Abstract
Background
The disparity between the number of patients waiting for an organ transplant and availability of donor organs increases each year in Canada. Donation after cardiac death (DCD), following withdrawal of life support in patients with hopeless prognoses, is a means of addressing the shortage with the potential to increase the number of transplantable organs.
Methods
We conducted a retrospective, single-centre chart review of organs donated after cardiac death to the Multi-Organ Transplant Program at the London Health Sciences Centre between July 2006 and December 2007. In total, 34 solid organs (24 kidneys and 10 livers) were procured from 12 DCD donors.
Results
The mean age of the donors was 38 (range 18–59) years. The causes of death were craniocerebral trauma (n = 7), cerebrovascular accident (n = 4) and cerebral hypoxia (n = 1). All 10 livers were transplanted at our centre, as were 14 of the 24 kidneys; 10 kidneys were transplanted at other centres. The mean renal cold ischemia time was 6 (range 3–9.5) hours. Twelve of the 14 kidney recipients (86%) experienced delayed graft function, but all kidneys regained function. After 1-year follow-up, kidney function was good, with a mean serum creatinine level of 145 (range 107–220) μmol/L and a mean estimated creatinine clearance of 64 (range 41–96) mL/min. The mean liver cold ischemia time was 5.8 (range 5.5–8) hours. There was 1 case of primary nonfunction requiring retransplantation. The remaining 9 livers functioned well. One patient developed a biliary anastomotic stricture that resolved after endoscopic stenting. All liver recipients were alive after a mean follow-up of 11 (range 3–20) months. Since the inception of this DCD program, the number of donors referred to our centre has increased by 14%.
Conclusion
Our initial results compare favourably with those from the transplantation of organs procured from donors after brain death. Donation after cardiac death can be an important means of increasing the number of organs available for transplant, and its widespread implementation in Canada should be encouraged.
Abstract
Contexte
L’écart entre le nombre de patients en attente de transplantation d’organe et la disponibilité d’organes de donneurs se creuse chaque année au Canada. Le don après la mort cardiaque (DMC) suivant le retrait du maintien des fonctions vitales chez les patients dont le pronostic est sans espoir permet de lutter contre la pénurie et pourrait augmenter le nombre d’organes transplantables.
Méthodes
Nous avons effectué une étude rétrospective unicentrique de dossiers portant sur des organes donnés après la mort cardiaque par le Programme de transplantation d’organes multiples au Centre des sciences de la santé de London entre juillet 2006 et décembre 2007. Au total, on a prélevé 34 organes pleins (24 reins et 10 foies) de 12 donneurs en état de mort cardiaque.
Résultats
Les donneurs avaient en moyenne 38 (intervalle de 18 à 59) ans. Les décès avaient été causés par un traumatisme crâniocérébral (n = 7), un accident vasculaire cérébral (n = 4) et une hypoxie cérébrale (n = 1). Les 10 foies ont été transplantés à notre centre, ainsi que 14 des 24 reins. Les 10 autres reins ont été transplantés à d’autres centres. L’ischémie froide du rein a duré en moyenne 6 (intervalle de 3 à 9,5) heures. Chez 12 des 14 receveurs d’un rein (86 %), le greffon a commencé à fonctionner tardivement, mais tous les reins ont recommencé à fonctionner. Au suivi à 1 an, la fonction rénale était bonne, la concentration moyenne de créatinine sérique s’établissait à 145 (intervalle de 107 à 220) μmol/L et la clairance glomérulaire estimative moyenne, à 64 (intervalle de 41 à 96) mL/min. L’ischémie froide du rein a duré en moyenne 5,8 (plage de 5,5 à 8) heures. Il y a eu un cas de non-fonctionnement primitif qui a obligé à procéder à une autre transplantation. Les 9 autres foies ont bien fonctionné. Un patient a présenté une sténose anastomotique biliaire qui est disparue après la pose d’un stent par endoscopie. Tous les receveurs d’un foie étaient vivants après un suivi moyen de 11 (intervalle de 3 à 20) mois. Depuis le début de ce programme de don après la mort cardiaque, le nombre de donneurs dirigés à notre centre a augmenté de 14 %.
Conclusion
Nos premiers résultats se comparent favorablement à ceux de la transplantation d’organes prélevés chez des donneurs après la mort cérébrale. Le don après la mort cardiaque peut être un moyen important d’accroître le nombre d’organes disponibles pour la transplantation. Il faudrait en encourager la généralisation au Canada.
The disparity between the number of patients on transplant waiting lists and the number of organs donated from deceased individuals increases each year in Canada. This organ shortage has prompted the establishment of various task forces, parliamentary committees and organ-procurement organizations. Despite the attention organ shortage has received and the efforts made by many involved in this field, the national organ donation rate has not improved substantially. The annual rate remains at a mediocre level (13 per million population) compared with other countries such as the United States (24 per million population) and Spain (35 per million population).1
An ignored donor source in Canada has been donation after cardiac death (DCD), previously known as non–heart beating donation. Every day, life support is withdrawn from patients with devastating conditions and hopeless prognoses. For some of these individuals, organs can be donated after death occurs following withdrawal of life support if specific criteria are met.
