Abstract
The primary focus of chemoprevention research is the prevention of cancer using pharmacological, biological, and nutritional interventions. Chemotherapeutic approaches that have been used successfully for both the prevention and treatment of a number of human malignancies have arisen from the identification of specific agents and appropriate molecular targets. Although drug-metabolizing enzymes have historically been targeted in attempts to block the initial, genotoxic events associated with the carcinogenic process, emerging evidence supports the idea that manipulating drug-metabolizing enzymes may also be an effective strategy to be used for treating tumor progression, invasion, and, perhaps, metastasis. This report summarizes a symposium that presents some recent progress in this area. One area of emphasis is the development of a CYP17 inhibitor for treatment of prostate cancer that may also have androgen-independent anticancer activity at higher concentrations. A second focus is the use of a mouse model to investigate the effects of aryl hydrocarbon receptor and Cyp1b1 status and chemopreventative agents on transplacental cancer. A third area of focus is the phytochemical manipulation of not only cytochrome P450 (P450) enzymes but also phase II inflammatory and antioxidant enzymes via the nuclear factor-erythroid 2-related factor 2 pathway to block tumor progression. A final highlight is the use of prodrugs activated by P450 enzymes to halt tumor growth and considerations of dosing schedule and targeted delivery of the P450 transgene to tumor tissue. In addition to highlighting recent successes in these areas, limitations and areas that should be targeted for further investigation are discussed.
The goal of this symposium was to explore the potential promise and pitfalls associated with the use of drug-metabolizing enzymes and the regulators of their expression and activity as targets for novel chemoprevention or therapeutic strategies. Although the term “chemoprevention” originally referred to agents with pharmacological activities capable of inhibiting the initial stages of tumorigenesis (Sporn et al., 1976), our current use of chemoprevention extends this historical definition to include agents, either naturally occurring or chemically synthesized, that can be effective not only in preventing but also in curing cancer (Russo, 2007). As our concept of chemoprevention has evolved, so too have our expectations of ideal chemopreventive agents been extended to include agents that not only alter the pharmacokinetics and disposition of chemical carcinogens [i.e., via inhibition of phase I/induction of phase II drug-metabolizing enzymes (De Flora and Ferguson, 2005)] but also inhibit the actions of activated oncogenes and act as antioxidant and anti-inflammatory agents. Limitations to further development of new chemopreventive/chemotherapeutic approaches include the need for appropriate and relevant preclinical models that can rigorously determine the potential of these drugs for clinical success.
A number of recent studies that have reported the novel features of specific cytochrome P450 (P450) enzymes contribute to the idea that targeting enzymes of this superfamily may provide unique and effective strategies for enhancing the tumor-specific properties of chemopreventive/therapeutic agents. First, investigations were conducted concerning the recent classification of cytochromes P450, such as those of the CYP2, CYP3, CYP4, CYP17, and CYP19 families, as “cancer-modifying” genes. This classification is based upon the ability of these P450s to catalyze the biotransformation of substrates, such as bile acids, testosterone, estrogen, and other sterols, and in this manner alter the tissue concentration of substances with tumor-promoting activities (Nebert and Dalton, 2006). One of the best examples of therapeutic success obtained using a P450-inhibition strategy to target P450s with cancer-modifying properties is illustrated by the CYP19 (aromatase) inhibitor/breast cancer paradigm and, as described herein, a CYP17 inhibitor/prostate cancer paradigm (Bruno and Njar, 2007). Second, observations were made on P450s, such as CYP1B1, suggesting that they are up-regulated in a number human cancers and that modifications in the expression levels of at least CYP1B1 can significantly modulate tumor progression (Castro et al., 2008). These findings indicate that approaches designed to inhibit CYP1B1 expression may provide a chemopreventive/therapeutic benefit. Third, there were observations that many tumor cells lack expression of specific P450s. In this case, administration of anticancer prodrugs in combination with tumor-specific expression of the prodrug-activating enzymes may prove useful in widening the therapeutic index of our currently used chemotherapeutics (Ma and Waxman, 2008). Finally, novel classes of chemopreventive/therapeutic agents are being developed that can target both drug-metabolizing enzymes and disease (i.e., cancer)-modifying pathways. Examples of this type of agent are the phenylethyl isothiocyanate analogs, which induce the nuclear factor-erythroid 2-related factor 2 (Nrf-2) battery of drug-metabolizing enzymes while also inhibiting the nuclear factor-κβ pathway and exhibit potent in vivo anti-inflammatory properties. For example, novel isothiocyanates are recently developed chemopreventive agents that have been shown to exhibit significant anti-inflammatory properties (Prawan et al., 2009). Success in any of these approaches will likely provide novel opportunities for maximizing the tumoricidal effects while minimizing the toxic side effects of chemopreventive and therapeutic agents.
