Abstract
Background
Primary hyperparathyroidism (PHPT) is associated with an increased risk of cardiovascular disease, including hypertension. The purpose of this study was to determine the effect of parathyroidectomy on systolic and diastolic blood pressures (BP) in hypertensive patients with PHPT.
Methods
A retrospective review of medical records was performed in 368 patients undergoing parathyroidectomy and 96 patients undergoing thyroidectomy by a single surgeon. We evaluated changes in serum calcium, parathyroid hormone (PTH), and BP before and 6 months after surgery.
Results
In patients undergoing parathyroidectomy with hypertension (n = 147), a significant decrease in both systolic and diastolic BP was observed; systolic BP decreased from 152.5 ± 10.5 to 140.3 ± 16.2 mmHg (P < .001) and diastolic BP decreased from 94.5 ± 6.8 to 81.7 ± 10.3 mmHg (P < .001). In these patients, PTH decreased from 136 ± 186 to 58.7 ± 44.3 pg/mL (P < .001) and serum calcium decreased from 11.1 ± 0.6 to 9.5 ± 0.7 mg/dL (P < .001). In patients undergoing parathyroidectomy without hypertension (n = 145) and thyroidectomy alone (n = 96), no significant change in systolic or diastolic BP was observed.
Conclusion
Parathyroidectomy in hypertensive patients seems to reduce both systolic and diastolic BP . The mechanisms responsible for this effect are unknown and deserve further study.
Primary hyperparathyroidism (PHPT) is a common endocrine condition characterized by oversecretion of parathyroid hormone (PTH). PHPT can lead to bone loss and pain, nephrolithiasis, gastrointestinal disturbances, and neuromuscular and cognitive dysfunction.1,2
Earlier studies have suggested an association between hyperparathyroidism and hypertension. A majority of patients with PHPT have been reported to have hypertension3; patients with hypertension have also been reported to have elevated PTH levels compared with normotensive patients.4 The mechanism by which hyperparathyroidism might effect blood pressure (BP) is unknown. The effect of parathyroidectomy on BP has been inconsistent in literature. Some studies have found a reduction in BP,5,6 whereas others have demonstrated no significant change in BP.7,8
In this study, we performed a retrospective review of medical records from a single medical center, over a 10-year period, to determine whether parathyroidectomy was associated with improvement in BP in patients with PHPT. We also examined the records of hypertensive patients undergoing thyroidectomy for nontoxic thyroid disease as a control group.
METHODS
Study patients
We obtained approval from the Emory University Institutional Review Board to conduct our study. We reviewed the records of patients who were ≥16 years and undergoing parathyroidectomy for PHPT or thyroidectomy for nontoxic thyroid disease at Emory University Hospital from 1997 to 2006. All of the operations were performed by a single endocrine surgeon during this time period.
Study protocol
We collected demographic information including age, gender, body mass index, ethnicity and current medications. In patients undergoing a parathyroidectomy, we recorded preoperative and postoperative PTH, calcium, albumin, and systolic and diastolic BP. The postoperative BP was taken on a single postoperative visit at a scheduled 6-month follow-up visit (range, 4–7). The BP was taken by our nursing staff with an automated cuff while the patient was seated. In patients undergoing thyroidectomy, we recorded preoperative and postoperative systolic and diastolic BP. Patients with stage I hypertension (systolic BP ≥140 or diastolic BP ≥90) or greater were included in the hypertensive arm of the study. We excluded patients who (1) had changes in antihypertensive medications during the pre-operative study period; (2) were referred pre-operatively to cardiology for control of BP; (3) had a systolic BP >200; (4) required repeat parathyroid surgery; or (5) had secondary or tertiary hyperparathyroidism.
Statistical analysis
Statistical evaluation of the results was performed by using Microsoft Excel 2008 (Seattle, WA) and Graph Pad Prism 5 (La Jolla, CA). We used descriptive statistics to summarize data on systolic BP, diastolic BP, PTH, and calcium. The differences between the pre-operative and postoperative mean values were evaluated using the Student paired t test. P ≤.05 was considered significant.
