Abstract
OBJECTIVE
Despite widespread dissemination of target values, achieving a blood pressure of <130/80 mmHg is challenging for many individuals with diabetes. The purpose of the present study was to examine temporal trends in blood pressure control in hypertensive individuals with diabetes as well as the potential for race, sex, and geographic disparities.
RESEARCH DESIGN AND METHODS
We analyzed baseline data from the REasons for Geographic And Racial Differences in Stroke (REGARDS) study, a national, population-based, longitudinal cohort study of 30,228 adults (58% European American and 42% African American), examining the causes of excess stroke mortality in the southeastern U.S. We calculated mean blood pressure and blood pressure control rates (proportion with blood pressure <130/80 mmHg) for 5,217 hypertensive diabetic participants by year of enrollment (2003–2007) using multivariable logistic regression models.
RESULTS
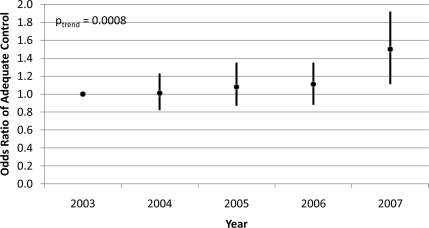
Only 43 and 30% of European American and African American diabetic hypertensive participants, respectively, demonstrated a target blood pressure of <130/80 mmHg (P < 0.001). However, a temporal trend of improved control was evident; the odds of having a blood pressure <130/80 mmHg among diabetic hypertensive participants of both races enrolled in 2007 (as compared with those enrolled in 2003) were ∼50% greater (P < 0.001) in multivariate models.
CONCLUSIONS
These data suggest temporal improvements in blood pressure control in diabetes that may reflect broad dissemination of tighter blood pressure control targets and improving medication access. However, control rates remain low, and significant racial disparities persist among African Americans that may contribute to an increased risk for premature cardiovascular disease.
In 2003, the Joint National Committee (JNC) on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure published (1) revised recommendations (JNC 7) on the management of hypertension that recommended a lower target for patients with diabetes (130/80 mmHg) than for the general population with uncomplicated essential hypertension (140/90 mmHg). This differential target was originally based on early studies (2,3), suggesting a benefit from further blood pressure reduction in helping to offset higher renal and cardiovascular risk. Subsequent evidence from the UK Prospective Diabetes Study (UKPDS) (4), the Hypertension Optimal Treatment (HOT) (5) Study, the Action in Diabetes and Vascular Disease: Preterax and Diamicron MR Controlled Evaluation (ADVANCE) (6) Study, and the Stop Atherosclerosis in Native Diabetics Study (SANDS) (7) all demonstrated improved outcomes in patients assigned to tighter blood pressure control. The Action to Control Cardiovascular Risk in Diabetes (ACCORD) (8) Study, despite discontinuation of an intensive glucose reduction arm in February 2008 (9), is investigating the value of reducing blood pressure to ≤120 mmHg, and results will be available soon.
Published goal values for blood pressure in patients with diabetes of <130 mmHg for systolic blood pressure and <80 mmHg for diastolic blood pressure represent a differential and more aggressive target for diabetic patients when compared with uncomplicated nondiabetic patients with essential hypertension. However, the extent to which this differential goal has been effectively achieved in routine practice has not been sufficiently examined, especially in large national samples. Wang (10) examined the effect of this guideline change on hypertension control in diabetic patients during the time period 1995 through 2005 and demonstrated only a modest differential improvement in blood pressure control in diabetic subjects. However, this physician office–based study was insufficient to examine the population-level impact of the 2003 JNC 7 guideline change. Population-level data from National Health and Nutrition Examination Survey 1999 through 2004 (11) suggest more substantial improvement in blood pressure control in patients with diabetes; however, the timing of these observations does not allow examination of the longitudinal effects of the 2003 guideline change. Additionally, investigators have not sufficiently examined the potential for racial and geographic differences in the extent to which blood pressure control has improved in a population-based sample in response to these guideline changes. Because of differential risks for diabetic complications by race, such studies are of critical importance. Therefore, the purpose of the present study is to examine temporal trends in blood pressure control in hypertensive individuals with diabetes as well as the potential for race, sex, and geographic disparities. To meet these goals, the primary analysis herein is to compare mean systolic and diastolic blood pressure values and the proportion of hypertensive diabetic subjects with guideline-recommended blood pressure values by race, sex, and region across different time points over the time period 2003 through 2007.