Inhibitors of 17α-Hydroxylase 17,20-Lyase (CYP17) as Agents for Prostate Cancer Therapy (Vincent C. O. Njar)
The current clinical success of aromatase (CYP19) inhibitors that are used to treat breast cancer (Jordan and Brodie, 2007) has led many investigators, including our research group, to question whether inhibitors of additional P450s may similarly be effective in treating other hormonally responsive cancers (Bruno and Njar, 2007; Moreira et al., 2008). With this in mind, the use of inhibitors of 17α-hydroxylase/17,20-lyase (CYP17), a key multifunctional enzyme that lies at the crossroads of androgen and corticoid biosynthesis, holds considerable promise in treating prostate cancer. This approach is based on the knowledge that 1) androgens are strongly implicated in the progression of prostate cancer, 2) prostate cells as well as prostate cancer cells continuously produce androgens, and 3) systemic ablation of androgen is highly effective in treating prostate cancer (Bruno and Njar, 2007; Moreira et al., 2008; Harris et al., 2009).
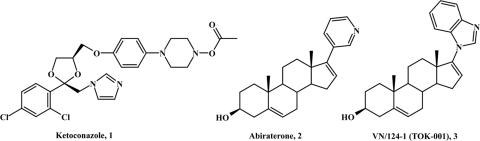
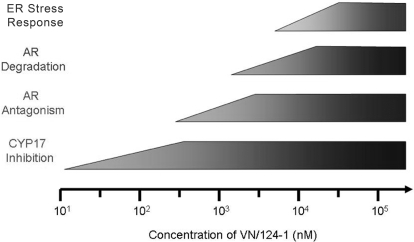
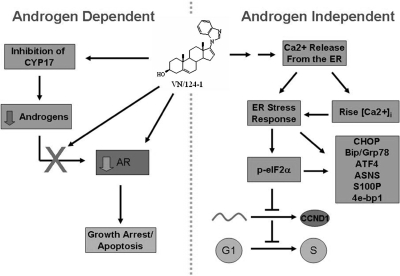
Whereas the antifungal drug ketoconazole (Fig. 1, 1) has proven to be efficacious in the treatment of some prostate cancer patients, its use is limited because of its broad spectrum in inhibiting several P450s, which results in toxicity (Small et al., 1997). The clinical efficacy of a more specific CYP17 inhibitor, abiraterone (Fig. 1, 2), is currently being investigated in phase III clinical trials (Attard et al., 2009a,b). Our group has recently developed novel atypical CYP17 inhibitors that also possess other desirable antiprostate cancer activities, including androgen receptor (AR) antagonism and AR down-regulation. Of these, the most promising is 3β-hydroxy-17-(1H-benzimidazole-1-yl)androsta-5,16-diene (VN/124-1, now called TOK-001) (Fig. 1, 3), which is more effective than castration in inhibiting prostate cancer tumor growth. In addition, the agent is also more effective than abiraterone or the clinically used antiandrogen bicalutamide (Handratta et al., 2005; Bruno et al., 2008; Vasaitis et al., 2008). Recent studies indicate that VN/124-1 is capable of inducing degradation of the AR and induction of endoplasmic reticulum (ER) stress response, and its effects on the various targets are concentration-dependent (Bruno et al., 2008; Vasaitis et al., 2008). At low concentrations, VN/124-1 primarily inhibits CYP17. At moderate concentrations, VN/124-1 is an effective AR antagonist, and at high concentrations, this compound is capable of inducing AR degradation and ER stress (Fig. 2). A summary of our current understanding of VN/124-1's androgen-dependent and androgen-independent mechanisms of action is presented in Fig. 3. More importantly, VN/124-1 inhibits three critical pathways for androgen activity in castrate-resistant prostate cancer, a condition that is attributed to the mortality of the disease. VN/124-1 (TOK-001) is currently being developed by Tokai Pharmaceuticals (Cambridge, MA) and is anticipated to enter clinical phase I/II trials in the 3rd quarter of 2009. We strongly believe that these multiple activities of VN/124-1 are responsible for its efficacy against prostate cancer growth, and we envision that these complementary types of promiscuous anticancer activities may prove to be invaluable in thwarting drug-resistance mechanisms.