RESULTS
We reviewed the records of 368 patients with PHPT who underwent parathyroidectomy at Emory University Hospital between 1997 and 2006. The demographics of all of the patients undergoing parathyroidectomy are presented in Table I.
Table I.
Demographic of patients undergoing parathyroidectomy for primary hyperparathyroidism at Emory University Hospital (1997–2006)
| Group | Value |
|---|---|
| All patients with PHPT (n = 368) | |
| Age (yrs) | 52 ± 13 |
| Gender, n (%) | |
| Male | 132 (35.7) |
| Female | 236 (64.3) |
| Ethnicity, n (%) | |
| Non-Hispanic white | 224 (60.9) |
| Non-Hispanic black | 90 (24.4) |
| Other | 54 (14.7) |
| BMI mean (kg/ m2) | 29.6 ± 6.6 |
| eGFR | 81.8 ± 12.0 |
| Hypertensive patients* (n = 147) | |
| Age (yrs) | 56 ± 14 |
| Gender, n (%) | |
| Male | 43 (29.3) |
| Female | 104 (70.7) |
| Ethnicity (n) | |
| Non-Hispanic white | 78 (53.1) |
| Non-Hispanic black | 53 (36.1) |
| Other | 16 (10.9) |
| BMI mean (kg/ m2) | 29.7 ± 7.0 |
| eGFR | 87.8 ± 46.0 |
| Antihypertensive use in hyperparathyroid patients with hypertension (n = 116)† |
|
| ACEI | 35.3% (41) |
| α-blocker (central) | 9.5% (11) |
| α-blocker (peripheral) | 2.6% (3) |
| ARB | 19.0% (22) |
| β-blocker | 37.9% (44) |
| CCB | 44.8% (52) |
| Diuretics | 31.9% (37) |
| Vasodilators | 3.4% (4) |
Hypertension defined as systolic blood pressure ≥ 120 and diastolic blood pressure ≥ 80; includes subjects with primary hyperparathyroidism, secondary hyperparathyroidism, and tertiary hyperparathyroidism.
Total may equal >100%.
Results are presented as mean values ± SD, unless otherwise noted. ACEI, Angiotensin-converting enzyme inhibitor; CCB, calcium channel blocker; eGFR, estimated glomerular filtration rate (calculated by the Modification of Diet in Renal Disease method).
We identified 196 of the subjects with PHPT with at least stage 1 hypertension. We further excluded 49 patients who were referred to cardiology for management of BP or had adjustment of their antihypertensive regimen pre-operatively, with 147 patients remaining for our final analysis in the hypertensive arm of the study. In our study population, 116 patients were currently taking antihypertensive medications. The medications that the patients were taking are presented in Table I.
Calcium and PTH levels
Calcium and PTH levels significantly decreased in all hypertensive patients with a cure rate of 99.1% (Table II). This pattern was also seen in patients with hypertension who were currently treated with antihypertensive medications (Table III). Among the subset of patients with no change or increase in BP after surgery there was a significant decrease in PTH but a nonsignificant decrease in calcium levels (Table IV).
Table II.
Operative outcomes in all hypertensive patients (systolic BP ≥140 and diastolic BP ≥90; n = 147*s) with primary hyperparathyroidism
| Pre-operatively | Postoperatively | P value | |
|---|---|---|---|
| PTH (pg/mL) | 136 ± 186 | 58.7 ± 44.3 | <.001 |
| Calcium (mg/dL) | 11.0 ± 0.6 | 9.5 ± 0.7 | <.001 |
| Systolic BP (mmHg) | 152.5 ± 10.5 | 140.3 ± 16.2 | <.001 |
| Diastolic BP (mmHg) | 94.5 ± 6.8 | 81.7 ± 10.3 | <.001 |
Results are presented as mean values ± SD.
Includes only the patients with pre-operative and postoperative values.
BP, Blood pressure; PTH, parathyroid hormone.
Table III.
