Abstract
Background Insecticide-treated mosquito nets (ITNs) and indoor-residual spraying (IRS) are recommended strategies for preventing malaria in children. While their impact on all-cause child mortality is well documented, their impact on reducing malaria-attributable mortality has not been quantified. While the impact of intermittent preventive therapy in pregnant women (IPTp) and ITNs in pregnancy for improving birth outcomes is also well established, their impact on preventing neonatal or child mortality has not been quantified.
Methods We performed two systematic literature reviews in Plasmodium falciparum endemic settings; one to estimate the effect of ITNs and IRS on preventing malaria-attributable mortality in children 1–59 months, and another to estimate the effect of ITNs and IPTp on preventing neonatal and child mortality through improvements in birth outcomes.
Results We estimate the protective efficacy (PE) of ITNs and IRS on reducing malaria-attributable mortality 1–59 months to be 55%, with a range of 49–61%, in P. falciparum settings. We estimate malaria prevention interventions in pregnancy (IPTp and ITNs) to have a pooled PE of 35% (95% confidence interval: 23–45%) on reducing the prevalence of low birth weight (LBW) in the first or second pregnancy in areas of stable P. falciparum transmission.
Conclusion This systematic review quantifies the PE of ITNs for reducing malaria-attributable mortality in children, and the PE of IPTp and ITNs during pregnancy for reducing LBW. It is assumed the impact of IRS is equal to that of ITNs on reducing malaria-attributable mortality in children. These data will be used in the Lives Saved Tool (LiST) model for estimating the impact of malaria prevention interventions. These data support the continued scale-up of these malaria prevention interventions in endemic settings that will prevent a considerable number of child deaths due directly and indirectly to malaria.
Keywords: Systematic review, malaria prevention, child mortality, insecticide-treated mosquito nets, indoor-residual spraying, intermittent preventive therapy in pregnant women
Introduction
Approximately 1.38 billion people in the world are exposed to stable Plasmodium falciparum transmission, which is the species responsible for most malaria deaths.1 The bulk of the burden of malaria mortality in 2007 occurred among the estimated 108 million African children exposed to stable P. falciparum transmission.1 Malaria in sub-Saharan Africa was estimated to have caused over 800 000 child deaths in 2000.2
Fortunately, effective interventions for preventing malaria mortality in children are available and are being scaled-up across malaria endemic areas of Africa. These include insecticide-treated mosquito nets (ITNs), indoor-residual spraying (IRS) and intermittent preventive therapy in pregnant women (IPTp). Both ITNs and IRS prevent malaria transmission by reducing the chances that an individual will be bitten by an infective Anopheles mosquito. IPTp is the administration of two or more treatment doses of an effective antimalarial drug given at defined intervals during pregnancy of at least 1 month, regardless of whether the woman has a parasite infection at the time of treatment. It acts as treatment of existing infections (symptomatic or not) and as prophylaxis by limiting the development of infection for an interval of time in pregnancy.
ITNs and IRS are recommended strategies for preventing malaria in children with their impact on all-cause child mortality (ACCM) well demonstrated.3–7 Two ITN trials have attempted to assess the effect of ITNs on mortality due to malaria in children.8,9 However, these studies yielded non-significant results that were inconsistent with reductions in ACCM, likely because of misclassification bias from post-mortem verbal autopsies.10–12 Thus, their impact on reducing deaths due to malaria in children has not been well quantified. While IPTp and ITNs for preventing malaria in pregnancy and improving birth outcomes is also well established, their impact on preventing neonatal or child mortality has not been quantified. We performed systematic literature reviews to identify individual and community-randomized controlled trials to estimate the effect of ITNs and IRS on preventing malaria-attributable mortality, defined here as mortality due directly to malaria, in children 1–59 months (assuming no malaria deaths occur during the neonatal period), and to estimate the effect of ITNs and IPTp on preventing neonatal and child deaths through improvements in birth outcomes, in P. falciparum endemic settings.
Materials and methods
These reviews of effectives of the interventions are shaped in large part by the needs of the Lives Saved Tool (LiST) model. In that model, increases in coverage of an intervention results in a reduction of one or more cause-specific deaths or in reduction of a risk factor. Therefore, the reviews and the GRADE process used were designed to develop estimates of the effect of an intervention in reducing either a risk factor or a death due to specific cause. For more details of the review methods, the adapted grade approach or the LiST model see other articles in this supplement.
To quantify the protective effect of ITNs and IRS in preventing direct-malaria deaths in children, and for IPTp and ITNs among pregnant women in preventing neonatal and child deaths through improved birth outcomes, we conducted a systematic literature review to identify individual and community-randomized controlled trials using PUBMED, WHOLIS, CAB Abstracts via OVID Global Health, SIGLE and LILAC search engines. An attempt was made to identify unpublished studies through contact with experts in the field. Studies were limited to those implemented in areas of endemic P. falciparum malaria transmission. Where insufficient data from individual or community-randomized controlled trials could be identified, we included quasi-experimental and observational studies.
Data from studies meeting the inclusion criteria, as outlined below, were reviewed and data were abstracted into a standardized dataset. Extracted data included the following study characteristics: site, duration, target population, design, intervention definition, outcome definitions, raw data on outcomes of interest, study effect with 95% confidence intervals (CIs) and standard errors for each outcome, and any noted limitations or biases. The study quality was assessed according to the GRADE technique adapted by the Child Health Epidemiology Reference Group.13 Studies were grouped according to type of study outcome and study designs for meta-analysis using STATA 10.0. Meta-analyses are reported as the Mantel–Haenszel pooled relative risks (RRs) with accompanying 95% CIs. For community-randomized controlled trials, the empirically estimated standard errors as reported in the literature, either directly or estimated from 95% CIs, were used in the meta-analysis.
ITNs for children
We sought to measure the effect of ITNs in comparison with no mosquito net on child health outcomes in P. falciparum malaria endemic settings. To be included in this analysis, ITN trials had to measure one of the following outcomes among children under 5 years old: malaria-attributable mortality, all-cause mortality, incidence of severe or uncomplicated malaria or the prevalence of malaria parasite infection. Studies assessing the impact of insecticide-treated barriers for vector controls other than ITNs, such as insecticide-treated curtains, were excluded, as the LiST model only includes ITNs. A comprehensive and thorough Cochrane Review was performed through 2002 and published in 2004.3 Relevant data were included from the 2004 Cochrane Review, with our search focused on identifying eligible studies conducted after the inclusion dates of the Cochrane Review (post 2002). A combination of the following search terms was used: malaria, Plasmodium; bednet, mosquito net, ITN, LLIN, insecticide-treated, impregnated, permethrin, lambdacyhalothrin, deltamethrin and cyfulthrin. Studies that compared ITNs with untreated mosquito nets were excluded.
IRS
We sought studies that measured the effect of IRS compared with no spraying on child health outcomes related to malaria in P. falciparum malaria endemic settings. To be included in this analysis, IRS trials had to measure one of the following outcomes among children under 5 years old: malaria-attributable mortality, all-cause mortality, incidence of severe or uncomplicated malaria or the prevalence of malaria parasite infection. A combination of the following search terms was used: malaria, Plasmodium, IRS, insecticide, deltamethrin, Lambda-cyhalothrin, Icon, dichloro-diphenyl-trichloroethane and Bendiocarb. Studies that evaluated IRS plus another intervention (e.g. ITNs), for which the IRS-specific effect could not be isolated, were excluded.
