INTRODUCTION
The primary goal of physical rehabilitation for people with chronic lung disease, including chronic obstructive lung disease (COPD), is to improve function. In terms of the International Classification of Functioning, Disability and Health (ICF),1 physical therapy typically focuses on improving activity, which may result in increased participation in pursuits that are meaningful to the individual. A commonly used and related concept is functional status. Keith2 described functional status as “physical function including activity restrictions and fitness; psychological function including affective and cognitive functioning, social function including limitations in usual roles or major activity, social integration, social contact, and intimacy.” There are 2 primary methods of assessing functional status—questionnaires and performance-based tests. The most frequently used tools are questionnaires. Generic questionnaires such as the Functional Status Questionnaire,3 Extended Activities of Daily Living scale,4 and the SF-365 are available. However, disease specific questionnaires such as the Chronic Respiratory Questionnaire,6 the St. George's Respiratory Questionnaire,7 and the Pulmonary Functional Status and Dyspnea Questionnaire8 are commonly used for people with chronic lung disease. Questionnaires are generally inexpensive, quick to administer, and allow patients to express their perception of their function. However, there are a number of disadvantages associated with the use of questionnaires.9–12 Specifically, patients' responses may be affected by social and personal expectations of the purpose of the questionnaire. Also, responses may change depending on a patient's cognition or psychological status. In some circumstances, patients may state that they are capable of completing a task but do not consider the time required to complete the activity. Without additional information that is difficult to quantify, a patient may appear to function well when this is not the case. Another difficulty associated with the use of questionnaires is that disease progression in people with a chronic disease may result in activity limitation that could decrease the symptoms of interest. Such a change could erroneously be interpreted as an improvement in health status. For instance, people who experience dyspnea while climbing stairs may stop doing this activity and take the elevator instead. When questioned, this person may no longer report dyspnea when climbing stairs. The person may not be trying to hide the truth, but may have forgotten the discomfort once it no longer occurs.
Objective, performance-based tests avoid many of the difficulties noted above. The six-minute walk test (6MWT) is the most frequently used objective test of functional capacity for people with respiratory disease.13 Patients are told to walk as far as possible, in 6 minutes, over a 100 foot, level, indoor course. The psychometric properties of the test have been examined in detail and the test has been shown to be a reliable measure of the distance walked in people with COPD when it is conducted according to standardized guidelines.13,14 The length of the hallway used for the walk,15 the instructions given to the subject,16 the type and amount of encouragement given,16 and the number of learning trials17 have all been shown to affect test performance and reliability. The test is simple to administer and generally well accepted by patients but it does not assess how walking ability affects functional status or participation, as it is defined in the ICF model. Furthermore, it does not assess how dyspnea during unsupported arm activities8,18,19 such as making beds, shelving dishes and doing the laundry affects functional status. As the prevalence of COPD in women increases20–23 the definition and assessment of function will likely need to expand to include more of these activities of daily living (ADL). Most objective tests of physical performance, like the 6MWT, focus on mobility dysfunction or on people having severe limitations.24–27 In contrast, the Assessment of Motor and Process Skills (AMPS) is a 26 item test that measures the quality of a person's activities of daily living (ADL).28 Unfortunately, the test is time consuming to conduct and it would be exhausting for many people with COPD. Furthermore, the assessment of process ability that is an integral part of this test is not usually relevant for people with COPD. The AMPS has not been validated in people with COPD in whom dyspnea plays a significant role in limiting function. Thus the Glittre ADL test was developed to address the need for a more representative, objective assessment of function in people with COPD.12
TEST ADMINISTRATION