Operative outcomes in hypertensive patients (systolic BP ≥140 and diastolic BP ≥90) with primary hyperparathyroidism on antihypertensive medication (n = 116)
| Pre-operatively | Postoperatively | P value | |
|---|---|---|---|
| PTH (pg/mL) | 166.8 ± 233.0 | 58.0 ± 53.0 | <.001 |
| Calcium (mg/dL)* | 10.9 ± 0.6 | 9.6 ± 0.8 | <.001 |
| Systolic BP (mmHg) | 153.9 ± 10.5 | 141.2 ± 15.0 | <.001 |
| Diastolic BP (mmHg) | 94.2 ± 7.3 | 80.5 ± 9.4 | <.001 |
Results are presented as mean values ± SD.
Corrected for albumin.
BP, Blood pressure; PTH, parathyroid hormone.
Table IV.
Operative outcomes in hypertensive patients (systolic BP ≥140 and diastolic BP ≥90) with primary hyperparathyroidism who had no change or increase in blood pressure after surgery (n = 13)
| Pre-operatively | Postoperatively | P value | |
|---|---|---|---|
| PTH (pg/mL) | 159.7 ± 112.2 | 71.0 ± 556.3 | .005 |
| Calcium (mg/dL)* | 10.6 ± 0.8 | 10.1 ± 0.9 | .2 |
| Systolic BP (mmHg) | 148.7 ± 17.3 | 160.1 ± 18.0 | .03 |
| Diastolic BP (mmHg) | 86.3 ± 5.4 | 88.1 ± 8.5 | .42 |
Results are presented as mean values ± SD.
Corrected for albumin.
BP, Blood pressure; PTH, parathyroid hormone.
BP measurements before and after parathyroid exploration and parathyroidectomy
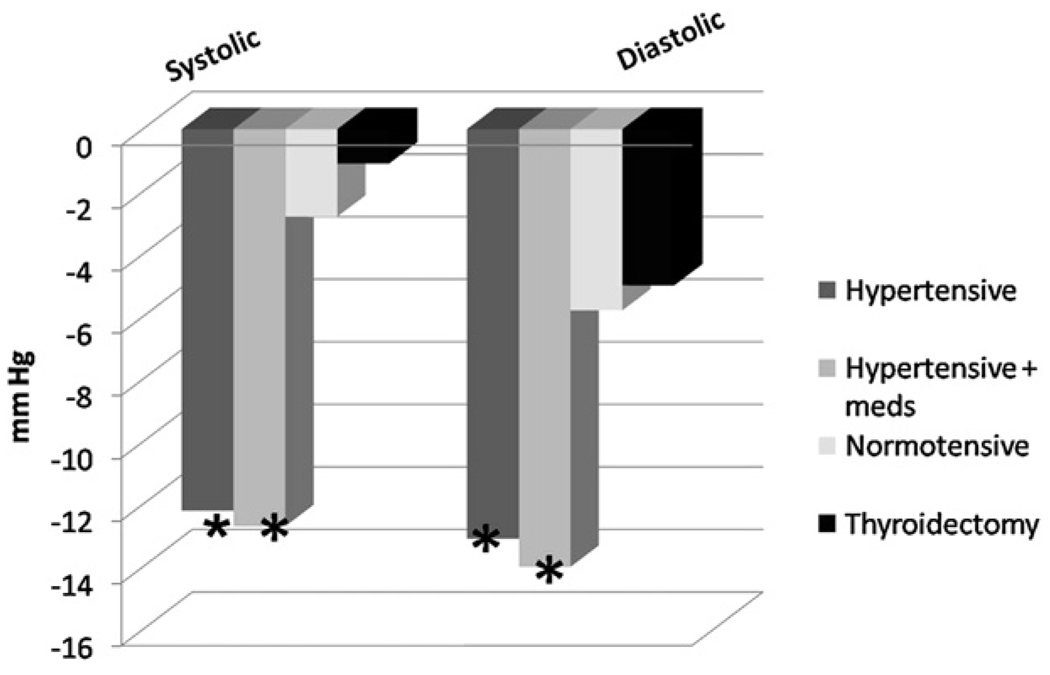
The mean systolic and diastolic BP decreased in the total population of hypertensive patients and hypertensive patients on antihypertensive therapy (Table II and Table III). Patients with PHPT experienced a significant decrease in both systolic BP (152.5 ± 10.5 to 140.3 ± 16.2 mmHg; P < .001) and diastolic BP (94.5 ± 6.8 to 81.7 ± 10.3 mmHg; P < .001; Table II and Table III). In patients with an increase in systolic BP (n = 13), there was no significant change in diastolic BP. In this group of patients, PTH levels fell significantly without statistically significant change in calcium (Table IV). In the subset of patients with normal preoperative BP (n = 145), a mean decrease of 2.8 mmHg and 5.8 mmHg was observed in systolic BP and diastolic BP, respectively. This change was not significant (P = .47; Figure).