RESEARCH DESIGN AND METHODS
The REasons for Geographic And Racial Disparities in Stroke (REGARDS) study is a study of health disparities and stroke incidence, the methods of which have been described in detail elsewhere (12). In short, the study is a population-based, longitudinal cohort study of 30,228 subjects aged >45 years, 55% of whom are male, 45% female, 42% African American, 58% European American, 56% from stroke belt regions, and 44% from the rest of the country. The study was designed to examine the causes of excess stroke mortality in the southeastern U.S. and among African Americans, relative to the rest of the nation. Because of the large size of this study, its national scope, its enrollment of the cohort during the implementation of new guidelines for blood pressure control in diabetic subjects, and the inclusion of large numbers of adults with diabetes, many of whom also have hypertension, this study provides a unique opportunity to examine recent trends in blood pressure control among African American and European American hypertensive adults with diabetes using baseline data assembled across 5 years in the REGARDS study.
The study included a detailed computer-assisted telephone interview with each adult subject to collect demographic characteristics, including age, race (each subject self-reported race; this study compared only African American and European American subjects), sex, annual household income (<$20,000/year, $20,000–$35,000/year, >$35,000–$75,000/year, and >$75,000/year), education level (less than high school education, high school graduate, some college, and college graduate or higher), health insurance, health behaviors such as smoking (categorized as nonsmoker, past smoker, or current smoker), exercise (how often per week they exercised enough to work up a sweat; categorized as never, one to three times per week, or four or more times per week), alcohol consumption (categorized as nondrinker, one to seven drinks per week, and seven or more drinks per week), and medical history information.
Following the telephone interview, each subject was evaluated by a trained health professional who conducted an in-home assessment that included measurement of height and weight via standard procedures, after which BMI was calculated as the weight in kilograms divided by the square of height in meters. Blood pressure was obtained with an aneroid sphygmomanometer, using the appropriate cuff size and measured after being in the seated position with both feet on the floor for at least 3 min. Blood pressure measurement was repeated twice, and the average value was used in these analyses. At the home visit, blood specimens were obtained and total and HDL cholesterol were measured in accordance with the National Cholesterol Education Program guidelines (13). All medications were carefully recorded at the home visit, and self-reported medication adherence/nonadherence was assessed based on a validated scale (14).
For the present study, all subjects were identified who reported in their telephone interview that a physician had told them that they had both hypertension/high blood pressure and diabetes, as well as those who reported having hypertension and who had a fasting blood glucose >125 mg/dl measured during the home visit. Excluded from these analyses were any subjects who failed to respond to either the question on self-reported hypertension or self-reported diabetes (n = 32) and those without self-reported hypertension (n = 12,774), resulting in an analysis cohort of 5,217 subjects. The study was approved by the institutional review board, and each subject provided informed consent.
The primary analysis was to compare mean systolic and diastolic blood pressure values (obtained during the home visit) and the proportion of subjects meeting guideline-recommended blood pressure goals (<130/80 mmHg), by race, among hypertensive subjects with diabetes enrolled at different time points over the time period 2003 through 2007. The mean blood pressure values were compared between races and across time using a general linear model that adjusted for age, sex, region (categorized as stroke belt, stroke buckle, rest of the nation), exercise, income, education, smoking, total and HDL cholesterol, and the number of antihypertensive medications. Hypertensive diabetic subjects were also compared by race with respect to the proportion of subjects whose blood pressure was <130/80 mmHg, examined first in an unadjusted (crude) logistic regression model and in additional models that progressively adjusted for 1) demographic characteristics (race, age and sex, and region) and year of enrollment, 2) after further adjustment for risk factors related to both hypertension and diabetes (BMI and exercise), 3) after further adjustment for factors related to access to care and the potential for blood pressure control (income, education, insurance, medication use, and self-reported medication nonadherence), and finally 4) after adjustment for levels of cardiovascular risk by the introduction of additional cardiovascular risk factors (smoking and total and HDL cholesterol). All analyses were performed using SAS version 9 (SAS, Cary, NC).