Prevention of malaria during pregnancy related to improved birth outcomes
Intermittent preventive therapy in pregnant women
We sought studies that measured the effect of at least two doses per pregnancy of IPTp with sulphadoxine–pyrimethamine (SP) vs a placebo on child health outcomes within P. falciparum malaria endemic settings, independent of ITNs. For IPTp trials to be included in this analysis, one of the following outcomes had to be measured: intrauterine growth retardation (IUGR), pre-term delivery, prematurity, low birth weight (LBW), perinatal mortality, neonatal mortality, infant mortality or child mortality. Two comprehensive reviews have been published with data through 2006.14,15 In addition to relevant data from the Cochrane Review meeting the inclusion criteria, a literature search was conducted limited to studies published after 2006. A combination of search terms was used including: malaria, Plasmodium, sulphadoxine, pyrimethamine, IPT, IPTp, intermittent preventive treatment and pregnancy. Trials that compared two doses of IPTp to another drug (not a placebo) were excluded, as were trials that assessed IPTp compared with ITNs where the effect of IPTp against a placebo could not be isolated.
ITNs for pregnant women
We sought studies that measured the effect of access to ITNs among pregnant women vs no ITNs on child health outcomes within P. falciparum malaria endemic settings, independent of IPTp. For ITN trials to be included in this analysis, one of the following outcomes had to be measured: IUGR, pre-term birth, LBW, perinatal mortality, neonatal mortality, infant mortality or child mortality. Trials that compared ITNs with untreated nets were excluded, as were trials that assessed ITNs plus IPTp where the effect of ITNs against no mosquito net (placebo) could not be isolated. As a thorough and comprehensive systematic review was recently published with data through February 2009,16 we did not attempt to update their findings but reference those within the review that met our inclusion/exclusion criteria.
Deriving the impact of ITNs on malaria-attributable mortality in children from observed reductions in ACCM
While there are robust data for the protective efficacy (PE) of ITNs against ACCM among children 1–59 months,3 no such data are currently available on their impact of malaria-attributable mortality. It was therefore necessary to derive an estimate of the PE of ITNs for reducing malaria-attributable mortality (PEMAM) from ACCM thusly.
| (1) |
where PEACCM is equal to the PE (per cent) of ITNs in reducing ACCM among children aged x, and ß is equal to an estimate of the per cent of deaths from all-causes due to malaria among children aged x in areas without access to malaria prevention interventions. Due to the likelihood of misclassification bias where ß is estimated from post-mortem verbal autopsies,10–12 we present two methods.
The first approach used a pooled estimate of the PEACCM among children 1–59 months across trials, represented as PEACCM 1–59 m, and an aggregate estimate of ß based on the per cent of all <5 deaths across 20 countries with stable malaria transmission in sub-Saharan African in 2000 that were due directly to malaria, which was estimated to be 22.4% (95% CI 19.8–24.9%), represented here as ß<5.17 However, it was then necessary to remove neonatal deaths from this estimate of ß<5 to get the proportion of all deaths 1–59 months due to malaria, represented by ß1–59 m. It has previously been estimated that ∼26% of child deaths occurred during the first month of life in sub-Saharan Africa between 2000 and 2003.18 Assuming no malaria deaths occur during the neonatal period, ß1–59 m was estimated as the per cent of malaria deaths <5 (ß<5 = 22.4%)/(100–26%) or 30.2%. Using Equation (1), the PE of ITNs on direct malaria mortality 1–59 months (PEMAM 1–59 m) is estimated as: the pooled PEACCM 1–59/30.2%.
An alternative disaggregated approach uses estimates of PEACCM 1–59 and ß within each ITN trial study site rather than using a pooled estimate of the PEACCM among children 1–59 months across trials (PEACCM 1–59 m) and an aggregate estimate of ß under the general premise outlined previously. Using equation (1), an estimate of PEMAM 1–59 m within each study site is obtained as: PEACCM 1–59/ß1–59 m. As estimates of ß within each study were obtained from post-mortem verbal autopsies among all children <5 years old, ß1–59 m was estimated with the removal of neonatal deaths as outlined above. The resultant PEDMM 1–59 m (%) were then transformed to RRs (RR = [(100 − PE)/100] and pooled across trials with a meta-analysis weighted by the inverse standard error of the RR for ACCM reductions obtained by each trial.
Results
ITNs for children
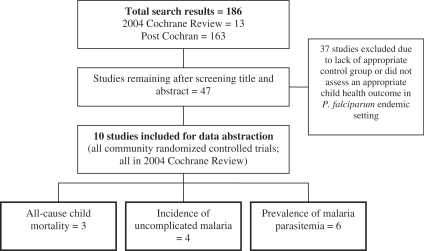
The Cochrane Review included 14 studies performed in stable P. falciparum endemic settings, all of which were conducted in sub-Saharan Africa. Ten of these studies included the effect of ITNs vs no nets with outcomes specific to children3 (Figure 1), of which three reported the effect of ITNs on ACCM8,19,20 (Supplementary Table 1). All of these trials used an intention-to-treat analysis for assessing the impact of ITNs on ACCM, where intervention villages were provided with high household ITN coverage (nearly 100%) and control villages received no ITNs. ITN use by children in these trials ranged from 50% to 97%, depending on the season. Four studies also reported the effect of ITNs on the incidence of uncomplicated malaria,21–24 while six reported the effect of ITNs on the prevalence of malaria parasitemia8,20,21,25–27 (Supplementary Table 1). Two trials that assessed the impact of ITNs on ACCM also attempted to assess their impact on malaria-attributable mortality; neither showed significant results.8,9 However, both were excluded from the 2004 Cochrane Review because of the likelihood of misclassification bias from post-mortem verbal autopsies that resulted in contradictory results with ACCM, which is a much more robust outcome measure. Both are also excluded here.
Figure 1.
Results of systematic review on the effect of ITNs on child health outcomes
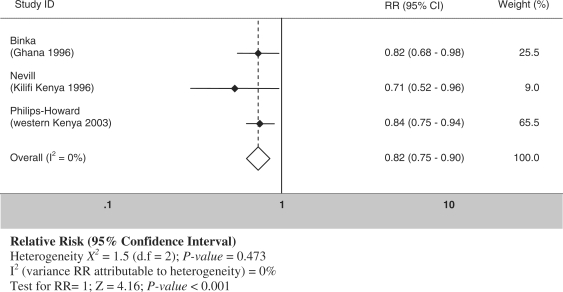
The systematic review of studies published after 2002 revealed 163 abstracts, of which 24 contained an outcome of interest. Only two of these studies were randomized trials, one limited to infants28 and one comparing ITNs to untreated nets.3 Both studies were therefore excluded. The resulting meta-analyses, which are largely consistent with the 2004 Cochrane Review without the inclusion of the trial assessing the impact of insecticide-treated curtains,29 show a PE of ITNs for reducing ACCM 1–59 months = 18% (RR = 0.82: 95% CI = 0.75–0.90) (Figure 2 and Table 1). Four trails show a PE of ITNs for reducing uncomplicated malaria incidence in children by 51% (RR = 0.49: 95% CI = 0.44–0.54), while six trials show a PE of ITN for reducing malaria parasite infection prevalence in children by 17% (RR = 0.83: 95% CI = 0.64–0.88) (Table 1).
Figure 2.
Forest plot for the meta-analysis of the effect of ITNs on reducing ACCM
Table 1.
