Abstract
Although criminal justice involvement has repeatedly been associated with human immunodeficiency virus (HIV)/sexually transmitted infection prevalence and sexual risk behaviors, few studies have examined whether arrest or incarceration uniquely contributes to sexually risky behavior. We examined the temporal relationship between criminal justice involvement and subsequent sexual HIV risk among men in methadone maintenance treatment in New York City. A random sample of 356 men was interviewed at baseline (time 1), 6-month (time 2), and 12-month (time 3) follow-ups. Propensity score matching, negative binomial, and multiple logistic regression were used to isolate and test the effect of time 2 arrest and incarceration on time 3 sexual risk behaviors. Incidence of time 2 criminal justice involvement was 20.1% for arrest and 9.4% for incarceration in the prior 6 months. Men who were arrested at time 2 demonstrated increased number (adjusted incidence rate ratio [IRR] = 1.62; 95% confidence intervals [CI] = 1.11, 2.37) and proportion (IRR = 1.36; 95% CI = 1.07, 1.72) of unprotected vaginal sex acts at time 3. Men incarcerated at time 2 displayed increased number (IRR = 2.07; 95% CI = 1.23, 3.48) and proportion (IRR = 1.45; 95% CI = 1.06, 1.99) of unprotected vaginal sex acts at time 3. Within this sample of drug-involved men, arrest and incarceration are temporally associated with and may uniquely impact successive sexual risk-taking. Findings underscore the importance of HIV prevention interventions among individuals with low-intensity criminal justice involvement. Developing prevention efforts aimed at short-term incarceration, community reentry, and alternatives to incarceration settings will address a large and under-researched segment of the criminal justice population. Alternative approaches to current criminal justice policy may result in public health benefits.
Keywords: Criminal justice involvement, HIV, Sexual risk behavior, Methadone, Men
Introduction
Human immunodeficiency virus (HIV) and other sexually transmitted infections (STIs) among men in the criminal justice system are well established as a serious public health concern.1–4 HIV/STI prevalence in criminal justice populations is higher than in the general population for nearly every demographic grouping of men, and many studies document increased levels of sexual risk behaviors associated with criminal justice involvement.5–7 A recent review summarized that incarcerated populations (compared to the general population) initiate sex at an earlier age, have more sexual partners, and use STI prevention methods more inconsistently.1
Although there is a clear disparity in HIV/STI prevalence and risk among male offenders, a question which has not been adequately addressed is whether criminal justice involvement uniquely contributes to a confluence of HIV/STI risk factors for these men. In order to assess criminal justice involvement as a contributor to HIV risk, two important issues must be considered: temporality and confounding. Most studies which have linked criminal justice involvement and sexual risk utilize cross-sectional designs which lack the ability to examine temporal relationships. One exception is Johnson and Raphael’s analysis of national-level panel data, which finds strong effects of male incarceration on both male and female AIDS infection rates among African Americans.8 Additionally, any relationship found between criminal justice involvement and sexual risk behavior is likely to be influenced by confounding, given that both issues involve a complex interaction of individual, social, and structural factors. Widespread within criminal justice populations are drug abuse and mental illness, which have repeatedly been linked to sexual risk behaviors.9–15 Among male offenders, correlates of sexual risk-taking include past sexual or physical victimization,16 unstable housing,17 poverty and unemployment,18 and social stress linked to race and socioeconomic status.19
In a previous cross-sectional study of men in drug treatment, we found that recent arrest or incarceration was associated with several sexual risk behaviors.20 To build upon this work, we utilize panel data from the same sample of men in order to establish temporality. The purpose of this paper is to examine the temporal relationship between criminal justice involvement and subsequent sexual HIV risk behaviors among men with serious drug use histories (herein referred to as “drug-involved” men). By using panel data with careful measurement of social and behavioral determinants of HIV/STIs, we aim to isolate the effect of criminal justice involvement on sexual risk behaviors and control for the influence of numerous confounding variables. The significance of this study is its examination of the possible influence of criminal justice involvement on sexual HIV/STI risk—an area of very limited research. Findings from this study may inform HIV prevention interventions with criminal justice populations as well as public health and criminal justice policy.
Methods
Participants
The data for this study come from an epidemiologic study of the social and behavioral determinants of HIV/STI risk among men in methadone treatment, which was conducted between 1999 and 2004. A methadone-maintained sample was chosen for several reasons, including their relative stability compared to other drug-using men as well as their continued vulnerability to drug use, sexual risk behaviors, and criminal involvement.21–23 Using a random number generator in SPSS, we randomly selected 1,300 men from the total population of 2,067 men enrolled in seven methadone maintenance treatment programs in New York City. Of these 1,300 randomly selected men, 25 men were excluded from screening because they did not demonstrate sufficient English-speaking proficiency to provide informed consent, and three men were excluded from screening due to a severe cognitive or psychiatric impairment that interfered with their ability to give informed consent. From the remaining 1,272 men, 194 refused to participate in the study and 304 missed two or more appointments to be screened and did not participate. Of the 774 men who completed a screening interview, 356 met eligibility criteria and participated in the study. Eligibility criteria included men, aged 18 years or older, who were enrolled in methadone treatment for at least 3 months, and who reported having a sexual relationship with a woman during the past year. Participants completed a 90-min face-to-face, structured baseline (time 1) interview administered by experienced male interviewers, and identical follow-up assessments were conducted at 6 and 12 months post-baseline (times 2 and 3). A detailed recruitment and sample description is available in a previous paper.24
Measures
In order to establish temporal ordering, outcomes were identified at time 3, exposure at time 2, and potential confounders at time 1.