RESULTS
This study included 5,217 subjects who reported having both hypertension and diabetes. Details regarding the study population are given in Table 1. The majority of the European Americans with hypertension and diabetes were male, while the majority of African Americans with hypertension and diabetes were female. As detailed in Table 2, mean blood pressure in European American diabetic hypertensive subjects was significantly lower than that in African American diabetic hypertensive subjects (130 ± 16/75 ± 10 mmHg vs. 135 ± 17/78 ± 10 mmHg) (P < 0.001). While the majority of subjects in both races were not at a target blood pressure value of <130/80 mmHg, significantly more European American than African American diabetic hypertensive subjects were at or below this threshold (43 vs. 30%, respectively; P < 0.001). In multivariate-adjusted models, the odds of African American subjects being below this target value were 39% lower than the odds of European American subjects (Table 3). Further, in multivariate-adjusted models, the odds of being below this target value were 66% higher in women than men. Self-reported medication adherence was not significantly different by race, sex, or year of enrollment; however, older age was associated with modestly lower medication adherence that was independent of education and income level. There was no clear pattern of correlates in multivariate-adjusted models that might explain the racial differences in blood pressure control. There were also no significant geographic trends in multivariate models; hypertensive diabetic subjects from the southeastern U.S. had blood pressure control rates that did not differ from those observed in subjects from across the country after other factors were controlled for.
Table 1.
Demographic and cardiovascular risk characteristics by race of the REGARDS study population with hypertension and diabetes (n = 5,217)
| European American | African American | |
|---|---|---|
| n | 2,054 | 3,163 |
| Mean age (years) | 67.2 ± 8.4 | 65.7 ± 8.6 |
| Sex (% female) | 43.2 | 62.1 |
| Stroke belt resident (%) | 64.1 | 54.1 |
| Less than high school education (%) | 11.4 | 26.9 |
| High school graduate (%) | 29.0 | 29.0 |
| Some college (%) | 29.6 | 23.9 |
| College graduate (%) | 30.0 | 20.2 |
| Health insurance (%) | 95.6 | 91.4 |
| Household annual income (%) | ||
| <$20,000 | 20.8 | 37.9 |
| $20,000–$35,000 | 30.1 | 32.1 |
| $35,000–$75,000 | 35.4 | 23.2 |
| >$75,000 | 13.7 | 6.9 |
| Proportion on antihypertensive medication reporting any nonadherence (%) | 35.5 | 34.2 |
| Current smoker (%) | 11.7 | 15.2 |
| Weekly exercise (%) | ||
| None | 43.2 | 43.1 |
| One to three times | 30.4 | 34.7 |
| Four or more times | 26.5 | 22.3 |
| Alcohol use (%) | ||
| None | 5.7 | 2.2 |
| Less than one drink per day | 35.2 | 28.7 |
| More than one drink per day | 59.1 | 69.1 |
| Mean BMI | 32 ± 6 | 33 ± 7 |
| Mean total cholesterol (mg/dl) | 176 ± 41 | 181 ± 42 |
| Mean HDL cholesterol (mg/dl) | 43 ± 13 | 50 ± 15 |
Data are means ± SD unless otherwise indicated.
Table 2.
Mean systolic and diastolic pressure values in diabetic hypertensive subjects and proportion meeting guideline targets by race
| European American | African American | |
|---|---|---|
| n | 2,054 | 3,163 |
| Systolic blood pressure | 130 ± 16 | 135 ± 17* |
| Diastolic blood pressure | 75 ± 10 | 78 ± 10* |
| Percent meeting American Diabetes Association guidelines (<130/80 mmHg) | 43% | 30% |
Data are means ± SD unless otherwise indicated.
*P < 0.01.
Table 3.