Fig. 1.
Chemical structures of CYP17 inhibitors: ketoconazole (1), abiraterone (2), and VN/124-1 (TOK-001) (3).
Fig. 2.
VN/124-1's mechanisms of action by concentration.
Fig. 3.
Schematic representation of androgen-dependent and androgen-independent mechanisms of action of VN/124-1.
Chemoprevention of Polycyclic Aromatic Hydrocarbon-Dependent Transplacental Cancer in a Mouse Model: Role of Cyp1b1 (Zhen Yu, David J. Castro, Frank J. Gonzalez, and David E. Williams)
Whereas the fetus and infant are at considerable risk from the adverse effects of many environmental carcinogens, the mechanisms that underlie transplacental carcinogenesis and the extent to which they may be effectively inhibited by chemopreventive agents is poorly understood. Key issues that must be addressed with respect to chemoprevention lie within the metabolism and disposition of both the carcinogen and the chemopreventive agent. With this in mind, we have recently developed a mouse model of transplacental carcinogenesis. In this model, maternal administration of a potent polycyclic aromatic hydrocarbon (PAH), dibenzo[a,l]pyrene (DBP), results in a high incidence of mortality due to an aggressive T-cell lymphoma. In the surviving offspring, a 100% incidence of lung adenomas and carcinomas develop, in addition to liver lesions in the majority of the males (Yu et al., 2006a). This model could recapitulate human fetal exposure to PAHs from maternal diet and airborne particles, including direct and second-hand tobacco smoke as a causative factor in leukemias/lymphomas in children and young adults. In addition, this model provides a unique, in vivo paradigm with which to compare the relative efficacy of several chemopreventive agents.
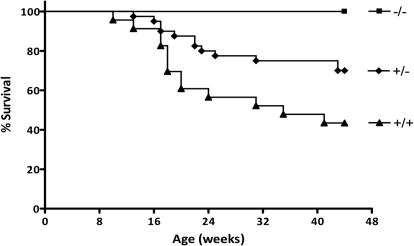
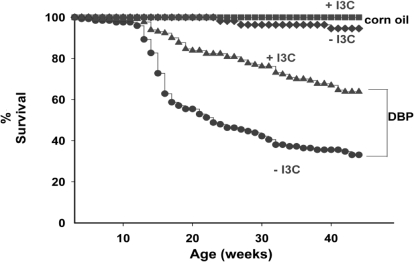
Our work at the mechanistic level has initially focused on the aryl hydrocarbon receptor (AHR)/CYP1B1 pathway. Use of dams and fetuses that varied with respect to their AHR-responsive status have shown that it is the AHR-responsive dam that can decrease the risk to the fetus, presumably via effects that include a decrease in the bioavailability of the carcinogenic PAH to the fetus (Yu et al., 2006a). Similar studies have also been performed using dams and fetuses that varied with respect to their Cyp1b1 genotypes. Here, a tight correlation between DBP-dependent transplacental lymphoma mortality and fetal Cyp1b1 gene dosage was observed (Fig. 4). With respect to benzo(a)pyrene-dependent lung cancer, however, no relationship between disease endpoint and Cyp1b1 genotype could be observed.
Fig. 4.
Transplacental lymphoma mortality and fetal Cyp1b1 genotype. [Reproduced from Castro DJ, Baird WM, Pereira CB, Giovanini J, Lohr CV, Fischer KA, Yu Z, Gonzalez FJ, Krueger SK, and Williams DE (2008) Fetal mouse Cyp1b1 and transplacental carcinogenesis from maternal exposure to dibenzo(a,l)pyrene. Cancer Prev Res (Phila Pa) 1:128–134. Copyright © 2008 American Association for Cancer Research. Used with permission.]
