Abstract
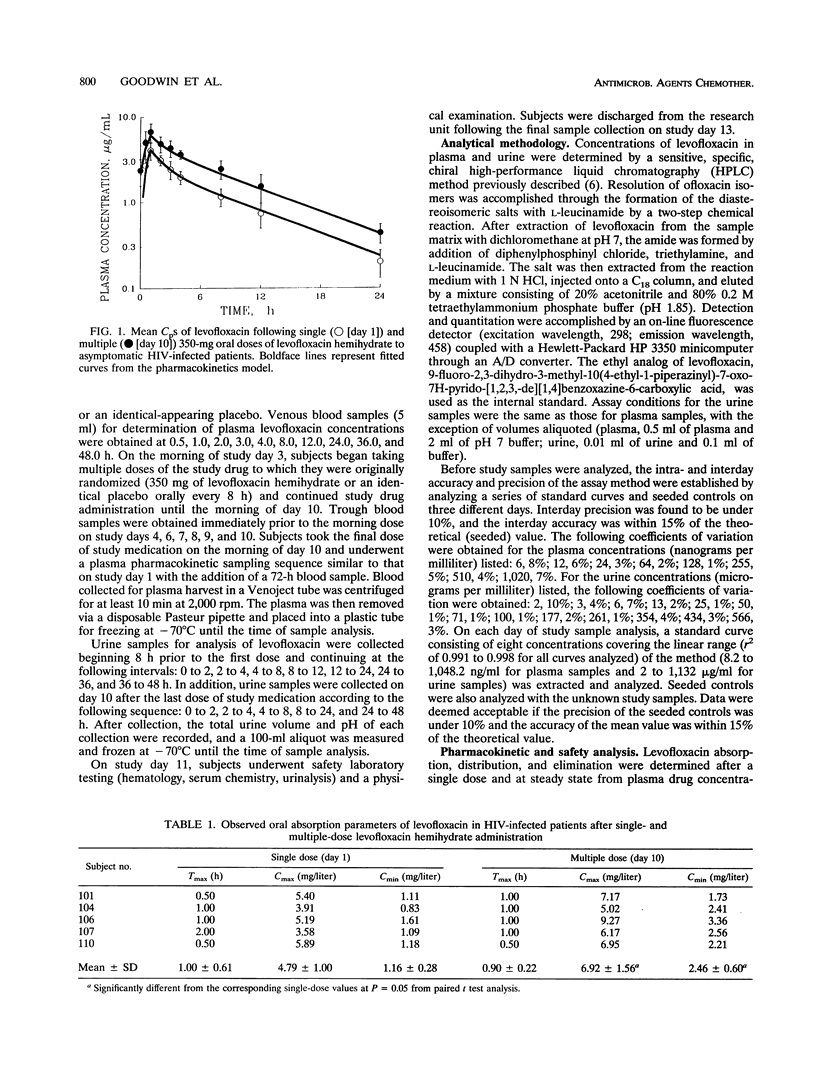
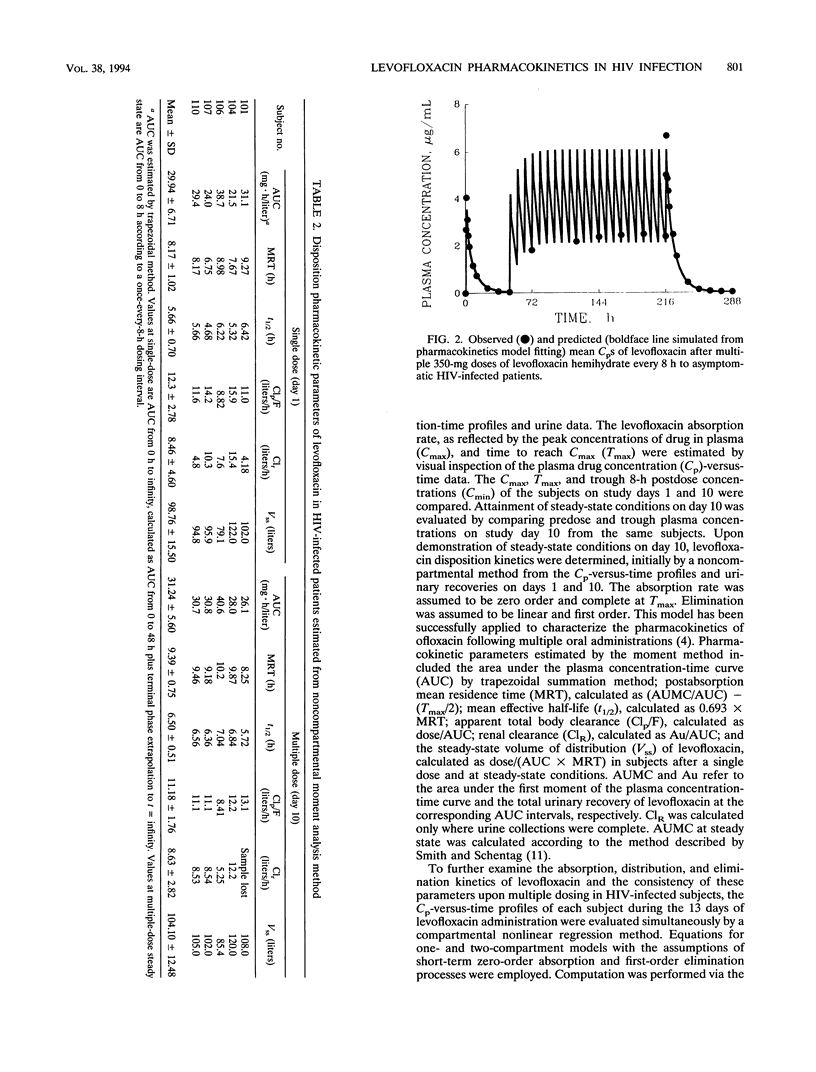
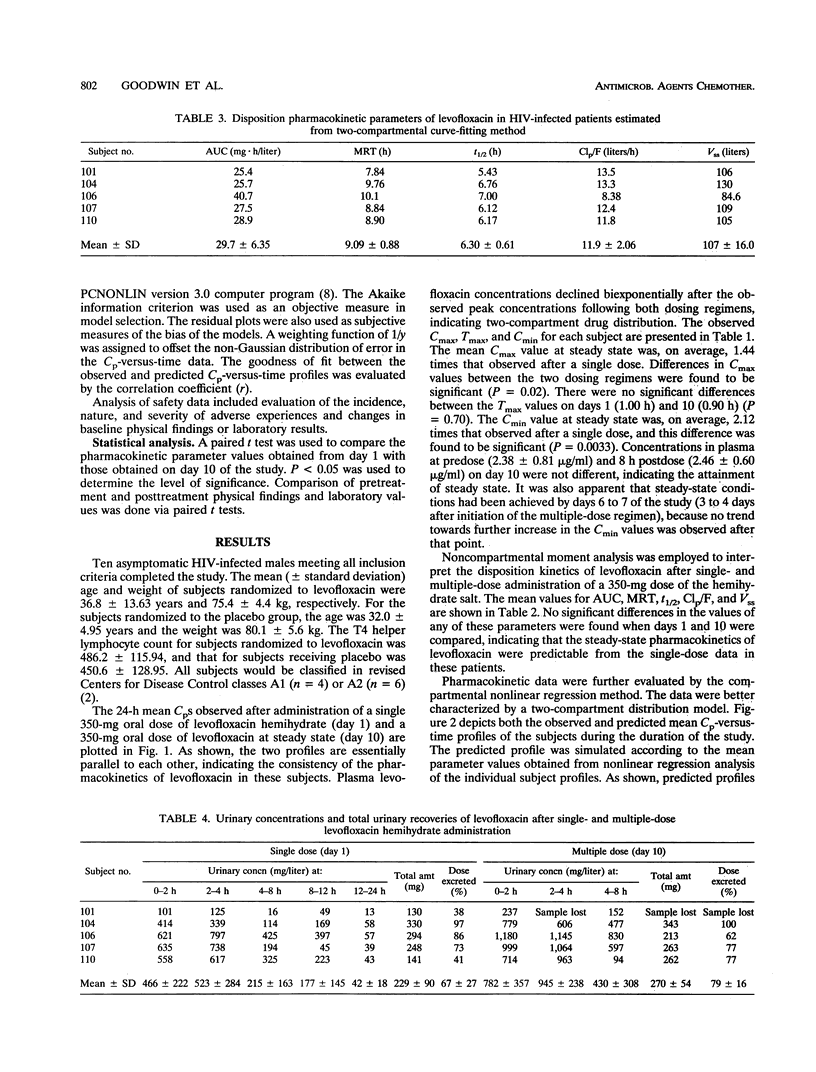
Levofloxacin, the bacteriologically active isomer of ofloxacin, has microbiologic activity against many pathogens common in human immunodeficiency virus (HIV)-infected patients, including Mycoplasma species which may be cofactors in the progression of HIV disease. The purpose of this phase I, double-blind, randomized (1:1), placebo-controlled trial was to evaluate the pharmacokinetics and safety of levofloxacin hemihydrate in 10 asymptomatic HIV-infected males. Plasma concentrations by chiral high-performance liquid chromatography (HPLC) were evaluated for 48 h after a single 350-mg oral dose, at morning predose during the multiple-dosing phase, and for 72 h at steady state after a week of 350 mg every 8 h orally. Mean +/- standard deviation levofloxacin pharmacokinetic parameters (by noncompartmental moment method) after multiple dosing were as follows: area under the concentration-time curve, 31.24 +/- 5.60 mg.h/liter; apparent total body clearance, 11.18 +/- 1.76 liters/h; renal clearance, 8.63 +/- 2.82 liters/h; steady-state volume of distribution, 104.10 +/- 12.48 liters; and effective half-life, 6.50 +/- 0.51 h. Single-dose parameters were not significantly different from the multiple-dose parameters, with the exception of peak concentrations in plasma, which were 4.79 +/- 1.00 and 6.92 +/- 1.56 mg/liter for single- and multiple-dose data, respectively. Essentially identical parameter values were obtained from