Correlates of blood pressure <130/80 mmHg among hypertensive diabetic patients from multivariate model
| Demographic | Fitness | Socioeconomic status | CV risk factor | |
|---|---|---|---|---|
| n | 5,214 | 5,064 | 4,299 | 4,054 |
| Race | 0.55 (0.49–0.62) | 0.55 (0.48–0.62) | 0.59 (0.51–0.68) | 0.61 (0.52–0.70) |
| Female sex | 1.27 (1.12–1.43) | 1.38 (1.22–1.57) | 1.45 (1.26–1.67) | 1.66 (1.42–1.94) |
| Age (10-year difference) | 1.06 (0.99–1.14) | 1.00 (0.93–1.07) | 0.99 (0.91–1.08) | 0.97 (0.88–1.05) |
| 2004 (relative to 2003) | 0.99 (0.83–1.18) | 0.99 (0.82–1.19) | 1.04 (0.86–1.27) | 1.01 (0.82–1.23) |
| 2005 (relative to 2003) | 1.24 (1.02–1.50) | 1.23 (1.01–1.50) | 1.15 (0.93–1.42) | 1.08 (0.87–1.35) |
| 2006 (relative to 2003) | 1.24 (1.01–1.53) | 1.28 (1.03–1.58) | 1.20 (0.95–1.51) | 1.11 (0.88–1.35) |
| 2007 (relative to 2003) | 1.62 (1.31–2.00) | 1.64 (1.32–2.03) | 1.62 (1.28–2.05) | 1.50 (1.18–1.92) |
| Stroke belt region | 0.98 (0.87–1.11) | 0.97 (0.86–1.10) | 1.02 (0.89–1.17) | 1.04 (0.90–1.20) |
| BMI | 0.97 (0.96–0.98) | 0.97 (0.96–0.98) | 0.97 (0.96–0.98) | |
| Exercise one to three times per week (relative to none) | 0.95 (0.82–1.09) | 0.92 (0.79–1.06) | 0.90 (0.77–1.05) | |
| Exercise four or more times per week (relative to none) | 1.02 (0.88–1.19) | 1.00 (0.85–1.18) | 0.99 (0.83–1.17) | |
| Income $20,000–$35,000 (relative to <$20,000) | 1.07 (0.90–1.28) | 1.08 (0.90–1.29) | ||
| Income $35,000– $75,000 (relative to <$20,000) | 1.36 (1.12–1.65) | 1.38 (1.13–1.69) | ||
| Income >$75,000 (relative to <$20,000) | 1.27 (0.96–1.66) | 1.30 (0.98–1.72) | ||
| Education high school graduate (relative to less than high school graduate) | 1.15 (0.94–1.41) | 1.19 (0.96–1.46) | ||
| Education some college (relative to less than high school graduate) | 1.20 (0.97–1.48) | 1.20 (0.97–1.50) | ||
| Education college graduate (relative to less than high school graduate) | 1.08 (0.86–1.35) | 1.09 (0.86–1.38) | ||
| Insurance | 0.74 (0.56–0.98) | 0.80 (0.60–1.07) | ||
| Medication adherence | 1.08 (0.94–1.24) | 1.07 (0.93–1.23) | ||
| Current smoking | 0.92 (0.75–1.12) | |||
| Total cholesterol (10 mg/dl) | 0.95 (0.93–0.97) | |||
| HDL (10 mg/dl) | 0.95 (0.90–1.00) |
Data are odds ratio (95% CI) unless otherwise indicated.
Most compelling, however, were the differences observed across the time period of enrollment. There was a significant trend for those enrolled in later years to have better blood pressure control. Mean systolic blood pressure for hypertensive diabetic African Americans enrolled in 2003 was 135.5 mmHg, while mean systolic blood pressure for those enrolled in 2007 was 130.7 mmHg. Similarly, mean systolic blood pressure for hypertensive diabetic European Americans enrolled in 2003 was 131.6 mmHg, while mean systolic blood pressure for those enrolled in 2007 was 125.9 mmHg. When examined in multivariate-adjusted models that progressively adjusted for demographics, BMI, exercise, income, education, insurance, self-reported medication adherence, smoking, total cholesterol, and HDL cholesterol, the odds of achieving a blood pressure <130/80 mmHg among those enrolled in 2007 were 50% higher than among those subjects enrolled in 2003, regardless of race (P = 0.0008 for trend) (Fig. 1). There was no significant race × time interaction observed across this time period, suggesting that improvements over time did not differ by race.