Figure.
Mean change in blood pressure after parathyroidectomy and after thyroidectomy (*P ≤ .01).
BP measurements before and after thyroidectomy
We identified 96 patients who had hypertension and nontoxic thyroid disease who underwent thyroidectomy during the same time period by the same surgeon. The mean age of the patients was 53.6 ± 11.0 years and, there were 21.2% males and 78.8% females in this group, which as similar to the parathyroidectomy population (P = .31). In this control group, the preoperative systolic BP was 152.6 ± 12.5 mmHg and the diastolic BP was 80.5 ± 8.0 mmHg. After surgery, the systolic and diastolic BP was 151.4 ± 21.6 and 75.1 ± 10.4 mmHg, respectively (P = .64).
DISCUSSION
In this retrospective study, we have demonstrated that parathyroidectomy reduces BP in hypertensive patients with PHPT. Such an effect was not observed among patients undergoing thyroidectomy alone or in the normotensive population undergoing parathyroidectomy. The reduction in BP occurred in all hypertensive patients regardless of treatment with antihypertensive medications. Of those patients who were on antihypertensives, there were no changes in medications postoperatively. A mean reduction of ≥10 mmHg in both systolic and diastolic BP, seen our in our study, approximates a 40% reduction in stroke rates and 30% reduction in ischemic heart disease according to a meta-analysis of 61 prospective studies.9 The association between hypertension and hyperparathyroidism has been established in previous observational studies.10 The prospective cohort study of the Health Professionals Study reported increased incidence of hypertension with higher quartiles of PTH.11
Several small studies have examined the effect of parathyroidectomy on BP in patients with PHPT. Kov ács et al6 reported that systolic BP significantly decreased within 1 week of parathyroid exploration and removal of hyperactive glands in 16 normotensive patients with primary HPT. Two prospective studies of 18 and 21 patients did not find a decrease in BP after parathyroidectomy.7,8 In contrast, Broulik et al5 reported a significant reduction in systolic and diastolic BP 6 months after parathyroidectomy surgery in 86 hypertensive normotensive patients with primary HPT. Nilsson et al7 and Stefenelli et al12 prospectively evaluated 20 and 38 patients with hypertension and primary HPT and found no reduction in systolic or diastolic BP after a period of 41–59 months after parathyroid exploration and removal of hyperactive glands, respectively. Bollerslev et al13 reported no change in BP in 99 patients with asymptomatic hyperparathyroidism undergoing parathyroid exploration compared with a medically treated group over a period of 2 years. Diamond et al10 reported significant reductions in systolic BP in 75 normotensive and hypertensive patients 30 months after parathyroid surgery. In contrast with these studies, the postoperative period in this study is shorter and conclusions cannot be made regarding the durability of this decrease in systolic BP and diastolic BP. Another group of patients had an increase in their systolic BP. In this small population (n = 13), PTH levels fell significantly, but serum calcium levels did not decrease. The number of patients here is too small to make tangible conclusions regarding the effects of calcium versus decrease in PTH on BP.
The effect of PTH infusion on BP has been examined in several experimental models. Hulter et al14 reported that continuous infusion of PTH over a 12-day period in healthy patients resulted in hypercalcemia and hypertension. Lowering of PTH levels by calcium infusion also reduces BP in normal patients, but not in parathyroidectomized patients.15,16 In contrast, Jespersen et al17 demonstrated that infusion of PTH 1–34 over 2 hours reduced mean arterial pressure in 10 men with essential hypertension. These studies suggest that PTH administration may lower BP acutely and raise BP when given chronically.
