Abstract
Background
Since loss of height may indicate vertebral fracture, the accuracy of the information on height is relevant for clinical practice. We undertook this study to compare reported and measured loss of height among post-menopausal women in a primary care setting. We also analyzed the determinants of this height loss.
Methods
In an observational study conducted between December 2007 and May 2008, we asked 1779 randomly selected general practitioners to recruit the first five female patients who were more than 60 years of age, regardless of the reason for the consultation. Using a questionnaire, physicians collected data on demographic and clinical variables, history of osteoporosis and current anti-osteoporotic treatment. We used three assessments of height: tallest height in early adulthood recalled by the patient, estimated current height reported by the patient at the visit and current measured height. We defined loss of height as the difference between the patient’s tallest recalled height and her current measured height.
Results
A total of 8610 patients were included in the analysis; the mean age was 70.9 (standard deviation [SD] 7.2) years. The mean loss of height was 4.5 cm. The mean current reported height was 2.1 (SD 2.5) cm lower than the tallest recalled height and 2.4 (SD 2.6) cm lower than the measured current height. The best predictors of a loss of height of 3 cm or more were age (odds ratio [OR] 1.09, 95% confidence interval [CI] 1.08–1.10), previous vertebral fracture (OR 1.49, 95% CI 1.16–1.91), previous nonvertebral fracture (OR 1.26, 95% CI 1.06–1.51), thoracic kyphosis (OR 2.07, 95% CI 1.69–2.55), scoliosis (OR 1.35, 95% CI 1.12–1.63), back pain (OR 1.22, 95% CI 1.07–1.39) and osteoporosis (OR 1.39, 95% CI 1.20–1.60).
Interpretation
Our study showed that the patients’ estimated current height was not correct, with a mean difference of −2.5 cm from the current measured height. The mean height loss was 4.5 cm. Previous vertebral fracture and thoracic kyphosis were strong determinants of the height loss.
Loss of height is common with advancing age.1,2 Causes include changes in curvature of the spine, narrowing of intervertebral discs and vertebral fractures. Height loss is associated with back pain and thoracic hyperkyphosis.3,4 Two-thirds of adults have back pain at any time. Controversies exist about the need for radiographs of the spine: Does the benefit of detecting treatable disorders of the spine such as vertebral fracture outweigh the harm of unnecessary radiographs? Loss of height is usually recorded as one of the clinical signs to help identify postmenopausal women with vertebral fractures.5 The use of this parameter to decide whether radiography is needed depends on the threshold for height loss associated with a strong risk of vertebral fracture. The thresholds useful in clinical practice to detect prevalent vertebral fracture range from 3 cm to 6 cm,6–9 with the risk of prevalent fracture increasing with the magnitude of the height loss. Thus, the accuracy of the information on height is relevant for clinical practice.
We conducted this study to compare reported and measured loss of height in a large population of women more than 60 years old in a primary care setting and to analyze the determinants of this height loss.
Methods
Study design
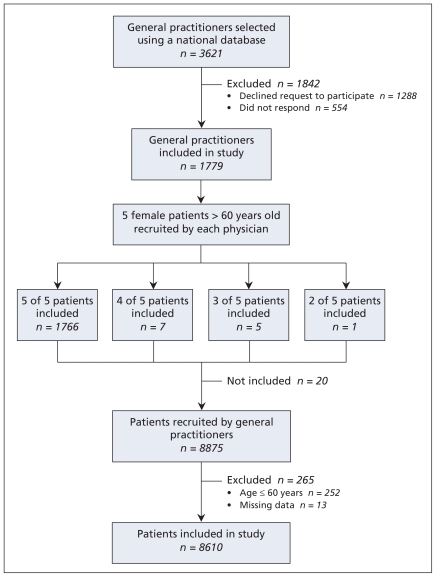
We conducted a multicentred observational study between December 2007 and May 2008 at primary care practices in France. We randomly selected general practitioners from a national representative database. To be eligible, physicians had to have a large practice that included women more than 60 years old. We estimated that the sample would need to include at least 3500 general practitioners. We selected 3621 general practitioners and contacted them by phone; 1779 agreed to participate (Figure 1).
Figure 1.