The concept of DCD is not new. It was the only source of organs for transplantation in the 1950s and 1960s.2 After brain-death criteria were defined and adopted in 1968, donation after neurologic death (DND) became the primary source of organs for transplant, and DCD mainly ceased, except at some European and American transplant centres. Recently, there has been renewed interest in DCD as a means of addressing the inadequate supply of organs. A Canadian multidisciplinary consensus conference organized by the Canadian Council for Donation and Transplantation (CCDT) was convened in 2005 to discuss DCD.3,4 More than 100 professionals from critical care medicine, nursing, transplant surgery, bioethics, the legal profession, hospital administration, donor families and organ recipients met for 3 days to comprehensively examine DCD. They reached consensus that DCD should go forward in Canada, under specific guidelines that they detailed in a consensus document.4 Subsequent to the conference, our centre began using DCD organs to meet the needs of patients with organ failure. In this article, we present our initial experience with kidney and liver transplantation using DCD organs.
Methods
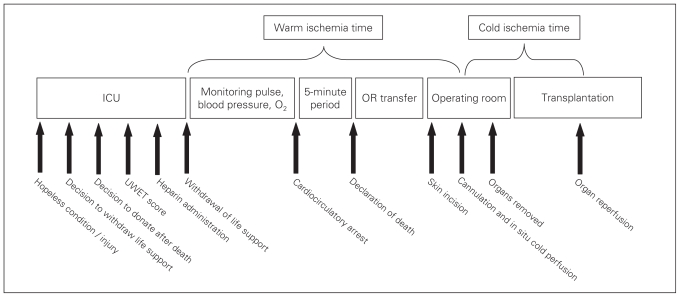
We performed a retrospective, single-centre chart review of DCD transplants at our institution. The following describes the different steps of our DCD protocol, which was developed by the hospital’s intensivists, ethicist and transplant professionals and was eventually approved by the institution’s Medical Advisory Committee. It is the accepted view at London Health Sciences Centre that organ donation is the right of all individuals, and part of end-of-life care should ensure the opportunity to donate. The sequence of events in the DCD process described below is illustrated in Figure 1.
Fig. 1.
Timeline of events associated with donation after cardiac death. ICU = intensive care unit, OR = operating room, UWET = University of Wisconsin Donation After Cardiac Death Evaluation Tool.
Donors and donation process
From July 2006 through December 2007, the London Health Sciences Centre Multi-Organ Transplant Program removed 34 organs (24 kidneys and 10 livers) from 12 DCD donors. The donors were individuals with devastating neurologic injury with no hope for recovery but who did not fulfill the criteria for neurologic death. Each was critically ill in the intensive care unit (ICU) on mechanical ventilation. The decision to withdraw life support was made by the patient’s family in conjunction with the staff in the ICU. In each case, the family initiated the discussion about the possibility of organ donation. It was only after the wishes of the family and the next-of-kin were expressed that potential donors were referred to our program. The possibility of organ donation was discussed only after the decision to withdraw life support had been made. After the transplant specialists determined the individual’s suitability for organ donation, families were informed that organ donation would occur only after cardiocirculatory arrest, absence of breathing and declaration of death by 2 physicians from the ICU. It was explained that if death did not occur within 2 hours after the withdrawal of life support, organ donation would not occur, and end-of-life care would be continued as per institutional protocol. Detailed consent for donation was obtained from the family, and separate consent was obtained for the administration of heparin before withdrawing life support.
Prior to organ donation, DCD donors were screened in an identical fashion to DND donors to rule out communicable disease, malignant disease and other comorbidities that could jeopardize transplant outcomes. A detailed social and medical history of the donor was obtained, and a thorough physical examination was performed in the ICU to exclude conditions or diseases that would contraindicate donation. Routine hematological testing to screen donors for infectious disease included serology for hepatitis B and C, HIV, human T lymphocyte virus-1 and -2, syphilis, West Nile virus, Epstein–Barr virus and cytomegalovirus. Routine liver and kidney function tests (serum creatinine, blood urea nitrogen, liver enzymes, serum bilirubin and international normalized ratio) were performed to assess the quality of the organs. Blood samples were also taken for ABO blood group identification, human leukocyte antigen tissue typing and crossmatching with recipient blood. Donor abdominal imaging was not performed systematically before organ retrieval, although it had been performed for some patients as part of their care for conditions that resulted in their hospital admission (e.g., multiple trauma). For this initial experience, donor age was limited to 60 years to exclude marginal donors who are known to have higher risk of poor graft outcomes.