Several mechanisms have been proposed to explain the relationship between HPT and hypertension. Kovács et al18 and Gennari et al19 suggested that PTH directly stimulates activity of the renin–aldosterone system to increase BP. In their studies, they demonstrated that parathyroidectomy decreased BP and decreased plasma levels of renin and aldosterone. Others have suggested that PTH stimulates secretion of aldosterone and cortisol from the adrenal cortex.20 Other hypothesized mechanisms for PTH to induce hypertension include endothelial dysfunction,21 increased sympathetic activity,22 or a direct effect on vascular smooth muscle cells.23 Increased arterial wall stiffness, an independent risk factor for cardiovascular disease, has been found to be elevated in patients with HPT.24 Kosch et al25 reported that the endothelial dysfunction seen in patients with HPT could be reversed with parathyroidectomy.
The limitations of our study include its retrospective design and a single BP measurement both in the pre-operative and postoperative time periods. Although we demonstrate that parathyroidectomy is associated with a significant reduction in BP, we cannot establish causality. In addition, we did not have measurements of serum vitamin D levels in our patient population; low vitamin D has also been associated with hypertension.26 Our mean follow-up was only 6 months after parathyroidectomy, thus limiting our conclusions to only short-term effects of surgery on BP.
In conclusion, we demonstrate that parathyroidectomy significantly reduces BP 6 months after surgery in patients with pre-existing hypertension and PHPT. The effect of parathyroidectomy on lowering BP was equally significant on systolic and diastolic BPs. These findings suggest further investigation be performed to elucidate mechanisms responsible for hypertension in patients with hyperparathyroidism.
Acknowledgment
Supported by the National Institutes of Health Grant #NIIH K23AR054334.
Biographies
Dr Randall P. Owen (Bronx, NY): I’m not sure that I read this correctly, but it seemed that you excluded 49 patients that were undergoing some type of cardiologic evaluation in the peri-operative period. It seems to me that those patients might increase the average of the peri-operative and postoperative hypertension, and therefore by excluding those patients from this analysis you might skew your results. I was just wondering if I got that straight and if that’s an accurate analysis.
Dr Jvotirmay Sharma (Atlanta, GA): Those patients underwent a change in their hypertensive regimen and their hypertensive medications. Therefore, the value of the effects of the parathyroidectomy would be confounded by the change in the medication regimen and we did not include them in the study. I did do the analysis and there was a significant decrease in their respective BP, but I could not say that change was from parathyroidectomy or whether it was because of an increase in their β-blockade or other medications that they were given after the cardiologist’s examination.
Dr Mark S. Cohen (Kansas City, KS): My question is, I know this is a retrospective review, but did you look at all a year after surgery if their hypertension recurred?
Dr Jvotirmay Sharma (Atlanta, GA):We don’t have data for about 60% of patients >6 months out, and for the patients that we do have information—and I did not include that in this analysis—we did see a decrease in BP. But I cannot say past 6 months, that’s the limitation of this study.
Dr Stuart D. Wilson (Milwaukee, WI): I think we all want this to be true. How did you select which BP to use, because the patients are seen numerous times in the clinic. I remember years ago George Leight did a study on parathyroidectomy patients, and he picked the last calcium that was measured before the patient went to surgery, and of course in that group of patients out of the 100 there were 5 or 6 who had normal calcium because there was some fluctuation. Did you pick the highest or lowest? I think that makes a considerable difference in the outcome.
Dr Jvotirmay Sharma (Atlanta, GA): It does make a difference. All the blood measurements are in the same clinical study setting, so these are all BP measurements that the patient had when they came to see the surgeon. So it was in the same room, the room hasn’t changed for the last 8 or 9 years, so it was similar nurses, the same equipment, and the same scene, that is, Dr Weber, in clinic. Postoperatively this was also the same. We did not have many patients with multiple BP measurements because this was only looking at BP measurements in the pre-operative and postoperative clinic visit and did not include BP measurements in the hospital or during the surgery. A more precise study could be performed by using 24-hour BP cuffs that measure intermittent BP during the entire day.