Recruitment of the general practitioners and patients.
The general practitioners were asked to recruit the first five female patients who were more than 60 years of age, regardless of the reason for the consultation. During the visit, the physicians completed a questionnaire with the following information: patient’s age, weight, start of menopause, history of fracture after age 45 years, history of spinal disease such as osteoarthritis, history of back pain, past or current intake or corticosteroids for three or more months, history of osteoporosis and current use of anti-osteoporosis treatment. They checked the patients’ charts to see whether bone densitometry had been performed; the diagnosis of osteoporosis was defined by a T score of −2.5 or less.
The physicians were also asked to review the recruited patients’ files to see if they had had any radiographs of the spine performed. They checked the radiographs or the radiologists’ reports in the files for data on the presence or absence of vertebral fractures, scoliosis, thoracic kyphosis or osteoarthritis of the spine.
Measurement of loss of height
We used three assessments of height in this study: tallest recalled height, current reported height and current measured height. The tallest recalled height was obtained using either the height recorded on documentation (passport, national identity card) between 20 and 50 years of age or the tallest height at 20 years of age recalled by the patient.
Current reported height was the estimated current height reported by the patient at the visit before any measurement.
Current measured height was measured with the use of an electronic stadiometer. Each patient was measured without shoes, with her heels, buttocks and back to the stadiometer backboard. The patient’s head was maintained in the Frank-fort plane, with the lower edge of the left eye socket in the same horizontal plane as the notch superior to the tragus of the left ear.10,11 The patient was instructed to stretch to a fully erect position while keeping her feet flat on the floor. Height was recorded to the closest millimetre during normal respiration.10,11 Three consecutive measurements were obtained, and the mean was recorded.
Statistical analysis
We used means and standard deviations (SDs) for continuous variables and percentage distributions for discrete variables. Means were compared with use of the Mann–Whitney and Kruskal–Wallis tests. Loss of height was defined as the difference between the patient’s tallest recalled height and the current measured height.
We performed logistic regression analysis to determine predictive factors of height loss among patients who had a loss of height of at least 3 cm (v. < 3 cm) and among those who had a loss of height of at least 6 cm (v. < 6 cm). As an exploratory analysis, we used information from the radiologists’ reports, where available in the women’s files, to study the relation between height loss and risk of vertebral fracture. We performed sensitivity and specificity analyses to determine the threshold for height loss to use in the multivariable analysis.
Results
Patient characteristics
A total of 8875 postmenopausal women were recruited by the general practitioners; we excluded 265 (3.0%) of them because of missing data concerning their age or because they were 60 years of age or younger.
The baseline characteristics of the remaining 8610 women are reported in Table 1. Overall, 2391 (27.8%) of the patients reported a history of clinical fracture after age 45 years (13.1% reported a wrist fracture, 9.2% a vertebral fracture, 2.3% a hip fracture and 7.4% another“other” fracture). Of the 4238 patients who had undergone bone densitometry, 1938 (45.7%) had osteoporosis. Overall, 2936 (34.1%) of the 8610 patients were receiving at least one anti-osteoporosis agent (bisphosphonate, parathyroid hormone, selective estrogen receptor modulator or strontium ranelate); this proportion was 38.3% (n = 1609) among the 4201 women who were more than 70 years old.
Table 1.
Characteristics of 8610 female patients more than 60 years of age who were included in the study
| Characteristic | Value |
|---|---|
| Age, yr, mean (SD) | 70.9 (7.2) |
| Age at start of menopause, yr, mean (SD) | 50.0 (4.2) |
| Weight, kg, mean (SD) | 65.8 (11.9) |
| Body mass index, mean (SD) | 26.6 (4.7) |
| Previous or current use of corticosteroids for ≥ 3 mo, % (no.) | 5.3 (446/8483) |
| History of clinical fracture after age 45 years, % (no.) | 27.8 (2391/8610) |
| Wrist | 13.1 (1129/8610) |
| Vertebra | 9.2 (796/8610) |
| Hip | 2.3 (200/8610) |
| Other | 7.4 (634/8610) |
| Finding on radiograph, % (no.) | |
| Vertebral fracture | 12.7 (973/7683) |
| Scoliosis | 23.1 (1753/7604) |
| Thoracic kyphosis | 24.2 (1836/7582) |
| Osteoporosis,* % (no.) | 45.7 (1938/4238) |
| ≥ 1 anti-osteoporosis agent,† % (no.) | 34.1 (2936/8610) |
Note: SD = standard deviation.