Chemopreventive agents tested thus far in our model include indole-3-carbinol, green tea, (−)epigallocatechin gallate (EGCG), caffeine, and chlorophyllin. Indole-3-carbinol was found to prevent the development of lymphomas and multiplicity of lung adenomas; in the case of lung, only if the dams were AHR-responsive (Fig. 5). Whereas green tea was found to protect against DBP-induced lymphoma mortality, this protective effect seemed to be primarily due to the caffeine but not to the EGCG components of the tea (Castro et al., 2008). However, with respect to DBP-induced lung adenomas, all treatments (i.e., caffeinated and decaffeinated green tea, caffeine, and EGCG) were found to decrease tumor multiplicity. Finally, the protective effects of chlorophyllin were found to be highly dependent on its route of administration. Whereas coadministration of chlorophyllin and DBP by gavage provided a significant protection against DBP-initiated carcinogenesis, administration of chlorophyllin in the diet failed to confer an observable protective effect. Taken together, this work illustrates the need for understanding the unique characteristics of chemopreventive agents that may limit their in vivo efficacy in preclinical models.
Fig. 5.
In dams heterozygous for responsive and nonresponsive versions of the AHR receptor (AHRb-1/d), exposure to indole-3-carbinol in the maternal diet protects the offspring from transplacental DBP mortality. [The figure has been drawn on the basis of the findings in Yu et al. (2006b).]
Targeting Nrf2, Phase I, and Phase II Metabolizing Enzymes for Effective Chemoprevention Strategies (Ying Huang and Ah-Ng T. Kong)
A number of natural products have been found to exert beneficial health effects, including phytochemicals such as EGCG found in tea, curcumin present in the Indian spice turmeric, and phenylethyl isothiocyanate and sulforaphane, constituents of cruciferous vegetables. As chemopreventive agents, these phytochemicals have been described as exerting blocking effects, suppressive effects, or both blocking and suppressive effects (Wattenberg, 1985). Mechanisms that underlie blocking effects primarily involve inhibition of phase I and phase II metabolism. However, in some cases, chemopreventive agents, such as indole-3-carbinol, have been found to block phase II metabolism while enhancing phase I metabolism. Likewise, several phytochemicals that can inhibit the ability of the AHR to up-regulate its target P450s can act as either partial agonists or antagonists of the AHR. These observations have led many researchers to question whether the enzyme-modifying activities of these natural products play significant roles in mediating their chemopreventive effects. Addressing these concerns will most likely involve use of genetically modified mouse models.
More recent studies have found that phytochemicals, such as isothiocyanates that induce phase II enzymes, are electrophiles capable of activating the antioxidant response. In our laboratory, we have found that isothiocyanates induce mitogen-activated protein kinase (MAPK) and extracellular signal-regulated kinase (ERK) signaling cascades as well as activate the Nrf2 pathway. Nrf2 is a member of the Cap‘n’collar family of proteins that appears to act as a redox sensor. Cellular exposure to agents such as phenylethyl isothiocyanate release Nrf2 from its Keap1-mediated repression, allow Nrf2 to translocate to the nucleus, and activate antioxidant response element-responsive genes. Genes up-regulated via the Nrf2 pathway are those that encode phase II enzymes, MAPK, heat shock proteins, and transport proteins. What is not clear at this point is whether phytochemicals can regulate Nrf2-mediated gene transcription by different mechanisms or whether the differential effects observed by these agents are a function of their potency with respect to their ability to activate Nrf2. Combination therapies that include cotreatments of curcumin and sulforaphane result in synergistic responses that not only involve induction of detoxification pathways but also up-regulation of proteins involved in other oxidative stress-related signaling pathways, such as ubiquitin degradation.
