Abstract
Few recent publications have highlighted theoretical and methodological challenges using respondent-driven sampling (RDS). To explore why recruitment with RDS may work in some populations and not in others, we assess the implementation of RDS to recruit female sex workers (FSWs) and injection drug users (IDUs) into a human immunodeficiency virus biological and risk behavior survey in Tallinn, Estonia. Recruitment of FSWs was slower and more challenging than that of IDUs. The IDU study recruited 350 participants within 7 weeks, while the FSW study recruited 227 participants over 28 weeks. Implementation modifications that did not negatively impact key RDS theoretical and methodological requirements were used to improve recruitment during the FSW study. We recommend that all RDS studies include a formative research process to involve the participation of target populations and key persons associated with these populations in the study planning and throughout the implementation processes to improve recruitment from the outset and to respond to poor recruitment during data collection.
Keywords: Injecting drug users, Female sex workers, Respondent-driven sampling, HIV, Estonia
Introduction
Monitoring the course of the human immunodeficiency virus (HIV) epidemic among injecting drug users (IDUs) and sex workers (SWs) is essential for developing appropriate and effective interventions, shaping policy, and estimating future spread. However, few sampling strategies are available for gathering reliable and generalizable data from these hidden and highly marginalized populations.1,2 Over the past several years, public health researchers have experimented with a variant of chain-referral sampling known as respondent-driven sampling (RDS) to assess HIV prevalence and associated risk behavior data of IDUs and SWs.
RDS relies on peers to recruit their peers from within their social networks, thereby encouraging participation by individuals that are not easily accessed through other types of sampling methods. Long recruitment chains encourage the participation of less visible participants as well as those who are not exposed to services and outreach programs. Through the collection of participants’ social network sizes and recruitment patterns, RDS data can be analyzed to provide representative estimates and confidence intervals.3,4
From 2005-2007 in Tallinn, the capital city of Estonia, surveillance studies on HIV prevalence and sexual risk behaviors among female SWs (FSWs) and IDUs using RDS were carried out. Both FSWs and IDUs are important high risk groups impacting the course of the HIV epidemic in Estonia.5 Current data show that the HIV epidemic in Estonia is driven mostly by the use of non-sterile injection equipment and that approximately 4.3% of the population, aged 15-44 years, in the capital region inject drugs.6 HIV among IDUs is estimated to be around 50%,7–9 and incidence is estimated at >20/100 person years at risk.10 IDUs in Tallinn tend to be well networked through buying, selling, and injecting activities (Des Jarlais DC, unpublished data).
Compared to IDUs, little research has been conducted among FSWs in Estonia. FSWs, mostly concentrated in the capital, Tallinn, have an estimated HIV prevalence of 7.6% 11 and tend to work in a hierarchy of locations ranging from elite brothels and “love flats” to truck stops. Cellular phone and internet technology enables sex work to be highly dispersed and spatially mobile.12
This paper examines the implementation of RDS methodology in two separate subpopulations: FSWs and IDUs. We evaluate and compare recruitment efficiency and sampling challenges, as well as provide findings and recommendations from both studies. The findings from this evaluation should assist researchers in understanding some barriers to successful RDS recruitment.
Methods
Participants
Two studies designed to assess HIV prevalence and associated risk behaviors among current FSWs and IDUs were conducted using RDS methods from 2005 to 2007 (Table 1). Formative research was conducted to plan study logistics and to assess the target population’s interest. The methodology included interviews with gatekeepers (three among the FSW group, and two among the IDU group), members of the target population (three among FSWs, five among IDUs), mapping, and piloting data collection instruments. We gathered information to identify individual seeds, refine logistical issues (proper incentive amount, interview locations, hours and days for interviews), and develop materials.
Table 1.