REFERENCES
- 1.NIH conference. Diagnosis and management of asymptomatic primary hyperparathyroidism: consensus development conference statement. Ann Intern Med. 1991;114:593–597. doi: 10.7326/0003-4819-114-7-593. [DOI] [PubMed] [Google Scholar]
- 2.Scholz DA, Purnell DC. Asymptomatic primary hyperparathyroidism. 10-year prospective study. Mayo Clin Proc. 1981;56:473–478. [PubMed] [Google Scholar]
- 3.Nainby-Luxmoore JC, Langford HG, Nelson NC, Watson RL, Barnes TY. A case-comparison study of hypertension and hyperparathyroidism. J Clin Endocrinol Metab. 1982;55:303–306. doi: 10.1210/jcem-55-2-303. [DOI] [PubMed] [Google Scholar]
- 4.McCarron DA, Pingree PA, Rubin RJ, Gaucher SM, Molitch M, Krutzik S. Enhanced parathyroid function in essential hypertension: a homeostatic response to a urinary calcium leak. Hypertension. 1980;2:162–168. doi: 10.1161/01.hyp.2.2.162. [DOI] [PubMed] [Google Scholar]
- 5.Broulik PD, Horký K, Pacovský V. Blood pressure in patients with primary hyperparathyroidism before and after parathyroidectomy. Exp Clin Endocrinol. 1985;86:346–352. doi: 10.1055/s-0029-1210507. [DOI] [PubMed] [Google Scholar]
- 6.Kovács L, Góth MI, Szabolcs I, Dohán O, Ferencz A, Szilágyi G. The effect of surgical treatment on secondary hyperaldosteronism and relative hyperinsulinemia in primary hyperparathyroidism. Eur J Endocrinol. 1998;138:543–547. doi: 10.1530/eje.0.1380543. [DOI] [PubMed] [Google Scholar]
- 7.Nilsson IL, Aberg J, Rastad J, Lind L. Maintained normalization of cardiovascular dysfunction 5 years after parathyroidectomy in primary hyperparathyroidism. Surgery. 2005;137:632–638. doi: 10.1016/j.surg.2005.02.001. [DOI] [PubMed] [Google Scholar]
- 8.Piovesan A, Molineri N, Casasso F, Emmolo I, Ugliengo G, Cesario F, et al. Left ventricular hypertrophy in primary hyperparathyroidism. Effects of successful parathyroidectomy. Clin Endocrinol (Oxf) 1999;50:321–328. doi: 10.1046/j.1365-2265.1999.00651.x. [DOI] [PubMed] [Google Scholar]
- 9.Lewington S, Clarke R, Qizilbash N, Peto R, Collins R Prospective Studies Collaboration. Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies. Lancet. 2002;360:1903–1913. doi: 10.1016/s0140-6736(02)11911-8. [DOI] [PubMed] [Google Scholar]
- 10.Diamond TW, Botha JR, Wing J, Meyers AM, Kalk WJ. Parathyroid hypertension. A reversible disorder. Arch Intern Med. 1986;146:1709–1712. [PubMed] [Google Scholar]
- 11.Taylor EN, Curhan GC, Forman JP. Parathyroid hormone and the risk of incident hypertension. J Hypertens. 2008;26:1390–1394. doi: 10.1097/HJH.0b013e3282ffb43b. [DOI] [PubMed] [Google Scholar]
- 12.Stefenelli T, Abela C, Frank H, Koller-Strametz J, Globits S, Bergler-Klein J, et al. Cardiac abnormalities in patients with primary hyperparathyroidism: implications for follow-up. J Clin Endocrinol Metab. 1997;82:106–112. doi: 10.1210/jcem.82.1.3666. [DOI] [PubMed] [Google Scholar]
- 13.Bollerslev J, Jansson S, Mollerup CL, Nordenström J, Lundgren E, Tørring O, et al. Medical observation, compared with parathyroidectomy, for asymptomatic primary hyperparathyroidism: a prospective, randomized trial. J Clin Endocrinol Metab. 2007;92:1687–1692. doi: 10.1210/jc.2006-1836. [DOI] [PubMed] [Google Scholar]
- 14.Hulter HN, Melby JC, Peterson JC, Cooke CR. Chronic continuous PTH infusion results in hypertension in normal patients. J Clin Hypertens. 1986;2:360–370. [PubMed] [Google Scholar]
