Abstract
Background
Recent increases in orthopedic surgical services in Canada have added further demand to an already stretched orthopedic workforce. Various initiatives have been undertaken across Canada to meet this demand. One successful model has been the use of physician assistants (PAs) within the Winnipeg Regional Health Authority (WRHA). This study documents the effect of PAs working in an arthroplasty practice from the perspective of patients and health care providers. We also describe the costs, time savings for surgeons and the effects on surgical throughput and waiting times.
Methods
We calculated time savings by the use of a daily diary kept by the PAs. Surgeons’, residents’, nurses’ and patients’ opinions about PAs were recorded by use of a selfadministered questionnaire. We calculated costs using forgone general practitioner (GP) surgical assist fees and salary costs for PAs. We obtained information about surgical throughput and wait times from the WRHA waitlist database.
Results
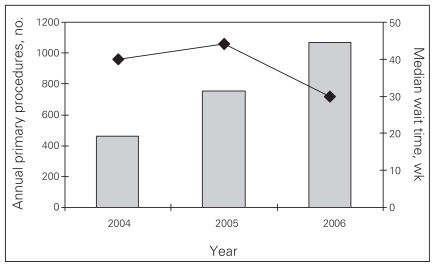
In this study, PAs “saved” their supervising physician about 204 hours per year; this time can be used for other clinical, administrative or research duties. Physician assistants are regarded as important members of the health care team by surgeons, nurses, orthopedic residents and patients. When we compared the billing costs with those that would have been generated by the use of GP surgical assists, PAs were essentially cost neutral. Furthermore, they potentially freed GPs from the operating room to spend more time delivering primary care. We found that use of the double operating room model facilitated by PAs increased the surgical throughput of primary hip and knee replacements by 42%, and median wait times decreased from 44 weeks to 30 weeks compared with the preceding year.
Conclusion
Physician assistants integrate well into the care team and can increase surgical volumes to reduce wait times in a cost-effective manner.
Abstract
Contexte
L’ajout récent de services de chirurgie orthopédique au Canada a accru la demande imposée à un effectif orthopédique déjà très taxé. On a lancé diverses initiatives au Canada pour répondre à cette demande. Le recours aux adjoints au médecin (AM) à l’Office régional de la santé de Winnipeg (ORSW) est un modèle qui connaît du succès. Cette étude décrit l’effet des AM dans une pratique d’arthroplastie du point de vue des patients et des fournisseurs de soins. Nous décrivons aussi les coûts, le temps gagné par les chirurgiens, ainsi que les effets sur le roulement des patients en chirurgie et sur les temps d’attente.
Méthodes
Nous avons calculé les économies de temps à l’aide d’un journal quotidien tenu par les AM. Nous avons utilisé un questionnaire autoadministré pour réunir les opinions des chirurgiens, des médecins résidents, des infirmières et des patients au sujet des AM. Nous avons calculé les coûts d’utilisation des frais d’assistance chirurgicale auxquels ont renoncé les omnipraticiens (OP) et les coûts salariaux des AM. Nous avons tiré de la base de données sur les listes d’attente de l’ORSW de l’information sur le roulement des patients en chirurgie et sur les temps d’attente.
Résultats
Selon cette étude, les AM permettent à leurs médecins surveillants de « gagner » quelque 204 heures par année, temps que ceuxci peuvent consacrer à d’autres activités cliniques, administratives ou de recherche. Les adjoints au médecin sont considérés comme des membres importants de l’équipe de soins par les chirurgiens, les infirmières, les médecins résidents en orthopédie et les patients. Lorsque nous avons comparé les coûts de facturation à ceux qu’aurait produits le recours à des OP comme assistants en chirurgie, l’impact des AM sur les coûts est essentiellement neutre. De plus, ils peuvent libérer les OP de la salle d’opération pour leur permettre de consacrer plus de temps à la prestation de soins primaires. Nous avons constaté que le recours au modèle double de salle d’opération facilité par les AM avait augmenté de 42 % le roulement des patients qui avaient subi une arthroplastie primaire de la hanche et du genou, et que les temps d’attente médians étaient passés de 44 à 30 semaines comparativement à l’année précédente.
Conclusion
Les adjoints au médecin s’intègrent bien à l’équipe de soins et peuvent augmenter le roulement des patients en chirurgie afin de réduire les temps d’attente de façon rentable.