To predict whether clinical deterioration and death would occur within the assigned time after withdrawal of life support, the University of Wisconsin Donation After Cardiac Death Evaluation Tool (UWET) was used.5 The UWET criteria were derived from standard weaning protocols used in hospitals for patients who will be extubated. The evaluation occurs after the ventilator has been disconnected for a period of up to 10 minutes. At the end of this time, ventilatory rate, tidal volume and negative inspiratory force are measured in conjunction with observation of the patient’s oxygen saturation. Each parameter is scored on a scale of 1 to 3 corresponding to its predicted impact on the patient’s overall suitability for DCD. The numeric score from this evaluation assigns additional points corresponding to the patient’s age, body mass index, vasopressor and inotrope dependence, and type of intubation. The final score reflects an assessment of the patient’s suitability as a DCD candidate.
If a donor is referred from a distant hospital, on-site personnel in the donor institutions provided relevant and timely information that allowed us to make important decisions about donor candidacy and arrange the recipient’s surgery to dovetail with the organ retrieval. Our retrieval team travelled to the donor hospitals in advance of the planned withdrawal from life support. There was usually 24-hour notice, which allowed ample time for recipient selection. Coordination and collaboration with distant hospitals worked well throughout the entire process.
Organ procurement, preservation and transplant surgery
Withdrawal from life support was conducted in the ICU in 6 cases and in the operating room (OR) in 6 cases. The site was determined by ICU personnel in accordance with the family’s desires and the local hospital protocol. Following cardiocirculatory arrest, a 5-minute waiting period was observed before death was pronounced by 2 physicians not involved with transplantation. During this period, cardiocirculatory arrest, apnea and unconsciousness had to be observed. The 5-minute waiting period was in accordance with the recommendations of the CCDT forum and the American College of Critical Care Medicine.4,6 After declaration of death, when withdrawal of life support occurred in the ICU, the body of the donor was promptly transferred to the OR for donation.
Withdrawal from life support was managed by ICU staff according to institutional protocol for end-of-life care, whether it occurred in the OR or ICU. No one involved in the withdrawal of life support had any role or participation in organ procurement or transplantation. The donor’s family was present during withdrawal of life support if they desired. About 30 minutes before withdrawal of life support, 30 000 units of heparin were given intravenously to the donor. No other drugs or interventions were used before death.
Prior to the initiation of the withdrawal of life support, the surgical team presented to a designated OR and prepared for organ procurement. Periodic reports of the donor’s vital signs (heart rate, arterial blood pressure, respiratory rate) plus oxygen saturation and urine output during this period were conveyed to the transplant surgeons.
After death was pronounced, the donor’s abdomen and chest were prepped and draped in a sterile fashion. The surgeon made a midline abdominal incision, and the aorta and inferior vena cava were exposed and cannulated. In situ cold perfusion of the kidneys and liver with Custodiol histidine-tryptophan-ketoglutarate solution (HTK; Methapharm Inc.) via the aorta was begun. The vena cava cannula was opened to gravity drainage. A third cannula was inserted into the superior mesenteric vein for additional liver perfusion. Ice slush provided surface cooling of the liver and kidneys. The surgeon then extended the laparotomy to a sternotomy for exposure and clamping of the supraceliac aorta. The livers and kidneys were dissected during the cold perfusion and removed separately. The organs were stored in HTK solution at 4°C.
We defined warm ischemia time (WIT) as the period of time from initiation of the withdrawal of life support to the initiation of cold perfusion. The cold ischemia time (CIT) was defined as the period of time from the initiation of cold perfusion until reperfusion of the allograft in the recipient. Every effort was made to minimize CIT by starting the recipient operations in a timely fashion, which resulted in overlapping donor and recipient operations. Because withdrawal of life support was a planned event, it allowed time for the intended recipients, who were blood-group compatible with the donor, to be selected, notified and admitted to hospital in preparation for the transplant surgery. For renal transplantation, it allowed satisfactory time for tissue typing and crossmatching of donor and recipient blood samples.
When consent was obtained from kidney and liver transplant recipients preoperatively, they were informed that the organs would be procured from donors after cardiac death and that there was an association with a greater chance of primary nonfunction, delayed graft function and, in the case of the liver, a higher incidence of biliary complications. Delayed graft function was defined as the need for dialysis in the first week after transplantation.
Standard techniques of liver and kidney transplantation were used. The livers were whole grafts placed in the orthotopic position. Kidneys were transplanted into the iliac fossa. The immunosuppressive protocol used for liver transplant recipients was primarily tacrolimus, mycophenolate mofetil and prednisone. For kidney recipients, polyclonal anti–T cell antibody (Thymoglobulin; Genzyme) induction with delayed introduction of tacrolimus was used because delayed graft function was expected. Maintenance immunosuppression for kidney transplant recipients was tacrolimus-based with mycophenolate mofetil and prednisone.
As per our transplant protocol for DCD, every liver recipient underwent allograft biopsy 1 hour after arterial reperfusion in the OR and at 3 months after transplant. In addition, magnetic resonance cholangiography was performed at 3 and 12 months after transplant because of the increased incidence of bile duct strictures in liver grafts from DCD.7 Ultrasound-guided allograft biopsy was performed between postoperative days 7 and 10 in kidney recipients with delayed graft function to rule out acute rejection. We calculated creatinine clearance (CrCl) using the Cockroft–Gault formula.