Description of the female sex worker (FSW) and injecting drug user (IDU) study designs incorporating formative research results, Tallinn, Estonia
| FSW STUDY | IDU STUDY | |
|---|---|---|
| Target population | Current FSW (a person reporting exchanging sex for money, drugs, or goods within the past 3 months) | Current IDU (a person reporting injecting drugs within the past 2 months) |
| Eligibility criteria | Females, 18 years or older, exchanged sex for money, drugs or goods | Male or female, 18 years or older, reported injecting drugs |
| Place, time (year of data collection) | Tallinn 2005-2006 | Tallinn 2007 |
| Aim of the study | Estimating HIV and risk behavior prevalence | Estimating HIV and risk behavior prevalence |
| Questionnaire adapted from: | Shakarshvili A et al. 200519 | DesJarlais DC et al. 200620 |
| Biological samples for HIV testing | Venous blood (serum; the first 16 study participants), oral fluid specimens for the remainder a | Venous blood (serum)b |
| Recruitment method | RDS | RDS |
| Number of seeds and diversification of seeds | Six seeds representing diverse subgroups of FSWs (e.g., ethnicity, age, and sex work venue); 37 extra seeds were enrolled during data collection | Five seeds representing diverse subgroups of IDUs (e.g., ethnicity, gender, injection drug type used, and age) |
| Primary incentive (for study participation) | Gift coupon for department store valued at 10 USD; free STI/HIV check-up and gynecological consultation | Gift coupon for grocery store valued at 10 USD |
| Secondary incentive (for recruiting peers) | Gift coupon for department store valued at 10 USD | Gift coupon for grocery store valued at 5 USD |
| The study site | ||
| Setting | SW counseling center, NGO, at home, or place of their choosing | SEP, NGO Convictus |
| Location | Central, or place of their choosing | Central |
| Days and hours of operation | M, F 15.00-19.00 | M, T, W, Th, F |
| T, W, Th 12.00-19.00 | 10.00-14.00 | |
aVenous blood collected from the first 16 participants was tested with HIV-1/HIV-2 III plus from Abbott Laboratories (Abbott Park, Illinois, USA). The remaining participants were tested using oral fluid specimens with an OraSure device (Epitope Inc., Oregon, USA). Duplicates were screened using Vironostica HIV Uni-Form II plus 0 (BioMerieux, Boxtel, Netherlands),21 and confirmatory testing was conducted on initially reactive specimens using Western blot assay (New LAV Blot I, Bio-Rad, Marnes la Coquette, France)
bVenous blood was collected and tested with HIV-1/HIV-2 III plus from Abbott Laboratories (Abbott Park, Illinois, USA)
As in all RDS studies, recruitment began with a set number of non-randomly selected seeds representing diverse types of FSWs and IDUs. Eligible participants were provided coupons for recruiting three of their peers (either FSWs or IDUs). Coupons were uniquely coded to link participants to their survey responses and biological specimens and for monitoring who recruited whom. Participants who completed the study received a primary incentive for study participation and a secondary incentive for each eligible recruit who enrolled into the study (Table 1).
IDUs were offered pre- and post-test HIV counseling along with their test result. FSWs were referred to a conveniently located dedicated medical center for HIV counseling and testing and free sexually transmitted infections (STI; syphilis, chlamydia, gonorrhea, and trichomoniasis) testing, results and, if appropriate, treatment.
Measures
Both studies used a structured questionnaire administered by trained interviewers to inquire about socio-demographic characteristics, sex work/drug use history, HIV sexual-risk behaviors, and harm reduction service utilization.
To measure social network sizes, FSWs were asked, “How many FSWs do you know personally and have seen within last 3 months?” IDUs were asked, “How many IDUs do you know personally and have seen within last 6 months?” We also asked questions about each participant’s recruiter (how would you describe your relationship to the person who referred you to this study, that is, the person who gave you this coupon?) to assess whether participants recruited known people (those in their social network) or strangers. RDS requires that the probability of selection be based on recruitment within social networks (known persons) and that the sample forms one complete social network component.13
Data Analysis
Qualitative data on recruitment progress and sampling challenges were collected through interviewers and site supervisors’ field notes taken during data collection.
Groups were compared by using risk ratios with 95% confidence intervals (CI) and exact tests to guide interpretation. A proportional odds ordinal logistic regression model was used to assess the association between network size and the number of recruits.
RDS Analysis Tool v. 6.0.1 14 was used to weigh the sample to control for differences in recruitment patterns and network sizes. Recruitment biases were explored in both samples using the respondent-driven sampling analysis tool (RDSAT) to adjust for differences in network size and for homophily (the extent to which recruiters are likely to recruit individuals similar to themselves) in order to provide population-based estimates of the study population characteristics.
A homophily index of H = 1.0 reflects 100% homophily for a specific characteristic, indicating that all recruitment ties are formed with other members having the same value on the characteristic. In contrast, H = −1.0 reflects 100% heterophily, indicating that all recruitment ties are formed with members having the opposite value on the characteristic.15 RDS assumes that participants recruit randomly from the population within their social networks, so high positive or negative homophily could be an indication that a sample does not form one complete social network component.
