Abstract
Background
Although multiple strategies for autologous breast reconstruction exist, a vertical midline scar in the abdominal wall as a result of previous laparatomy or abdominoplasty represents a major surgical challenge. To date, little research has been conducted on the regeneration potential of the abdominal wall’s superficial vascular, perforator and choke vessel system after surgery using a vertical approache.
Methods
We present the cases of 8 patients, of whom 7 underwent autologous breast reconstruction. One patient received a thigh reconstruction. All patients had a vertical abdominal midline scar as a result of a previous surgical intervention. In 3 of the 7 patients, the breast was reconstructed using an MS-2-vertical rectus abdominis myocutaneous (VRAM) free flap. In 4 of these patients, an MS-2-transverse rectus abdominis myocutaneous (TRAM) free flap was performed. The thigh reconstruction used a transverse deep inferior epigastric perforator (DIEP) free flap. Clinical follow-up was done 12 months after operation.
Results
All 3 patients who received an MS-2-VRAM had good aesthetic results. Vertical midline scars had no negative effect on surgical outcomes, perfusion and tissue viability of the 4 MS-2-TRAM and transverse DIEP free flaps.
Conclusion
These clinical findings indicate that the regeneration potential of the abdominal wall’s superficial vascular system in the presence of vertical surgical scars has been greatly underestimated. Use of MS-2-VRAM free flaps in patients with vertical abdominal scars seems to be a suitable and successful alternative in the reconstruction algorithm.
Autologous breast reconstruction following a mastectomy still represents a major challenge for reconstructive surgeons.1,2 At present, surgeons may choose from a multitude of available method to determine the most favourable surgical approach.3–11 Every method has its own particular indication, benefits and disadvantages, and the optimal one should be specifically tailored to each patient’s individual needs. Thus, the preoperative plan for breast reconstruction should be made with great care and in close communication with the patient.12 Hartrampf and colleagues8 described the transverse rectus abdominis myocutaneous (TRAM) free flap and thereby set a keystone for surgical possibilities in autologous breast reconstruction. Advances in the field of microsurgical perforator flap surgery have made the use of autologous tissue for breast reconstruction a preferred concept.
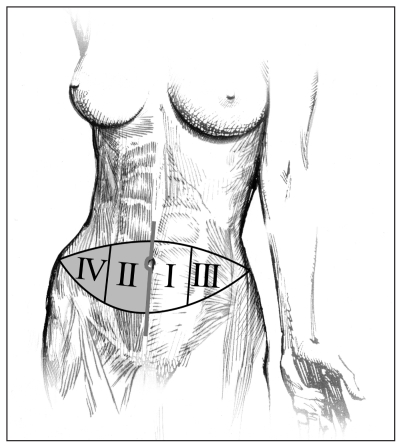
In this context, the transverse deep inferior epigastric perforator (DIEP) flap or the MS-2-TRAM with a small part of the rectus abdominis muscle are ideal flaps suitable for autologous breast reconstruction.13–16 Reasons for the popularity of the DIEP or MS-2-TRAM flaps include the availability of a large amount of tissue for the reconstruction of large breasts, an aesthetically pleasing donor-site scar and a reliable vascular anatomy, as described by Allen.5,6 However, these particular kinds of perforator-based flaps are usually only indicated when the abdominal wall is fully intact. Scars and lesions from previous surgical procedures, such as laparotomy or abdominoplasty, represent a contraindication to such flaps. In particular, a vertical scar in the midline of the abdominal wall may cause major postoperative complications. Necrosis of the distal part of the flap may occur because of poor midline crossover blood flow into zones 2 and 4, which are located distal to the horizontal midline scar (Fig. 1).17–19
Fig. 1.
Position of perfusion zones 1 to 4 according to the midline vertical scar in a left-sided transverse deep inferior epigastric perforator flap.
Patients with a small breast volume on the healthy side usually only require a small tissue volume for reconstruction. As a result, a 1-side transverse DIEP or MS-2-TRAM free flap, which includes only zones 1 and 3, may be favourable and possible. In cases of bilateral breast reconstruction, these techniques are also used.
