, Sacks DA. Trends in the prevalence of preexisting diabetes and gestational diabetes mellitus among a racially/ethnically diverse population of pregnant women, 1999–2005. Diabetes Care 2008;31:899–904 [DOI] [PubMed] [Google Scholar]
- 8. Getahun D, Nath C, Ananth CV, Chavez MR, Smulian JC. Gestational diabetes in the United States: temporal trends 1989 through 2004. Am J Obstet Gynecol 2008;198:525.e1–e5 [DOI] [PubMed] [Google Scholar]
- 9. Kourtis AP, Bansil P, McPheeters M, Meikle SF, Posner SF, Jamieson DJ. Hospitalizations of pregnant HIV-infected women in the USA prior to and during the era of HAART, 1994–2003. AIDS 2006;20:1823–1831 [DOI] [PubMed] [Google Scholar]
- 10. U.S. Agency for Healthcare Research and Quality. Introduction to the HCUP Nationwide Inpatient Sample (NIS), 2003 [article online], 2005. Available from http://www.hcup-us.ahrq.gov/db/nation/nis/NIS_Introduction_2003_v7.pdf. Retrieved 1 August 2007
- 11. Steiner C, Elixhauser A, Schnaier J. The healthcare cost and utilization project: an overview. Eff Clin Pract 2002;5:143–151 [PubMed] [Google Scholar]
- 12. Houchens RL, Elixhauser A. Using the HCUP nationwide inpatient sample to estimate trends. HCUP Methods Series Report 2005-01 [article online], 2005. Available from http://www.hcup-us.ahrq.gov/reports/TrendReport2005_1.pdf. Accessed 1 August 2007
- 13. Consumer Price Indexes—All Urban Consumers (CPI-U) [article online], 2009. Available from ftp://ftp.bls.gov/pub/special.requests/cpi/cpiai.txt. Retrieved 10 September 2007
- 14. Martin JA, Hamilton BE, Sutton PD, Ventura SJ, Menacker F, Munson ML. Births: final data for 2003. Natl Vital Stat Rep 2005;54:1–116 [PubMed] [Google Scholar]
- 15. Beckles GLA, Thompson-Reid PE. (Eds.). Diabetes and Women's Health Across the Life Stages: A Public Health Perspective. Atlanta, GA, U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Division of Diabetes Translation, 2001. [Google Scholar]
- 16. Report of the Expert Committee on the Diagnosis and Classification of Diabetes Mellitus. Diabetes Care 1997;20:1183–1197 [DOI] [PubMed] [Google Scholar]
- 17. Sonnenberg GE. The new classification and diagnostic criteria for diabetes mellitus: rationale and implications. WMJ 1998;97:27–29, 38 [PubMed] [Google Scholar]
- 18. Carpenter MW, Coustan DR. Criteria for screening tests for gestational diabetes. Am J Obstet Gynecol 1982;144:768–773 [DOI] [PubMed] [Google Scholar]
- 19. Dabney B, Gosschalk A. Diabetes in Rural America. Rural Healthy People 2010: A Companion Document to Healthy People 2010. Vol. 1. College Station, TX, The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center, 2003. [Google Scholar]
- 20. Marcin JP, Schembri MS, He J, Romano PS. A population-based analysis of socioeconomic status and insurance status and their relationship with pediatric trauma hospitalization and mortality rates. Am J Pub Health 2003;93:461–466 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Cubbin C, Smith GS. Socioeconomic inequalities in injury: critical issues in design and analysis. Annu Rev Public Health 2002;23:349–375 [DOI] [PubMed] [Google Scholar]
- 22. Wang Y, Beydoun MA. The obesity epidemic in the United States—gender, age, socioeconomic, racial/ethnic, and geographic characteristics: a systematic review and meta-regression analysis. Epidemiol Rev 2007;29:6–28 [DOI] [PubMed] [Google Scholar]
- 23. Evertsen J, Alemzadeh R, Wang X. Increasing incidence of pediatric type 1 diabetes mellitus in southeastern Wisconsin: relationship with body weight at diagnosis. PLoS ONE 2009;4:e6873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Yasmeen S, Romano PS, Schembri ME, Keyzer JM, Gilbert WM. Accuracy of obstetric diagnoses and procedures in hospital discharge data. Am J Obstet Gynecol 2006;194:992–1001 [DOI] [PubMed] [Google Scholar]
- 25. Devlin HM, Desai J, Walaszek A. Reviewing performance of birth certificate and hospital discharge data to identify births complicated by maternal diabetes. Matern Child Health J 2009;13:660–666 [DOI] [PubMed] [Google Scholar]