RDSAT was also used to estimate whether equilibrium was reached on key variables and the number of waves needed for each variable to reach equilibrium. Equilibrium is a statistic that provides evidence that the final sample is independent of the non-randomly selected seeds.15 The key variables used to assess equilibrium were age, ethnicity, gender, and HIV status.
Results
Studies’ Participants
Final sample sizes were 227 FSWs and 350 IDUs. Sixteen percent of IDUs (56/350) were females. HIV prevalence was substantially higher among IDUs than among FSWs (8% vs. 55%, OR = 0.14, 95% CI: 0.08-0.21, Fisher’s exact test p < 0.001). A lower percentage of FSWs compared to IDUs reported 9 years or less of formal education (30% vs. 53%, OR = 0.56, 95% CI: 0.44-0.69, Fisher’s exact test p < 0.001). The proportion of Russian speakers was 85% in both samples.
Five IDUs (1% of subjects or one male and four females) reported providing commercial sex services within the last 6 months. The four female IDUs reported engaging in commercial sex among whom three reported always using condoms with paying partners. Of the FSWs, 77% reported always using condoms with paying clients.
Low percentages of FSWs reported current (within the last 4 weeks) non-injection drug use (23%) and injection drug use (n=15, 6.6%). Among the FSWs who reported injecting drugs in the previous month, 11 (73%) reported not sharing needles and other injection equipment within the previous month. Sharing needles and other injection equipment within the previous month was reported by the 25% of IDUs.
Practical Experiences Using RDS among FSWs and IDUs
Description of the study designs incorporating formative research results are provided in Table 1. Seeds for both studies were contacted through service organizations (SW counseling center/syringe exchange program [SEP] outreach workers). During the eighth week into the study, FSW recruitment slowed significantly, which resulted in the addition of more seeds to increase recruitment. New seeds were selected through (1) contacts made by telephone with FSWs from brothels, apartments, saunas, and massage parlors advertised in newspapers/erotic magazines/through Internet enlisted in a process of spatial mapping; (2) community FSW contacts by field workers; and (3) contacts with night club, bar, and street-based FSWs approached directly during weekly field outreach visits. Field staff learned that many FSWs did not want to travel to the centrally located interview site. In response, we began conducting interviews in a location preferred by FSW participants such as at their workplace (e.g., apartment, brothel) or at a public location (e.g., cafeteria). In addition, we modified the biological sample collection from venous blood to oral fluid to comply with legal restrictions that prohibited the collection of blood outside of health facilities.
The type and value of the incentive was refined during formative research. Although both IDUs and FSWs preferred cash incentives, we were unable to use cash money due to local regulations. Additional limits for incentives were set by ethical considerations and the study budget. For IDUs, the primary (worth 10 USD) and secondary (worth 5 USD) incentives consisted of vouchers for purchases at a local grocery store.
Finding suitable incentives for FSWs was more challenging. Formative research indicated that FSWs were interested in receiving monetary incentives above what the study budget could afford. As an alternative, FSWs reported that they were interested in an incentive consisting of a free and prescheduled visit to a gynecologist which included HIV and STI testing together with reproductive counseling. In addition, FSWs received a gift card (worth 10 USD for the primary incentive and 10 USD for the secondary incentive) for redemption at the central department store to compensate their time and travel costs.
FSWs reported preferring afternoon hours rather than evening or morning hours for study participation. Although most IDUs had no time preferences for study participation, some mentioned preferring late evenings. However, we decided not to offer evening enrollment hours due to safety issues and routine work schedules.
Recruitment Comparison
Overall, FSW recruitment was slower and more challenging than that of IDUs. However, in the IDU study there were some challenges associated with large numbers of IDUs wanting to enroll in the study at the same time (Table 2).
Table 2.