- 15.Gennari C, Nami R, Bianchini C, Aversa AM. Blood pressure effects of acute hypercalcemia in normal patients and thyroparathyroidectomized patients. Miner Electrolyte Metab. 1985;11:369–373. [PubMed] [Google Scholar]
- 16.Kamycheva E, Jorde R, Haug E, Sager G, Sundsfjord J. Effects of acute hypercalcaemia on blood pressure in patients with and without parathyroid hormone secretion. Acta Physiol Scand. 2005;184:113–119. doi: 10.1111/j.1365-201X.2005.01436.x. [DOI] [PubMed] [Google Scholar]
- 17.Jespersen B, Randløv A, Abrahamsen J, Fogh-Andersen N, Kanstrup IL. Effects of PTH(1–34) on blood pressure, renal function, and hormones in essential hypertension: the altered pattern of reactivity may counteract raised blood pressure. Am J Hypertens. 1997;10:1356–1367. doi: 10.1016/s0895-7061(97)00275-6. [DOI] [PubMed] [Google Scholar]
- 18.Kovács L, Góth MI, Szabolcs I, Dohśn O, Ferencz A, Szilágyi G. The effect of surgical treatment on secondary hyperaldosteronism and relative hyperinsulinemia in primary hyperparathyroidism. Eur J Endocrinol. 1998;138:543–547. doi: 10.1530/eje.0.1380543. [DOI] [PubMed] [Google Scholar]
- 19.Gennari C, Nami R, Gonnelli S. Hypertension and primary hyperparathyroidism: the role of adrenergic and renin-angiotensin-aldosterone systems. Miner Electrolyte Metab. 1995;21:77–81. [PubMed] [Google Scholar]
- 20.Mazzocchi G, Aragona F, Malendowicz LK, Nussdorfer GG. PTH and PTH-related peptide enhance steroid secretion from human adrenocortical cells. Am J Physiol Endocrinol Metab. 2001;280:E209–E213. doi: 10.1152/ajpendo.2001.280.2.E209. [DOI] [PubMed] [Google Scholar]
- 21.Nilsson IL, Rastad J, Johansson K, Lind L. Endothelial vasodilatory function and blood pressure response to local and systemic hypercalcemia. Surgery. 2001;130:986–990. doi: 10.1067/msy.2001.118368. [DOI] [PubMed] [Google Scholar]
- 22.Vlachakis ND, Frederics R, Valasquez M, Alexander N, Singer F, Maronde RF. Sympathetic system function and vascular reactivity in hypercalcemic patients. Hypertension. 1982;4:452–458. doi: 10.1161/01.hyp.4.3.452. [DOI] [PubMed] [Google Scholar]
- 23.Perkovic V, Hewitson TD, Kelynack KJ, Martic M, Tait MG, Becker GJ. Parathyroid hormone has a prosclerotic effect on vascular smooth muscle cells. Kidney Blood Press Res. 2003;26:27–33. doi: 10.1159/000069761. [DOI] [PubMed] [Google Scholar]
- 24.Smith JC, Page MD, John R, Wheeler MH, Cockcroft JR, Scanlon MF, et al. Augmentation of central arterial pressure in mild primary hyperparathyroidism. J Clin Endocrinol Metab. 2000;85:3515–3519. doi: 10.1210/jcem.85.10.6880. [DOI] [PubMed] [Google Scholar]
- 25.Kosch M, Hausberg M, Vormbrock K, Kisters K, Gabriels G, Rahn KH, et al. Impaired flow-mediated vasodilation of the brachial artery in patients with primary hyperparathyroidism improves after parathyroidectomy. Cardiovasc Res. 2000;47:813–818. doi: 10.1016/s0008-6363(00)00130-9. [DOI] [PubMed] [Google Scholar]
- 26.Judd SE, Nanes MS, Ziegler TR, Wilson PW, Tangpricha V. Optimal vitamin D status attenuates the age-associated increase in systolic blood pressure in white Americans: results from the third National Health and Nutrition Examination Survey. Am J Clin Nutr. 2008;87:136–141. doi: 10.1093/ajcn/87.1.136. [DOI] [PubMed] [Google Scholar]