Quality assessment of trials of the evidence for ITNs for preventing malaria deaths in children <5 years old
|
Quality assessment |
Summary findings |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Directness |
Intervention |
Control |
||||||||
| No. of studies | Design | Limitations | Consistency of results | Generalizability to population of interest | Generalizability to intervention of interest | No. of events | Denominator | No. of events | Denominator | Pooled RR (95% CI) |
| ACCM: high outcome-specific quality | ||||||||||
| 3 | CRCT | Not blinded | Consistent, χ2 for heterogeneity (2 df) = 1.5 | High | High | 1412 | 47 886 | 1709 | 48 152 | 0.82 (0.75–0.90) |
| Uncomplicated malaria incidence: high outcome-specific quality | ||||||||||
| 4 | CRCT | Not blinded | Inconsistent, χ2 for heterogeneity (3 df) = 9.39 | High | High | 543 | 30 602 | 1021 | 29 316 | 0.49a (0.44–0.54) |
| Prevalence of malaria parasite infection: high outcome-specific quality | ||||||||||
| 6 | CRCT | Not blinded | Inconsistent, χ2 for heterogeneity (6 df) = 83.5 | High | High | 2183 | 3921 | 2665 | 4093 | 0.83a (0.64–0.88) |
CRCT, community randomized controlled trial.
aRandom effects model.
Based on Rule 1,30 the PE of ITNs on reducing malaria-attributable mortality should therefore be derived from high quality evidence of reductions in ACCM. The first approach, as outlined in the materials and methods section, using the pooled estimate of the PEACCM among children 1–59 months across trials (PEACCM 1–59 m = 18%) and the aggregate proportion of all under five deaths due directly to malaria in 2000 1–59 months (ß1–59 m = 30.2%) yielded an estimate of the PE of ITNs at reducing malaria-attributable mortality 1–59 months = 60%. The second approach using the disaggregated method yielded a pooled PE of ITN at reducing malaria-attributable mortality 1–59 months = 49% (Table 2). Our best estimate therefore suggests that the PE of ITNs on malaria-attributable mortality 1–59 months ranges between 49% and 60%, with the point estimate for the LiST model being the mid-point of 55% (Box 1).
Table 2.
Disaggregated meta-analysis of ITN trials for estimating the PE of ITNs for preventing malaria deaths in children 1–59 months
| Study site/study year | RR for all cause child mortality 1–59 months (95% CI) | Standard error of the RR | PE at reducing ACCM 1–59 months (%) (95% CI) | Per cent of deaths from all causes due directly to malaria (ß)a (years) | Ref. | PE of ITNs on malaria- specific mortality (%) |
|---|---|---|---|---|---|---|
| Ghana (Kassena-Nankana) 1993–958 | 0.82 (0.68–0.98) | 0.093 | 18 | 41 (1993–95) | 8,62 | 44 |
| Kenya (Kilifi) 1993–9520 | 0.71 (0.52–0.96) | 0.157 | 29 | 46 (1991–93) | 62,63 | 63 |
| Kenya (Asembo/Gem) 1997–9919 | 0.84 (0.75–0.94) | 0.058 | 16 | 36 (1997–98) | 19,62 | 44 |
| Meta-analysis | 0.82 (0.75–0.90) | 18 (10–25) | 49b |
aß in Equation (1): per cent deaths from all causes due to malaria 1–59 months = per cent deaths from all causes due to malaria 0–59 months/74%; assuming no malaria deaths occur in the neonatal period and that 26% of deaths in children under five occur in the neonatal period18.
bRandom effects model; χ2 (2 df) = 6.3.
Box 1 Cause-specific mortality effect and quality grade of the estimate for the effect of ITNs and IRS.
Cause specific mortality to act on:
Malaria-attributable mortality among children 1–59 months.
Cause-specific effect and range:
55% (49–60%)
Quality of input evidence:
Moderate (three high-quality community-randomized controlled trials assessing ITNs on the reduction of ACCM 1–59 months).
These data are supported by data on the reduction of uncomplicated malaria incidence obtained from high-quality community-randomized controlled trials,21–24 as well as by cross-sectional studies assessing changes in the prevalence of malaria parasite infections under programme conditions.60
Proximity of the data to cause specific mortality effect:
Moderate (all-cause mortality 1–59 months).
Limitations of the evidence:
There were no randomized controlled trials on the impact of IRS. The PE for malaria-specific mortality 1–59 months had to be derived from ACCM with data on the proportion of all child deaths due to malaria coming from post-mortem verbal autopsies with known limitations.10,12,61
IRS
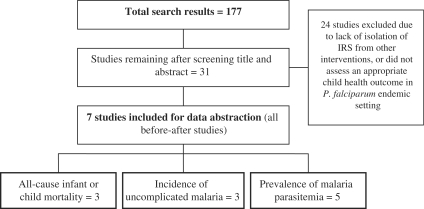
The literature review revealed 177 abstracts for IRS, of which 31 included outcomes of interest among children in P. falciparum endemic settings of sub-Saharan Africa (Figure 3). Seven studies met the inclusion criteria and are included in this analysis: three prior to 1976 and four since 1996 (Table 3).4–7,31–33 The only community-randomized controlled trial identified in the search was excluded because it was among refugees and therefore lacked external validity.34 Other studies with desired outcomes were excluded because they did not represent comparisons of IRS to control households, but included ITNs and other interventions. Two of the seven studies contained the outcome of IRS on ACCM,5,6 three contained all-cause infant mortality,5–7 three contained incidence of uncomplicated malaria7,31,32 and five contained the prevalence of malaria parasitemia in children6,31,32,35,36 (Supplementary Table 2).
Figure 3.
Results of systematic review on the effect of IRS on child health outcomes
Table 3.
Quality assessment of trials of the evidence for IRS to prevent malaria deaths in children <5 years old
|
Quality assessment |
Summary findings |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Directness |
Intervention |
Control |
||||||||
| No. of studies | Design | Limitations | Consistency | Generalizability to population of interest | Generalizability to intervention of interest | No. of events | Denominator | No. of events | Denominator | Pooled RR (95% CI) |
| ACCM: low outcome-specific quality | ||||||||||
| 2 | Before/after | Serious | χ2 for heterogeneity (1 df) = 11.8 | High | High | 190 | 2000 | 373 | 2000 | 0.53a (0.40–0.71) |
| All-cause infant mortality: low outcome-specific quality | ||||||||||
| 3 | Before-after | Serious | χ2 for heterogeneity (2 df) = 10.2 | High | High | 235 | 9542 | 477 | 9080 | 0.47a (0.40–0.54) |
| Uncomplicated malaria incidence: low outcome-specific quality | ||||||||||
| 3 | Before/after | Serious | χ2 for heterogeneity (2 df) > 100 | High | High | Unknown | Unknown | Unknown | Unknown | 0.25a (0.03–2.23) |
| Prevalence of malaria parasite infection: low outcome-specific quality | ||||||||||
| 5 | Before/after | Serious | χ2 for heterogeneity (4 df) > 100 | High | High | Unknown | Unknown | Unknown | Unknown | 0.16a (0.03–0.94) |
A limitation = serious means that there is a substantial threat of bias based on the study design used.
aRandom effects model.
While showing positive reductions in the malaria burden, all included studies evaluated the effect of IRS on child health outcomes using a pre/post-study design and therefore suffer from serious methodological weaknesses which limit internal validity and subsequent interpretation of results vis-à-vis IRS PE on malaria-attributable mortality (Table 3). Based on the fact that IRS impact on malaria morbidity has been shown to be similar to that of ITNs for which there are robust empirical data,37 IRS PE on malaria-specific mortality in the LiST model will be set equal to ITNs at 55% as described above.