T score ≤ −2.5.
Bisphosphonate, parathyroid hormone, selective estrogen receptor modulator or strontium ranelate.
Radiographs of the spine were available in the files of 5179 (60.2%) of the recruited patients. They were performed within one year before the visit for 1819 (35.1%) and more than one year before the visit for 3360 (64.9%). The radiograph or radiologist’s report showed clinical vertebral fracture in 12.7% (973/7683) patients, scoliosis in 23.1% (1753/7604), thoracic kyphosis in 24.2% (1836/7582) and osteoarthritis of the spine in 50.9% (3835/7534).
Height loss
The different height values are presented in Table 2. The tallest recalled height was estimated at the mean age of 20.7 (SD 4.0) years, on the basis of documentation (passports, identity card) in 4.4% and the patient’s memory of height attained in young adulthood in 95.6%. The mean estimated current height reported by the women the day of the visit was significantly lower than the mean tallest recalled height at age 20 (difference −2.1 [SD 2.5] cm) and the mean measured height (difference −2.4 [SD 2.6] cm) (Table 2).
Table 2.
Measurements of height
| Variable | Mean (SD) |
|---|---|
| Age at tallest recalled height, yr | 20.7 (4.0) |
| Age at visit, yr | 70.9 (7.2) |
| Tallest recalled height, cm | 162.0 (5.9) |
| Current height reported by patient, cm | 160.0 (6.1) |
| Current measured height, cm | 157.5 (6.5) |
| Height lost,* cm | 4.5 (3.0) |
Note: SD = standard deviation.
Loss of height was defined as the difference between the patient’s tallest recalled height and the current measured height.
The mean height lost was 4.5 (SD 3.0) cm. Overall, 165 (2.0%) of the patients did not lose any height, 5843 (70.9%) had a loss of at least 3 cm, and 2239 (27.1%) had a loss of at least 6 cm; the remaining 363 patients had a loss of less than 3 cm.
The mean loss of height was 4.8 cm (SD 3.0) among the patients who were taking anti-osteoporosis treatment and 4.3 cm (SD 2.9) among those not taking such treatment (p < 0.001).
Determinants of height loss
The multivariable analysis showed that the best predictors of a loss of height of 3 cm or more were age, previous vertebral fracture, previous nonvertebral fracture, thoracic kyphosis, scoliosis, back pain and osteoporosis. The best determinants of a loss of 6 cm or more were age, previous vertebral fracture, previous nonvertebral fracture, thoracic kyphosis and scoliosis (Table 3).
Table 3.
Factors associated with loss of height of 3 cm or more (n = 5660)
| Variable | Loss of height; adjusted OR* (CI 95%) | |
|---|---|---|
| ≥ 3 cm | ≥ 6 cm | |
| Age at visit | 1.09 (1.08–1.10) | 1.09 (1.08–1.10) |
| Age at start of menopause | 0.98 (0.97–1.00) | – |
| Back pain | 1.22 (1.07–1.39) | – |
| Previous vertebral fracture | 1.49 (1.16–1.91) | 1.80 (1.49–2.19) |
| Previous clinical fracture | 1.26 (1.06–1.51) | 1.13 (1.49–2.19) |
| Scoliosis | 1.35 (1.12–1.63) | 1.15 (0.94–1.39) |
| Thoracic kyphosis | 2.07 (1.69–2.55) | 1.90 (1.60–2.27) |
| Osteoporosis† | 1.39 (1.20–1.60) | – |
Note: CI = confidence interval, OR = odds ratio.
Each variable was adjusted for the other variables in the table.
T score ≤ −2.5.