Outcomes (Time 3): Sexual Risk Behaviors
Unprotected sex was measured as the number and proportion of vaginal and anal sex acts across partners in the prior 30 days in which a male or female condom was not used. Additional sexual HIV risk behaviors assessed in the past 6 months included having multiple (two or more) sexual partners, sex trading (buying or selling sex for drugs and/or money), and having sex with someone known or suspected to be HIV positive and/or an injection drug user (IDU).
Exposure (Time 2): Criminal Justice Involvement
In this paper, we use the general term “criminal justice involvement” to refer broadly to any involvement in the criminal justice system (including being arrested and/or incarcerated) as well as the more specific terms “arrest” and “incarceration.” Participants self-reported lifetime incidence of arrest and incarceration, as well as incidence of arrest and incarceration in the past 6 months. Length of the most recent incarceration was also reported.
Potential Confounders (Time 1)
Participants self-reported sociodemographic characteristics including age, race/ethnicity, education, monthly income, marital and parental status, employment, and housing status. Drug use histories were reported, and recent drug use was operationalized as the number of types of illicit drugs used over the past 6 months (range 0–6). Scales from the Brief Symptom Inventory (BSI) measured mental health symptomology, including the General Severity Index, Positive Symptom Total, and the Psychoticism Subscale.25 Past physical or sexual abuse victimization was measured using the Childhood Sexual Abuse Interview26 and the Childhood Trauma Questionnaire.27 Baseline and follow-up assessments also included self-reported HIV infection status and past diagnosis of an STI.
Data Analysis
Of the 356 men who completed the baseline interview, over 80% (289) participated in a 6-month follow-up, and 79% (280) completed the 12-month follow-up assessment. Univariate analyses indicated that men lost to follow-up did not differ significantly from retained men on background or outcome variables assessed at time 1. To reduce the potential bias due to missing data and differential attrition in the panel data, multiple imputation was performed using the multivariate imputation by chained equations (MICE) function in Stata 9.28
,
29 This process involves creating several copies (m) of the complete dataset (for this study m = 5), each of which has missing values imputed from prediction models based on the non-missing data. Subsequent regression estimates are averaged across the created datasets to give a single estimate, which takes into account any variation in imputed values across datasets. Obtaining valid standard errors (and confidence intervals) for each averaged point estimate via “Rubin’s rules”29 involves combining information on within-imputation (W) and between-imputation (B) variation; the total variance in the averaged estimate (T) is then derived by  .30
.30
Although the men in this study have many similarities based on their involvement in methadone treatment, individual differences on a variety of sociodemographic and background characteristics undoubtedly remain, and these differences may be associated with one’s likelihood to be involved in the criminal justice system. In order to account for these individual differences within the sample, we estimated the effect of criminal justice involvement on later sexual risk behaviors using propensity score estimators.31 We calculated a predicted probability (or propensity score) that each individual was arrested at time 2 based on a number of time 1 confounders. Additionally, a separate propensity score model was calculated using incarceration at time 2 (versus no incarceration at time 2). Each of these weighting procedures yielded two groups that were similar on all measured time 1 confounders but differing primarily on arrest or incarceration at time 2. The following time 1 variables were used to calculate propensity score weights to balance the exposure and control groups: age, race/ethnicity, education, income, number of children, history of physical or sexual abuse, unemployment, homelessness, recent drug use, HIV status, recent STI diagnosis, and BSI Global Severity Index, Positive Symptom Total, and Psychoticism Subscale. Additionally, balance was maintained on time 1 variables related to the exposure and outcomes: lifetime history of arrest or incarceration and level of baseline sexual risk behavior (a composite score of types of sexual risk practiced at time 1; range 0–5).
We then estimated associations between arrest and incarceration at time 2 and sexual risk behavior outcomes at time 3. The count variable outcomes for number of unprotected vaginal and anal sex acts demonstrated considerable overdispersion (unprotected vaginal sex acts  , s
2 = 70.56; unprotected anal sex acts
, s
2 = 70.56; unprotected anal sex acts  , s
2 = 1.44). Negative binomial regression was therefore employed for these unprotected sex outcomes with further offset for exposure (total vaginal or anal sex acts) in order to estimate incidence rate ratios (IRRs) and 95% confidence intervals (CIs) of the number and proportion of unprotected sex acts. We used logistic regression to estimate odds ratios (ORs) and 95% CIs for the association between arrest and incarceration at time 2 and the remaining time 3 sexual risk outcomes (multiple sex partners, sex with a risky partner, and sex trading). Each regression model was enhanced by subsequent covariance adjustment of time 1 variables used in the propensity score weighting process. This combined method is superior to using either propensity scores or covariance adjustment alone.32
, s
2 = 1.44). Negative binomial regression was therefore employed for these unprotected sex outcomes with further offset for exposure (total vaginal or anal sex acts) in order to estimate incidence rate ratios (IRRs) and 95% confidence intervals (CIs) of the number and proportion of unprotected sex acts. We used logistic regression to estimate odds ratios (ORs) and 95% CIs for the association between arrest and incarceration at time 2 and the remaining time 3 sexual risk outcomes (multiple sex partners, sex with a risky partner, and sex trading). Each regression model was enhanced by subsequent covariance adjustment of time 1 variables used in the propensity score weighting process. This combined method is superior to using either propensity scores or covariance adjustment alone.32
Results
Background Characteristics
Table 1 presents characteristics of the study sample at time 1. The majority of the sample identified as either Latino or African American, and these men had experienced a number of historic and recent hardships, including high levels of physical and sexual abuse histories, unemployment, and homelessness. Self-reported HIV infection was high (14%), and mental health symptomology, as measured by the three BSI scales, was higher in severity than in the general male population.25 Recent drug use was common, particularly heroin (50%), marijuana (38%), and powder cocaine (33%).