Prevention of malaria during pregnancy related to improved birth outcomes
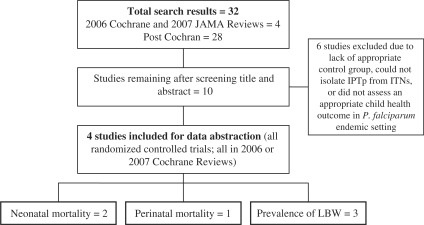
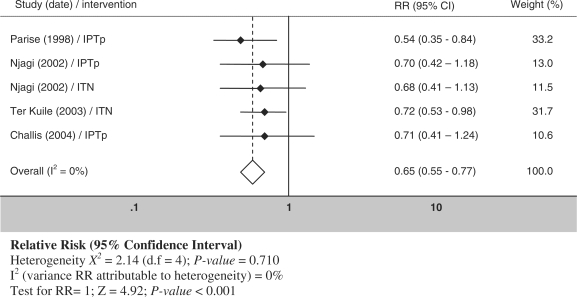
The 2006 Cochrane Review and the 2007 review for IPTp included four studies performed in areas of stable P. falciparum transmission which included the effect of IPTp vs placebo with outcomes specific to birth outcomes or child health.14,15 An additional literature search limited to articles published after the Cochrane Review (post 2006) revealed 23 abstracts; the only trial which contained an outcome of interest was excluded because it assessed the impact of IPTp +ITNs vs ITNs alone, where the effect of IPTp alone vs a placebo could not be isolated38 (Figure 4). Of the studies included here, two contained the outcome of neonatal mortality,39,40 one contained perinatal mortality40 and three contained the outcome of LBW prevalence (<2500 g)39,41,42 (Supplementaey Table 3). All were conducted in sub-Saharan Africa. The meta-analysis of data available from two randomized controlled trials shows no evidence of a statistically significant reduction in neonatal mortality among women in the first or second pregnancy (Table 4).14 The one study that assessed the impact of IPTp on perinatal mortality was also insignificant among women in the first or second pregnancy. Based on two randomized controlled trials, the 2006 Cochrane Review shows that IPTp, isolated from ITNs, significantly reduces the prevalence of LBW with an RR of 0.58 (95% CI: 0.43–0.78) among pregnant women in their first or second pregnancy. A more recent review containing three randomized controlled trials (the two previous trials in the 2006 Cochrane Review plus one additional trial) within the context of SP resistance and ITNs in sub-Saharan Africa found IPTp among women in their first or second pregnancy significantly reduces the prevalence of LBW with an RR of 0.71 (95% CI: 0.55–0.92). A meta-analysis limited to studies without ITNs shows that IPTp reduces the prevalence of LBW with an RR of 0.64 (95% CI: 0.56–0.72), resulting in IPTp having a PE of 36% (95% CI: 28–44%) independent of ITNs (data not shown).
Figure 4.
Results of systematic review on the effect of IPTp on child health outcomes
Table 4.
Quality assessment of trials of the evidence for IPTp and ITNs used during first or second pregnancy for preventing adverse birth outcomes and mortality
|
Quality assessment |
Summary findings |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Directness |
Intervention |
Control |
||||||||
| No. of studies | Design | Limitations | Consistency | Generalizability to population of interest | Generalizability to intervention of interest | No. of events | Denominator | No. of events | Denominator | Pooled RR (95% CI) |
| Neonatal mortality: IPTP: high outcome-specific quality | ||||||||||
| 2 | RCT | Consistent, χ2 for heterogeneity (1 df) = 0.96 | High | High | 25 | 1034 | 36 | 1057 | 0.62 (0.37–1.05) | |
| Perinatal mortality: IPTp: high outcome-specific quality | ||||||||||
| 1 | RCT | High | High | 44 | 432 | 58 | 472 | 0.83 (0.52–1.20) | ||
| LBW: IPTp and ITNs used during pregnancy: high outcome-specific quality | ||||||||||
| 5 (3 IPTp and 2 ITN) | RCT and CRCT | ITN trials not blinded | Consistent, χ2 for heterogeneity (4 df) = 2.14 | High | High | 139a | 1676a | 208a | 1684a | 0.65 (0.55–0.77) |
RCT, randomized controlled trial; CRCT, community randomized controlled trial.
aDatamissing for Njagi et al., 2003.41
Results from two trials included in the recently published 2009 Cochrane Review show access to ITNs, isolated from IPTp, to reduce LBW with an RR of 0.71 (95% CI: 0.54–0.92), suggesting that ITNs have a PE of 29% (95% CI: 8–46%) among women in the first or second pregnancy in areas of stable P. falciparum transmission, independent of IPTp.16,41,43 While the Njagi (2002) study used individual randomization and the ter Kuile (2003) study used community randomization, both assessed the impact of access to ITNs based on intention-to-treat, thus individual use was not assessed. There was no available evidence of ITNs preventing pre-term deliveries or neonatal mortality.
As the effects of IPTp and ITNs used during pregnancy have similar causal pathways for improving birth outcomes as measured by LBW, and as there is no evidence of a synergistic effect between them,38 the data were pooled with a meta-analysis to yield an RR of 0.65 (95% CI: 0.55–0.77) for reducing LBW from either IPTp or ITNs among women in the first or second pregnancy (Table 4 and Figure 5). A pooled PE point estimate of 35% is therefore suggested for use in the LiST model for malaria prevention during the first two pregnancies with either IPTp or ITNs for preventing LBW (Box 2).
Figure 5.
Forest plot for the meta-analysis of the effect of IPTp and ITNs used during first or second pregnancy for reducing LBW vs no IPTp (placebo) or ITNs
Box 2 PE estimate and quality grade of IPTp and ITNs used during pregnancy at reducing LBW.
Cause-specific outcome to act on:
LBW among first or second pregnancies.
Cause-specific effect and range:
35% (23–45%)
Quality of input evidence:
High (five high-quality randomized controlled trials assessing IPTp (3) and ITNs (2) on the reduction of LBW among a woman’s first two pregnancies).
Proximity of the data to cause-specific mortality effect:
Moderate (LBW in the LiST model acts through IUGR as a risk factor for neonatal and post-neonatal child mortality). However, there is robust evidence that LBW, due to IUGR and prematurity, increases the risk of neonatal and early infant mortality.50–52,59
Limitations of the evidence:
Ideally, the impact of IPTp and ITNs in pregnancy could be quantified on the outcome of neonatal and/or infant mortality. However, as of yet the pooled estimate for IPTp and ITNs for reducing neonatal mortality is no statistically significant as the trials were not powered to detect slight changes in this outcome. As data become available it will be important to quantify the effect of malaria prevention interventions during pregnancy on neonatal and child mortality.
Discussion
We performed a systematic review of the published and unpublished literature to quantify the best estimate for the PE of ITNs and IRS for preventing mortality due directly to malaria in children 1–59 months, and the effect of ITNs and IPTp on preventing neonatal and child deaths through improvements in birth outcomes, in P. falciparum endemic settings. Results will be used for the default settings of PE in the LiST model for estimating the number of child malaria deaths that can be prevented from scale-up of these malaria prevention interventions.