Results
Donors and donation process
From July 2006 to December 2007, 14 donors were accepted for DCD in our program. Two continued to have spontaneous respiration beyond the 2-hour time limit after the initiation of withdrawal of life support, therefore donation was abandoned. One died 13 minutes later; the other died 12 hours later. Organ donation occurred in the other 12 cases, and 34 organs were removed and transplanted. The liver was procured from 10 donors, and both kidneys were retrieved from all 12 donors. The results related to the donors and the procurement process are summarized in Table 1 and Table 2. During the same period, organs were transplanted from 85 DND donors at our centre. Therefore, the initiation of DCD accounted for a 14% increase in the number of donors.
Table 1.
Demographic characteristics of donation after cardiac death donors at London Health Sciences Centre between July 2006 and December 2007
| Donor | Age, yr | Sex | Cause of death | Days in ICU | BMI, kg/m2 | Initial sCr, μmol/L | AST, U/L | ALT, U/L | Bilirubin, μmol/L |
|---|---|---|---|---|---|---|---|---|---|
| 1 | 18 | F | Trauma | 3 | 24 | 57 | 96 | 147 | 14 |
| 2 | 31 | M | Trauma | 4 | 31 | 128 | 65 | 44 | 16 |
| 3 | 59 | F | Trauma | 6 | 23 | 49 | 44 | 120 | 10 |
| 4 | 31 | M | CVA | 3 | 42 | 84 | 120 | 68 | 16 |
| 5 | 49 | F | Trauma | 19 | 47 | 58 | 18 | 25 | 11 |
| 6 | 43 | F | Trauma | 4 | 22 | 61 | 45 | 39 | 19 |
| 7 | 50 | M | CVA | 2 | 28 | 76 | 50 | 112 | 5 |
| 8 | 24 | M | Anoxia | 1 | 26 | 84 | 37 | 31 | 6 |
| 9 | 21 | F | Trauma | 2 | 28 | 65 | 58 | 13 | 4 |
| 10 | 45 | M | CVA | 5 | 28 | 62 | 119 | 158 | 2 |
| 11 | 50 | F | CVA | 3 | 28 | 46 | 18 | 10 | 19 |
| 12 | 32 | M | Trauma | 47 | 27 | 48 | 24 | 27 | 3 |
ALT = alanine aminotransferase; AST = aspartate aminotransferase; BMI = body mass index; CVA = cerebrovascular accident; F = female; ICU = intensive care unit; M = male; sCR = serum creatinine.
Table 2.
Data related to the procurement of donation after cardiac death organs
| Donor | Site of WLS | UWET score | Warm ischemia time, min | Distance travelled, km* | Organs used |
|---|---|---|---|---|---|
| 1 | ICU | 14 | 26 | Local | Liver, kidney |
| 2 | ICU | 14 | 26 | Local | Liver, kidney |
| 3 | ICU | 13 | 124 | Local | Liver, kidney |
| 4 | OR | 14 | 32 | 110 | Kidney |
| 5 | ICU | 14 | 88 | Local | Liver, kidney |
| 6 | ICU | 11 | 128 | 200 | Kidney |
| 7 | OR | 21 | 41 | 110 | Liver, kidney |
| 8 | OR | 18 | 24 | 130 | Liver, kidney |
| 9 | OR | 16 | 50 | 130 | Liver, kidney |
| 10 | OR | 14 | 101 | 200 | Liver, kidney |
| 11 | OR | 24 | 30 | 130 | Liver, kidney |
| 12 | ICU | 14 | 37 | 200 | Liver, kidney |
ICU = intensive care unit; OR = operating room; UWET = University of Wisconsin Donation After Cardiac Death Evaluation Tool;5 WLS = withdrawal of life support.
Local was defined as within 5 km.
The demographic characteristics of the 12 organ donors are shown in Table 1. The mean donor age was 37.8 (standard deviation [SD] 13, range 18–59) years. Seven donors had head trauma; 2 had head injuries only and 5 had additional musculoskeletal injuries (spinal, pelvic and femoral fractures) and chest trauma. Four donors had cerebrovascular accidents and 1 had cerebral hypoxia. Four donors were admitted to London Health Sciences Centre and 8 were in hospitals within 200 km of our centre. The mean UWET score was 16 (SD 4, range 11–24), indicating a moderate chance for continued breathing after extubation.
The mean WIT was 58.9 (SD 40, range 24–128) minutes. When withdrawal of life support occurred in the ICU instead of the OR, it added about 5 minutes to the WIT. Two kidneys were removed from each donor. Two donors were excluded from liver donation because of long combined warm and cold ischemic times in 1 donor and elevated liver enzymes in another. Of the 12 donors, 7 had a rapid decrease in blood pressure and oxygen saturation after initiation of withdrawal of life support, and cardiocirculatory arrest occurred within 30 minutes. In 3 donors, cardiocirculatory arrest occurred after 60 minutes. However, their mean arterial pressure was below 55 mm Hg for less than 30 minutes (short period of organ hypoperfusion).