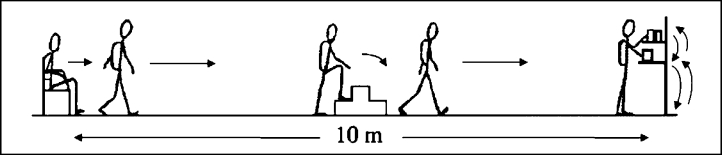
The Glittre ADL test is a standardized test that uses ADL-like activities that involve rising from a chair, lifting, carrying, and bending.12 The primary outcome is the time taken to complete the test. Figure 1 shows a schematic representation of the test. Subjects are instructed to rise from a chair and walk 10 meters, ascending a 2-step rise about half way along that distance, to reach a shelving unit. The shelves are positioned at shoulder and waist height. The subject moves 3 cartons, each weighing 1 kg, from the upper to the lower shelf and then to the floor. The sequence is reversed so that each carton is returned to the top shelf before the subject returns to the starting position at the chair. At that time the subject sits down and immediately rises to begin the next lap. The test ends when a subject completes 5 of these laps. Subjects are told to perform the test as quickly as possible. Rests are allowed but subjects are told to resume activity as soon as possible. No encouragement is given during the test. Each step of the rise is 17 cm high and 24 cm deep. During the test, patients wear a backpack filled with a 2.5 (women) or 5 kg (men) weight. The 2.5 kg weight simulates the weight of a supplemental oxygen unit, which can be exchanged for the weight when appropriate. This allows the addition of oxygen for future tests without affecting the integrity of the test. In order to standardize the test time to be useful for both genders, the authors state that doubling the backpack weight for men “yielded about the same range of time to complete the test in both genders.”12 The differential backpack weight appears to be a way to normalize for differences in muscle mass between men and women, which could affect test time. However, this crude adjustment may affect test validity. Further investigation of the affect of this method of correcting for gender differences need to be investigated.
Figure 1.
Schematic representation of the Glittre ADL-Test.
Reproduced with permission by Elsevier, Co.
VALIDITY
Skumlien et al12 assessed the validity of the test in 57 subjects (31 male) who were entering an inpatient pulmonary rehabilitation program in Norway. The mean FEV1 (forced expiratory volume in 1 sec) for the group was 48% of predicted, indicating moderate to severe disease according to the Global Initiative on Obstructive Lung Disease (GOLD) classification.29
The activities in the test were based on work by Lareau and colleagues8 and on the London Chest Activity of Daily Living Scale.30 Furthermore, the occupational therapists who worked in the pulmonary rehabilitation program believed they were appropriate. The test, including subject instructions, was administered in less than 20 minutes. The mean ADL-time was 4.67 minutes (range 2.57-14.47).
Validity was tested by comparing ADL-time with results from standardized disease specific questionnaires and the 6MWT. Scores from the St. George's Respiratory Questionnaire (SGRQ) that assesses health-related quality of life and the Pulmonary Functional Status and Dyspnea Questionnaire (PFSDQ) were compared to ADL-time. The total and subscales scores for the 2 questionnaires were used in the validity study. The SGRQ has subscale scores for symptoms (SGRQsym), activities that cause or are limited by breathlessness (SGRQact) and the impact of disease on social function and psychological disturbances (SGRQimp).31 Higher scores indicate poorer health.31 A Spearman Signed Rank test demonstrated significant correlation (r = 0.43, p < 0.01) between ADL-time and SGRQ activity scores.12 The PFSDQ provides an assessment of the effect of dyspnea during 79 ADLs (PFSDQdys); the change in activity level on those 79 activities that has occurred since developing COPD (PFS-DQact) as well as a general assessment of how the person feels during most day-to-day activities (PFSDQ6).32 Spearman Signed rank test demonstrated significant correlation (r = 0.30 − 0.35, p < 0.05) with PFSDQ dyspnea and general assessment scales.12 Interestingly, the ADL-time was significantly correlated with the SGRQact (p < 0.01) but not the PFSDQact, raising concerns about test validity. The correlation between ADL time and the 6MWT distance (6MWD) (ρ = − 0.82, p < 0.05) was strong but there was a great deal of variability in the ADL-time at any given 6MWD, particularly when subjects did not cover much distance. Both the ADL-time and the 6MWD were significantly correlated with the PFSDQdys (ρ = 0.30 and ρ= −0.47, respectively) and the SGRQact (ρ = 0.43 and ρ= −0.56, respectively). Correlations with measures of lung function, age, body mass index, and hospitalization rate during the preceding year were similar for the 6MWD and the ADL-time.