curve-fitting analysis when the entire 13-day plasma concentration profiles of the subjects were analyzed simultaneously by a two-compartmental distribution model. Levofloxacin pharmacokinetics in HIV-infected patients remained linear upon multiple dosing. The dosing regimen studied provides levels in plasma and urine well above those found to be effective in vitro against pathogens common in HIV-infected patients. Levofloxacin was well- tolerated in this group of asymptomatic HIV-infected males: there were no statistically significant differences in adverse effects in the two groups (P = 0.22). Use of placebo control helped to differentiate disease-related adverse effects from those related to the study drug.
Full text
PDF


Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Flor S. C., Rogge M. C., Chow A. T. Bioequivalence of oral and intravenous ofloxacin after multiple-dose administration to healthy male volunteers. Antimicrob Agents Chemother. 1993 Jul;37(7):1468–1472. doi: 10.1128/aac.37.7.1468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flor S. Pharmacokinetics of ofloxacin. An overview. Am J Med. 1989 Dec 29;87(6C):24S–30S. [PubMed] [Google Scholar]
- Fu K. P., Lafredo S. C., Foleno B., Isaacson D. M., Barrett J. F., Tobia A. J., Rosenthale M. E. In vitro and in vivo antibacterial activities of levofloxacin (l-ofloxacin), an optically active ofloxacin. Antimicrob Agents Chemother. 1992 Apr;36(4):860–866. doi: 10.1128/aac.36.4.860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lehr K. H., Damm P. Quantification of the enantiomers of ofloxacin in biological fluids by high-performance liquid chromatography. J Chromatogr. 1988 Mar 4;425(1):153–161. doi: 10.1016/0378-4347(88)80015-x. [DOI] [PubMed] [Google Scholar]