Access to hip and knee replacement surgeries in Canada has generated considerable political interest in the past several years. In 2005, the federal and provincial ministers of health announced benchmarks of 26 weeks for hip and knee replacement surgery. Each provincial government was to develop its own strategy and, by the end of 2007, establish individual multiyear targets to reach these benchmarks.1 Accordingly, between 2004/05 and 2005/06, there was a 17% increase in the volume of hip and knee replacement surgery.2 These rapid increases in surgical services have added further demand to an already stretched Canadian orthopedic workforce.3
To meet this demand, different initiatives have been implemented across Canada, including the Alberta Hip and Knee Replacement Project (www.albertaboneandjoint.com/hipandknee.asp) and advanced practice physical therapists in Ontario.4 Part of Manitoba’s approach to physician shortages has been to employ physician assistants (PAs), who are currently employed across many disciplines within the Winnipeg Regional Health Authority (WRHA), including the high-volume academic arthroplasty program at Concordia Hospital. The WRHA is the first Canadian health region (outside of the armed forces) to employ PAs and, accordingly, there is little published about their roles and effectiveness in a Canadian context.
In addition to describing the role that PAs can play in a Canadian academic arthroplasty group, we sought to document the amount of time that PAs save their supervising physician by undertaking tasks that the surgeon would have otherwise done; document the perceptions of patients, surgeons, orthopedic residents and allied health care providers around the role of PAs; examine costs by comparing the salary costs of PAs to the forgone surgical assist fees (usually a general practitioner); and determine the impact of PAs on surgical throughput and wait times for hip and knee replacement surgery.
The Concordia Joint Replacement Group (CJRG) consists of 4 fellowship-trained orthopedic surgeons specializing in primary and revision hip and knee replacement surgery. The group performs about 1400 joint replacements per year, 24% of which are revisions. Emergency fracture work and “surgical procedure add-ons” during revision surgery account for about another 450 procedures per year. Because of this high volume of work and the low number of residents rotating through the service, the group hired 2 PAs in January 2003 and added a third in May 2006. The PAs take first call with their supervising physician, provide first-assist services in the operating room (OR), write postoperative orders, generate operative notes, undertake daily working rounds and complete discharge summaries. They are paid by the WRHA but report to their supervising surgeons.
The addition of PAs to the CJRG team has allowed a single surgeon to run 2 rooms during a single operating day, increasing the volume from 3 to 7 primary joints per day. This was accomplished by using 1 physician assistant per room, with each room having its own dedicated nursing team and anesthesiologist. While the surgeon operates in one room with assistance from the first physician assistant, the second physician assistant helps to position, prepare and drape the next patient in the second room. On completion of the first operation, the surgeon leaves the first room to immediately start operating in the second room. When the surgeon leaves the first room, the first physician assistant closes the incision, completes the paperwork and assists with room changeover.
Methods
To investigate the time savings, we performed an examination of the various tasks performed by PAs on the arthroplasty service to determine the time savings for the surgeon. This was accomplished by use of a daily diary kept by the PAs, discussions with the PAs and observation of the time required for the various tasks. The tasks selected were those that would previously have been done by the surgeon but were now delegated to a PA.
To document perceptions about PAs, we used a survey administered to all full-time ward nurses on the surgical ward, all full-time operating room nurses, all orthopedic residents still in the training program who had rotated through the arthroplasty rotation, all 4 orthopedic surgeons and a convenience sample of 25 arthroplasty in-patients. The survey was administered in a blinded fashion, and respondents were assured of anonymity of their responses. The University of Manitoba Biomedical Research Ethics board provided ethical review and approval for this survey. We constructed the survey with input from orthopedic surgeons and PAs. It was assessed for face validity and was administered to a sample of respondents before being finalized.
To supplement data from the patient questionnaires, 1-year postoperative selfreported satisfaction scores for patients undergoing primary hip or knee replacement surgery in 2006 were obtained from the CJRG prospective arthroplasty database.5 As part of their routine follow-up, patients who agreed to participate in the database answered the question: “How satisfied are you with the results of you hip/knee replacement surgery?” The answer options included very unsatisfied, unsatisfied, neutral, satisfied and very satisfied. This prospective database was approved by the University of Manitoba Biomedical Research Ethics board.