Based on the meta-analysis-derived PE of ITNs on ACCM 1–59 months of 18%, we estimate the PE of ITNs and IRS on reducing malaria-attributable mortality 1–59 months to be 55%, with a range of 49–61%. We surmise this may be a slight underestimate of the true impact of ITNs on reducing child mortality because the impact of ITNs ascertained by the trials were likely biased towards the null from the beneficial effect of ITNs to unprotected children in control villages as a result of their community effect.44
Two community-randomized controlled trials attempted to assess the impact of ITNs on malaria-attributable mortality.8,9 The trial from the Gambia showed a non-significant PE against child deaths due to malaria of 14%, while the trial from Ghana showed a non-significant reduction in PE of 22% against this outcome. These results are lower than expected and stand in contradiction to the trial results for the PE against ACCM of 23 and 18%, respectively, as well as compared with the results of this meta-analysis of an 18% PE of ITNs against ACCM. In light of these contradictions, we surmise error due to misclassification, which likely resulted in bias as well as increased variance about point estimates,10–12 limits the validity of these estimates from the Gambia and Ghana.
We used two methods to derive the PE of ITNs on malaria-attributable mortality based on their observed effect on ACCM. We surmise the first approach resulting in a PE of 60% yields the most robust estimate because the proportion of all deaths due to malaria was estimated across 31 studies within 14 countries with P. falciparum transmission between 1980 and 2000, thus it is likely less sensitive to systematic errors in post-mortem verbal autopsies as compared with the second method which was estimated across only three study sites in three countries.
We propose that the default coverage indicator for ITN and IRS in the LiST model use a composite indicator for the proportion of households protected by either intervention established from the following two indicators: the proportion of households with ≥1 ITN, and the proportion of households sprayed by IRS in the past 12 months.45 We suggest that ITN household possession be used instead of ITN use by children <5 for the following reasons. First, the trials from which the meta-analysis-derived 18% PE of ITNs on reducing ACCM 1–59 months were all based on intention-to-treat analyses, meaning the estimated RRs were based on whether or not a child lived in a village that was given ITNs or not; while use was measured separately within intervention villages, it never entered into the RR estimates. Second, ITN household possession captures the community effect of ITNs better than individual use. Third, ITN use among children ascertained by household surveys such as the Demographic and Health Survey and the Unicef Multiple Indicator Cluster Survey, which are implemented during the dry season, yield underestimates of use during higher transmission seasons.46–49 Fourth, use last night, as measured by household surveys, is likely the lowest measure of regular use over time. And last, use by a child under five likely underestimates use by anyone in the house, which is important vis-à-vis the ‘bait and kill’ effect that ITNs provide for reducing the overall abundance of Anopheles mosquitoes.
Our meta-analysis shows the PE of malaria prevention interventions in pregnancy (IPTp or ITNs) to have a pooled PE of 35% (95% CI: 23–45%) on reducing the prevalence of LBW in the first two pregnancies within areas of stable P. falciparum transmission. LBW has been shown to be associated with marked increases in neonatal and infant mortality.50–52 While LBW is due to either IUGR or pre-term delivery, the effect of malaria prevention interventions during pregnancy on LBW in the LiST model acts solely through IUGR with a 35% PE. Using IUGR as a proxy for LBW seems reasonable as it has been shown that IUGR is the predominant cause of LBW in settings of high malaria transmission.53,54 The effect of IUGR has two effects in the LiST model as noted elsewhere.30 First, children with IUGR have a greater RR of dying during the neonatal period, with increased RR of dying due to diarrhoea (RR = 2.0), sepsis/pneumonia (RR = 2.0) and asphyxia (RR = 2.3). Second, IUGR increases the chance that the child will be stunted, which in turn increases the RR for measles, malaria, diarrhoea and pneumonia deaths by ages in the post-neonatal period.
It should be noted that that malaria prevention during pregnancy shows a significant protective effect against perinatal mortality when two trials on regular prophylaxis are included in the analysis [RR = 0.73 (95% CI = 0.53–0.99)].14 One trial in the Gambia evaluated weekly pyrimethamine-dapsone provision55 while the other in Uganda assessed weekly chloroquine provision.56 However, we have chosen to omit these studies from the LiST model as continuous daily or weekly provision of antimalarials does not fit the definition of IPTp that is being implemented across stable P. falciparum malaria settings in sub-Saharan Africa.
Data from two randomized controlled trials show IPTp reduces neonatal mortality by 38% among women in the first or second pregnancy [RR = 0.62 (95% CI: 0.37–1.05)]; this result was not statistically significant as neither trial was powered to assess this outcome.39,40 This is supported by estimates that suggest LBW from malaria in pregnancy in areas of stable transmission account for as much as 11% of neonatal deaths and 6% of all infant deaths.52 Additionally, maternal malaria has been shown to be associated with increased risk of prematurity specifically, which has been shown to be associated with increased neonatal and early infant mortality.57–59 If this effect of IPTp/ITNs can be better quantified with additional data, from additional analyses of conducted randomized controlled trials or from observational data, its effect during pregnancy for reducing neonatal and infant mortality directly should be used in the LiST model instead of acting indirectly through IUGR. Until then, the effect of IPTp and ITNs on neonatal and early infant mortality, estimated through IUGR, will likely be underestimated in the LiST model.
We propose that the default coverage indicator in the LiST model for IPTp and ITNs used in pregnancy be comprised of a composite indicator for the proportion of pregnant women protected by either intervention established from the following two indicators: the proportion of women who received IPTp during antenatal care visits during their last pregnancy, and the proportion of pregnant women who slept under an ITN the previous night.45 In the LiST model for IPTp, the coverage indicator applies only to women in their first or second pregnancy in countries with stable P. falciparum transmission where IPTp is national policy. While the indicators for IPTp and ITNs are not contemporaneous, they are readily available from most national household surveys and approximate coverage of either intervention. However, the two studies that were used to quantify the effect of ITNs on birth outcomes used different units of randomization which has implications for selecting the appropriate coverage indicator for LiST.41,43 Njagi and colleagues (2002) randomized individual pregnant women to receive ITNs, which is much closer to assessing the individual effect of ITN use, while ter Kuile and colleagues (2003) randomized communities and thus their estimated PE is a result of whether or not a pregnant woman lived in a village with high ITN household possession. Thus, there is no perfect indicator of ITN coverage that matches both studies. For this reason, we have chosen to recommend ITN use (personal protection) over ITN household possession in the LiST model for assessing the impact of ITNs/IPTp on reducing LBW to be most conservative (i.e. ITN use is always lower than ITN household possession).
There are several limitations of using the LiST model to estimate the number of child malaria deaths that could be prevented through scale-up of prevention intervention coverage. First, the PE of ITNs and IRS is assumed constant across intervention coverage. Based on previous observations from the ITN trials, it is likely that the true protective effect of vector control interventions increases with increasing coverage due to a community effect, which at this point is unaccounted for in the LiST model.44 Second, the LiST model does not currently account for the PE of ITN/IRS scale-up on indirect malaria mortality where malaria is eliminated as a coinfection that contributes to a child death. This likely results in a significant underestimation of the true number of child deaths that could be prevented from malaria prevention intervention scale-up. Third, the coverage of interventions in the LiST model are assumed independent, while in reality it is likely people exposed to one malaria intervention are more likely to be exposed to other malaria interventions as a result of access to health care issues, resulting in an overestimate of impact. And last, the LiST model does not account for any possible synergistic effect between ITNs and IRS for preventing child malaria deaths. If data become available that show any such effects, the LiST model should account for this dimension on PE.