Comparison of the RDS recruitment among female sex workers (FSWs) and injecting drug users (IDUs), Tallinn, Estonia
| FSW—study 1 | IDU—study 2 | |||||
|---|---|---|---|---|---|---|
| All | Without non-productive seeds | |||||
| Sample size | 227 | 210 | 350 | |||
| Number of recruiting months | 7 | 7 | 2 | |||
| Number of seeds | 43 | 26 | 5 | |||
| Number (%) of productive seeds | 26 (60%) | 26 (100%) | 5 (100%) | |||
| Network size (mean, SD) reported by participants | 4.9 (3.7) | 4.1 (2.5) | 70 (101.4) | |||
| Number of waves | ||||||
| Mean, median | 1.6, 1 | 2.7, 2 | 7.8, 4 | |||
| Range | 0-8 | 1-8 | 1-16 | |||
| Size of recruitment chains | ||||||
| Mean, SD | 5.3 (7.7) | 8.1 (8.9) | 55.6 (95.4) | |||
| Relationship with the recruiting peer (N/%) | ||||||
| Close friend/friend | 45 (20%) | 45 (21%) | 107/31% | |||
| Acquaintance | 129 (57%) | 129 (61%) | 187/53% | |||
| Stranger | 5 (2%) | 5 (2%) | 44/13% | |||
| Sex partner | 0 (0%) | 0 (0%) | 6/2% | |||
| Number of recruits per person | ||||||
| Seeds | Other | Seeds | Other | Seeds | Other | |
| 0 | 40% | 62% | 0 | 62% | 0 | 52% |
| 1 | 28% | 14% | 46% | 14% | 20% | 14% |
| 2 | 19% | 12% | 31% | 12% | 60% | 20% |
| 3 | 14% | 13% | 23% | 13% | 20% | 14% |
| Equilibrium reached for key variables | ||||||
| Percentagea | N of wavesb | Percentage | N of waves | Percentage | N of waves | |
| Age <20 | 6 | 5 | 6 | 4 | 8 | 5 |
| Age 20-24 | 34 | 5 | 32 | 4 | 31 | 5 |
| Age >=25 | 39 | 5 | 39 | 4 | 38 | 5 |
| Ethnicity (Russian) | 81 | 4 | 87 | 3 | 87 | 2 |
| Ethnicity (Estonian) | 14 | 4 | 13 | 3 | 13 | 2 |
| Gender (male) | NA | NA | NA | NA | 80 | 2 |
| Gender (female) | 100 | 0 | 100 | 0 | 20 | 2 |
| HIV status (pos) | 6 | 3 | 6 | 3 | 58 | 2 |
| Homophily for key variables | ||||||
| Age <20 | 0.232 | 0.229 | 0.297 | |||
| Age 20-24 | 0.153 | 0.155 | 0.181 | |||
| Age >=25 | 0.27 | 0.274 | 0.084 | |||
| Ethnicity (Russian) | 0.23 | 0.233 | −0.002 | |||
| Ethnicity (Estonian) | 0.13 | 0.127 | 0.115 | |||
| Gender (male) | NA | 0.135 | ||||
| Gender (female) | 0.037 | |||||
| HIV status (pos) | 0.192 | 0.193 | 0.207 | |||
| Education (<9 years) | 0,287 | 0.294 | 0.097 | |||
| Education (10-12 years) | 0,099 | 0.08 | 0.007 | |||
| Education (>12 years) | −1 | −1 | 0.156 | |||
aPercentage in stationary distribution;
bNumber of waves required to reach equilibrium within the radius of 0.02
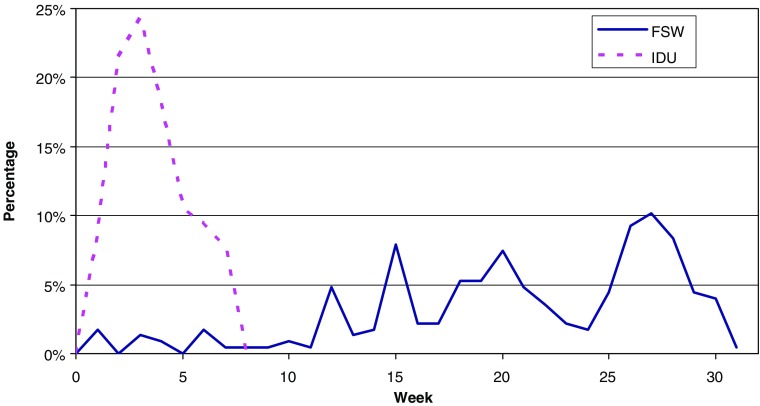
A total of 227 FSWs were recruited over a period of 28 weeks using RDS methods (Figure 1). In addition to the six initial seeds, 37 more seeds were added 2 months after the study commenced to increase the rate of recruitment. Among the 43 FSW seeds, only 60% were effective (measured as recruiting at least one peer into the study).
FIGURE 1.