We undertook a cost analysis by comparing the salary costs of 3 PAs to the cost savings generated by the forgone general practitioner (GP) surgical assist fees. These forgone assist fees refer to the billings that would normally have been generated by the GPs assisting in the operating room but were not because a PA assisted instead. We calculated the savings by manually reviewing the last 100 surgical procedures performed in 2006 by each of the 4 surgeons to determine the cost savings (sum of all forgone GP assist fees) per 100 procedures. This “cost savings per procedure” was then multiplied by the total number of procedures completed by the surgeon in the entire year to estimate cost savings for the year. Fees for each surgical procedure and the associated assist fees were obtained from the Manitoba Physician’s Manual published by the Manitoba Ministry of Health (Apr. 1, 2007, www.gov.mb.ca/health/manual/).
We also assessed the impact of the use of PAs on hip and knee replacement waiting times by examining the reduction in the number of patients on the group’s arthroplasty waiting list and the subsequent decrease in waiting times that could be attributed to the use of 2 operating rooms. Data for the waiting lists were provided by the WRHA orthopedic waitlist coordinator.
Results
Time savings for the supervising physician
Table 1 outlines the typical 50-minute time savings for a surgeon per arthroplasty patient. The total surgical volume for this group was 1409 primary and revision joints in 2006. Physician assistants were involved in about 69.4% of these cases. This translates to a surgeon time savings of 815 hours per year, about 204 hours per surgeon or four 50-hour work weeks per surgeon.
Table 1.
Surgeon time saving per patient associated with the use of a physician assistant
| Activity | Time savings, min |
|---|---|
| Foley catheter insertion, patient positioning and draping | 15 |
| Wound closure | 10 |
| Orders or operating room notes | 3 |
| Daily rounds (total over a 5-day hospital stay) | 15 |
| Discharge prescriptions | 3 |
| Discharge summary | 4 |
| Total | 50 |
Perceptions of physician assistants
Orthopedic surgeon survey
All 4 orthopedic surgeons completed the survey (Table 2). Overall, the surgeons had very positive opinions of PAs. One surgeon commented that the capabilities of PAs exceed that of R5 residents.
Table 2.
Orthopedic surgeons’ (n = 4) perceptions of physician assistants
| Perception | Agree, % | Neutral, % | Disagree, % |
|---|---|---|---|
| A fully trained PA provides surgical assistance equal to an R5 | 100 | — | — |
| The presence of a PA has improved your job satisfaction | 100 | — | — |
| The presence of a PA has safely allowed you to do more surgical volume | 100 | — | — |
| The care of your patients on the ward is improved by the assistance of PAs | 100 | — | — |
| The care of your patients in the OR is improved by the assistance of PAs | 100 | — | — |
| PAs greatly decrease the amount of “scut work”* that you have to do | 100 | — | — |
OR = operating room; PA = physician assistant.
Daily tasks necessary for patient care but do not require the extensive training of an orthopedic surgeon.
Operating room nurse survey
We distributed surveys to all 12 OR nurses; 10 completed and returned the questionnaires (83% response rate; Table 3). Overall, the OR nurses reported that PAs were valuable team members. They also felt that the PAs improved the care of orthopedic surgery patients in the operating room, provided surgical assistance superior to family practitioners and that they were necessary to run 2 ORs.
Table 3.
Operating room nurses’ (n = 10) perceptions of physician assistants
| Perception | Agree, % | Neutral, % | Disagree, % |
|---|---|---|---|
| PAs improve the care of orthopedic surgery patients in the OR | 70 | 30 | — |
| PAs generally provide a level of surgical assistance superior to GPs | 90 | 10 | — |
| PAs are necessary for a surgeon to run 2 operating rooms effectively | 90 | 10 | — |
| PAs are important team members in the operating room | 80 | 20 | — |
| PAs perform tasks that really should fall within the scope of nursing | 40 | 60 | — |
GP = general practitioner; OR = operating room; PA = physician assistant.
A significant proportion of OR nurses (40%) felt that tasks performed by PAs in the OR fell within the scope of nursing practice. Discussion with several of the operating room nurses and the OR manager revealed that these responses reflected the fact that PAs often displaced nurses from traditional nursing tasks such as inserting Foley catheters or helping to position patients. The nurses’ concern were not that the PAs were filling an expanded allied health care role that should be performed by nurses but, that during an operating room day, they were undertaking some activities that were traditionally performed by nurses.
Ward nurse survey
The survey was completed by all 22 ward nurses (Table 4). They felt that patient care, information flow and patient rounds were enhanced by the PAs and that PAs were important members of the ward team. One ward nurse provided the following written comment: “It develops a sense of ‘team’ to have them visible on our unit and a part of our everyday.”
Table 4.