Figure 1.
Odds of hypertension control among hypertensive diabetic participants. Odds ratio and 95% CIs; n = 4,054; 2003 reference year. Adjusted for race, sex, age, region, BMI, weekly exercise income, education, insurance, availability, adherence to treatment, smoking, total cholesterol, and HDL.
CONCLUSIONS
This nationwide study of blood pressure control in African American and European American hypertensive diabetic subjects demonstrates that less than half of the subjects in both racial groups had a measured blood pressure less than the target of 130/80 mmHg recommended by the American Diabetes Association and in JNC 7, that race and sex disparities in blood pressure control continue to exist, but that between 2003 and 2007 there has been improved blood pressure control in both racial groups. The need for careful blood pressure control in hypertensive diabetic subjects is underscored by the fact that blood pressure control is one of the most important determinants of cardiovascular risk (4,15,16); it is the subject of numerous investigations, including current studies to investigate the magnitude of blood pressure lowering (6–9), and it is a major component of published guidelines on patient management that have been widely promulgated (1,17). Our data showed that income, education, insurance, and medication adherence were not independently associated with inadequate blood pressure control when other variables were controlled for, suggesting that other factors may be influencing this outcome. The potential reasons for inadequate blood pressure control are numerous and include not only patient knowledge but also biological resistance, patient lifestyle/behavioral choices, comorbid conditions and treatments, medication nonadherence, and health system factors, including limited access to care, discrimination by race and sex, competing demands of providers, lack of knowledge or adoption of the guideline, and the lack of treatment intensification. These and other factors have been recently described in the study by Bosworth et al. (18).
Data from the REGARDS study reported previously by Safford et al. (19) demonstrated that African American hypertensive subjects were more likely to have a more intense antihypertensive regimen than European Americans across all age and income strata but still were more likely to have elevated blood pressure values. This suggests treatment resistance and/or medication nonadherence. However, our findings demonstrated no racial differences in self-reported medication adherence. These findings are in contrast to those of Bosworth et al. (20), who found that African Americans in the Veterans Administration system were 81% more likely than European Americans to be nonadherent with medications for blood pressure control. However, the findings of Bosworth et al. were not limited to diabetic subjects. The fact that a smaller proportion of male than female diabetic hypertensive subjects had a measured blood pressure that was less than published target values may contribute to sex differences in premature mortality in this high-risk population.
Most significant, however, was the improvement between 2003 and 2007 in the proportion of diabetic hypertensive enrollees in both races who met target blood pressure control values. These gains were substantial and clinically important for both African Americans and European Americans. This trend has important national public health implications with respect to reducing cardiovascular risk in this high-risk population. The reason for this trend of improved blood pressure control is not clear but may relate to improved dissemination or adoption of more stringent blood pressure control target values, improved patient-specific self-management and/or lifestyle choices, improved treatment intensification, improved access to medical care, and/or improved access to antihypertensive medications as a result of the national implementation of Medicare Part D coverage and generic reduced out-of-pocket cost (WalMart-type) formularies (21). These latter factors may be particularly important, considering that the largest improvement in the proportion of subjects with adequate blood pressure control occurred between 2006 and 2007 following the implementation of both Medicare Part D insurance and WalMart's reduced-cost formulary, both in 2006.
The present study has limitations, including its cross-sectional design, the use of self-reported disease and medication adherence measures, and the lack of data on proteinuria. Specifically, it is possible that for reasons we do not understand, hypertensive diabetic individuals recruited to the study during the latter years were more likely to have improved blood pressure control. The REGARDS study did adjust its sampling rates to meet race and sex recruitment goals; however, these analyses were stratified by race and controlled for sex, and, as such, race would not have played a role in any results and sex would not have played a role in the multivariable results. In addition, we attempted to adjust for other factors that could have changed over the study period (adherence, access to health insurance, etc.), and these factors failed to mediate the observed temporal improvement in control. Nevertheless, it is possible that factors that we did not account for in the analysis could have changed over time and confounded our results. However, these potential weaknesses are offset by the large and representative nature of this national population-based study and by the measurement of blood pressure in the home by a trained professional using a standardized protocol.