Unfortunately, birth and death registries are generally not available in most malaria-endemic countries for ascertaining changes in malaria-specific mortality. Until such data become available, the LiST model should be used to estimate the likely impact that is occurring across countries vis-à-vis prevention of child malaria deaths from intervention coverage scale-up. Additionally, there are now several rounds of population-based household surveys, such as the Demographic and Health Survey and the Multiple Indicator Cluster Survey, that allow the measurement of child survival intervention coverage and ACCM at two or more time points. As a result, the usefulness of the LiST model could potentially be gauged from comparison with empirical data on time trends in ACCM and intervention coverage from these surveys.
An additional systematic review focused on quantifying the PE of additional malaria interventions against child mortality that will be included in the LiST model is planned, including case management of uncomplicated and severe malaria and intermittent preventive therapy in infants. Additionally, future versions of the LiST model will include interventions that prevent miscarriage and stillbirths. As there is evidence that access to ITNs in the first or second pregnancy in areas of stable P. falciparum transmission prevents fetal loss (RR = 0.67, 95% CI = 0.47 – 0.97),16 this intervention will be incorporated into future versions of LiST for estimating this outcome.
Conclusions
This systematic review quantifies the PE of ITNs and IRS for reducing malaria-attributable mortality, and the PE of IPTp and ITNs during pregnancy for reducing LBW. These data support the continued scale-up of these malaria prevention interventions in endemic settings that will prevent a considerable number of child deaths due directly and indirectly to malaria. These PE estimates will allow the use of the LiST model for estimating the likely impact of past intervention scale-up, as well as for predicating future impact of intervention scale-up by national malaria control programmes.
Supplementary Data
Supplementary data are available at IJE online.
Funding
US Fund for UNICEF from the Bill & Melinda Gates Foundation (grant 43386) to ‘Promote evidence-based decision making in designing maternal, neonatal and child health interventions in low- and middle-income countries’.
Acknowledgements
This study was part of a large effort by the Child Health Epidemiology Reference Group to document the protective efficacies of child survival interventions for use in the LiST model. We thank all CHERG members for their comments, collaboration and encouragement throughout this process. We also thank Richard Cibulskis (WHO), Mac Otten (WHO), Alex Rowe [Centers for Disease Control and Prevention (CDC)], Steven Yoon (CDC), Meghna Desai (CDC), Larry Slutsker (CDC) and Jacek Skarbinski (CDC) for their thoughtful comments on the draft manuscript. The Department of International Health and Development, Tulane University School of Public Health and Tropical Medicine is also thanked for its support.
Conflict of interest: None declared.
KEY MESSAGES.
We estimate the protective efficacy of insecticide-treated mosquito nets and indoor-residual spraying on reducing malaria-attributable mortality 1–59 months to be 55%, with a range of 49–61%, in Plasmodium falciparum settings.
We estimate malaria prevention interventions in pregnancy (intermittent preventive therapy and insecticide-treated mosquito nets) to have a pooled protective efficacy of 35% (95% confidence interval: 23–45%) on reducing the prevalence of low birth weight in the first or second pregnancy in areas of stable Plasmodium falciparum transmission.
These data support the continued scale-up of these malaria prevention interventions in endemic settings that will prevent a considerable number of child deaths due directly and indirectly to malaria.
These protective efficacy estimates will allow the use of the LiST model for estimating the likely impact of past intervention scale-up, as well as for predicating future impact of intervention scale-up by national malaria control programs.
References
- 1.Hay SI, Guerra CA, Gething PW, et al. A world malaria map: Plasmodium falciparum endemicity in 2007. PLoS Med. 2009;6:e1000048. doi: 10.1371/journal.pmed.1000048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Rowe AK, Samantha YR, Robert WS, et al. The burden of malaria mortality among African children in the year 2000. Int J Epidemiol. 2006;35:691–704. doi: 10.1093/ije/dyl027. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Lengeler C. Insecticide-treated bed nets and curtains for preventing malaria. Cochrane Database Syst Rev. 2004;:CD000363. doi: 10.1002/14651858.CD000363.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Bradley D. Morbidity and mortality at Pare-Taveta, Kenya and Tanzania, 1954-66: the effects of a period of malaria control. In: Feachem R, Jamison D, editors. Disease and Mortality in sub-Saharan Africa. New York: University Oxford Press; 1991. pp. 248–63. [Google Scholar]
- 5.Molineaux L, Gramiccia G. The Garki Project: Research on the Epidemiology and Control of Malaria in the Sudan Savanna of West Africa. Geneva: WHO; 1980. [Google Scholar]
- 6.Pringle G. Malaria in the Pare area of Tanzania. 3. The course of malaria transmission since the suspension of an experimental programme of residual insecticide spraying. Trans R Soc Trop Med Hyg. 1967;61:69–79. doi: 10.1016/0035-9203(67)90055-7. [DOI] [PubMed] [Google Scholar]
- 7.Payne D, Grab B, Fontaine RE, Hempel JH. Impact of control measures on malaria transmission and general mortality. Bull World Health Organ. 1976;54:369–77. [PMC free article] [PubMed] [Google Scholar]
- 8.Binka FN, Kubaje A, Adjuik M, et al. Impact of permethrin impregnated bednets on child mortality in Kassena-Nankana district, Ghana: a randomized controlled trial. Trop Med Int Health. 1996;1:147–54. doi: 10.1111/j.1365-3156.1996.tb00020.x. [DOI] [PubMed] [Google Scholar]
- 9.D'Alessandro U, Olaleye BO, McGuire W, et al. Mortality and morbidity from malaria in Gambian children after introduction of an impregnated bednet programme. Lancet. 1995;345:479–83. doi: 10.1016/s0140-6736(95)90582-0. [DOI] [PubMed] [Google Scholar]
- 10.Todd JE, De Francisco A, O'Dempsey TJ, Greenwood BM. The limitations of verbal autopsy in a malaria-endemic region. Ann Trop Paediat. 1994;14:31–6. doi: 10.1080/02724936.1994.11747689. [DOI] [PubMed] [Google Scholar]