Ward nurses’ (n = 22) perceptions of physician assistants
| Perception | Agree, % | Neutral, % | Disagree, % |
|---|---|---|---|
| PAs improve the care of orthopedic surgery patients on the ward | 100 | — | — |
| PAs improve the flow of information to patients and their families | 100 | — | — |
| PAs facilitate patient rounds | 95 | 5 | — |
| PAs are important team members on the ward | 100 | — | — |
| PAs perform tasks that really should fall within the scope of nursing | 32 | 18 | 50 |
PA = physician assistant.
Results about whether the PAs tasks fell within the scope of nursing were ambiguous. One-third of respondents agreed that the tasks fell within nursing, one-fifth had a neutral opinion and one-half disagreed. A discussion with the clinical resource nurse on the ward (formerly termed the “charge nurse”) revealed similar opinions to those expressed by the operating room nurses. Some of the tasks that the PAs occasionally performed on the ward traditionally fell within the scope of nursing practice. These included removing hemovac drains, changing dressings for wound inspections and inserting Foley catheters. Thus, the concern was not that the PAs were filling nursing roles but that the PAs were occasionally undertaking some activities on the ward that were traditionally performed by nurses.
Orthopedic resident survey
Surveys were completed by all 6 orthopedic residents who had undertaken rotations on the arthroplasty service when PAs were present and who had not yet graduated from the orthopedic training program (Table 5). In general, their responses were more variable than the other groups surveyed.
Table 5.
Orthopedic surgery residents’ (n = 6) perceptions of physician assistants
| Perception | Agree, % | Neutral, % | Disagree, % |
|---|---|---|---|
| PAs improve resident workload | 83 | 17 | — |
| PAs relieve you of clinical responsibilities so that you can attend teaching | 66 | 17 | 17 |
| PAs facilitate your training experience during the arthroplasty rotation | 50 | 50 | — |
| PAs improve your learning experience on the ward | — | 66 | 33 |
| PAs improve the OR experience | 33 | 50 | 17 |
OR = operating room; PA = physician assistant.
The residents were nearly unanimous that PAs reduced their workload, and they generally felt that PAs relieved them of clinical responsibilities so that they could attend to teaching. Half of the residents agreed that “PAs facilitate their training experience during the arthroplasty rotation”; the other half were neutral but didn’t feel that PAs specifically improved their learning on the ward or in the OR. These varied responses about PAs improving the learning experience probably reflect the fact that if a resident is on a surgeon’s rotation, then the PA is not present in the operating room, nor is the PA primarily responsible for taking care of that surgeon’s patients on the ward. Thus, the residents would receive little direct teaching or supervision from the PAs.
Patient survey
The survey was administered to 25 patients, and responses were received from 24 (96%). Overall, the patients expressed very positive opinions of PAs (Table 6). Some patients specifically commented that PAs were helpful in providing information and explaining aspects of their care.
Table 6.
Patients’ (n = 24) perceptions of physician assistants
| Perception | Agree, % | Neutral, % | Disagree, % |
|---|---|---|---|
| PAs improve your care on the ward | 79 | 21 | — |
| PAs improve the flow of information to patients and their families | 83 | 17 | — |
| I think PAs are a good idea | 96 | 4 | — |
| PAs are important team members on the ward | 92 | 8 | — |
| I am satisfied with the care I’ve received from the clinical assistants | 96 | 4 | — |
OR = operating room; PA = physician assistant.
One year after surgery, responses to the satisfaction question were available from 626 out of 1070 patients (58.5%). Overall, 91.3% of hip patients reported being satisfied or very satisfied and 87.7% of knee patients reported being satisfied or very satisfied.
Cost analysis
We manually reviewed the last 402 procedures of 2006. Physician assistants were present for 279 of the 402 procedures (69.4%), and the total forgone GP assist fees were $56 113.00 for the 402 procedures, which resulted in an average cost savings of $139.58 per procedure. The total number of surgical procedures for all 4 surgeons for the year was 1936, including fracture work and “surgical add-ons” for revision cases. Based on these costs savings per case and volumes, the estimated total annual forgone GP surgical assist fees was $270 226.88.
The WRHA remuneration schedule for PAs indicates that the cost of employing 3 PAs in 2006 was between $270 000 and $327 000, which was very similar to the forgone GP surgical assist fees.