Proportion of female sex worker (FSW) and injecting drug user (IDU) study subjects recruited weekly over the study period, Tallinn, Estonia.
To compare the FSW and IDU networks, we assessed network characteristics in the sample of all FSWs and in a sub-sample of FSWs after excluding non-productive seeds. The maximum number of waves was eight; mean and median numbers for the entire FSW sample were 1.6 and 1 and 2.7 and 2 for the sub-sample without non-productive seeds.
The IDU study recruited 350 (out of the projected sample size of 350) within a period of 7 weeks. Recruitment was maintained with just five seeds (all effective). The maximum number of waves for IDUs was 16 (mean 7.8, median 4).
Unadjusted mean network size for IDUs was 55.6 (SD 95.4) and 4.9 (SD 3.7) (4.1, SD 2.3 after excluding non-productive seeds) for FSWs. The proportion of friends/close friends among recruiters was lower for FSWs compared to IDUs (20% vs. 31%, OR = 0.65, 95% CI: 0.48-0.88, Fisher’s exact test p < 0.01), while the proportion of strangers was higher among IDUs compared to FSWs (13% vs. 2%, OR = 5.71, 95% CI: 2.39-13.81, Fisher’s exact test p < 0.001). Most of the remaining recruitment ties for FSWs and IDUs were among acquaintances (57% for FSWs and 53% for IDUs, OR = 1.06, 95% CI: 0.91-1.23, p > 0.05), indicating that the majority of recruitment ties were made up of persons in the recruiters’ social network.
In both the FSW and IDU samples, the distribution of the number of recruits per person differed for the seeds compared to recruits. Seeds were significantly more successful in recruitment measured by recruiting one, two, or three new participants (FSW including all seeds p = 0.03; FSW including only productive seeds p < 0.0001; IDU p = 0.02).
Although network size was not predictive of the number of recruits for both IDU and FSW samples, the association approached statistical significance for FSWs (p = 0.09).
Reaching Equilibrium for Key Characteristics
The equilibrium for key variables (age, ethnicity, gender, HIV positive status) was reached within two to five recruitment waves.
We compared recruitment biases in both samples using RDSAT adjusted proportions and unadjusted observed sample proportions on the same variables. Sample proportions in the FSW study (unadjusted) fell within the confidence bounds of the RDS-adjusted population estimates with few exceptions. If portions had not been adjusted with RDSAT, i.e., in the case of snowball sampling, the estimate for HIV prevalence would be higher by 4% (sample proportion of HIV positive 8%, adjusted proportion 4%, CI 1-6%). Unadjusted proportion for FSWs who never used condoms with their main partners was overestimated by 22% (data not shown).
The IDU-unadjusted sample proportions fell within the CIs of the RDS-adjusted population proportions with few exceptions. Unadjusted proportions for sometimes using condoms with a main sexual partner were overestimated by 10%, syringe/needle sharing was overestimated by 8%, and having health insurance was underestimated by 4% (data not shown).
Homophily
Estimates for homophily indexes for key variables in both samples were close to zero, suggesting a single underlying population for each group. The only exception was in the FSW study whereby women with 12 or more years of education had high negative homophily, indicating that most recruitment ties were formed with members recruiting new subjects with different values on this characteristic (e.g., all women with 12 or more years of education were recruited by women with less than 12 years of education).
Discussion
Overall, RDS was easier to implement among IDUs than among FSWs in Estonia. There are several possible factors for the differences in recruitment among IDUs (fast recruitment) and FSWs (slow recruitment). Earlier RDS studies in these subpopulations indicate that groups having past positive experiences with services and outreach could affect involvement in study efforts.16,17 Exposure to programs providing useful services to stigmatized populations who practice illegal behaviors may build some level of trust whereby these populations feel more comfortable participating in research. IDUs in Estonia have been receiving SEP services since 1999 and a sizable proportion (60-80%) of IDUs recruited in a 2005-2007 RDS study reported using SEP services at least once in their lifetime.7 On the contrary, Estonia has only one program specifically targeting FSWs. Thirteen percent of FSWs reported visiting the designated SW counseling and STI testing site.5
Other barriers to FSW enrollment may arise from the changing context in which sex work occurs in the region. Formative research indicates that FSWs form smaller peer network groups compared to IDUs (average network size for FSWs was five versus 70 for IDUs). Furthermore, some FSWs reported that they have no interaction with other FSWs (e.g., self-employed FSWs using the internet or media to solicit clients) and others reported that their social networks were made up of distinct sub-networks within the larger networks of FSWs (e.g., brothel-based FSWs).