Table 1.
Time 1 background characteristics of men in methadone maintenance treatment programs, New York City (N = 356)
n or 
|
Percentage or SD | |
|---|---|---|
| Age (years) |

|
SD = 8.5 |
| Years of schooling |

|
SD = 2.3 |
| Income ($/month) |

|
SD = 958 |
| Number of children |

|
SD = 1.5 |
| Race/ethnicity (n) | ||
| Latino | 161 | 45% |
| African American | 134 | 38% |
| Unemployed in the past 6 months | 169 | 47% |
| Homeless in the past 6 months | 61 | 17% |
| Lifetime history of physical abuse | 137 | 38.5% |
| Lifetime history of sexual abuse | 149 | 42% |
| Any drug use in past 6 months | 257 | 72% |
| Number of drugs used, past 6 months |

|
SD = 1.42 |
| Used heroin, past 6 months | 177 | 50% |
| Used powder cocaine, past 6 months | 117 | 33% |
| Used crack cocaine, past 6 months | 70 | 20% |
| Used marijuana, past 6 months | 134 | 38% |
| Duration of methadone treatment (years) |

|
SD = 7.4 |
| HIV positive | 51 | 14% |
| Diagnosed with STI in past 6 months | 16 | 4.5% |
| BSI Global Severity Index |

|
SD = .63 |
| BSI Positive Symptom Total |

|
SD = 14.17 |
| BSI Psychoticism Scale |

|
SD = .67 |
Criminal Justice Involvement
Nearly all of the men in the sample (94%) reported at least one arrest in their lifetime, and lifetime prevalence of incarceration was 74%. Regarding time 2 criminal justice involvement, 20.1% of the sample was arrested and 9.4% was incarcerated in the previous 6 months. Length of incarceration at time 2 was relatively brief: range = 0–150 days,  (SD = 32.6). Although lifetime incarcerations may have occurred in both prisons and jails, the incarcerations defined as time 2 exposures in this study would have occurred exclusively in jails, as prison sentences by definition are a minimum of 1 year in duration.
(SD = 32.6). Although lifetime incarcerations may have occurred in both prisons and jails, the incarcerations defined as time 2 exposures in this study would have occurred exclusively in jails, as prison sentences by definition are a minimum of 1 year in duration.
Sexual Risk Behaviors
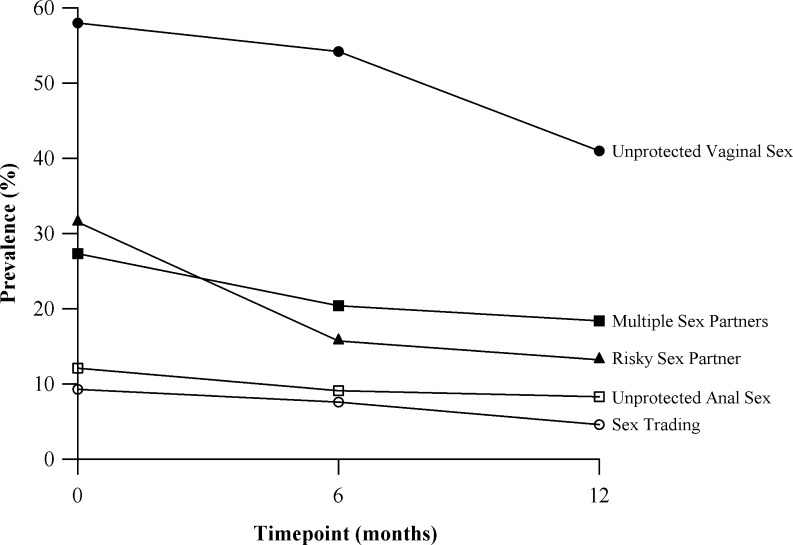
Figure 1 summarizes the prevalence of HIV risk behaviors over the three time periods of the study. The most prevalent HIV risk behavior reported was unprotected vaginal sex (ranging from 41% to 58%), followed by having multiple sex partners, sex with a risky partner, unprotected anal sex, and sex trading (buying or selling sex for drugs and/or money). The mean number of unprotected vaginal sex acts in the past 30 days at time 3 was  (SD = 8.4), and the mean number of unprotected anal sex acts was
(SD = 8.4), and the mean number of unprotected anal sex acts was  (SD = 1.2). Only four men in the study sample reported any sexual activity with a male partner in the past 6 months, and all reported anal sex acts were with female partners (male insertive).
(SD = 1.2). Only four men in the study sample reported any sexual activity with a male partner in the past 6 months, and all reported anal sex acts were with female partners (male insertive).
FIGURE 1.
Sexual risk behaviors over time of men in methadone maintenance treatment programs, New York City (N = 356).
Propensity Score Weighting Balance Results
Prior to the propensity score weighting process, unweighted models demonstrated marked differences between exposure and control groups on the following time 1 variables: being Black, being Latino, income, unemployment, homelessness, number of children, physical or sexual abuse history, drug use, BSI Psychoticism Scale, and HIV prevalence. After propensity score weighting procedures were employed, no significant differences were found in the weighted models using t test mean comparisons.
Longitudinal Associations between Time 2 Criminal Justice Involvement and Time 3 Sexual Risk Behaviors
Unprotected Sex (Table 2)
Table 2.