Waiting times
The addition of PAs to CJRG’s team allowed a single surgeon to run 2 rooms during a single operating day, thus increasing the volume from 3 to 7 primary joint surgeries per day. Owing to the unpredictability of revision surgery, the group did not undertake revision surgeries during double days.
Table 7 outlines how the addition of double rooms aided the group in significantly increasing surgical volumes and reducing waiting times for patients. In fact, the use of double rooms in 2006 increased primary joint volumes by 316, an increase from the 754 that would have been done had no double rooms been used. This is an increase of 42% in primary joint volume directly attributable to the double room model. This significant increase in volume was possibly because of the double rooms, because the surgeons had very little time in their schedules to pick up any more OR time, other than by creating “double days.” During this time, the median wait time for surgery decreased from a high of 44 to 30 weeks (Fig. 1).
Table 7.
Surgical volumes and waiting times for the 4 Concordia Joint Replacement Group surgeons, by year
| Year | Wait list count at the end of year | Annual total procedures, no. | Annual primary procedures, no. | Waiting time, wk, median | “Double” days, no. | Extra surgeries performed because of double days, no. |
|---|---|---|---|---|---|---|
| 2004 | 1129 | 758 | 462 | 40 | 0 | 0 |
| 2005 | 1131 | 1085 | 755 | 44 | 34 | 136 |
| 2006 | 980 | 1409 | 1070 | 30 | 79 | 316 |
Fig.1.
Surgical volume and wait times in the Winnipeg Regional Health Authority from 2004 to 2006. Diamonds indicate median waiting times.
Discussion
In this study, PAs were found to “free up” 204 hours per year, or the equivalent of four 50-hour work weeks, for their supervising physician. This time could be used for other activities such as operating in a second theatre, other patient care–related duties, research activities or administrative work. Furthermore, surgical throughput was greatly enhanced: PAs allowed for use of the double room model, which increased the group’s surgical throughput of primary joint replacements by 42% over the preceding year and facilitated a reduction in median wait times from 44 weeks to 30 weeks.
An indirect benefit of using PAs in the operating room is the possibility of freeing up general practitioners to remain in their clinic to provide primary care. This is particularly salient because access to primary care physicians is an issue across Canada.6 In fact, if one assumes conservatively that assisting with one arthroplasty procedure or emergency case would take a GP away from the office for a minimum of 2 hours, the 1344 surgical cases (both elective and emergency) that the PAs provided first surgical assistance for equals 2688 hours in the office, or sixty-seven 4-hour work weeks, which is the equivalent of 1.5 GPs working 40 hours per week for 44 weeks per year.
Both operating room and ward nurses felt that PAs were important team members who improved care delivery. However, they did not feel that PAs filled an expanded health care provider role that should be in the domain of nursing. Orthopedic surgeons felt strongly that PAs improved the quality of care for their patients both in the operating room and on the ward. They also felt that PAs relieved them of many of the daily tasks necessary for patient care but that do not require the extensive training of an orthopedic surgeon (colloquially termed “scut work”). Most importantly, patients reported very positively that PAs improved the care that they received on the ward and that PAs were important members of their care team. Furthermore, the patients’ selfreported 1-year postoperative satisfaction rates for knee and hip replacements of 87.7% and 91.3%, respectively, compares very favourably with those reported in the literature (82% for knees7 and 89% for hips8).
Whereas orthopedic residents reported that PAs decreased their workload, they appeared less convinced that PAs improved their learning. However, when scheduling permited, some of the orthopedic surgeons still asked for surgical assistance from a PA when performing hip replacements with a resident. This allowed the attending to stand on the same side of the patient as the resident, thus providing closer supervision and education while the resident operated.
Evidence from this study supports the hypothesis that PAs are exceedingly cost effective. Although their salary costs were found to be budget neutral (the salary costs were essentially the same as the forgone GP assist fees), the value added is impressive: they may greatly increase surgical volume, facilitate patient care and, in an indirect way, potentially increase access to general practitioners.
There is very little literature on the use of PAs within the Canadian health care system. Sigurdson,9 using data from 2 hospitals in Halifax, Nova Scotia, demonstrated that the use of PAs could significantly increase surgical productivity. His business case analysis indicated that this would be achieved in a cost-effective manner if the addition of a PA increased a plastic surgeon’s productivity by 37% or greater. Additionally, he noted that the use of a PA would allow one surgeon to simultaneously run 2 operating rooms, thereby achieving even greater efficiency. His predictions are consistent with our findings: PAs allowed the double room model, increased surgical volumes by 42% and did so in a cost-neutral fashion.