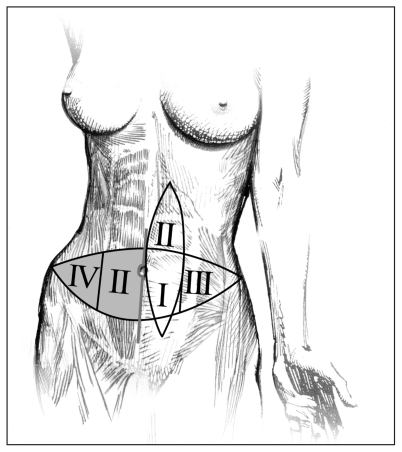
When large amounts of tissue are required for reconstruction, other surgical concepts have to be used. In these cases, surgeons may use a vertical DIEP or an MS-2-vertical rectus abdominis myocutaneous (VRAM) free flap. In contrast to the transverse DIEP flaps, the vertical DIEP or MS-2-VRAM flaps have only 2 zones of perfusion (Fig. 2).20 To date, vertical DIEP and MS-2-VRAM flaps have not been well described in the literature, but they seem to be suitable and successful alternatives and should be included in surgeons’ reconstruction algorithms.
Fig. 2.
In contrast to the transverse deep inferior epigastric perforator (DIEP) flap, the vertical DIEP flap has only 2 zones of perfusion, as described by Dinner and colleagues.20
Few research data are available about the regeneration potential of the abdominal wall’s superficial vascular, perforator and choke vessel system in the presence of vertical scarring. In addition, the delay phenomenon has been described solely for local flaps.21,22 So far, it has been believed that a vertical abdominal scar represents a contraindication for the use of a transverse DIEP or MS-2-TRAM free flap when reconstructive tissue located distally from the scar is needed. In this context the “delay phenomenon” for angiosomes, as described by Taylor and colleagues,23 needs to be discussed. It may also be relevant to the regeneration potential of perforator vessels, choke vessels and the subdermal vascular plexus in the presence of vertical abdominal scarring. A new understanding of these mechanisms may lead to the prudent use of flap tissue distal to a scar.
Methods
We present the cases of 8 women who received reconstructive surgery of a breast or thigh. Seven of the patients previously had breast cancer, whereas 1 patient had severe pain stemming from a 15-year-old third-degree burn scar located on her right medial thigh. All 7 breast cancer patients had received a curative mastectomy and subsequent radiochemotherapy. Following oncological treatment, all 7 patients were referred to our department to receive autologous breast reconstruction. The average time between mastectomy and reconstruction was 15 months. The patient with the burn scar sought our medical attention with the goal of alleviating her severe pain. We performed a Doppler ultrasound in all patients to identify the major perforator vessels.
Three of the 8 patients received MS-2-VRAM free flaps. Their average age was 59 years (ages 55, 58 and 64, respectively). Each had a vertical scar on the abdominal wall following laparotomy (Fig. 3). In these 3 patients, we inserted a small part of the rectus abdominis muscle of about 1 cm × 5 cm. This part included 2 perforator vessels. The cranial perforator was always proximal to the umbilical line. The average operation time for each of the 3 MS-2-VRAM free flaps was 5 hours.
Fig. 3.
Intraoperative situation after left breast reconstruction of the upper 2 quadrants with an MS-2-vertical rectus abdominis myocutaneous free flap because of a vertical scar from a previous laparotomy.