In the 2 remaining donors, cardiac arrest occurred at 2 hours, and the mean arterial pressure stayed below 55 mm Hg for more than 40 minutes. In the first of these 2 cases, the decision to use the kidneys and liver was based on the appearance of the organs during procurement, their perfusion characteristics and a normal biopsy in the case of the liver. The liver from this donor failed to function, and emergency repeat transplantation was required 5 days after the first transplant. Based on this experience, the liver was not transplanted from the other donor who had a similar long WIT (donor no. 6). Thus, 10 livers and 24 kidneys were procured and transplanted. The organ procurement data are presented in Table 2. Overall, there were no complications during the procurement process.
All livers and 14 of the 24 kidneys were transplanted at our centre. Ten kidneys were transplanted elsewhere (7 in Hamilton and 3 in Toronto). Cold ischemia time averaged 5.2 (SD 1.5, range 3–7.25) hours for liver grafts and 6.7 (SD 2.5, range 3–25.5) hours for kidney grafts.
Kidney transplantation
The demographics of the 14 kidney recipients (12 men, 2 women) are shown in Table 3. The mean age was 54.1 (SD 5, range 36–77) years. The mean time on dialysis before transplantation was 30 (SD 20, range 12–76) months. The recipients were not highly sensitized to panel reactive antibody (< 20%) except for recipient no. 12, who previously had received a combined liver/kidney transplant. Polyclonal anti–T cell antibody induction (Thymoglobulin, 1.5 mg/kg/day, titrated according to leukocyte, lymphocyte and platelet counts) was given until the allograft recovered from delayed graft function (serum creatinine [sCr] < 300 μmol/L) or for a maximum of 10 days, with delayed introduction of tacrolimus. Maintenance immunosuppression was tacrolimus-based, targeting trough tacrolimus levels between 10 and 12 ng/mL during the first month, 8–10 ng/mL by 3 months and 5–8 ng/mL at 6 months. Mycophenolate mofetil and prednisone were started at the time of transplant and continued thereafter. Twelve of the 14 patients (85.7%) experienced delayed graft function and required temporary dialysis for a mean of 12 (SD 6, range 2–25) days after transplantation. There were no cases of primary nonfunction.
Table 3.
Characteristics of kidney recipients and functional outcomes
| Recipient | Age, yr | Sex | Kidney disease | Cold ischemia time, h | LOS, d | Delayed graft function | Postoperative dialysis, d | sCr:CrCl, μmol/L:mL/min | Follow-up, mo | |
|---|---|---|---|---|---|---|---|---|---|---|
| 6 months | 12 months | |||||||||
| 1 | 59 | F | Chronic glomerulonephritis | 3.5 | 13 | No | 0 | 112:52 | 107:54 | 20 |
| 2 | 61 | F | Polycystic | 4.5 | 14 | No | 0 | 102:60 | 109:56 | 20 |
| 3 | 55 | M | Diabetes | 4 | 20 | Yes | 10 | 122:82 | 122:83 | 20 |
| 4 | 49 | M | Hypertension | 8.5 | 15 | Yes | 9 | 157:37 | 145:41 | 20 |
| 5 | 59 | M | Wegener disease | 9 | 16 | Yes | 16 | 194:49 | 220:43 | 15 |
| 6 | 62 | M | Unknown | 4.25 | 15 | Yes | 13 | 164:54 | 149:59 | 15 |
| 7 | 36 | M | Polycystic | 4.25 | 16 | Yes | 10 | 189:61 | 146:83 | 14 |
| 8 | 45 | M | IgA nephropathy | 9.5 | 29 | Yes | 25 | 182:59 | 186:57 | 14 |
| 9 | 55 | M | Polycystic | 8.25 | 16 | Yes | 19 | 160:61 | 126:96 | 14 |
| 10 | 44 | M | Focal and segmental | 4 | 16 | Yes | 13 | 155:70 | 145:90 | 14 |
| glomerulosclerosis | ||||||||||
| 11 | 68 | M | Diabetes | 3 | 15 | Yes | 11 | 192:38 | 166:47 | 13 |
| 12 | 57 | M | Calcineurin inhibitor toxicity | 7 | 18 | Yes | 12 | 121:64 | 120:61 | 13 |
| 13 | 49 | M | Focal and segmental glomerulosclerosis | 13 | 12 | Yes | 2 | 160:54* | — | 3 |
| 14 | 77 | M | Hypertension | 25.5 | 11 | Yes | 5 | 109:61* | — | 3 |
CrCl = estimated creatinine clearance; F = female; LOS = length of stay; M = male; sCr = serum creatinine.
Value at 3-month follow-up.
Postoperative complications included 3 urinary tract infections, 1 perinephric hematoma requiring blood transfusion and 3 wound problems managed conservatively with wound packing. Seven of the 14 patients underwent biopsy because of prolonged delayed graft function (> 7 d). All of them showed mild to moderate acute tubular necrosis without any features of acute rejection.