- 11.Chandramohan D, Setel P, Quigley M. Effect of misclassification of causes of death in verbal autopsy: can it be adjusted? Int J Epidemiol. 2001;30:509–14. doi: 10.1093/ije/30.3.509. [DOI] [PubMed] [Google Scholar]
- 12.Mobley CC, Boerma JT, Titus S, Lohrke B, Shangula K, Black RE. Validation study of a verbal autopsy method for causes of childhood mortality in Namibia. J Trop Pediat. 1996;42:365–69. doi: 10.1093/tropej/42.6.365. [DOI] [PubMed] [Google Scholar]
- 13.Atkins D, Best D, Briss PA, et al. Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Garner P, Gulmezoglu AM. Drugs for preventing malaria in pregnant women. Cochrane Database Syst Rev. 2006;:CD000169. doi: 10.1002/14651858.CD000169.pub2. [DOI] [PubMed] [Google Scholar]
- 15.ter Kuile FO, van Eijk AM, Filler SJ. Effect of sulfadoxine-pyrimethamine resistance on the efficacy of intermittent preventive therapy for malaria control during pregnancy: a systematic review. JAMA. 2007;297:2603–16. doi: 10.1001/jama.297.23.2603. [DOI] [PubMed] [Google Scholar]
- 16.Gamble CL, Ekwaru JP, ter Kuile FO. Insecticide-treated nets for preventing malaria in pregnancy (Review) Cochrane Database Syst Rev. 2009;2:1–51. [Google Scholar]
- 17.Rowe AK, Steketee RW. Predictions of the impact of malaria control efforts on all-cause child mortality in sub-Saharan Africa. Am J Trop Med Hyg. 2007;77:48–55. [PubMed] [Google Scholar]
- 18.Bryce J, Boschi-Pinto C, Shibuya K, Black RE. WHO estimates of the causes of death in children. Lancet. 2005;365:1147–52. doi: 10.1016/S0140-6736(05)71877-8. [DOI] [PubMed] [Google Scholar]
- 19.Phillips-Howard PA, Nahlen BL, Kolczak MS, et al. Efficacy of permethrin-treated bed nets in the prevention of mortality in young children in an area of high perennial malaria transmission in western Kenya. Am J Trop Med Hyg. 2003;68:23–9. [PubMed] [Google Scholar]
- 20.Nevill CG, Some ES, Mung'ala VO, et al. Insecticide-treated bednets reduce mortality and severe morbidity from malaria among children on the Kenyan coast. Trop Med Int Health. 1996;1:139–46. doi: 10.1111/j.1365-3156.1996.tb00019.x. [DOI] [PubMed] [Google Scholar]
- 21.Henry MC, Assi SB, Rogier C, et al. Protective efficacy of lambda-cyhalothrin treated nets in Anopheles gambiae pyrethroid resistance areas of Cote d'Ivoire. Am J Trop Med Hyg. 2005;73:859–64. [PubMed] [Google Scholar]
- 22.Marbiah NT, Petersen E, David K, Magbity E, Lines J, Bradley DJ. A controlled trial of lambda-cyhalothrin-impregnated bed nets and/or dapsone/pyrimethamine for malaria control in Sierra Leone. Am J Trop Med Hyg. 1998;58:1–6. doi: 10.4269/ajtmh.1998.58.1. [DOI] [PubMed] [Google Scholar]
- 23.Sexton JD, Ruebush II TK, Brandling-Bennett AD, et al. Permethrin-impregnated curtains and bed-nets prevent malaria in Western Kenya. Am J Trop Med Hyg. 1990;43:11–8. doi: 10.4269/ajtmh.1990.43.11. [DOI] [PubMed] [Google Scholar]
- 24.ter Kuile FO, Terlouw DJ, Kariuki SK, et al. Impact of permethrin-treated bed nets on malaria, anemia, and growth in infants in an area of intense perennial malaria transmission in western Kenya. Am J Trop Med Hyg. 2003;68:68–77. [PubMed] [Google Scholar]
- 25.Fraser-Hurt N, Felger I, Edoh D, et al. Effect of insecticide-treated bed nets on haemoglobin values, prevalence and multiplicity of infection with Plasmodium falciparum in a randomized controlled trial in Tanzania. Trans R Soc Trop Med Hyg. 1999;93(Suppl 1):47–51. doi: 10.1016/s0035-9203(99)90327-9. [DOI] [PubMed] [Google Scholar]
- 26.Moyou-Somo R, Lehman LG, Awahmukalah S, Ayuk Enyong P. Deltamethrin impregnated bednets for the control of urban malaria in Kumba Town, South-West Province of Cameroon. J Trop Med Hyg. 1995;98:319–24. [PubMed] [Google Scholar]
- 27.ter Kuile FO, Terlouw DJ, Phillips-Howard PA, et al. Impact of permethrin-treated bed nets on malaria and all-cause morbidity in young children in an area of intense perennial malaria transmission in western Kenya: cross-sectional survey. Am J Trop Med Hyg. 2003;68:100–7. [PubMed] [Google Scholar]
- 28.Etang J, Chouaibou M, Toto JC, et al. A preliminary test of the protective efficacy of permethrin-treated bed nets in an area of Anopheles gambiae metabolic resistance to pyrethroids in north Cameroon. Trans R Soc Trop Med Hyg. 2007;101:881–84. doi: 10.1016/j.trstmh.2007.05.012. [DOI] [PubMed] [Google Scholar]
- 29.Habluetzel A, Diallo DA, Esposito F, et al. Do insecticide-treated curtains reduce all-cause child mortality in Burkina Faso? Trop Med Int Health. 1997;2:855–62. doi: 10.1046/j.1365-3156.1997.d01-413.x. [DOI] [PubMed] [Google Scholar]
- 30.Friberg IK, Bhutta ZA, Darmstadt GL, et al. Comparing modelled predictions of neonatal mortality impacts using LiST with observed results of community-based intervention trials in South Asia. Int J Epidemiol. 2010;39(Suppl 1):i11–20. doi: 10.1093/ije/dyq017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Kleinschmidt I, Sharp B, Benavente LE, et al. Reduction in infection with Plasmodium falciparum one year after the introduction of malaria control interventions on Bioko Island, Equatorial Guinea. Am J Trop Med Hyg. 2006;74:972–78. [PubMed] [Google Scholar]
- 32.Protopopoff N, Van Bortel W, Marcotty T, et al. Spatial targeted vector control is able to reduce malaria prevalence in the highlands of Burundi. Am J Trop Med Hyg. 2008;79:12–8. [PubMed] [Google Scholar]
- 33.Teklehaimanot HD, Teklehaimanot A, Kiszewski A, Rampao HS, Sachs JD. Malaria in Sao Tome and principle: on the brink of elimination after three years of effective antimalarial measures. Am J Trop Med Hyg. 2009;80:133–40. [PubMed] [Google Scholar]
- 34.Charlwood JD, Qassim M, Elnsur EI, et al. The impact of indoor residual spraying with malathion on malaria in refugee camps in eastern Sudan. Acta Tropica. 2001;80:1–8. doi: 10.1016/s0001-706x(01)00152-8. [DOI] [PubMed] [Google Scholar]
- 35.Romi R, Razaiarimanga MC, Raharimanga R, et al. Impact of the malaria control campaign (1993-1998) in the highlands of Madagascar: parasitological and entomological data. Am J Trop Med Hyg. 2002;66:2–6. doi: 10.4269/ajtmh.2002.66.2. [DOI] [PubMed] [Google Scholar]
- 36.Sharp BL, Ridl FC, Govender D, Kuklinski J, Kleinschmidt I. Malaria vector control by indoor residual insecticide spraying on the tropical island of Bioko, Equatorial Guinea. Malaria J. 2007;6:52. doi: 10.1186/1475-2875-6-52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Guyatt HL, Corlett SK, Robinson TP, Ochola SA, Snow RW. Malaria prevention in highland Kenya: indoor residual house-spraying vs. insecticide-treated bednets. Trop Med Int Health. 2002;7:298–303. doi: 10.1046/j.1365-3156.2002.00874.x. [DOI] [PubMed] [Google Scholar]