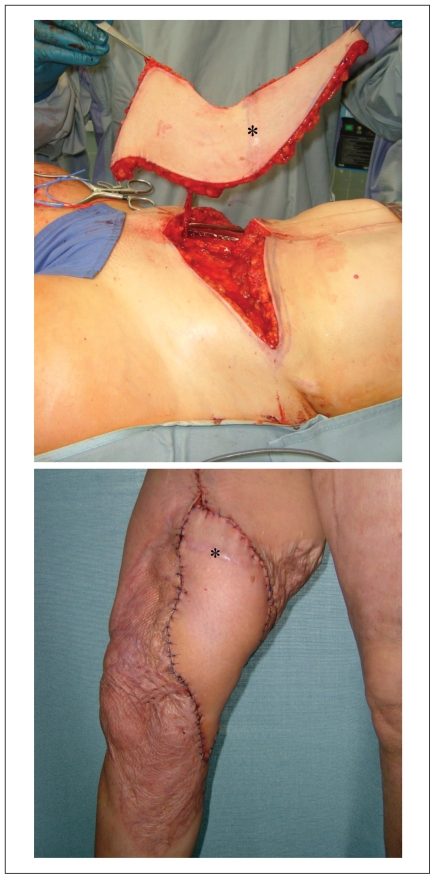
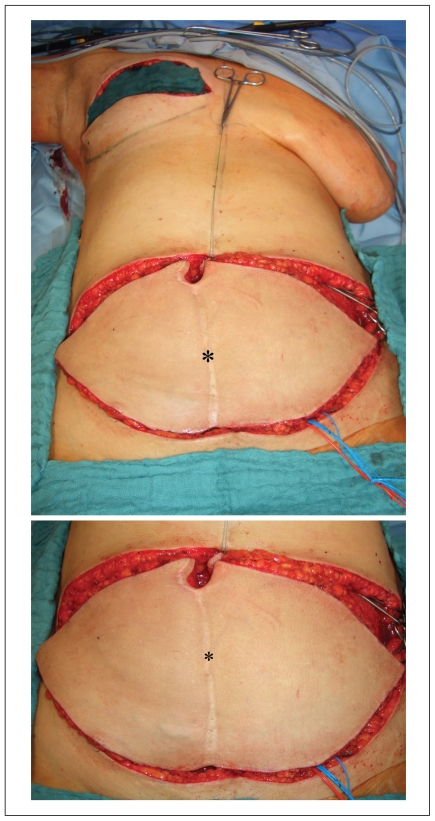
The other 5 patients received transverse DIEP or MS-2-TRAM free flaps. Their average age was 52 years (ages 47, 48, 50, 54 and 60). One of these 5 patients received a thigh reconstruction (Fig. 4) using a transverse DIEP free flap. The other 4 patients underwent breast reconstruction (Fig. 5) with MS-2-TRAM free flaps. These particular kinds of free flaps were used even though the patients all had a vertical abdominal scar from a previous laparotomy. In all 5 patients, the laparotomy was performed between 6 and 8 years before the reconstructive surgery.
Fig. 4.
(Top) Intraoperative situation after preparation of the transverse deep inferior epigastric perforator (DIEP) flap with a vertical scar (*) from a laparotomy. (Bottom) Postoperative situation 1 week after reconstruction of the patient’s right medial thigh with a transverse DIEP free flap including zone 2 distal to the vertical scar (*).
Fig. 5.
(Top) Intraoperative situation after dissection of the MS-2-transverse rectus abdominis myocutaneous (TRAM) free flap with a vertical scar (*) after laparotomy and a lower horizontal scar after cesarean section. (Bottom) Intraoperative situation in which all 4 horizontal zones of the MS-2-TRAM free flap showed full clinical viability and perfusion distal to the midline vertical scar (*) (zones 2 and 4).
In addition, 1 of the patients had a typical horizontal scar as a result of a cesarean section that had been performed 21 years ago. The preoperative surgical plan was to use a 1-side transverse DIEP or MS-2-TRAM free flap, which included only zones 1 and 3, because the patients’ preference was to have no scars in the buttock, thigh or back area. She also did not allow use of alloplastic material. Additionally, all 5 patients desired a reduction of tissue in the abdominal area to decrease local adipositas. One patient indicated that we should use as much tissue as technically possible to reconstruct the breast. The intraoperative perfusion and viability of the tissue distal to the scar, which was represented by zones 2 and 4, was clinically tested for 15 minutes. Cutaneous capillary filling time and tissue colour were observed. Even though the intraoperative findings did not reveal any areas of minor perfusion or poor tissue viability distal to the vertical scar, we performed a resection of zone 4 as a precautionary measure. Zone 4 represented the most distal part of tissue in relation to the vertical scar. As a consequence, zone 4 was routinely resected for all patients.
Results
During clinical follow-up 12 months after operation, it was found that all 3 patients who received the MS-2-VRAM free flap had good aesthetic results. Also, there was no noticeable bulging or hernias. In addition, we found no clinical evidence of a negative effect of the MS-2-TRAM free flaps or transverse DIEP free flaps on surgical outcomes, perfusion and viability of tissue located distal to the midline abdominal wall scar.