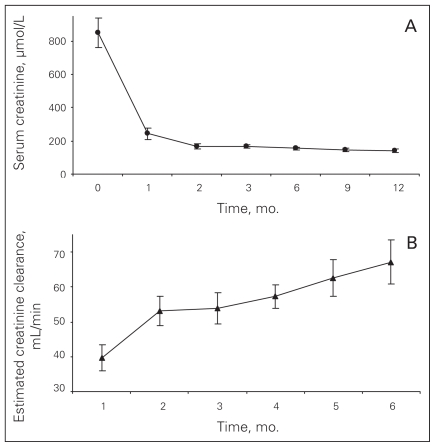
The mean length of stay (LOS) in hospital was 16 (SD 4, range 11–29) days. At 12 months follow-up (n = 12), the mean sCr level was 141 (SD 34, range 107–220) μmol/L with a corresponding estimated CrCl of 67 (SD 21, range 41–96) mL/min. Changes in sCr and CrCl over time are illustrated in Figure 2. None of the recipients had experienced clinical acute rejection after a mean follow-up of 14 (range 3–20) months.
Fig. 2.
Kidney function in 14 kidney recipients: (A) serum creatinine and (B) estimated creatinine clearance. Results are expressed as mean and standard error.
Liver transplantation
The characteristics of the patients who received liver transplants are shown in Table 4. All 10 recipients were alive after a mean follow-up of 11 (range 3–18) months. The mean age of the recipients was 51.8 (SD 14, range 26–69) years. The mean Model of End-Stage Liver Disease score was 22.1 (SD 9, range 13–40). Of the 10 liver transplant recipients, 6 had stable cirrhosis; 3 of these patients had hepatocellular carcinoma. The other 4 recipients had been admitted to hospital before the transplant because of decompensated liver disease. One of them had hepatorenal syndrome and another had fulminant liver failure requiring life support. At the time of the transplant, 5 recipients received an average of 4 units of packed red blood cells, and in one case (no. 5), the bleeding was so severe that the abdominal cavity required packing. This patient required a total of 11 units of packed red blood cells. Two days later when the coagulopathy was corrected, the patient returned to the OR for pack removal. The remaining 5 patients did not require blood transfusion.
Table 4.
Characteristics of liver recipients and outcomes
| Recipient | Age, yr | Sex | Diagnosis | MELD score | LOS, d | Ischemia time, min | Primary nonfunction | Biliary stricture | Follow-up, mo, status | |
|---|---|---|---|---|---|---|---|---|---|---|
| Warm | Cold | |||||||||
| 1 | 65 | F | Alcohol-induced liver cirrhosis | 25 | 11 | 26 | 7.25 | No | No | 20, alive |
| 2 | 47 | M | Primary sclerosing cholangitis | 21 | 11 | 26 | 5.5 | No | No | 20, alive |
| 3 | 69 | M | Hepatitis B virus Hepatocellular carcinoma | 20 | 68 | 124 | 3 | Yes | No | 14,* alive |
| 4 | 51 | M | Alcohol-induced liver cirrhosis Hepatocellular carcinoma | 20 | 12 | 88 | 4 | No | No | 14, alive |
| 5 | 58 | M | α1-anti-trypsin deficiency Hepatocellular carcinoma | 13 | 28 | 41 | 6.7 | No | Yes | 10, alive |
| 6 | 56 | M | Hepatitis C virus | 14 | 11 | 24 | 5 | No | No | 10, alive |
| 7 | 60 | F | Nonalcoholic steatohepatitis | 20 | 17 | 50 | 7 | No | No | 7, alive |
| 8 | 33 | M | Autoimmune hepatitis | 13 | 10 | 101 | 6 | No | No | 6, alive |
| 9 | 26 | F | Fulminant hepatic failure | 42 | 27 | 30 | 6.25 | No | No | 6, alive |
| 10 | 53 | M | Alcohol-induced liver cirrhosis | 33 | 13 | 37 | 6 | No | No | 3, alive |
F = female; LOS = length of stay; M = male; MELD = Model of End-Stage Liver Disease.
Retransplanted.
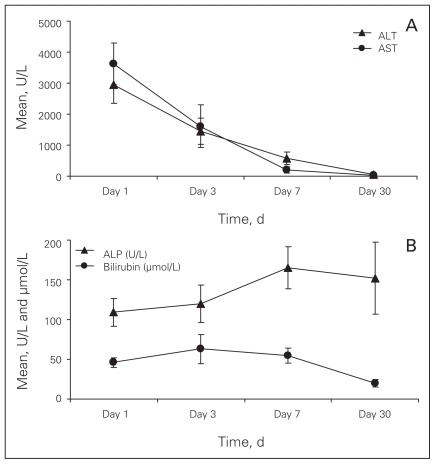
There was one episode of primary nonfunction of the liver (donor no. 3). This donor was 59 years old, and the WIT was 128 minutes. The liver biopsy (pretransplantation) showed a mild degree of cholestasis in zone 3, no evidence of liver cell necrosis or injury and less than 5% steatosis. The recipient received a retransplantation 5 days after the first transplant with a liver from a DND donor. If we exclude this patient, who had a 68-day hospital stay, the mean length of stay for the liver transplant recipients was 15 (SD 7, range 11–28) days. The mean liver enzyme and serum bilirubin levels on postoperative days 1, 3, 7 and 30 are shown in Figure 3. The mean peak aspartate aminotransferase (AST) and alanine aminotransferase (ALT) levels were 3631 U/L and 2947 U/L, respectively. The enzyme levels showed a steady decline to normal levels by the second week after transplant.