Relation between height loss and vertebral fracture
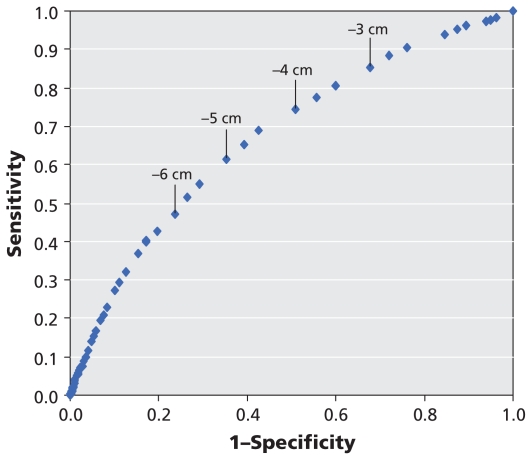
Of the 6713 patients whose general practitioner could determine the presence or absence of a vertebral fracture from the radiograph or radiologic report, 973 (14.5%) had a vertebral fracture. Compared with patients who did not have a vertebral fracture, those who did were significantly older (mean 74.4 [SD 7.4] v. 70.2 [SD 6.9] years), shorter (mean 155.9 [SD 7.1] v. 157.8 [SD 6.3] cm), thinner (mean 63.1 [SD 11.3] v. 66.1 [SD 11.8] kg) and lost more height (mean 6.1 [SD 3.4] v. 4.3 [SD 2.8] cm) (p < 0.001 for each comparison). They reported current use of corticosteroids, osteoporosis and previous non-vertebral fracture more often than the women without vertebral fractures. With respect to the presence of vertebral fracture on the radiologist’s report, a threshold of 4 cm of height loss had a sensitivity of 74% and a specificity of 49%; a threshold of 6 cm had a sensitivity of 47% and a specificity of 76% (Figure 2). Multivariable analysis using a threshold of height loss of at least 4 cm showed that the best predictors of the presence of vertebral fracture were age, a history of height loss of at least 4 cm, back pain and previous nonvertebral fracture.
Figure 2.
Sensitivity and specificity analysis (receiver operating characteristics curve) of the relation between loss of height and presence of vertebral fracture on the radiologic report.
Interpretation
We observed a mean loss of height of 4.5 cm since early adulthood in a large population of postmenopausal women in primary care practices. The patient’s estimated current height was not a correct assessment of this parameter. There was a significant difference (−2.1 cm) between the current height reported by the women during the visit and their tallest recalled height at age 20. Despite this “pessimistic” view, the estimated current height was wrong, with the measured height being actually 2.4 cm lower. The prevalence of vertebral fractures on radiologic reports was 12.7%. We found that the risk of existing vertebral fracture was significantly higher among patients with a height loss of at least 4 cm, a threshold similar to the one recommended by the International Society for Clinical Densitometry.7
Previous studies have shown that patients’ estimated current and recalled heights tend to be higher than measured heights and that the tallest recalled height may be overestimated.12,13 Overestimated height increased with age, occurring in 70% of those aged 80 and older. Compared with people with normal bone density, a significantly higher proportion of men with osteoporosis (76% v. 47%, p < 0.001) and women with osteoporosis (52% v. 35%, p < 0.001) overestimated their height. In addition, significant misclassification of self-reported height and weight occurred among people in poor health and those with poor performances on memory and calculation tests.14,15 However, previous studies did not show that the reported current height was lower than the tallest recalled height. Our finding of a difference of −2.1 cm between these values was surprising, because the patients had just given their tallest recalled height. A previous study showed that women who consulted in primary health care increased the severity of their complaint and had a pessimistic appraisal of their health.16
Loss of height may occur for several reasons, such as postural change, degenerative intervertebral disc disease or vertebral fracture. In a population-based study of the incidence of clinical vertebral fracture, only 30% of women who had a vertebral fracture visited a health care provider with symptomatic complaints.17 Measurement of height loss could be an accurate method for detecting prevalent vertebral fractures; however, there are discrepancies concerning the relevant threshold for height loss.18,19 In a study involving 322 post-menopausal women with osteoporosis, Siminosky and colleagues showed that a loss of height greater than 6.0 cm rules in prevalent vertebral fracture and proposed that patients with a loss of at least 6 cm should have a radiograph taken.9 In a population-based, retrospective study, Gunnes and colleagues found that the risk of vertebral fracture increased about five-fold among women who had a loss of at least 3 cm in height compared with those who had maintained height.6
The differences in thresholds may be explained by the differences in the patients’ characteristics and the type of recruitment (primary care setting or not). The high prevalence of height loss in our study population contrasts with the low prevalence of vertebral fracture, which suggests that height loss is not fully explained by the presence of vertebral fractures. Siminovski and colleagues showed that the average height loss per vertebral fracture is 0.97 cm,9 which suggests that height loss is linked not only to vertebral fractures. In our study, age, thoracic kyphosis and scoliosis were other strong determinants of height loss.