Discussion
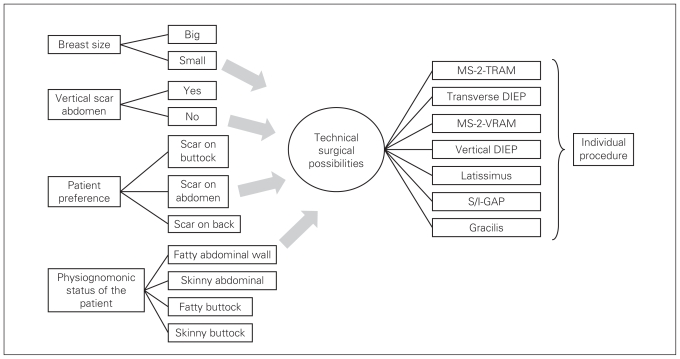
The loss of one or in some cases even both breasts because of mastectomy represents a major psychologic trauma to female breast cancer patients and is a major challenge for reconstructive surgeons. Reconstructive surgery is especially challenging when abdominal scars from previous surgical interventions are present.24–26 Surgeons can choose from several options when deciding the appropriate surgical approach. Only precise analysis of each individual case can lead to an indication of successful overall treatment. Careful planning and good communication with the patient are crucial to successful surgical outcomes (Fig. 6).
Fig. 6.
Important factors in the algorithm for autologous breast reconstruction. DIEP = deep inferior epigastric perforator; S/I-GAP = superior/inferior gluteal artery perforator; TRAM = transverse rectus abdominis myocutaneous, VRAM = vertical rectus abdominis myocutaneous.
Within the last decade, great advances have been made in microsurgical perforator flap surgery; these have led to increased numbers of breast reconstructions using autologous tissue. Transverse DIEP or MS-2-TRAM with a small part of the rectus abdominis muscle are ideal flaps for autologous breast reconstruction. In this context, the reconstruction with a transverse DIEP or MS-2-TRAM flap is not limited to breast reconstruction. Especially in patients with high fat volumes in the abdominal area, use of a DIEP flap, which always includes an abdominoplasty, may be indicated for the reconstruction of other parts of the body. In our case, the patient with the third-degree burn scar on her thigh received a DIEP flap. The use of this perforator-based flap is usually only indicated when the abdominal wall is free of scars and lesions from previous surgical procedures, such as laparotomy or abdominoplasty. In particular, a vertical scar in the midline of the abdominal wall was thought to represent a major problem. However, we believe that a vertical scar does not automatically mean that a transverse DIEP or MS-2-TRAM free flap is impossible. The good clinical results in our patients show that successful reconstruction with these kinds of flaps is possible.19,27 In 5 cases, we performed breast and thigh reconstruction with MS-2-TRAM flaps and a transverse DIEP, even though the patients also had a vertical scar. One patient even had an additional scar from a cesarean section. In all 5 cases, we had originally planned to use 1-side DIEP flaps, because we had assumed that zones 2 and 4 of the flaps would show no perfusion. Surprisingly, though, all 4 zones showed optimal and perfect perfusion during the operations. We still resected zone 4 in the 5 cases to reduce the risk of late distal necrosis of the free flaps, especially because future viability of the subcutaneous fat is more variable than that of the skin alone. Many authors suggest resecting zone 4 when using a transverse DIEP or MS-2-TRAM free flap in cases where no vertical scars are present. In their clinical study, Holm and colleagues28 presented an inversion of zones 2 and 3, which was contrary to the classic perfusion zone theory. Our clinical findings, however, could not verify this inversion.
In cases in which the required breast volume is low, a 1-side transverse DIEP or MS-2-TRAM free flap and thus resection of zone 2 and 4 is advisable. However, in cases that necessitate more breast volume, surgeons must decide during the operation if the flap is adequately perfused distal to the scar and whether it can be used for reconstruction. So far, the scientific literature offers little information about the regeneration and, thus, the revascularization potential of the abdominal wall’s superficial vascular, perforator and choke vessel system following previous vertical surgical approaches. Thus, it is believed that a vertical abdominal scar represents an automatic contraindication for the use of a DIEP or MS-2-TRAM free flap. Our clinical findings do not confirm such an automatic contraindication.