Fig. 3.
Mean liver enzymes and serum bilirubin in 9 liver recipients: (A) aspartate aminotransferase (AST) and alanine aminotransferase (ALT), and (B) alkaline phosphatase (ALP) and bilirubin. Results are expressed as mean and standard error. We excluded recipient no. 4 from this analysis because of primary nonfunction.
The liver recipients did not receive induction immunosuppression. The liver transplant immunosuppressive protocol was based on tacrolimus, mycophenolate mofetil and prednisone. The tacrolimus target trough levels were between 10 and 12 ng/mL during the first month, 8 and 10 ng/mL between 2 and 3 months and between 6 and 8 ng/mL thereafter.
No hepatic artery thrombosis or hepatic artery stenosis occurred. One recipient developed a biliary anastomotic stricture 3 weeks after transplantation; it resolved after endoscopic stenting. No evidence of ischemic-type biliary stricture was diagnosed by postoperative ultrasound or magnetic resonance cholangiography. One patient developed mild elevation of liver enzymes 1 month after liver transplant. Liver biopsy results showed no evidence of rejection, and the patient’s liver enzymes returned to normal 1 week later. Biopsies performed 3 months after transplant showed no histological abnormalities compared with baseline biopsies. None of the recipients experienced episodes of clinical acute rejection.
Discussion
Our initial experience with renal and liver allografts from DCD donors is encouraging and similar to the recent experiences reported by other centres.8–13 Our patient and graft survival rates were good, and they were comparable to our results with renal and liver transplants from DND donors. The positive outcomes achieved in this experience may have been influenced by the fact that we were stringent in our donor selection and excluded donors with specific risk factors such as age greater than 60 years. We considered it important to use conservative donor selection criteria to maximize the chance of success. It naturally follows that an initial successful experience would have a positive impact on the future of DCD in our program.
The 100% renal allograft survival rate is the most encouraging aspect of our experience. Although there was a higher incidence of delayed graft function, recipients had excellent 6-month and 1-year CrCl. The broad experience shows that the incidence of delayed graft function is more than twice what is seen with DND donors but that the 1- and 3-year graft survival rates are not significantly different.14–20 It is accepted that the higher incidence of delayed graft function is related to ischemic injury sustained during the period of warm ischemia. Thus, restriction of WIT to less than 2 hours is desirable, and some centres restrict it to only 1 hour. To compensate for the expected warm ischemic injury, we made every effort to keep the period of cold ischemia at a minimum. This approach imposed logistical difficulties because recipient surgery often required 2 or even 3 ORs working simultaneously. Additional resources, specifically OR staff, were required. Also, delayed graft function required temporary dialysis support and increased the length of stay in hospital for recipients, thus affecting hospital resources and increasing medical costs.21
Although delayed graft function has been associated with poorer graft survival in kidneys transplanted from DND donors,22,23 this association is less apparent in kidneys transplanted from DCD donors.24 The difference in the long-term impact of delayed graft function in these 2 types of donors may be related in part to the significant release of proinflammatory cytokines and catecholamines associated with neurologic death, which results in injury to organs in the donor before their procurement.25 The absence of these physiologic derangements in DCD donors may, in some measure, compensate for the injury caused by warm ischemia in DCD donors. There is evidence that a short CIT can improve immediate function in both DND and DCD, in a cost-effective fashion.19,26,27 We made whatever arrangements were necessary to minimize CIT and thereby optimize graft function. Nevertheless, a high incidence of delayed graft function occurred. We did not utilize machine pulsatile perfusion during the cold ischemic period to potentially reduce graft injury during the preservation period,16,28 because its effectiveness in preventing delayed graft function remains controversial.19,29 However, because the delayed graft function rate in our series was high even with a short average CIT, the issue of machine perfusion needs to be revisited.
According to the CCDT guidelines and other published reports,4,13,17 WIT should not exceed 2 hours. Although kidneys can tolerate long warm ischemia periods compared with other solid organs, extending the WIT increases the risk of cortical necrosis and primary nonfunction, particularly in organs from more marginal donors. Despite exceeding the 2-hour guideline for WIT in 2 donors, good outcomes were achieved, reflecting the individual variability of donor organs to sustain ischemic injury. In these 2 cases (donor nos. 3 and 6), cardiac arrest occurred within 2 hours but the time required to transfer the donor to the OR extended the WIT to more than 120 minutes. It is still our policy to restrict the WIT for kidneys to less than 2 hours, but rigid adherence to this time frame would have resulted in the loss of 4 kidneys for transplants that had successful outcomes. Therefore, other factors such as age of the donor and duration of hypotension in the agonal period need to be considered in individual cases.