Incidence rate ratios (IRR) and odds ratios (OR) and 95% confidence intervals (CI) for the relationship between criminal justice involvement (time 2) and subsequent sexual risk behaviors (time 3) with covariance adjustment (time 1) among men in methadone maintenance treatment programs, New York City (N = 356)
| Dependent variable: sexual HIV/STI risk behaviors: time 3 | ||||||
|---|---|---|---|---|---|---|
| Independent variable: criminal justice involvement: time 2 | Number of unprotected vaginal sex acts, past 30 days | Proportion unprotected vaginal sex acts, past 30 days | Proportion unprotected anal sex acts, past 30 days | More than one sexual partner, past 6 months | Sex with someone HIV+ or IDU, past 6 months | Participant engaged in sex trading, past 6 months |
| Participant arrested in past 6 months | ||||||
| Unadjusted model | IRR = 1.74** (1.16, 2.62) | IRR = 1.45* (1.01, 3.47) | IRR = 0.54 (0.18, 1.66) | OR = 1.21 (0.57, 2.58) | OR = 0.72 (0.26, 1.97) | OR = 0.87 (0.23, 3.26) |
| Adjusted model | IRR = 1.62** (1.11, 2.37) | IRR = 1.36** (1.07, 1.72) | IRR = 0.45 (0.11, 1.79) | OR = 1.18 (0.54, 2.61) | OR = 0.74 (0.28, 1.95) | OR = 1.24 (0.26, 5.99) |
| Post hoc adjusted modela | IRR = 1.75** (1.16, 2.64) | IRR = 1.35* (1.05, 1.73) | ||||
| Participant incarcerated in past 6 months | ||||||
| Unadjusted model | IRR = 1.42* (1.11, 2.28) | IRR = 1.23* (1.03, 1.50) | IRR = 1.21 (0.88, 1.66) | OR = 1.30 (0.32, 5.32) | OR = 1.18 (0.20, 6.80) | OR = 1.47 (0.11, 19.6) |
| Adjusted model | IRR = 2.07** (1.23, 3.48) | IRR = 1.45** (1.06, 1.99) | IRR = 1.14 (0.79, 1.64) | OR = 1.51 (0.25, 9.24) | OR = 1.15 (0.23, 5.79) | OR = 1.73 (0.03, 89.2) |
| Post hoc adjusted modela | IRR = 1.90* (1.04, 3.48) | IRR = 1.65** (1.17, 2.34) | ||||
Adjusted models include the following time 1 covariates: age, race/ethnicity, education, income, recent unemployment, recent homelessness, history of physical or sexual abuse, number of children, number of drugs used past 6 months, HIV status, recent diagnosis of an STI, BSI Global Severity Index, BSI Positive Symptom Total, BSI Psychoticism Subscale, and composite of sexual risk behaviors past 6 months
*p ≤ 0.05, **p ≤ 0.01
aPost hoc adjusted models also include covariance adjustment for time 1 number of unprotected vaginal sex acts
Arrest at time 2 was associated with an increased number of unprotected vaginal sex acts across partners in the past 30 days at time 3 (adjusted IRR = 1.62; 95% CI = 1.11–2.37) and higher proportion of unprotected vaginal sex at time 3 (adjusted IRR = 1.36; 95% CI = 1.07–1.72). Likewise, incarceration at time 2 was associated with increased number (adjusted IRR = 2.07; 95% CI: 1.23–3.48) and proportion (adjusted IRR = 1.45; 95% CI = 1.06–1.99) of unprotected vaginal sex acts at time 3. At the 95% confidence level, we did not detect a significant association between arrest or incarceration and subsequent unprotected anal sex.
Additional Sexual Risk Behaviors
As seen in Table 2, arrest and incarceration at time 2 were not significantly associated with having multiple sex partners, sex with a risky partner, and sex trading at time 3. Although most of the odds ratios reported for associations with incarceration are above 1.0, suggesting a trend of increased risk, these associations were not significant at the 95% confidence level or the 90% level.
Post Hoc Analyses
Based on our findings that the only time 3 outcome that was significantly associated with time 2 arrest or incarceration was unprotected vaginal sex, we conducted post hoc analyses to test the robustness of this association. Adjusted models using number and proportion of unprotected vaginal sex acts as outcomes were recalculated with further adjustment for time 1 number of unprotected vaginal sex acts. After this added adjustment for baseline levels of the outcome variable, time 2 arrest remained significantly associated with increased likelihood of subsequent number (adjusted IRR = 1.75; 95% CI = 1.16–2.64) and proportion (adjusted IRR = 1.35; 95% CI = 1.05–1.73) of vaginal sex acts at time 3. Similarly, time 2 incarceration remained significantly associated with increased number (adjusted IRR = 1.90; 95% CI = 1.04–3.48) and proportion (adjusted IRR = 1.65; 95% CI = 1.17–2.34) of unprotected vaginal sex acts at time 3.
Discussion
To our knowledge, this is the first study to examine the temporal relationship between criminal justice involvement and subsequent sexual risk behaviors among men. Although the study employs a relatively select sample of men on methadone, the findings add to our understanding of the criminal justice/HIV relationship among drug-involved men. A key finding in this study is that a temporal relationship exists between both arrest and short-term incarceration and unprotected vaginal sex. The significance of this relationship endured multiple adjustments for preceding confounders and additional post hoc analyses controlling for baseline levels of unprotected vaginal sex. These findings are consistent with previous research linking incarceration with unprotected sex6 , 7 , 17 , 33 but build on them by defining a temporal ordering of exposure and outcomes. Furthermore, this is the first known study to highlight a temporal relationship between arrest and sexual risk. Arrest is the first point of entry into the justice system and is therefore the most prevalent form of criminal justice involvement. Coupled with the reality of over 7 million releases from incarceration each year, the majority from local jails,34 understanding the sexual HIV/STI risk effects of arrest and short-term incarceration among community-based populations is an important area of public health research.