Taylor described the “delay phenomenon” for angiosomes in local flaps.23 We speculate that delay phenomenon may also play a role in the regenerative potential of perforator vessels, choke vessels and the subdermal vascular plexus in the presence of vertical abdominal scaring. In contrast, delay phenomenon may have only limited relevance on the contralateral side, because the perforators of the deep interior epigastric artery and the superficial interior epigastric artery (SIEA) vessels are still intact and, thus, blood supply is only eliminated in perforators of zone 1. However, more studies have to be conducted to fully understand the mechanisms and factors crucial to the survival of tissue distal from scars in free flap perforator surgery.
A limitation of this study is that our series included a small number of cases. An additional limitation is that we did not conduct a perfusion analysis that would have supported our clinical findings. Going forward, we suggest that aesthetic scales or computed tomography analysis be used to substantiate clinical findings, such as “good aesthetic results with no bulging or hernias.” In this context, upcoming results in recent studies in the field of tissue engineering and induction of angiogenesis through intermittent hypoxia may be promising.29,30
Of course, all other possibilities of autologous breast reconstruction should be discussed with the patient before the operation. In this context, the patient also has to be well informed about the reconstructive possibilities using alloplastic material combined with local axial pattern flaps, such as a latissimus dorsi muscle flap. Only if a patient with a vertical abdominal scar refuses these techniques should one opt to perform a reconstruction with transverse DIEP or MS-2-TRAM free flaps including, when necessary and possible, zones 2 and 4.
Santanelli and colleagues18 describe the use of free vertical DIEP flaps in 4 cases. All 4 patients needed breast reconstruction; however, they all had longitudinal midline abdominal scars. In addition, their patients did not have sufficient abdominal tissue for 1-side transverse DIEP flaps (zone 1 and 3). The presented aesthetic results were good, but, more importantly, the use of a vertical DIEP has highly relevant clinical implications for patients with vertical abdominal scars.
Our clinical results and experience using MS-2-VRAM flaps support the findings published by Santanelli and colleagues.18 Other authors have suggested the use of special techniques. Schoeller, for example, suggested the crossover anastomosis and Figus suggested the stacked free SIEA/DIEP flap.17,19 These methods are important and viable options for patients who request breast reconstruction with autologous tissue but who have a vertical scar on the abdominal wall. Of course, other alternative options should be explored and discussed with the patient. Finally, an important, safe and elegant alternative is the superior gluteal artery perforator flap, which is best performed by a very experienced surgeon.7
Conclusion
Although this was a small series of cases, our clinical findings show that, in patients with vertical scarring of the abdominal wall, the regeneration and revascularization potential of the superficial vascular system has been greatly underestimated. In addition, we found that the delay phenomenon may also play a role in free flap perforator surgery.31 However, so far, no studies and research results can quantify and predict the potential for regeneration and revascularization. Following a precise algorithm, reconstructive surgeons can choose from a vast spectrum of technical possibilities when performing autologous breast reconstruction.
Footnotes
Competing interests: None declared.
Contributors: Drs. Dragu and Unglaub conceived the article. Dr. Dragu, Wolf, Schnabl and Horch acquired the data. Drs. Dragu and Wolf wrote the article, which was critically reviewed by all other authors. All of the authors approved the final version submitted for publication.