Our study design had potential weaknesses. The information about the perceptions of PAs was obtained through a qualitative process of questionnaire use and follow-up discussions. This method was chosen because it is very difficult to formally measure many of the aspects of PA practice that may be acknowledged as important, such as the impact on teaching, patient communication and potential overlap with nursing roles and duties. However, one may argue that caregivers’ and patients’ perceptions of these aspects are probably not only fairly accurate but also very important. Furthermore, the information about patient’s perceptions was supported by their selfreported satisfactions rates 1 year after surgery.
The surgical care delivery model in this study used the “double room” setup, something that is uncommon across Canada. However, we do not feel that this detracts from the applicability of the cost-effectiveness findings, because PAs only work in 1 room at a time and the cost savings are dependant only on the forgone GP assist fees in that same room.
This examination of PAs working in a busy Canadian joint replacement practice demonstrates that PAs integrate well into the care team and can increase surgical volumes to reduce wait times in a cost-effective manner. We feel that other medical specialties faced with access to care challenges should give serious consideration to the use of PAs.
Footnotes
Competing interests: None declared for Dr. Bohm, Dr. Araneta, Mr. Rhule and Mr. Pitman. Dr. Dunbar has received paid consultancy from Stryker Orthopaedics.
Contributors: Drs. Bohm and Dunbar and Mr. Rhule designed the study and acquired and analyzed data. Mr. Araneta also acquired data. Dr. Bohm and Mr. Pitman wrote the article. All authors reviewed the article and approved its publication.
References
- 1.Ontario Ministry of Health and Long-Term Care. First ever common benchmarks will allow Canadians to measure progress in reducing wait times [news release] Dec 12, 2005. [(accessed 2009 Dec. 7)]. Available: www.health.gov.on.ca/english/media/news_releases/archives/nr_05/nr_121205.html.
- 2.Canadian Institute for Health Information (CIHI) Canadian Joint Replacement Registry (CJRR) 2007 annual report. Hip and knee replacements in Canada. Ottawa (ON): CIHI; 2008. [(accessed Dec. 7, 2009)]. Available: http://secure.cihi.ca/cihiweb/dispPage.jsp?cw_page=download_form_e&cw_sku=CJRRTHKR2007PDF. [Google Scholar]
- 3.The National Standards Committee of the Canadian Orthopaedic Association 2004. National workforce and services report. Montréal (QC): Canadian Orthopaedic Association; 2004. [(accessed Dec. 7, 2009)]. Available: www.coa-aco.org/images/stories/news/NSC_Report_2004_final.pdf. [Google Scholar]
- 4.Robarts S, Kennedy D, MacLeod AM, et al. A framework for the development and implementation of an advanced practice role for physiotherapists that improves access and quality of care for patients. Healthc Q. 2008;11:67–75. doi: 10.12927/hcq.2008.19619. [DOI] [PubMed] [Google Scholar]
- 5.Strasser S, Aharony L, Greenberger D. The patient satisfaction process: moving toward a comprehensive model. Med Care Rev. 1993;50:219–48. doi: 10.1177/107755879305000205. [DOI] [PubMed] [Google Scholar]
- 6.The College of Family Physicians of Canada. When the clock starts ticking. Wait times in primary care. Missisauga (ON): the College; 2006. [(accessed Dec. 7, 2009)]. Available: www.cfpc.ca/local/files/Communications/Wait_Times_Oct06_Eng.pdf. [Google Scholar]
- 7.Robertsson O, Dunbar M, Pehrsson T, et al. Patient satisfaction after knee arthroplasty: a report on 27,372 knees operated on between 1981 and 1995 in Sweden. Acta Orthop Scand. 2000;71:262–7. doi: 10.1080/000164700317411852. [DOI] [PubMed] [Google Scholar]
- 8.Mancuso CA, Salvati EA, Johanson NA, et al. Patients’ expectations and satisfaction with total hip arthroplasty. J Arthroplasty. 1997;12:387–96. doi: 10.1016/s0883-5403(97)90194-7. [DOI] [PubMed] [Google Scholar]
- 9.Sigurdson L. Meeting challenges in the delivery of surgical care: a financial analysis of the role of physician assistants. Halifax (NS): Saint Mary’s University; 2006. [(accessed Dec. 7, 2009)]. Available: http://web.mac.com/lsigurdson/Leif_Sigurdson/Profile_files/Surgical%20Care%20Challenges.pdf. [Google Scholar]