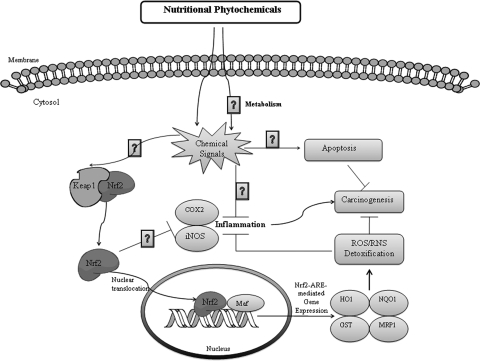
Further mechanistic insights into the role that the Nrf2 gene pathway may play in modifying human disease states have been obtained using genetically modified mice. For example, mice that lack the Nrf2 pathway have proven to be more susceptible to experimentally induced colitis and, as expected, express low levels of antioxidant/phase II-detoxifying enzymes [i.e., heme-oxygenase-1, NAD(P)H-quinone reductase-1, UDP-glucuronosyltransferase 1A1, and glutathione S-transferase μ-1]. In addition, an increase in the expression of proinflammatory cytokines/mediators [i.e., cyclooxygenase-2, inducible nitric oxide synthase, interleukin 1β, interleukin 6, and tumor necrosis factor α] was observed, which indicates that the Nrf2 pathway may also play a role in modifying the inflammatory response (Khor et al., 2006). Likewise, nrf2(−/−) mice were found to be more susceptible (compared with wild-type mice) to experimentally induced colorectal carcinogenesis. Additional links between the Nrf2 pathway, inflammatory response, and phase II drug-metabolizing enzymes have been observed by using the TRAMP mice model of prostate carcinogenesis. Taken together, these studies illustrate the promise associated with the use of phytochemicals, in particular isothiocyanates and other phase II/antioxidant enzyme inducers that target the NRF2/phase II enzyme pathway, to block inflammation and carcinogenesis (Fig. 6).
Fig. 6.
Schematic representation of Nrf2-dependent modulation of phase II, inflammatory, and antioxidant enzymes by nutritional phytochemicals. HO-1, heme-oxygenase-1; NQO1, NAD(P)H-quinone reductase-1; UGT, UDP-glucuronosyltransferase 1A1; GST, glutathione S-transferase μ-1; COX-2, cyclooxygenase 2; iNOS, inducible nitric oxide synthase; ROS, reactive oxygen species; RNS, reactive nitrogen species; MRP1, multidrug resistance protein 1.
Cytochrome P450 Prodrugs in Cancer Therapy-Targeting Tumor Cells and Tumor-Associated Endothelial Cells (Joshua C. Doloff, Jie Ma, and David J. Waxman)
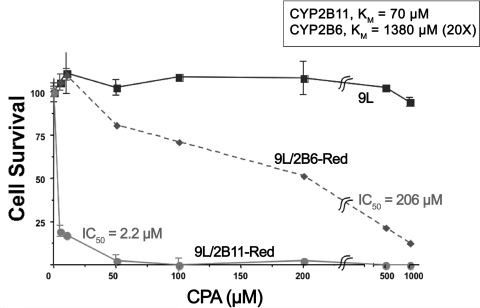
The major goal of prodrug therapy is to exploit the differential expression of P450s between the tumor and host cells to enhance the tumoricidal activities of chemotherapeutic drugs subject to P450 metabolism and to fine-tune optimal dosage regimens and spare host tissue from the toxic side effects of these drugs. Considerable progress has been made using enzyme-prodrug combinations that involve P450s and the anticancer alkylating agent prodrug cyclophosphamide. Whereas cyclophosphamide is metabolized by P450 enzymes primarily within the liver, its active 4-hydroxy metabolite is highly diffusible and can exert considerable tumoricidal effects in tumors that are distant from the liver. Metabolic activation of cyclophosphamide is preferentially catalyzed by the CYP2B subfamily, with CYP2B1 (rat) and CYP2B6 (human) showing good activity. More recent studies showed that the canine enzyme, CYP2B11, exhibits an atypically low Km and catalyzes cyclophosphamide 4-hydroxylation with very high efficiency (Chen et al., 2007) (Fig. 7). Thus, delivery of canine CYP2B11 into human tumors using retroviral or adenoviral gene delivery technologies may facilitate a cyclophosphamide-based CYP gene therapy that is effective, and more selective, at lower drug doses and exhibits less toxicity than traditional chemotherapies.
Fig. 7.
Retroviral delivery of CYP2B6 versus CYP2B11: evaluation of CYPA cytotoxicity.