References
- 1.Barnsley GP, Sigurdson L, Kirkland S. Barriers to breast reconstruction after mastectomy in Nova Scotia. Can J Surg. 2008;51:447–52. [PMC free article] [PubMed] [Google Scholar]
- 2.Beier JP, Horch RE, Bach AD. Breast reconstruction after breast-cancer surgery. N Engl J Med. 2009;360:418–9. doi: 10.1056/NEJMc082264. author reply 20–1. [DOI] [PubMed] [Google Scholar]
- 3.Bach AD, Kneser U, Kopp J, et al. [Possiblities for breast reconstruction following cancer surgery] [Article in German] MMW Fortschr Med. 2004;146:40–2. 4. [PubMed] [Google Scholar]
- 4.Kneser U, Jaeger K, Bach AD, et al. [Breast-reduction surgery — a long-term survey of indications and outcomes] [Article in German] MMW Fortschr Med. 2004;146:36–8. 40. [PubMed] [Google Scholar]
- 5.Allen RJ. DIEP versus TRAM for breast reconstruction. Plast Reconstr Surg . 2003;111:2478. doi: 10.1097/01.PRS.0000063118.22954.20. [DOI] [PubMed] [Google Scholar]
- 6.Allen RJ, Heitmann C. Perforator flaps — the history of evolution. Handchir Mikrochir Plast Chir. 2002;34:216–8. doi: 10.1055/s-2002-36286. [DOI] [PubMed] [Google Scholar]
- 7.Blondeel PN. The sensate free superior gluteal artery perforator (S-GAP) flap: a valuable alternative in autologous breast reconstruction. Br J Plast Surg. 1999;52:185–93. doi: 10.1054/bjps.1998.3032. [DOI] [PubMed] [Google Scholar]
- 8.Hartrampf CR, Scheflan M, Black PW. Breast reconstruction with a transverse abdominal island flap. Plast Reconstr Surg. 1982;69:216–25. doi: 10.1097/00006534-198202000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Dragu A, Kneser U, Horch RE. Post-mastectomy breast reconstruction: pectoralis major myomammary flap versus DIEP and MS-2-TRAM. World J Surg . 2008;32:502. doi: 10.1007/s00268-007-9311-0. [DOI] [PubMed] [Google Scholar]
- 10.Navin C, Agrawal A, Kolar KM. The use of latissimus dorsi miniflap for reconstruction following breast-conserving surgery: experience of a small breast unit in a district hospital. World J Surg. 2007;31:46–50. doi: 10.1007/s00268-006-0396-7. [DOI] [PubMed] [Google Scholar]
- 11.Ramakant P, Mishra A, Chand G. Oncoplastic breast-conserving surgery: analysis of quadrantectomy and immediate reconstruction with latissimus dorsi flap. World J Surg. 2008;32:1569. doi: 10.1007/s00268-007-9448-x. author reply 70. [DOI] [PubMed] [Google Scholar]
- 12.Leffler M, Horch RE, Bach AD. Aesthetic correction of tuberous breast deformity in a male-to-female transsexual patient. Plast Reconstr Surg. 2007;119:1138–40. doi: 10.1097/01.prs.0000253458.51770.fe. [DOI] [PubMed] [Google Scholar]
- 13.Saint-Cyr M, Chang DW, Robb GL, et al. Internal mammary perforator recipient vessels for breast reconstruction using free TRAM, DIEP, and SIEA flaps. Plast Reconstr Surg. 2007;120:1769–73. doi: 10.1097/01.prs.0000287132.35433.d6. [DOI] [PubMed] [Google Scholar]
- 14.Schaverien MV, Perks AG, McCulley SJ. Comparison of outcomes and donor-site morbidity in unilateral free TRAM versus DIEP flap breast reconstruction. J Plast Reconstr Aesthet Surg. 2007;60:1219–24. doi: 10.1016/j.bjps.2007.07.008. [DOI] [PubMed] [Google Scholar]
- 15.Tonseth KA, Hokland BM, Tindholdt TT, et al. Patient-reported outcomes after breast reconstruction with deep inferior epigastric perforator flaps. Scand J Plast Reconstr Surg Hand Surg. 2007;41:173–7. doi: 10.1080/02844310701383449. [DOI] [PubMed] [Google Scholar]
- 16.Yano K, Hosokawa K, Masuoka T, et al. Options for immediate breast reconstruction following skin-sparing mastectomy. Breast Cancer. 2007;14:406–13. doi: 10.2325/jbcs.14.406. [DOI] [PubMed] [Google Scholar]