The temporal relationship found between arrest and incarceration and unprotected vaginal sex warrants further investigation into whether criminal justice involvement exacerbates sexual risk-taking. There are several plausible mechanisms by which arrest or short-term incarceration could contribute to increased subsequent unprotected sex. One possibility is that men who are arrested or incarcerated may experience temporary but influential disruptions in functioning and stability, such as economic hardship, loss of housing, or relationship conflicts, which could contribute to more spontaneous and risky initiations of sexual activity.35–37 Similarly, considering that this sample is entirely composed of men on methadone, even short-term criminal justice involvement could disrupt continuity of substance abuse treatment, increasing one’s susceptibility to both increased drug use and sexual risk behaviors. Being arrested likely disrupts social networks and social capital,37 leading to altered networks that may influence norms and practices of HIV risk reduction strategies.38–41 Even short-term incarceration may expose men to risks such as unprotected sex within the correctional setting or high-risk sexual encounters upon release.42–44 Understanding how arrest and short-term incarceration may impact subsequent unprotected sex is subject to further research which can test these and other hypotheses. Additionally, the findings of this paper should be interpreted with the understanding that not all unprotected sex is equally unsafe. Future research would benefit from measurement of the context in which unprotected sex occurs, such as in monogamous relationships versus multiple/concurrent partnerships or among discordant couples. This approach would provide a more accurate appraisal of the level of HIV/STI risk associated with unprotected sex behaviors. Additionally, future research using longer-term longitudinal data could examine trends in the relationship between criminal justice involvement and sexual risk behaviors over time.
In this study, several risk behaviors found to be associated with criminal justice involvement in previous cross-sectional research, such as multiple partnerships,7 , 45 , 46 were not found to be temporally associated with arrest or incarceration. The findings of this paper do not necessarily contradict these studies; rather, they suggest that previously found associations may be spurious and are likely influenced by social and structural factors which impact upon both criminal justice involvement and sexual risk. Additionally, this study tests the effect of incident arrest or incarceration on sexual risk-taking. Given that this sample of men display high lifetime levels of criminal justice involvement, arrest or incarceration at one time point may not serve as a powerful predictor of all measured sexual risk behaviors. This study focuses on relatively older men whose drug abuse history is extensive; the relationship between criminal justice involvement and sexual risk-taking may be weaker for this sample compared to younger men with less intense involvement with drug abuse and its negative health effects. Despite these issues, HIV/STI prevalence and risk remains high among justice-involved men, and this study suggests that there may be aspects of sexual risk-taking that are uniquely affected by criminal justice involvement. These findings reinforce the notion that men involved in the criminal justice system remain a critical audience for tailored HIV/STI prevention interventions.42 , 47 , 48
This study’s findings underscore the importance of HIV/STI prevention research among individuals with low-intensity criminal justice involvement. While there is limited HIV prevention research being conducted in prison settings,4 , 49 HIV/STI prevention models targeting short-term jail inmates are virtually nonexistent. Providing services to jail inmates is difficult given their rapid cycle of arrest and release.34 HIV/STI prevention within jail systems could test brief, even single-session, risk reduction interventions, which have been shown effective in various populations.50–52 Additionally, HIV prevention studies could recruit participants from jail settings and implement prevention interventions upon community reentry—a high-risk window of opportunity for intervention.53 , 54 Providing HIV/STI prevention services to non-incarcerated arrestees could be accomplished in community settings such as probation and alternative to incarceration programs.
Future research can build upon this study’s findings by further contextualizing sexual HIV risk for criminal justice populations. Whereas this study suggests the influence of social factors on both criminal justice involvement and HIV risk, additional research is needed to better understand why people come to be exposed to risk or protective factors. Research on the HIV risk impact of criminal justice involvement should be conducted among different populations in order to ascertain if this relationship differs among diverse social and economic conditions. Although examining the role of specific mechanisms in the relationship between criminal justice involvement and sexual HIV risk was not within the scope of this paper, findings from this study suggest such research is warranted. This type of research would be well-served to incorporate qualitative research to better explore how both arrest and incarceration may affect sexual behaviors. As we build a contextual understanding of this relationship, HIV prevention with criminal justice populations can become more effective at reducing individual risk while working to alleviate social stressors such as homelessness and unemployment, which are overrepresented in the criminal justice system and have fundamental impacts upon health.55
This study has several potential limitations. The findings of the study may not be generalizable to the general population of men, and the study relies upon self-reported data such as HIV status. Incidence of time 2 arrest and incarceration, anal sex, and sex trading were somewhat rare; the resulting sample size may limit the power to detect significant differences in all study outcomes. Moreover, while the use of propensity score weighting in a temporal design is useful in controlling for confounders, the analyses herein are restricted to confounding variables that were measured in the parent study. Any temporal relationships found in this study should be interpreted carefully, as some potentially confounding factors may not have been measured. As previously stated, the research design examined the impact of incident arrest and incarceration on subsequent sexual HIV risk. Given the high occurrence of recidivism among criminal justice populations and the stress and hardship associated with criminal justice involvement, it is likely that repeated arrest or incarceration over the life course may have a cumulative impact on stress and health.56 Additionally, this study did not have the capacity to conduct interviews in incarceration settings; if men from the baseline sample were subsequently sentenced to long-term incarceration, they would likely be lost to follow-up. If, as this study suggests, low levels of criminal justice involvement have the potential to influence sexual risk-taking, then it is plausible that long-term incarcerations, which were not the focus of this study, may have even greater effects on high-risk sexual partnerships. Longer-term longitudinal studies which can assess effects of duration of incarceration on HIV risk behaviors over time are warranted.