- 38.Menendez C, Bardaji A, Sigauque B, et al. A randomized placebo-controlled trial of intermittent preventive treatment in pregnant women in the context of insecticide treated nets delivered through the antenatal clinic. PLoS ONE. 2008;3:e1934. doi: 10.1371/journal.pone.0001934. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Parise ME, Ayisi JG, Nahlen BL, et al. Efficacy of sulfadoxine-pyrimethamine for prevention of placental malaria in an area of Kenya with a high prevalence of malaria and human immunodeficiency virus infection. Am J Trop Med Hyg. 1998;59:813–22. doi: 10.4269/ajtmh.1998.59.813. [DOI] [PubMed] [Google Scholar]
- 40.Shulman CE, Dorman EK, Cutts F, et al. Intermittent sulphadoxine-pyrimethamine to prevent severe anaemia secondary to malaria in pregnancy: a randomized placebo-controlled trial. Lancet. 1999;353:632–36. doi: 10.1016/s0140-6736(98)07318-8. [DOI] [PubMed] [Google Scholar]
- 41.Njagi JK, Magnussen P, Estambale B, Ouma J, Mugo B. Prevention of anaemia in pregnancy using insecticide-treated bednets and sulfadoxine-pyrimethamine in a highly malarious area of Kenya: a randomized controlled trial. Trans R Soc Trop Med Hyg. 2003;97:277–82. doi: 10.1016/s0035-9203(03)90141-6. [DOI] [PubMed] [Google Scholar]
- 42.Challis K, Osman NB, Cotiro M, Nordahl G, Dgedge M, Bergstrom S. Impact of a double dose of sulphadoxine-pyrimethamine to reduce prevalence of pregnancy malaria in southern Mozambique. Trop Med Int Health. 2004;9:1066–73. doi: 10.1111/j.1365-3156.2004.01307.x. [DOI] [PubMed] [Google Scholar]
- 43.ter Kuile FO, Terlouw DJ, Phillips-Howard PA, et al. Reduction of malaria during pregnancy by permethrin-treated bed nets in an area of intense perennial malaria transmission in western Kenya. Am J Trop Med Hyg. 2003;68:50–60. [PubMed] [Google Scholar]
- 44.Hawley WA, Phillips-Howard PA, ter Kuile FO, et al. Community-wide effects of permethrin-treated bed nets on child mortality and malaria morbidity in western Kenya. Am J Trop Med Hyg. 2003;68:121–27. [PubMed] [Google Scholar]
- 45.Roll Back Malaria. Guidelines for Core Population-Based Indicators. Calverton, MD: Roll Back Malaria, MEASURE Evaluation, World Health Organization, UNICEF; 2008. [Google Scholar]
- 46.Binka FN, Adongo P. Acceptability and use of insecticide impregnated bednets in northern Ghana. Trop Med Int Health. 1997;2:499–507. [PubMed] [Google Scholar]
- 47.Alaii JA, Hawley WA, Kolczak MS, et al. Factors affecting use of permethrin-treated bed nets during a randomized controlled trial in western Kenya. Am J Trop Med Hyg. 2003;68:137–41. [PubMed] [Google Scholar]
- 48.Monasch R, Reinisch A, Steketee RW, Korenromp EL, Alnwick D, Bergevin Y. Child coverage with mosquito nets and malaria treatment from population-based surveys in African countries: a baseline for monitoring progress in roll back malaria. Am J Trop Med Hyg. 2004;71:232–38. [PubMed] [Google Scholar]
- 49.Korenromp EL, Miller J, Cibulskis RE, Kabir Cham M, Alnwick D, Dye C. Monitoring mosquito net coverage for malaria control in Africa: possession vs. use by children under 5 years. Trop Med Int Health. 2003;8:693–703. doi: 10.1046/j.1365-3156.2003.01084.x. [DOI] [PubMed] [Google Scholar]
- 50.Steketee RW, Nahlen BL, Parise ME, Menendez C. The burden of malaria in pregnancy in malaria-endemic areas. Am J Trop Med Hyg. 2001;64:28–35. doi: 10.4269/ajtmh.2001.64.28. [DOI] [PubMed] [Google Scholar]
- 51.Greenwood AM, Armstrong JR, Byass P, Snow RW, Greenwood BM. Malaria chemoprophylaxis, birth weight and child survival. Trans R Soc Trop Med Hyg. 1992;86:483–85. doi: 10.1016/0035-9203(92)90078-q. [DOI] [PubMed] [Google Scholar]
- 52.Guyatt HL, Snow RW. Malaria in pregnancy as an indirect cause of infant mortality in sub-Saharan Africa. Trans R Soc Trop Med Hyg. 2001;95:569–76. doi: 10.1016/s0035-9203(01)90082-3. [DOI] [PubMed] [Google Scholar]
- 53.Desai M, ter Kuile FO, Nosten F, et al. Epidemiology and burden of malaria in pregnancy. Lancet Infect Dis. 2007;7:93–104. doi: 10.1016/S1473-3099(07)70021-X. [DOI] [PubMed] [Google Scholar]
- 54.Watkinson M, Rushton DI. Plasmodial pigmentation of placenta and outcome of pregnancy in West African mothers. Br Med J (Clin Res Ed) 1983;287:251–54. doi: 10.1136/bmj.287.6387.251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Greenwood BM, Greenwood AM, Snow RW, Byass P, Bennett S, Hatib-N'Jie AB. The effects of malaria chemoprophylaxis given by traditional birth attendants on the course and outcome of pregnancy. Trans R Soc Trop Med Hyg. 1989;83:589–94. doi: 10.1016/0035-9203(89)90362-3. [DOI] [PubMed] [Google Scholar]
- 56.Ndyomugyenyi R, Magnussen P. Chloroquine prophylaxis, iron-folic acid supplementation or case management of malaria attacks in primigravidae in western Uganda: effects on maternal parasitaemia and haemoglobin levels and on birthweight. Trans R Soc Trop Med Hyg. 2000;94:413–18. doi: 10.1016/s0035-9203(00)90125-1. [DOI] [PubMed] [Google Scholar]
- 57.Steketee RW, Wirima JJ, Hightower AW, Slutsker L, Heymann DL, Breman JG. The effect of malaria and malaria prevention in pregnancy on offspring birthweight, prematurity, and intrauterine growth retardation in rural Malawi. Am J Trop Med Hyg. 1996;55:33–41. doi: 10.4269/ajtmh.1996.55.33. [DOI] [PubMed] [Google Scholar]
- 58.Menendez C, Ordi J, Ismail MR, et al. The impact of placental malaria on gestational age and birth weight. J Infect Dis. 2000;181:1740–45. doi: 10.1086/315449. [DOI] [PubMed] [Google Scholar]
- 59.Barros FC, Huttly SR, Victora CG, Kirkwood BR, Vaughan JP. Comparison of the causes and consequences of prematurity and intrauterine growth retardation: a longitudinal study in southern Brazil. Pediat. 1992;90:238–44. [PubMed] [Google Scholar]
- 60.Zambia Ministry of Health. Zambia National Malaria Indicator Survey 2008 Lusaka, Zambia: Zambia Ministry of Health; 2008. [Google Scholar]
- 61.Snow RW, Armstrong JR, Forster D, et al. Childhood deaths in Africa: uses and limitations of verbal autopsies. Lancet. 1992;340:351–55. doi: 10.1016/0140-6736(92)91414-4. [DOI] [PubMed] [Google Scholar]
- 62.Rowe AK, Rowe SY, Snow R, et al. Estimates of the burden of mortality directly attributable to malaria for children under 5 years of age in Africa for the year 2000 Final report. For the Child Health Epidemiology Reference Group (CHERG) Washington DC: Child Health Epidemiology Reference Group (CHERG);; 2006. [Google Scholar]
- 63.Korenromp EL, Williams BG, Gouws E, Dye C, Snow RW. Measurement of trends in childhood malaria mortality in Africa: an assessment of progress toward targets based on verbal autopsy. Lancet Infect Dis. 2003;3:349–58. doi: 10.1016/s1473-3099(03)00657-1. [DOI] [PubMed] [Google Scholar]