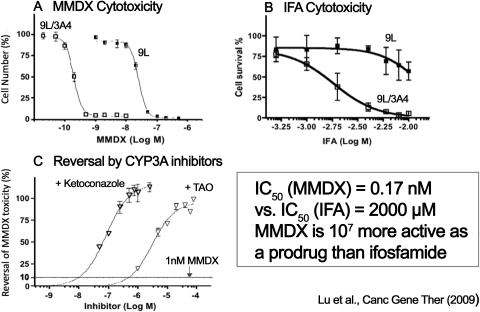
Potentiation of antitumor activity may also be realized using strategies based on CYP3A4-activated anticancer prodrugs, such as the doxorubicin derivative methoxymorpholinyl doxorubicin (MMDX; nemorubicin). We have found that retroviral transfer of CYP3A4 increases the sensitivity of 9L gliosarcoma cells to MMDX >100-fold (Fig. 8). In vivo tumor growth delay studies demonstrated that 9L tumors expressing CYP3A4 are particularly sensitive to MMDX administered intravenously or by direct intratumoral injection (Lu et al., 2009).
Fig. 8.
Tumor-cell cytotoxicity of CYP3A4-activated MMDX. A, MMDX cytotoxicity. B, incomplete Freund's adjuvant (IFA) cytotoxicity. C, reversal by CYP3A inhibitors. [The figure has been drawn on the basis of the findings in Lu et al., 2009.]
Additional studies performed in our laboratory have used metronomic chemotherapy approaches in which the chemotherapeutic drug (e.g., cyclophosphamide) is administered at a reduced dose but with a high frequency instead of the traditional intermittent, maximal tolerated dose schedule. Here, the effectiveness of metronomic dosage of cyclophosphamide used in combination with the potent vascular endothelial growth factor receptor-selective angiogenesis inhibitor axitinib (AG-013736) was examined. Treatment with axitinib alone was found to significantly inhibit angiogenesis of rat 9L tumors but only moderately delay tumor growth. Furthermore, whereas metronomic administration of cyclophosphamide induced substantial tumor regression, coadministration of axitinib with metronomic cyclophosphamide treatment was less effective and tumor growth was only static. This result may arise from the effects of axitinib on the tumor vasculature, which inhibits the delivery of 4-hydroxy cyclophosphamide to the tumor cells. Future success of this type of combination therapy may require careful consideration of drug doses and drug schedules to achieve an optimal decrease in tumor microvessel density while allowing for an appropriate level of chemotherapeutic drug uptake (Ma and Waxman, 2008).
Finally, we have undertaken several steps to improve current limitations associated with the use of viral-based gene delivery approaches, including the low efficiency of therapeutic gene delivery. Toward this end, we have constructed an oncolytic adenovirus, Adeno-hTERT-E1A, which bears deletions of the parent adenoviral E1B, E3A, and E3B regions but expresses the E1A oncoprotein under the regulation of a tumor-specific promoter, hTERT. In vivo experiments designed to compare the therapeutic properties of Adeno-hTERT-E1A with that of ONYX-015, an oncolytic adenovirus that has been widely tested in clinical trials, revealed that Adeno-hTERT-E1A exhibited superior antitumor activity, which could translate into superior efficacy and reduced toxicity in the clinical arena (Doloff et al., 2008). These studies illustrate the potential of using a combinatorial approach involving therapeutic gene delivery and an appropriate chemotherapeutic agent that may target drug-metabolizing enzymes and tumoricidal pathways.
In summary, a variety of approaches are being used to modulate cytochrome P450 enzymes to both prevent and treat cancer. The strategies presented herein focus not only on direct inhibition of cytochrome P450 enzymes but also on the influences of phytochemicals and genotype on regulatory mechanisms on carcinogenesis and the manipulation of cytochrome P450 enzymes to activate anticancer prodrugs. Although drug-metabolizing enzymes have historically been targeted in attempts to block the initiation of carcinogenesis, research in these areas demonstrate that manipulation of drug-metabolizing enzymes and the regulators of their expression and activity are also likely to be effective strategies for treating tumor progression, invasion, and perhaps, metastasis.