Another factor possibly affecting participation by FSWs is their fear of being identified as a FSW. Engaging in sex for money is not punishable under Estonia’s criminal code so long as it takes place within one’s own residence and is consensual among adults (≥18 years). Acting as a gatekeeper (pimp or procurer), providing space for someone to sell sex, and involving minors under the age of 18 are punishable offenses. As reported in other countries in Eastern Europe, including the former soviet republics, some of Estonia’s sex work activities are controlled by organized crime elements.16 In Estonia, there were indications that gatekeepers (i.e., madams at the brothels, pimps) were reluctant to allow FSWs under their control to participate in a study that might expose them to questioning by authorities. For instance, in some cases, gatekeepers were collecting coupons from FSW study participants and managing who they wanted to redeem them. As noted in other RDS studies of FSWs, inadequate incentives may pose a barrier to FSW enrollment.16,17 Unlike RDS studies of IDUs, the eligibility criteria linked to FSWs is based on behaviors related to how they earn a living. As such, it has been found that FSWs often try to equate the level of their incentive for participation on the amount of money they would have earned providing services to a client. This often results in incentive requests beyond the budget of the study.
The statistical theory upon which RDS is based suggests that if peer recruitment proceeds through a sufficiently large number of waves, the composition of the sample will stabilize, becoming independent of the seeds from which recruitment began, thereby overcoming any bias caused by the non-random selection of seeds.14 Equilibrium was achieved for both the IDU and FSW samples on average by one wave earlier for IDUs than for FSWs.
Homophily estimates from both samples indicate that participants did not exclusively form ties with individuals with either the same (homophily) or different (heterophily) characteristics measured within their social networks with a possible exception for the group of FSWs with higher education, whereby heterophily was high. This can be explained by the fact that there are few FSWs with higher education resulting in limited recruitment possibilities. Although the proportion of IDUs with higher education was even lower, selective sampling (low homophily) within this IDU subset may be explained by the substantially larger size of the target population in the region (estimated 2,000 FSWs and 10,000 IDUs in Tallinn area).11,12
These studies were limited in that the full network-size question was not asked (the definition of the population, age range, and geographical regions were missing). The network size-question sets up the probability of inclusion into the sample, and omission of eligibility criterion results in the possible overestimation of participants’ network sizes.
There are reasons to believe that some RDS requirements were not met for the FSW population in Tallinn. FSWs may not have been able to randomly recruit from their social networks due to interference by gatekeepers, and the addition of so many seeds in this study may have hindered naturally occurring network patterns. Furthermore, changes made during the course of the study, whereby we added a large number of additional seeds and adjusted the interview and testing location to increase FSW enrollment, may have impacted recruitment. Adding seeds during recruitment is an accepted practice in RDS and although it is best to minimize changes to a study protocol during data collection, conducting interviews and HIV testing in a location convenient to the study participants should not have any direct impact on the sampling requirements.
Furthermore, although changing a fixed site interview location during the course of a study can impact network sampling if there is spatial heterogeneity in the population, we believe that allowing FSWs to be interviewed in locations of their choosing may have enhanced sociometric depth and sustained recruitment. In an ideal RDS study, the incentives being offered should motivate all members of the population to be studied, and there should not be any relationship between the attractiveness of the incentives and the major outcome variables of the study. It is likely that more economically disadvantaged IDUs would have been more highly motivated to participate though we do not believe this would create a major bias because for the FSWs, the potential bias may be more of a problem. The FSWs who were motivated to participate because of a free STI examination might easily have been more at risk for STIs (including sexually transmitted HIV) resulting in an overestimation of HIV prevalence.
Recommendations
There are several recommendations for using RDS among IDUs and FSWs in Estonia and perhaps in other areas in the region. First, formative research, especially if the target population is not well known, is an important component to implementing most RDS studies. Through formative research, we learned that FSWs originally desired incentives that were too costly for our study budget and helped us find acceptable alternatives (e.g., STI testing and results). As public health researchers, this was particularly valuable information since the provision and acceptance of health care services and treatment, rather than money, is a benefit not only for the study participants but the wider population as well.