The strong correlation between ADL-time and the 6MWD suggests that the 2 tests are assessing a similar construct. This suggests that the 2 tests might be valuable in pulmonary rehabilitation practice. Generally, the correlation between the 6MWD and scores on the PFSDQ and the SGRQ was higher than that for the ADL-time, which would suggest that the 6MWT is a better tool to assess functional impairment associated with dyspnea. Skumlien et al12 state that the PFSDQ6, is the best score to assess functional limitation. However, the superiority of the PFSDQ6, as a gold standard measure of function has not been proven. In addition, the Glittre ADL is a functional test, where the PFSDQ is a self–report questionnaire. Therefore, associating the validity of the ADL-time to a survey result seems tenuous.
RELIABILITY
Each of the 57 patients who took part in the validation study repeated the ADL-test at the same time of day, one day after initial testing.12 This data was used to assess test-retest reliability. The dyspnea ratings for both tests were not different, therefore subjects were deemed to have expended the same effort on both test days. The Spearman ρ between ADL-test 1 and 2 was 0.93 (p < 0.001). Scores on ADL-test 2 were, on average, 0.37 min less than those for ADL-test 1 95% CI (− 0.20 to −0.54). Thus, the learning effect was considered to be 7% to the total ADL-time.
Responsiveness to Change
Skumlien et al12 assessed test responsiveness in 40 subjects (22 male) with a mean FEV1 of 45% of predicted. Subjects completed the ADL-test on admission to and following 4 weeks of daily participation in a multidisciplinary, inpatient pulmonary rehabilitation program. The program consisted of education, group and individual exercise, occupational therapy, and relaxation and energy conservation training. ADL-time decreased by 0.89 min [95% CI (-0.48 to −1.30)] following rehabilitation. The response after completing the rehabilitation program was significantly greater than the measured learning effect (p = 0.01). Unfortunately the change in ADL-time was not examined in relation to changes in the PFSDQ and the SGRQ.
Clinically Significant Difference
The minimally clinically important difference in ADL-time has not been determined; however, based on the pre- and posttesting results, the minimum statistically significant difference would be approximately a 1 minute decrease in ADL time.
CONCLUSION
The Glittre ADL-test is an easy to administer, simple, reliable test that assesses activities that simulate functional tasks. In addition to ambulation, the test includes rising from a chair, lifting, carrying, and bending. These tasks include activities using both lower and upper extremities that are deemed difficult for patients with COPD to perform. The inclusion of upper extremity activities makes it more similar to daily activity limitations than a walking test alone (6MWT). The test is also standardized for the use of oxygen during the test; however, further investigation on the gender effects of the weight of the oxygen tank needs to be documented.
The Glittre ADL test was field tested in Europe, in a group of patients participating in inpatient pulmonary rehabilitation. Pulmonary rehabilitation in Europe is similar to that in the United States; therefore, patients in this study should be representative of our patient's rehabilitation programs. It is surprising that the test's validity, when correlated with questionnaires addressing health-related quality of life, did not exceed that of the 6MWT. Skumlien and colleagues12 suggest that this may be because the questionnaires rely on the accuracy of patients' memories of activities that they may have discontinued. Comparison with another objective measure of functional status is needed to provide stronger support for the validity of the test. Presently, it would be difficult to recommend using the Glittre ADL-test in place of the 6MWT, which requires less equipment. In addition, the 6MWT is widely used and if properly administered, can be used to compare interventions from different research trials. However, with additional testing, the Glittre ADL test shows promise as a reliable and valid method to measure ability to perform activities of daily living in patients with COPD participating in rehabilitation.