This work was supported in part by the National Institutes of Health National Cancer Institute [Grants CA11799101, CA02744028, CA90890, CA073674, CA094828, CA118947, CA49248] (to V.C.O.N., D.E.W., A.N.K., and D.J.W., respectively); the National Institutes of Health National Institute of Environmental Health Sciences [Grants ES00726316A1, ES07060, ES00210] (to V.C.O.N., D.E.W.); and The Linus Pauling Institute at Oregon State University (to D.E.W.).
This report is a summary of a session under the same name as follows: Njar VCO, Williams DE, Kong A-NT, and Waxman DJ (2009) Targeting drug metabolizing enzymes for effective chemopreventive approaches. Experimental Biology 2009; 2009 Apr 18–22; New Orleans, LA; The American Society for Pharmacology and Experimental Therapeutics, Bethesda, MD.
Article, publication date, and citation information can be found at http://dmd.aspetjournals.org.
doi:10.1124/dmd.109.031351.
- P450
- cytochrome P450
- Nrf2
- nuclear factor-erythroid 2-related factor 2
- AR
- androgen receptor
- VN/124-1 (TOK-001)
- 3β-hydroxy-17-(1H-benzimidazole-1-yl)androsta-5,16-diene
- ER
- endoplasmic reticulum
- PAH
- polycyclic aromatic hydrocarbon
- DBP
- dibenzo(a,l) pyrene
- AHR
- aryl hydrocarbon receptor
- EGCG
- (−)epigallocatechin gallate
- MAPK
- mitogen-activated protein kinase
- MMDX
- methoxymorpholinyl doxorubicin.
References
- Attard G, Reid AH, Olmos D, de Bono JS. (2009a) Antitumor activity with CYP17 blockade indicates that castration-resistant prostate cancer frequently remains hormone driven. Cancer Res 69:4937–4940 [DOI] [PubMed] [Google Scholar]
- Attard G, Swennenhuis JF, Olmos D, Reid AH, Vickers E, A'Hern R, Levink R, Coumans F, Moreira J, Riisnaes R, et al. (2009b) Characterization of ERG, AR and PTEN gene status in circulating tumor cells from patients with castration-resistant prostate cancer. Cancer Res 69:2912–2918 [DOI] [PubMed] [Google Scholar]
- Bruno RD, Gover TD, Burger AM, Brodie AM, Njar VC. (2008) 17alpha-Hydroxylase/17,20 lyase inhibitor VN/124-1 inhibits growth of androgen-independent prostate cancer cells via induction of the endoplasmic reticulum stress response. Mol Cancer Ther 7:2828–2836 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bruno RD, Njar VC. (2007) Targeting cytochrome P450 enzymes: a new approach in anti-cancer drug development. Bioorg Med Chem 15:5047–5060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Castro DJ, Baird WM, Pereira CB, Giovanini J, Lohr CV, Fischer KA, Yu Z, Gonzalez FJ, Krueger SK, Williams DE. (2008) Fetal mouse Cyp1b1 and transplacental carcinogenesis from maternal exposure to dibenzo(a,l)pyrene. Cancer Prev Res (Phila Pa) 1:128–134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen CS, Jounaidi Y, Su T, Waxman DJ. (2007) Enhancement of intratumoral cyclophosphamide pharmacokinetics and antitumor activity in a P450 2B11-based cancer gene therapy model. Cancer Gene Ther 14:935–944 [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Flora S, Ferguson LR. (2005) Overview of mechanisms of cancer chemopreventive agents. Mutat Res 591:8–15 [DOI] [PubMed] [Google Scholar]
- Doloff JC, Waxman DJ, Jounaidi Y. (2008) Human telomerase reverse transcriptase promoter-driven oncolytic adenovirus with E1B-19 kDa and E1B-55 kDa gene deletions. Hum Gene Ther 19:1383–1400 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Handratta VD, Vasaitis TS, Njar VC, Gediya LK, Kataria R, Chopra P, Newman D, Jr, Farquhar R, Guo Z, Qiu Y, et al. (2005) Novel C-17-heteroaryl steroidal CYP17 inhibitors/antiandrogens: synthesis, in vitro biological activity, pharmacokinetics, and antitumor activity in the LAPC4 human prostate cancer xenograft model. J Med Chem 48:2972–2984 [DOI] [PubMed] [Google Scholar]