Second, it is important to speak to persons who may influence the implementation of an RDS study. For instance, if possible, engaging FSWs’ gatekeepers before and during the study could increase their understanding of the importance of the study methodology and encouraged them to not interfere with the distribution of recruitment coupons. This could also be an opportunity to explain that the study will ensure confidentiality and anonymity and that participation will not negatively impact FSWs’ work.
Third, given the number of complex theoretical requirements of RDS, this method should be conducted by researchers with experience in RDS implementation. Thorough theoretical and empirical knowledge are important for rigorous implementation of the planning, sampling, and analyses processes.
Fourth, it is important to detect and respond to poor recruitment during data collection without negatively impacting important theoretical and methodological requirements. Upon discovering that FSWs would not attend a fixed RDS site, we offered to interview and test them in a location convenient to them. Although this required changes to our testing protocol and the need to acquire new testing equipment, these adjustments allowed us to attain a larger sample while maintaining the RDS methodological requirements.
Fifth, gathering field notes during the recruitment process can be helpful for effectively detecting and responding to implementation challenges and informing future study design development.
Finally, it is essential for researchers to continue discussing the utilization challenges and improvements associated with using RDS in different populations and international settings. RDS is superior to other sampling method used for hard-to-reach populations for two important reasons: (1) it can produce rapid, cost-efficient recruitment; and (2) RDSAT-adjusted estimates are reported as being more representative than those gathered through other commonly used sampling methods.18
Overall, RDS is a major advance in conducting research among FSWs and IDUs in Estonia.
Acknowledgment
This research was supported in part through grant R01 DA 03574 from the US National Institute on Drug Abuse, by the Global Fund to Fight AIDS, Tuberculosis, and Malaria who funded this study through the National Institute for Health Development in Estonia (EST-202-G01-H-00), Norwegian Financial Mechanism/EEA (grant EE0016) and by US Civilian Research Development Foundation grant (ESX0-2722-TA-06).
Authors express their gratitude to the teams at the NGOs Me Aitame Sind, Corrigo, and to all participants of the study.
The content of this paper has not been published elsewhere, nor is it being considered elsewhere, nor are there any conflicts of interest contained therein.
Footnotes
Contributors
Uusküla, L. Johnston and D. Des Jarlais designed the approach for the comparison analysis. M. Raag performed the needed statistical analyses. A. Uusküla wrote the first draft of the manuscript. All authors contributed to revising the manuscript and have approved the final manuscript.
References
- 1.Magnani R, Sabin K, Saidel T, Heckathorn DD. Sampling hard to reach and hidden populations for HIV surveillance. AIDS. 2005;19(Suppl 2):S67–S72. doi: 10.1097/01.aids.0000172879.20628.e1. [DOI] [PubMed] [Google Scholar]
- 2.Semaan S, Lauby J, Liebman J. Street and network sampling in evaluation studies of HIV risk-reduction interventions. AIDS Rev. 2002;4:213–223. [PubMed] [Google Scholar]
- 3.Heckathorn DD. Respondent-driven sampling II: deriving valid population estimates from chain-referral samples of hidden populations. Soc Probl. 2002;49:11–34. doi: 10.1525/sp.2002.49.1.11. [DOI] [Google Scholar]
- 4.Salganik MJ, Heckathorn DD. Sampling and estimation in hidden populations using respondent-driven sampling. Sociol Method. 2004;34:193–239. doi: 10.1111/j.0081-1750.2004.00152.x. [DOI] [Google Scholar]
- 5.Trummal A, Fischer K, Raudne R. HIV-nakkuse levimus ning riskikäitumine prostitutsiooni kaasatud naiste hulgas Tallinnas. National institute for Health Protection, 2006. Accessed on: January 10, 2008. Available at: http://www.tai.ee/failid/PK_HIV_uurimuse_raport_12.2006_1_parandatud.pdf