In closing, this study builds on a relatively scant area of research that explores negative health effects associated with criminal justice involvement. Considering the economic and health costs of the ever-growing criminal justice system, a system that is increasingly described as problematic,53 it is an opportune time to aggressively consider alternative and complementary approaches to current criminal justice policy and practice. If, in fact, arrest and incarceration play a role in exacerbating sexual risk-taking, then exploring alternatives to incarceration and standard criminal justice sanctions may have distinct implications for improving sexual and public health. HIV/STI prevention research among criminal justice populations is a growing field—however, much work remains. Current models that target prisoners with long-term incarceration are an important area of research, but these efforts will not impact arrestees and others who spend little or no time in correctional facilities. The development of HIV/STI prevention efforts aimed at short-term jail incarcerations, reentry, and community settings will create a continuum of HIV prevention that reflects the complexity and breadth of the US criminal justice system.57–59 Building this HIV prevention continuum will require innovative collaborative efforts between criminal justice and community-based entities and the HIV prevention community.60 This approach is likely to improve the effectiveness of the criminal justice system in its stated goals of public safety and rehabilitation by bettering the public health of individuals and communities disproportionately impacted by involvement in the criminal justice system.
Acknowledgments
Dr. Epperson’s research is supported by a postdoctoral fellowship from the National Institute of Mental Health (NIMH) awarded to the Center for Behavioral Health Services & Criminal Justice Research (grant no. T32MH070313, P.I. Nancy Wolff). The parent study was supported by a National Institute on Drug Abuse (NIDA) grant awarded to P.I. Nabila El-Bassel (grant no. DA012335).
References
- 1.Seal DW. HIV-related issues and concerns for imprisoned persons throughout the world. Curr Opin Psychiatry. 2005;18:530–535. doi: 10.1097/01.yco.0000179492.08064.de. [DOI] [PubMed] [Google Scholar]
- 2.Boutwell A, Rich JD. HIV Infection Behind Bars. Clin Infect Dis. 2004;38:1761–1763. doi: 10.1086/421410. [DOI] [PubMed] [Google Scholar]
- 3.Braithwaite RL, Hammett T, Arriola KRJ. Introduction to the special issue: HIV/AIDS in correctional settings. AIDS Educ Prev. 2002;14:1–6. doi: 10.1521/aeap.14.7.1.23862. [DOI] [Google Scholar]
- 4.Braithwaite R, Stephens T, Treadwell H, Braithwaite K, Conerly R. Short-term impact of an HIV risk reduction intervention for soon-to-be-released inmates in Georgia. J Health Care Poor Underserved. 2005;16:130–139. doi: 10.1353/hpu.2005.0078. [DOI] [PubMed] [Google Scholar]
- 5.Maruschak LM. HIV in Prisons and Jails, 2002. Bur Justice Stat Bulletin. 2004;NCJ 205333:1–11.
- 6.Grinstead O, Zack B, Faigeles B, Grossman N, Blea L. Reducing postrelease HIV risk among male prison inmates: a peer-led intervention. Crim Justice Behav. 1999;26:453–465. doi: 10.1177/0093854899026004003. [DOI] [Google Scholar]
- 7.Margolis A, MacGowan R, Grinstead O, Sosman J, Kashif I, Flanigan T. Unprotected sex with multiple partners: implications for HIV prevention among young men with a history of incarceration. Sex Transm Dis. 2006;33:175–180. doi: 10.1097/01.olq.0000187232.49111.48. [DOI] [PubMed] [Google Scholar]
- 8.Johnson RC, Raphael S. The effects of male incarceration dynamics on AIDS infection rates among African-American women and men. Berkeley: University of California Press; 2006. [Google Scholar]
- 9.Blank MB, Eisenberg MM. HIV and mental illness: opportunities for prevention. J Prev Interv Community. 2007;33:1–4. doi: 10.1300/J005v33n01_01. [DOI] [PubMed] [Google Scholar]
- 10.Carey MP, Carey KB, Maisto SA. Prevalence and correlates of sexual activity and HIV-related risk behavior among psychiatric outpatients. J Consult Clin Psychol. 2001;69:846–850. doi: 10.1037/0022-006X.69.5.846. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Baillargeon JG. Psychiatric disorders, HIV infection and HIV/hepatitis co-infection in the correctional setting. AIDS Care. 2008;20:124–129. doi: 10.1080/09540120701426532. [DOI] [PubMed] [Google Scholar]
- 12.Braithwaite R, Stephens T. Use of protective barriers and unprotected sex among adult male prison inmates prior to incarceration. Int J STD AIDS. 2005;16:224–226. doi: 10.1258/0956462053420112. [DOI] [PubMed] [Google Scholar]