Limitations
Our study had several limitations. Although it was performed in a nonspecialist setting and involved women who were not referred for osteoporosis assessment, the proportion of patients who had osteoporosis or were taking anti-osteoporosis treatment was higher than expected. We can hypothesize that only general practitioners most interested in osteoporosis agreed to participate or that, by knowing the purpose of the study, the physicians preferentially included patients with osteoporosis. Prevalent vertebral fractures were assessed by the general practitioners after reviewing the radiographs or radiologic reports, and we were unable to confirm the diagnosis of fractures. It has been shown that up to 20% of fractures may not be recognized, in part because of an ambiguous radiologic report.20 With the proportion of missing data at less than 5%, we considered that our choice of method would not significantly alter the results.
Conclusion
In this observational study involving a large population of postmenopausal women more than 60 years old, we observed that the estimated current height reported by the women was incorrect, with a mean difference of −2.4 cm from the current measured height. Thus, general practitioners need to measure the height of their postmenopausal patients and not rely on reported estimates. Previous vertebral fracture and thoracic kyphosis were strong determinants of the height loss.
Footnotes
Funding: This study was conducted with an unrestricted grant from Merck. Merck had no role in the design of the study, the collection, analysis or interpretation of data, the writing of the report or the decision to submit the article for publication.
Previously published at www.cmaj.ca
Competing interests: Christian Roux and Erik Legrand received honoraria from Merck for participating in this study. No competing interests declared by Karine Briot, Denis Pouchain or Stéphanie Monnier. Stéphanie Monnier is employed at ABR Pharma, the contract research organization in charge of the implementation and operational follow-up of the study, the data management and the statistical analysis.
Contributors: Christian Roux, Erik Legrand and Denis Pouchain contributed to the study concept and design. Stéphanie Monnier was involved in the collection and assembly of data. All of the authors contributed to the analysis and interpretation of data. Karine Briot and Christian Roux drafted the manuscript. All of the authors revised the manuscript for important intellectual content and approved the final version submitted for publication.
This article has been peer reviewed.
REFERENCES
- 1.Kado DM, Huang MH, Karlamangla AS, et al. Hyperkyphotic posture predicts mortality in older community-dwelling men and women: a prospective study. J Am Geriatr Soc. 2004;52:1662–7. doi: 10.1111/j.1532-5415.2004.52458.x. [DOI] [PubMed] [Google Scholar]
- 2.Takahashi T, Ishida K, Hirose D, et al. Trunk deformity is associated with a reduction in outdoor activities of daily living and life satisfaction in community-dwelling older people. Osteoporos Int. 2005;16:273–9. doi: 10.1007/s00198-004-1669-3. [DOI] [PubMed] [Google Scholar]
- 3.Roux C, Briot K, Kolta S, et al. Thoracic kyphosis index as a risk factor for incident vertebral fractures and alteration of quality of life in postmenopausal women with osteoporosis. J Bone Miner Res. 2009:S38. [Google Scholar]
- 4.Spector TD, McCloskey EV, Doyle DV, et al. Prevalence of vertebral fracture in women and the relationship with bone density and symptoms: the Hingford Study. J Bone Miner Res. 1993;8:817–22. doi: 10.1002/jbmr.5650080707. [DOI] [PubMed] [Google Scholar]