REFERENCES
- 1.World Health Organization . International Classification Functioning, Disability and Health (ICF) Geneva, Switzerland: World Health Organization; 2001. [Google Scholar]
- 2.Keith RA. Functional status and health status. Arch Phys Med Rehabil. 1994;75:478–483. doi: 10.1016/0003-9993(94)90175-9. [DOI] [PubMed] [Google Scholar]
- 3.Jette A. Functional capacity evaluation: an empirical approach. Arch Phys Med Rehabil. 1980;61:85–89. [PubMed] [Google Scholar]
- 4.Lincoln NB, Gladman JRF. The extended activities of living scale: a further validation. Disabil Rehabil. 1992;14:41–43. doi: 10.3109/09638289209166426. [DOI] [PubMed] [Google Scholar]
- 5.Ware JE, Sherbourne CD. The MOS 36-item Short Form Health Survey (SF-36) Med Care. 1992;30:473–483. [PubMed] [Google Scholar]
- 6.Guyatt GH, Berman LB, Townsend M, et al. A measure of quality of life for clinical trials in chronic lung disease. Thorax. 1987;42:773–778. doi: 10.1136/thx.42.10.773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Jones PW, Quirk FH, Baveystock CM, et al. A selfcomplete measure of health status for chronic airflow limitation: the St. George's respiratory questionnaire. Am Rev Respir Dis. 1992;145:1321–1327. doi: 10.1164/ajrccm/145.6.1321. [DOI] [PubMed] [Google Scholar]
- 8.Lareau SC, Meek PM, Roos PJ. Development and testing of the modified version of the pulmonary functional status and Dyspnea questionnaire (PFSDQ-M) Heart Lung. 1998;27:159–168. doi: 10.1016/s0147-9563(98)90003-6. [DOI] [PubMed] [Google Scholar]
- 9.Belazi D. Measuring health status and quality of life in disease management programs. Disease Management. 2002;5:61–67. [Google Scholar]
- 10.Lareau SC, Breslin EH, Meek PM. Functional status instruments: outcome measure in the evaluation of patients with chronic obstructive pulmonary disease. Heart Lung. 1996;25:212–224. doi: 10.1016/s0147-9563(96)80032-x. [DOI] [PubMed] [Google Scholar]
- 11.ZuWallack R. Outcome Assessment. In: Hodgkin JE, Celli BR, Connors GL, editors. Pulmonary Rehabilitation. Guideline to Success. Philadelphia, Pa: Lippincott Williams & Wilkins; 2000. pp. 363–387. [Google Scholar]
- 12.Skumlien S, Hagelund T, Bjortuft O, Ryg MS. A field test of functional status as performance of activities of daily living in COPD patients. Resp Med. 2006;100:316–323. doi: 10.1016/j.rmed.2005.04.022. [DOI] [PubMed] [Google Scholar]
- 13.ATS Statement: Guidelines for the Six-Minute Walk Test. Am J Respir Crit Care Med. 2002;166:111–117. doi: 10.1164/ajrccm.166.1.at1102. [DOI] [PubMed] [Google Scholar]
- 14.Solway S, Brooks D, Lacasse Y, Thomas S. A qualitative systematic overview of the measurement properties of functional walk tests used in the cardiorespiratory domain. Chest. 2001;119:256–270. doi: 10.1378/chest.119.1.256. [DOI] [PubMed] [Google Scholar]
- 15.Sciurba F, Criner GJ, Lee SM, et al. Six-minute walk distance in chronic obstructive pulmonary disease: Reproducibility and effect of walking course layout and length. Am J Respir Crit CareMed. 2003;167:1522–1527. doi: 10.1164/rccm.200203-166OC. [DOI] [PubMed] [Google Scholar]
- 16.Guyatt GH, Pugsley SO, Sullivan MJ, et al. Effects of encouragement on walking test performance. Thorax. 1984;39:818–822. doi: 10.1136/thx.39.11.818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guyatt GH, Sullivan MJ, Thompson PJ, et al. The 6-min walk: a new measure of exercise capacity in patients with chronic CHF. Can Med Assoc J. 1985;132:919–923. [PMC free article] [PubMed] [Google Scholar]
- 18.Ries AL, Ellis B, Hawkins RW. Upper extremity training in chronic obstructive pulmonary disease. Chest. 1988;93:688–692. doi: 10.1378/chest.93.4.688. [DOI] [PubMed] [Google Scholar]
- 19.Tangri S, Woolf CR. The breathing pattern in chronic obstructive lung disease during performance of some common daily activities. Chest. 1973;63:126–127. doi: 10.1378/chest.63.1.126. [DOI] [PubMed] [Google Scholar]
- 20.Martinez FJ, Curtis JL, Sciurba F, et al. National Emphysema Treatment Trial Research Group. A randomized trial comparing lung-volume-reduction surgery with medical therapy for severe emphysema. N Engl J Med. 2003;348:2059–2073. doi: 10.1056/NEJMoa030287. [DOI] [PubMed] [Google Scholar]
- 21.Martinez FJ, Curtis JL, Sciurba F, et al. Sex differences in severe pulmonary emphysema. Am J Respir Crit Care Med. 2007;176:243–252. doi: 10.1164/rccm.200606-828OC. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Brisson L, Bryanton V, Camp P, et al. The Lung Association. Women and COPD. A National Report, 2006. Available at: http://www.lung.ca/_resources/Women_COPD_Report_2006.pdf Accessed October 10, 2008.