These data suggest substantial national improvements in blood pressure control in individuals with concurrent hypertension and diabetes, similar to that reported by McWilliams et al. (22). The etiology of these improvements is unknown, but they may reflect the broad dissemination of tighter blood pressure control targets and improving medication access. However, despite temporal trends suggesting improvement, significant racial disparities in successful blood pressure control persist among African Americans and may contribute to the increased risk for premature cardiovascular disease and stroke in this population. Additional interventions to facilitate the achievement of goal blood pressure values in all hypertensive diabetic subjects appear warranted.
Acknowledgments
The REGARDS research project is supported by a cooperative agreement (U01 NS041588) from the National Institute of Neurological Disorders and Stroke, National Institutes of Health, Department of Health and Human Services.
No potential conflicts of interest relevant to this article were reported.
Parts of this article were presented in abstract form at the American Diabetes Association 69th Annual Scientific Sessions, New Orleans, LA, 6 June 2009 (citation: Cummings DM, Howard G, Howard V, Safford M, Prince V, Kissela B, Sands C, Lackland DT, Doherty L. Temporal progress yet persistent racial disparities in blood pressure control in diabetes: national results from the REasons for Geographic And Racial Differences in Stroke [REGARDS] study. Diabetes 2009;58[Suppl. 1]:A27–A28).
Footnotes
The costs of publication of this article were defrayed in part by the payment of page charges. This article must therefore be hereby marked “advertisement” in accordance with 18 U.S.C. Section 1734 solely to indicate this fact.
References
- 1. Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo JL, Jr, Jones DW, Materson BJ, Oparil S, Wright JT, Jr, Roccella EJ. the National Heart, Lung, and Blood Institute Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: The seventh report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure: the JNC 7 report. JAMA 2003;289:2560–72 [DOI] [PubMed] [Google Scholar]
- 2. Du X, Cruickshank K, McNamee R, Saraee M, Sourbutts J, Summers A, Roberts N, Walton E, Holmes S. Case-control study of stroke and the quality of hypertension control in northwest England. BMJ 1997;314:272–276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Lazarus JM, Bourgoignie JJ, Buckalew VM, Greene T, Levey AS, Milas NC, Paranandi L, Peterson JC, Porush JG, Rauch S, Soucie JM, Stollar C. Achievement and safety of a low blood pressure goal in chronic renal disease: the Modification of Diet in Renal Disease Study Group. Hypertension 1997;29:641–650 [DOI] [PubMed] [Google Scholar]
- 4. UKPDS Study Group. Tight blood pressure control and risk of macrovascular and microvascular complications in type 2 diabetes: UKPDS 38. BMJ 1998;317:703–713 [PMC free article] [PubMed] [Google Scholar]
- 5. Zanchetti A, Hansson L, Ménard J, Leonetti G, Rahn K, Warnold I, Wedel H. the HOT Study Group: Risk assessment and treatment benefit in intensively treated hypertensive patients of the Hypertension Optimal Treatment (HOT) study. J Hyperten 2001;19:819–825 [DOI] [PubMed] [Google Scholar]
- 6. ADVANCE Collaborative Group. Effects of a fixed combination of perindopril and indapamide on macrovascular and microvascular outcomes in patients with type 2 diabetes mellitus: a randomised controlled trial. Lancet 2007;370(9590):829–40 [DOI] [PubMed] [Google Scholar]