- 13.Karberg JC, James DJ. Substance dependence, abuse, and treatment of jail inmates, 2002. Bur Justice Stat Spec Rep. 2005;NCJ:1–12. [Google Scholar]
- 14.Wohl AR, Johnson DF, Lu S, et al. HIV risk behaviors among African American men in Los Angeles county who self-identify as heterosexual. J Acquir Immune Defic Syndr. 2002;31:354–360. doi: 10.1097/00126334-200211010-00013. [DOI] [PubMed] [Google Scholar]
- 15.McCoy CB, Lai S, Metsch LR, Messiah SE, Zhao W. Injection drug use and crack cocaine smoking: independent and dual risk behaviors for HIV infection. Ann Epidemiol. 2004;14:535–542. doi: 10.1016/j.annepidem.2003.10.001. [DOI] [PubMed] [Google Scholar]
- 16.Belenko S, Lin J, O’Connor L, Sung H, Lynch K. Sexual and physical victimization as predictors of HIV risk among felony drug offenders. AIDS Behav. 2005;9:311–323. doi: 10.1007/s10461-005-9005-2. [DOI] [PubMed] [Google Scholar]
- 17.MacGowan R, Margolis A, Gaiter J, et al. Predictors of risky sex of young men after release from prison. Int J STD AIDS. 2003;14:519–523. doi: 10.1258/095646203767869110. [DOI] [PubMed] [Google Scholar]
- 18.Hammet TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. Am J Public Health. 2002;92:1789–1794. doi: 10.2105/AJPH.92.11.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Thomas JC, Sampson LA. High rates of incarceration as a social force associated with community rates of sexually transmitted infection. J Infect Dis. 2005;191:S55–S60. doi: 10.1086/425278. [DOI] [PubMed] [Google Scholar]
- 20.Epperson M, El-Bassel N, Gilbert L, Orellana E, Chang M. Increased HIV risk associated with criminal justice involvement among men on methadone. AIDS Behav. 2008;12:51–57. doi: 10.1007/s10461-007-9298-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Marsch LA. The efficacy of methadone maintenance interventions in reducing illicit opiate use, HIV risk behavior and criminality: a meta-analysis. Addiction. 1998;93:515–532. doi: 10.1046/j.1360-0443.1998.9345157.x. [DOI] [PubMed] [Google Scholar]
- 22.Mays D, Gordon A, Kelly M, Forman S. Violent criminal behavior and perspectives on treatment of criminality in opiate treatment. Subst Abus. 2005;26:33–42. doi: 10.1300/J465v26n02_05. [DOI] [PubMed] [Google Scholar]
- 23.Gilbert L, El-Bassel N, Rajah V, Foleno A, Frye V. Linking drug related activities with experiences of partner violence: a focus group study of women in methadone treatment. Violence Vict. 2001;16:517–536. [PubMed] [Google Scholar]
- 24.El-Bassel N, Gilbert L, Golder S, et al. Deconstructing the relationship between intimate partner violence and sexual IPV risk among drug-involved men and their female partners. AIDS Behav. 2004;8:429–439. doi: 10.1007/s10461-004-7327-0. [DOI] [PubMed] [Google Scholar]
- 25.Derogatis LR, Melisaratos N. The brief symptom inventory: an introductory report. Psychol Med. 1983;13:596–605. doi: 10.1017/S0033291700048017. [DOI] [PubMed] [Google Scholar]
- 26.Miller B. Child sexual abuse interview. Buffalo: New York State Research Institute on Alcoholism and Addictions; 1990. [Google Scholar]
- 27.Bernstein DP, Fink L, Handelsman L, et al. Initial reliability and validity of a new retrospective measure of child abuse and neglect. Am J Psychiatry. 1994;151:1132–1136. doi: 10.1176/ajp.151.1.18. [DOI] [PubMed] [Google Scholar]
- 28.Royston P. Multiple imputation of missing values. The Stata Journal. 2004;4:227–241. [Google Scholar]
- 29.Rubin DB. Multiple Imputation for Nonresponse in Surveys. New York: Wiley; 1987. [Google Scholar]
- 30.Carlin J, Li N, Greenwood P, Coffey C. Tools for analyzing multiple imputed datasets. The Stata Journal. 2003;3:226–244. [Google Scholar]
- 31.Dehejia R, Wahba S. Propensity score-matching methods for nonexperimental causal studies. Rev Econ Stat. 2002;84:151–161. doi: 10.1162/003465302317331982. [DOI] [Google Scholar]
- 32.Rubin D, Thomas N. Combining propensity score matching with additional adjustments for prognostic covariates. J Am Stat Assoc. 2000;95:573–585. doi: 10.1080/01621459.2000.10474233. [DOI] [Google Scholar]
- 33.Werb D, Kerr T, Small W, Li K, Montaner J, Wood E. HIV risks associated with incarceration among injection drug users: implications for prison-based public health strategies. J Public Health. 2008;30:126–132. doi: 10.1093/pubmed/fdn021. [DOI] [PubMed] [Google Scholar]
- 34.Hammett TM, Roberts C, Kennedy S. Health-related issues in prisoner reentry. Crime Delinq. 2001;47:390–411. doi: 10.1177/0011128701047003006. [DOI] [Google Scholar]
- 35.Wheelock D, Uggen C. Race, poverty and punishment: the impact of criminal sanctions on racial, ethnic, and socioeconomic inequality. National Poverty Center, University of Michigan. 2005:15–16.