- 17.Figus A, Fioramonti P, Ramakrishnan V. Stacked free SIEA/DIEP flap for unilateral breast reconstruction in a thin patient with an abdominal vertical midline scar. J Reconstr Microsurg. 2007;23:523–5. doi: 10.1055/s-2007-1022692. [DOI] [PubMed] [Google Scholar]
- 18.Santanelli F, Paolini G, Renzi L. Preliminary experience in breast reconstruction with the free vertical deep inferior epigastric perforator flap. Scand J Plast Reconstr Surg Hand Surg. 2008;42:23–7. doi: 10.1080/02844310701777574. [DOI] [PubMed] [Google Scholar]
- 19.Schoeller T, Wechselberger G, Roger J, et al. Management of infraumbilical vertical scars in DIEP-flaps by crossover anastomosis. J Plast Reconstr Aesthet Surg. 2007;60:524–8. doi: 10.1016/j.bjps.2006.11.008. [DOI] [PubMed] [Google Scholar]
- 20.Dinner MI, Dowden RV, Scheflan M. Refinements in the use of the transverse abdominal island flap for postmastectomy reconstruction. Ann Plast Surg. 1983;11:362–72. doi: 10.1097/00000637-198311000-00002. [DOI] [PubMed] [Google Scholar]
- 21.Callegari PR, Taylor GI, Caddy CM, et al. An anatomic review of the delay phenomenon: I. Experimental studies. Plast Reconstr Surg. 1992;89:397–407. discussion 17–8. [PubMed] [Google Scholar]
- 22.Dhar SC, Taylor GI. The delay phenomenon: the story unfolds. Plast Reconstr Surg. 1999;104:2079–91. doi: 10.1097/00006534-199912000-00021. [DOI] [PubMed] [Google Scholar]
- 23.Taylor GI, Corlett RJ, Caddy CM, et al. An anatomic review of the delay phenomenon: II. Clinical applications. Plast Reconstr Surg. 1992;89:408–16. discussion 17–8. [PubMed] [Google Scholar]
- 24.Heller L, Feledy JA, Chang DW. Strategies and options for free TRAM flap breast reconstruction in patients with midline abdominal scars. Plast Reconstr Surg. 2005;116:753–9. doi: 10.1097/01.prs.0000176252.29645.d0. discussion 60–1. [DOI] [PubMed] [Google Scholar]
- 25.Holzbach T, Mueller DF, Unbehaun N, et al. TRAM-flap perfusion across a midline scar 22 years after a lower median laparotomy. J Plast Reconstr Aesthet Surg. 2008;61:992–3. doi: 10.1016/j.bjps.2007.08.039. [DOI] [PubMed] [Google Scholar]
- 26.Parrett BM, Caterson SA, Tobias AM, et al. DIEP flaps in women with abdominal scars: Are complication rates affected. Plast Reconstr Surg. 2008;121:1527–31. doi: 10.1097/PRS.0b013e31816b14a5. [DOI] [PubMed] [Google Scholar]
- 27.Skillman JM, Pennington D. Refinements of the deep inferior epigastric perforator (DIEP) flap for optimal blood supply. Reply to Schoeller T, Wechselberger G, Roger J, Hussl H, Huemer GM. Management of infraumbilical vertical scars in DIEP-flaps by crossover anastomosis. J Plast Reconstr Aesthet Surg 2007;60:524–8. J Plast Reconstr Aesthet Surg. 2008;61:470–1. doi: 10.1016/j.bjps.2007.12.010. [DOI] [PubMed] [Google Scholar]
- 28.Holm C, Mayr M, Hofter E, et al. Perfusion zones of the DIEP flap revisited: a clinical study. Plast Reconstr Surg. 2006;117:37–43. doi: 10.1097/01.prs.0000185867.84172.c0. [DOI] [PubMed] [Google Scholar]
- 29.Bleiziffer O, Eriksson E, Yao F, et al. Gene transfer strategies in tissue engineering. J Cell Mol Med. 2007;11:206–23. doi: 10.1111/j.1582-4934.2007.00027.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Oh M, Chang H, Minn KW. The effects of tadalafil on axial-pattern skin flap survival in rats. Dermatol Surg. 2008;34:626–30. doi: 10.1111/j.1524-4725.2007.34118.x. discussion 30. [DOI] [PubMed] [Google Scholar]
- 31.Klinger M, Marazzi M, Vigo D, et al. Fat injection for cases of severe burn outcomes: a new perspective of scar remodeling and reduction. Aesthetic Plast Surg. 2008;32:465–9. doi: 10.1007/s00266-008-9122-1. [DOI] [PubMed] [Google Scholar]