- 7. Howard BV, Roman MJ, Devereux RB, Fleg JL, Galloway JM, Henderson JA, Howard WJ, Lee ET, Mete M, Poolaw B, Ratner RE, Russell M, Silverman A, Stylianou M, Umans JG, Wang W, Weir MR, Weissman NJ, Wilson C, Yeh F, Zhu J. Effect of lower targets for blood pressure and LDL cholesterol on atherosclerosis in diabetes: the SANDS randomized trial. JAMA 2008;299:1678–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. ACCORD Study Group. Buse JB, Bigger JT, Byington RP, Cooper LS, Cushman WC, Friedewald WT, Genuth S, Gerstein HC, Ginsberg HN, Goff DC, Jr, Grimm RH, Jr, Margolis KL, Probstfield JL, Simons-Morton DG, Sullivan MD. Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial: design and methods. Am J Cardiol 2007;99:21i–33i [DOI] [PubMed] [Google Scholar]
- 9. The Action to Control Cardiovascular Risk in Diabetes Study Group. Effects of intensive glucose lowering in type 2 diabetes. N Engl J Med 2008;358:2545–59 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Wang YR. Lack of effect of guideline changes on hypertension control for patients with diabetes in the U.S., 1995–2005. Diabetes Care 2007;30:49–52 [DOI] [PubMed] [Google Scholar]
- 11. Ong KL, Cheung BMY, Wong LYF, Wat NMS, Tan KCB, Lam KSL. Prevalence, treatment, and control of diagnosed diabetes in the U.S. National Health and Nutrition Examination Survey 1999–2004. Ann Epidemiol 2008;18:222–229 [DOI] [PubMed] [Google Scholar]
- 12. Howard VJ, Cushman M, Pulley L, Gomez CR, Go RC, Prineas RJ, Graham A, Moy CS, Howard G. The REasons for Geographic And Racial Differences in Stroke study: objectives and design. Neuroepidemiology 2005;25:135–43 [DOI] [PubMed] [Google Scholar]
- 13. National Cholesterol Education Program Expert Panel. Third Report of the National Cholesterol Education Program (NCEP) Expert Panel: Detection, Evaluation, and Treatment of High Blood Cholesterol in Adults (Adult Treatment Panel III), Final Report. Bethesda, MD, National Cholesterol Education Program, National Heart, Lung, and Blood Institute, National Institutes of Health, September 2002. (NIH publ. no. 02-5215) [Google Scholar]
- 14. Morisky DE, Green LW, Levine DM. Concurrent and predictive validity of a self-reported measure of medication adherence. Med Care 1986;24:67–74 [DOI] [PubMed] [Google Scholar]
- 15. The Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. N Engl J Med 1993;329:977–986 [DOI] [PubMed] [Google Scholar]
- 16. Haffner SM, Lehto S, Ronnemaa T, Pyorala K, Laakso M. Mortality from coronary heart disease in subjects with type 2 diabetes and in nondiabetic subjects with and without prior myocardial infarction. N Engl J Med 1998;339:229–234 [DOI] [PubMed] [Google Scholar]
- 17. Buse JB, Ginsberg HN, Barkis GL, Clark NG, Costa F, Eckel R, Fonseca V, Gerstein HC, Grundy S, Nesto RW, Pignone MP, Plutzky J, Porte D, Redberg R, Stitzel KF, Stone NJ. Primary prevention of cardiovascular diseases in people with diabetes mellitus: a scientific statement from the American Heart Association and the American Diabetes Association. Diabetes Care 2007;30:162–172 [DOI] [PubMed] [Google Scholar]
- 18. Bosworth HB, Powers B, Grubber JM, Thorpe CT, Olsen MK, Orr M, Oddone EZ. Racial differences in blood pressure control: potential explanatory factors. J Gen Intern Med 2008;23:692–8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Safford MM, Halanych JH, Lewis CE, Levine D, Houser S, Howard G. Understanding racial disparities in hypertension control: intensity of hypertension medication treatment in the REGARDS study. Ethnicity and Disease 2007;17:421–6 [PubMed] [Google Scholar]
- 20. Bosworth HB, Dudley T, Olsen MK, Voils CI, Powers B, Goldstein MK, Oddone EZ. Racial differences in blood pressure control: potential explanatory factors. Am J Med 2006;119:70.e9–e15 [DOI] [PubMed] [Google Scholar]
- 21. Wagner TH, Heisler M, Piette JD. Prescription drug co-payments and cost-related medication underuse. Health Econ Policy Law 2008;3:51–67 [DOI] [PubMed] [Google Scholar]
- 22. McWilliams JM, Meara E, Zaslavsky AM, Ayanian JZ. Differences in control of cardiovascular disease and diabetes by race, ethnicity, and education: U.S. trends from 1999 to 2006 and effects of Medicare coverage. Ann Intern Med 2009;150:505–515 [DOI] [PubMed] [Google Scholar]