- 5.Kaptoge S, Armbrecht G, Felsenberg D, et al. EPOS Study Group. When should the doctor order a spine x-ray? Identifying vertebral fractures for osteoporosis care: results from the European Prospective Osteoporosis Study (EPOS) J Bone Miner Res. 2004;19:1982–93. doi: 10.1359/JBMR.040901. [DOI] [PubMed] [Google Scholar]
- 6.Gunnes M, Lehmann EH, Mellstrom D, et al. The relationship between anthropometric measurements and fractures in women. Bone. 1996;19:407–13. doi: 10.1016/s8756-3282(96)00196-2. [DOI] [PubMed] [Google Scholar]
- 7.Vokes T, Bachman D, Baim S, et al. Vertebral fracture assessment: the 2005 ISCD official positions. J Clin Densitom. 2006;9:37–46. doi: 10.1016/j.jocd.2006.05.006. [DOI] [PubMed] [Google Scholar]
- 8.Krege JH, Siminoski K, Adachi JD, et al. A simple method for determining the probability a new vertebral fracture is present in postmenopausal women with osteoporosis. Osteoporos Int. 2006;17:379–86. doi: 10.1007/s00198-005-2005-2. [DOI] [PubMed] [Google Scholar]
- 9.Siminoski K, Jiang G, Adachi JD, et al. The accuracy of height loss during prospective monitoring for detection of incident vertebral fractures. Osteoporos Int. 2005;16:403–10. doi: 10.1007/s00198-004-1709-z. [DOI] [PubMed] [Google Scholar]
- 10.Norton K, Whittingham N, Carter L, et al. Measurement techniques in anthropometry. In: Norton K, Olds T, editors. Anthropometrica. Sydney (Australia): University of New South Wales Press; 1996. pp. 25–75. [Google Scholar]
- 11.Coles RJ, Clements DG, Evans WD. Measurements of height: practical considera-tions for the study of osteoporosis. Osteoporos Int. 1994;4:353–6. doi: 10.1007/BF01622197. [DOI] [PubMed] [Google Scholar]
- 12.Cline MG, Merdith KE, Boyer JT, et al. Decline of height with age in adults in a general population sample: estimating maximum height and distinguishing birth cohort effects from actual loss of stature with aging. Hum Biol. 1989;61:415–25. [PubMed] [Google Scholar]
- 13.Chandler PJ, Bock RD. Age changes in adult stature: trend estimation from mixed longitudinal data. Ann Hum Biol. 1991;18:433–40. doi: 10.1080/03014469100001732. [DOI] [PubMed] [Google Scholar]
- 14.Sahyoun NR, Maynard LM, Zhang XL, et al. Factors associated with errors in self-reported height and weight in older adults. J Nutr Health Aging. 2008;12:108–15. doi: 10.1007/BF02982562. [DOI] [PubMed] [Google Scholar]
- 15.Kuczmarski MF, Kuczmarski RJ, Najjar M. Effects of age on validity of self-reported height, weight, and body mass index: findings from the Third National Health and Nutrition Examination Survey, 1988–1994. J Am Diet Assoc. 2001;101:28–34. doi: 10.1016/S0002-8223(01)00008-6. [DOI] [PubMed] [Google Scholar]
- 16.Laakso V, Niemi PM, Grönroos M, et al. The worried young adult as a primary care patient. Fam Pract. 2005;22:406–11. doi: 10.1093/fampra/cmi038. [DOI] [PubMed] [Google Scholar]
- 17.Cooper C, Atkinson EJ, O’Fallon WM, et al. Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985–1989. J Bone Miner Res. 1992;7:221–7. doi: 10.1002/jbmr.5650070214. [DOI] [PubMed] [Google Scholar]
- 18.Tobias JH, Hutchinson AP, Hunt LP, et al. Use of clinical risk factors to identify postmenopausal women with vertebral fractures. Osteoporos Int. 2007;18:35–43. doi: 10.1007/s00198-006-0209-8. [DOI] [PubMed] [Google Scholar]
- 19.Roux C, Priol G, Fechtenbaum J, et al. A clinical tool to determine the necessity of spine radiography in postmenopausal women with osteoporosis presenting with back pain. Ann Rheum Dis. 2007;66:81–5. doi: 10.1136/ard.2006.051474. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Delmas PD, van de Langerijt L, Watts NB, et al. IMPACT Study Group. Under-diagnosis of vertebral fractures is a worldwide problem: the IMPACT study. J Bone Miner Res. 2005;20:557–63. doi: 10.1359/JBMR.041214. [DOI] [PubMed] [Google Scholar]