- 6.Uuskula A, Rajaleid K, Talu A, Abel K, Rüütel K, Hay G. Estimating injection drug use prevalence using state wide administrative data sources: Estonia, 2004. Addiction Res Th. 2007;15(4):411–424. doi: 10.1080/16066350701417533. [DOI] [Google Scholar]
- 7.Platt L, Bobrova N, Rhodes T, Uusküla A, Parry JV, Rüütel K, Talu A, Abel K, Rajaleid K, Judd A. High HIV prevalence among injecting drug users in Estonia: implications for understanding the risk environment. AIDS. 2006;20(16):2120–2123. doi: 10.1097/01.aids.0000247586.23696.20. [DOI] [PubMed] [Google Scholar]
- 8.Wilson TE, Sharma A, Zilmer K, Kalikova N, Uusküla A. The HIV prevention needs of injection drug users in Estonia. Int J STD AIDS. 2007;18(6):389–391. doi: 10.1258/095646207781024900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Uusküla A, McNutt LA, Dehovitz J, Fischer K, Heimer R. High prevalence of blood-borne virus infections and high-risk behaviour among injecting drug users in Tallinn, Estonia. Int J STD AIDS. 2007;18(1):41–46. doi: 10.1258/095646207779949907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Uusküla A, Kals M, Rajaleid K, Abel K, Talu A, Rüütel K, Platt L, Rhodes T, Dehovitz J. High-prevalence and high-estimated incidence of HIV infection among new injecting drug users in Estonia: need for large-scale prevention programs. J Public Health (Oxf) 2008;30(2):119–125. doi: 10.1093/pubmed/fdn014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Uusküla A, Fischer K, Raudne R, Kilgi H, Krylov R, Salminen M, Brummer-Korvenkontio H, St Lawrence JS, Aral SO. A study on HIV and hepatitis C virus among commercial sex workers in Tallinn. Sex Transm Infect. 2008;84(3):189–191. doi: 10.1136/sti.2007.027664. [DOI] [PubMed] [Google Scholar]
- 12.Aral SO, St Lawrence JS, Uusküla A. Sex work in Tallinn, Estonia: the sociospatial penetration of sex work into society. Sex Transm Infect. 2006;82(5):348–353. doi: 10.1136/sti.2006.020677. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Heckathorn DD. Extensions of respondent-driven sampling: analyzing continuous variables and controlling for differential degree. Socio Methodol. 2007;37:151–207. doi: 10.1111/j.1467-9531.2007.00188.x. [DOI] [Google Scholar]
- 14.Respondent-driven sampling. Accessed on: October 08, 2007. Available at: http://www.respondentdrivensampling.org.
- 15.Heckathorn DD. Respondent-driven sampling: a new approach to the study of hidden populations. Soc Probl. 1997;44:174–199. doi: 10.2307/3096941. [DOI] [Google Scholar]
- 16.Simic M, Johnston LG, Platt L, Baros S, Andjelkovic V, Novotny T, Rhodes T. Exploring barriers to ‘respondent-driven sampling’ in sex worker and drug-injecting sex worker populations in Eastern Europe. J Urban Health. 2006;83(Suppl 6):6–15. doi: 10.1007/s11524-006-9098-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Johnston LG, Malekinejad M, Rifkin MR, Kendall C, Rutherford GW. Implementation challenges to using respondent-driven sampling methodology for HIV biological and behavioral surveillance: field experiences in international settings. AIDS Behav. 2008;12(Suppl 4):S131–S141. doi: 10.1007/s10461-008-9413-1. [DOI] [PubMed] [Google Scholar]
- 18.Salganik MJ, Heckathorn DD. Sampling and estimation in hidden populations using respondent-driven sampling. Socio Meth. 2004;34:193–239. doi: 10.1111/j.0081-1750.2004.00152.x. [DOI] [Google Scholar]
- 19.Shakarishvili A, Dubovskaya LK, Zohrabyan LS, St Lawrence JS, Aral SO, Dugasheva LG, Okan SA, Lewis JS, Parker KA, Ryan CA. LIBRA project investigation team. Sex work, drug use, HIV infection, and spread of sexually transmitted infections in Moscow, Russian Federation. Lancet. 2005;366(9479):57–60. doi: 10.1016/S0140-6736(05)66828-6. [DOI] [PubMed] [Google Scholar]
- 20.Des Jarlais DC, Perlis TE, Stimson GV, Poznyak V, WHO Phase II Drug Injection Collaborative Study Group Using standardized methods for research on HIV and injecting drug use in developing/transitional countries: case study from the WHO Drug Injection Study Phase II. BMC Public Health. 2006;6:54. doi: 10.1186/1471-2458-6-54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Gallo D, George JR, Fitchen JH, Goldstein AS, Hindahl MS. Evaluation of a system using oral mucosal transudate for HIV-1 antibody screening and confirmatory testing. OraSure HIV Clinical Trials Group. JAMA. 1997;277(3):254–258. doi: 10.1001/jama.1997.03540270080030. [DOI] [PubMed] [Google Scholar]