- 23.Watson L, Vestbo J, Postma DS, et al. Gender differences in the management and experience of chronic obstructive pulmonary disease. Respir Med. 2004;98:1207–1213. doi: 10.1016/j.rmed.2004.05.004. [DOI] [PubMed] [Google Scholar]
- 24.Gerety MB, Mulrow CD, Ruley MR, et al. Development and validation of a physical performance instrument for the functionally impaired elderly: The Physical Disability Index (PDI) J Gerontol. 1993;48:M33–38. doi: 10.1093/geronj/48.2.m33. [DOI] [PubMed] [Google Scholar]
- 25.Guralnik JM, Simonsick EM, Ferrucci L, et al. A short physical performance battery assessing lower extremity function: association with self-reported disability and prediction of mortality and nursing home admission. J Gerontol. 1994;49:M85–94. doi: 10.1093/geronj/49.2.m85. [DOI] [PubMed] [Google Scholar]
- 26.Keith RA, Granger CV, Hamilton BB, Sherwin FS. The functional independence measure: a new tool for rehabilitation. In: Eisenberg MG, Grzesiak RC, editors. Advances in Clinical Rehabilitation. Vol.1. New York, NY: Springer; 1987. pp. 6–18. [PubMed] [Google Scholar]
- 27.Winograd CH, Lemsky CM, Nevitt MC, et al. Development of a physical performance and mobility examination. J Am Geriatr Soc. 1994;42:743–749. doi: 10.1111/j.1532-5415.1994.tb06535.x. [DOI] [PubMed] [Google Scholar]
- 28.Fisher AG. Assessment of Motor and Process Skills. Development, Standardization, and Administration Manual. 6th ed. Vol 1. Fort Collins, Colo: Three Star Press; 2006. [Google Scholar]
- 29.Rabe KF, Hurd S, Anzueto A, et al. Global Strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. GOLD Executive Summary. Am J Respir Crit Care Med. 2007;176:532–555. doi: 10.1164/rccm.200703-456SO. [DOI] [PubMed] [Google Scholar]
- 30.Garrod R, Bestall JC, Paul EA, Wedzicha JA, Jones PW. Development and validation of the standardized measure of activity of daily living in patients with severe COPD: the London chest activity of daily living scale (LCADL) Respir Med. 2000;94:589–596. doi: 10.1053/rmed.2000.0786. [DOI] [PubMed] [Google Scholar]
- 31.Jones PW, Quirk FH, Baveystock CM. The St. George's Respiratory Questionnaire. Respir Med. 1991;85(Suppl B):25–31. doi: 10.1016/s0954-6111(06)80166-6. [DOI] [PubMed] [Google Scholar]
- 32.Lareau SC, Carrieri-Kohlman V, Janson-Bjerklie S, Roos PJ. Development and testing of the Pulmonary Functional Status and Dyspnea Questionnaire (PFSDQ) Heart Lung. 1994;23:242–250. [PubMed] [Google Scholar]