- Harris WP, Mostaghel EA, Nelson PS, Montgomery B. (2009) Androgen deprivation therapy: progress in understanding mechanisms of resistance and optimizing androgen depletion. Nat Clin Pract Urol 6:76–85 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jordan VC, Brodie AM. (2007) Development and evolution of therapies targeted to the estrogen receptor for the treatment and prevention of breast cancer. Steroids 72:7–25 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khor TO, Huang MT, Kwon KH, Chan JY, Reddy BS, Kong AN. (2006) Nrf2-deficient mice have an increased susceptibility to dextran sulfate sodium-induced colitis. Cancer Res 66:11580–11584 [DOI] [PubMed] [Google Scholar]
- Lu H, Chen CS, Waxman DJ. (2009) Potentiation of methoxymorpholinyl doxorubicin antitumor activity by P450 3A4 gene transfer. Cancer Gene Ther 16:393–404 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ma J, Waxman DJ. (2008) Modulation of the antitumor activity of metronomic cyclophosphamide by the angiogenesis inhibitor axitinib. Mol Cancer Ther 7:79–89 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Moreira VM, Salvador JA, Vasaitis TS, Njar VC. (2008) CYP17 inhibitors for prostate cancer treatment–an update. Curr Med Chem 15:868–899 [DOI] [PubMed] [Google Scholar]
- Nebert DW, Dalton TP. (2006) The role of cytochrome P450 enzymes in endogenous signalling pathways and environmental carcinogenesis. Nat Rev Cancer 6:947–960 [DOI] [PubMed] [Google Scholar]
- Prawan A, Saw CL, Khor TO, Keum YS, Yu S, Hu L, Kong AN. (2009) Anti-NF-kappaB and anti-inflammatory activities of synthetic isothiocyanates: effect of chemical structures and cellular signaling. Chem Biol Interact 179:202–211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Russo GL. (2007) Ins and outs of dietary phytochemicals in cancer chemoprevention. Biochem Pharmacol 74:533–544 [DOI] [PubMed] [Google Scholar]
- Small EJ, Baron AD, Fippin L, Apodaca D. (1997) Ketoconazole retains activity in advanced prostate cancer patients with progression despite flutamide withdrawal. J Urol 157:1204–1207 [PubMed] [Google Scholar]
- Sporn MB, Dunlop NM, Newton DL, Smith JM. (1976) Prevention of chemical carcinogenesis by vitamin A and its synthetic analogs (retinoids). Fed Proc 35:1332–1338 [PubMed] [Google Scholar]
- Vasaitis T, Belosay A, Schayowitz A, Khandelwal A, Chopra P, Gediya LK, Guo Z, Fang HB, Njar VC, Brodie AM. (2008) Androgen receptor inactivation contributes to antitumor efficacy of 17{alpha}-hydroxylase/17,20-lyase inhibitor 3beta-hydroxy-17-(1H-benzimidazole-1-yl)androsta-5,16-diene in prostate cancer. Mol Cancer Ther 7:2348–2357 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wattenberg LW. (1985) Chemoprevention of cancer. Cancer Res 45:1–8 [PubMed] [Google Scholar]
- Yu Z, Loehr CV, Fischer KA, Louderback MA, Krueger SK, Dashwood RH, Kerkvliet NI, Pereira CB, Jennings-Gee JE, Dance ST, et al. (2006a) In utero exposure of mice to dibenzo[a,l]pyrene produces lymphoma in the offspring: role of the aryl hydrocarbon receptor. Cancer Res 66:755–762 [DOI] [PubMed] [Google Scholar]
- Yu Z, Mahadevan B, Löhr CV, Fischer KA, Louderback MA, Krueger SK, Pereira CB, Albershardt DJ, Baird WM, Bailey GS, et al. (2006b) Indole-3-carbinol in the maternal diet provides chemoprotection for the fetus against transplacental carcinogenesis by the polycyclic aromatic hydrocarbon dibenzo[a,l]pyrene. Carcinogenesis 27:2116–2123 [DOI] [PubMed] [Google Scholar]