- 36.Blankenship KM, Smoyer AB, Bray SJ, Mattocks K. Black–White disparities in HIV/AIDS: the role of drug policy and the corrections system. J Health Care Poor Underserved. 2005;16:140–156. doi: 10.1353/hpu.2005.0077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wolff N, Draine J. Dynamics of social capital of prisoners and community reentry: ties that bind? J Correct Health Care. 2004;10:457. doi: 10.1177/107834580301000310. [DOI] [Google Scholar]
- 38.Latkin CA, Forman V, Knowlton A, Sherman S. Norms, social networks, and HIV-related risk behaviors among urban disadvantaged drug users. Soc Sci Med. 2003;56:465–476. doi: 10.1016/S0277-9536(02)00047-3. [DOI] [PubMed] [Google Scholar]
- 39.Rhodes T, Singer M, Bourgois P, Friedman SR, Strathdee SA. The social structural production of HIV risk among injecting drug users. Soc Sci Med. 2005;61:1026–1044. doi: 10.1016/j.socscimed.2004.12.024. [DOI] [PubMed] [Google Scholar]
- 40.El-Bassel N, Gilbert L, Wu E, Chang M. A social network profile and HIV risk among men on methadone: do social networks matter? J Urban Health. 2006;83:602–613. doi: 10.1007/s11524-006-9075-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Latkin CA, Knowlton AR. Micro-social structural approaches to HIV prevention: a social ecological perspective. AIDS Care. 2005;17:102–113. doi: 10.1080/09540120500121185. [DOI] [PubMed] [Google Scholar]
- 42.Arriola KRJ. Debunking the myth of the safe haven: toward a better understanding of intraprison HIV transmission. Criminol Public Policy. 2006;5:137–147. doi: 10.1111/j.1745-9133.2006.00108.x. [DOI] [Google Scholar]
- 43.Krebs CP, Simmons M. Intraprison HIV transmission: an assessment of whether it occurs, how it occurs, and who is at risk. AIDS Educ Prev. 2002;14:53–64. doi: 10.1521/aeap.14.7.53.23865. [DOI] [PubMed] [Google Scholar]
- 44.Krebs CP. Inmate factors associated with HIV transmission in prison. Criminol Public Policy. 2006;5:113–135. doi: 10.1111/j.1745-9133.2006.00101.x. [DOI] [Google Scholar]
- 45.Khan MR, Wohl DA, Weir SS, et al. Incarceration and risky sexual partnerships in a southern US city. J Urban Health. 2008;85:100–113. doi: 10.1007/s11524-007-9237-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Adimora A, Schoenbach V, Martinson F, Donaldson K, Stancil T, Fullilove R. Concurrent partnerships among rural African Americans with recently reported heterosexually transmitted HIV infection. J Acquir Immune Defic Syndr. 2003;34:423–429. doi: 10.1097/00126334-200312010-00010. [DOI] [PubMed] [Google Scholar]
- 47.Braithwaite RL, Arriola AR. Male prisoners and HIV prevention: a call for action ignored. Am J Public Health. 2003;93:759–763. doi: 10.2105/AJPH.93.5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Hammett TM, Gaiter JL, Crawford C. Reaching seriously at-risk populations: health interventions in criminal justice settings. Health Educ Behav. 1998;25:99–120. doi: 10.1177/109019819802500108. [DOI] [PubMed] [Google Scholar]
- 49.Inciardi JA, Surratt HL, Martin SS, O’Connell DJ, Salandy AD, Beard RA. Developing a multimedia HIV and hepatitis intervention for drug-involved offenders reentering the community. Prison J. 2007;87:111. doi: 10.1177/0032885506299045. [DOI] [Google Scholar]
- 50.Kalichman SC, Cain D, Weinhardt L, et al. Experimental components analysis of brief theory-based HIV/AIDS risk-reduction counseling for sexually transmitted infection patients. Health Psychol. 2005;24:198–208. doi: 10.1037/0278-6133.24.2.198. [DOI] [PubMed] [Google Scholar]
- 51.Rutledge SE. Single-session motivational enhancement counseling to support change toward reduction of HIV transmission by HIV positive persons. Arch Sex Behav. 2007;36:313–319. doi: 10.1007/s10508-006-9077-8. [DOI] [PubMed] [Google Scholar]
- 52.Baker A, Kochan N, Dixon F, Heather N, Woadk A. Controlled evaluation of a brief intervention of HIV prevention among injecting drug users not in treatment. AIDS Care. 1994;6:559–570. doi: 10.1080/09540129408258670. [DOI] [PubMed] [Google Scholar]
- 53.Golembeski C, Fullilove R. Criminal (in) justice in the city and its associated health consequences. Am J Public Health. 2005;95:1701–1706. doi: 10.2105/AJPH.2005.063768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Freudenberg N. Coming home from jail: a review of health and social problems facing US jail populations and of opportunities for reentry interventions. Washington: Urban Institute; 2006. [Google Scholar]
- 55.Link B, Phelan J. Social conditions as fundamental causes of disease. J Health Soc Behav. 1995;35:80–94. doi: 10.2307/2626958. [DOI] [PubMed] [Google Scholar]
- 56.Pearlin L, Schieman S, Fazio EM, Meersman SC. Stress, health, and the life course: some conceptual perspectives. J Health Soc Behav. 2005;46:205–219. doi: 10.1177/002214650504600206. [DOI] [PubMed] [Google Scholar]
- 57.Hammett TM, Harmon MP, Rhodes W. The burden of infectious disease among inmates of and releasees from US correctional facilities, 1997. Am J Public Health. 2002;92:1789–1794. doi: 10.2105/AJPH.92.11.1789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Vlahov D, Putnam S. From corrections to communities as an HIV priority. J Urban Health. 2006;83:339–348. doi: 10.1007/s11524-006-9041-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Freudenberg N. Jails, prisons, and the health of urban populations: a review of the impact of the correctional system on community health. J Urban Health. 2001;78:214–235. doi: 10.1093/jurban/78.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Grinstead OA, Zack B, Faigeles B. Collaborative research to prevent HIV among male prison inmates and their female partners. Health Educ Behav. 1999;26:225. doi: 10.1177/109019819902600206. [DOI] [PubMed] [Google Scholar]