- Lo S. C., Dawson M. S., Wong D. M., Newton P. B., 3rd, Sonoda M. A., Engler W. F., Wang R. Y., Shih J. W., Alter H. J., Wear D. J. Identification of Mycoplasma incognitus infection in patients with AIDS: an immunohistochemical, in situ hybridization and ultrastructural study. Am J Trop Med Hyg. 1989 Nov;41(5):601–616. doi: 10.4269/ajtmh.1989.41.601. [DOI] [PubMed] [Google Scholar]
- Nozaki-Renard J., Iino T., Sato Y., Marumoto Y., Ohta G., Furusawa M. A fluoroquinolone (DR-3355) protects human lymphocyte cell lines from HIV-1-induced cytotoxicity. AIDS. 1990 Dec;4(12):1283–1286. doi: 10.1097/00002030-199012000-00018. [DOI] [PubMed] [Google Scholar]
- Smith I. L., Schentag J. J. Noncompartmental determination of the steady-state volume of distribution during multiple dosing. J Pharm Sci. 1984 Feb;73(2):281–282. doi: 10.1002/jps.2600730239. [DOI] [PubMed] [Google Scholar]
- Volberding P. A., Lagakos S. W., Koch M. A., Pettinelli C., Myers M. W., Booth D. K., Balfour H. H., Jr, Reichman R. C., Bartlett J. A., Hirsch M. S. Zidovudine in asymptomatic human immunodeficiency virus infection. A controlled trial in persons with fewer than 500 CD4-positive cells per cubic millimeter. The AIDS Clinical Trials Group of the National Institute of Allergy and Infectious Diseases. N Engl J Med. 1990 Apr 5;322(14):941–949. doi: 10.1056/NEJM199004053221401. [DOI] [PubMed] [Google Scholar]