In this study, the patient population was not highly sensitized to panel reactive antibody and was at low risk for rejection. Nevertheless, no clinical rejection occurred in this group of 14 kidney recipients, again raising the possibility that DCD donor organs may avoid substantial proinflammatory cytokine damage and thus decrease immune “visibility.”30,31 Clearly this is an area that requires further study. Anti–T lymphocyte antibody (Thymoglobulin) was used for induction immunosuppression in all renal recipients for its potent effect on T-cell function and its ability to reduce rates of acute rejection below 15%.32 However, it is evident that other factors in early rejection including non–T cells, innate immune cells (neutrophils, monocytes, natural killer cells) and parenchymal cells activated by ischemia-reperfusion may be targeted to abrogate rejection in these patients.33,34 Thus, DCD organs, through the reduction of inflammatory damage to the graft, may be at an immunologic advantage.
The outcomes in the liver recipients (100% patient and 90% allograft survival) have also been good. Single-centre reports from the University of Wisconsin, University of Pennsylvania and the Albert Einstein Institute7,8,35 demonstrated similar outcomes, including survival and complication rates, between recipients of DCD and DND livers. With increasing experience, a difference in 3-year graft survival was shown in recipients of DCD liver grafts.18,36 The latest experience shows a 10%–15% overall reduction in liver graft survival from DCD donors.37,38 Further experience in our program will determine if we observe slightly inferior results in terms of survival rates.
Our one case of liver primary nonfunction was likely due to prolonged WIT as well as donor age. The decision to proceed with liver transplantation in that case was made because, during the initial 90 minutes of WIT, the mean arterial pressure remained greater than 65 mm Hg and the oxygen saturation level remained above 70%, suggesting that there was adequate tissue oxygenation. Moreover, at the time of the organ procurement, the liver flushed well and had a normal appearance. Nevertheless, because of the nonfunction of this graft, we currently limit WIT for liver donation to 90 minutes. Despite the fact that we had several donors with a WIT above 30 minutes, only 2 of them had a mean arterial pressure below 55 mm Hg for more than 30 minutes during the agonal period. We believe that there is significant ischemic injury to the organs when the mean arterial pressure is below 55 mm Hg. Rather than restricting donors on the basis of an absolute WIT, a cutoff based on mean arterial pressure below a certain level for a certain length of time may be a better criterion for the safe use of organs from DCD donors.
The increased incidence of biliary complications, which occur in up to 38% of recipients of DCD livers, is assumed to be on the basis of ischemic injury to the biliary tree during the warm ischemia priod.7,39 Bile ducts are more sensitive to ischemia and reperfusion injury than are hepatocytes. The combination of these 2 factors may explain the higher incidence of ischemic-type strictures in grafts from DCD donors.7,40 Whether the single incidence of a biliary anastomotic stricture in our experience was a consequence of a DCD graft specifically or was merely an example of the 10%–15% incidence seen after all liver transplants is uncertain. There is some evidence that the use of HTK solution, compared with University of Wisconsin solution, for preservation may play a protective role against ischemic-type biliary stricture owing to its low viscosity and better perfusion of the biliary plexus.41,42 We explain to potential recipients of DCD livers that the situation is not ideal and that there is a higher rate of graft lost requiring repeat transplantation. Our experience has been that no recipient has declined transplantation after this has been explained to them.
In the context of perioperative risk and short-term outcome, it is important to recognize that graft and patient survival after liver transplantation depend on many factors, both related to the donor and recipient. Donor age above 60 years, WIT above 30 minutes and CIT above 10 hours are known graft-related risk factors. Repeat liver transplantation and severity of liver failure, especially the need for life support at the time of transplantation, are recipient risk factors associated with inferior outcomes.37,43 When none of these risk factors are present, there is no difference in allo-graft survival between grafts from DCD and DND donors. Graft survival is also comparable when there are no recipient risk factors but only one graft risk factor.37,43 In our experience, we have had success transplanting DCD liver grafts in one recipient who was critically ill with fulminant hepatic failure and was on life support and in a second recipient with acute kidney failure associated with decompensated cirrhosis. It is our policy to offer a DCD liver to the recipient who is the first priority on the waiting list. We have not attempted to preferentially allocate DCD livers or kidneys to recipients with better or poorer risk. Our experience so far suggests that we should not alter this approach.
We feel a strong obligation to control the one variable, CIT, that is known to affect graft outcome. We believe it is a crucial factor, and we commit personnel, time and resources to minimize the deleterious effect of cold ischemia. This approach requires that recipients are admitted and prepared before donor surgery. Effective communication between the different teams involved (ICU, donor team and recipient transplant team) is mandatory. A dedicated OR staff on standby for up to 2 hours for donor procurement is necessary. In liver transplantation, where CIT has more impact, timing of the surgical procedures is very important. The recipient surgery overlaps with the donor procedure. Consequently, several operating rooms are committed to simultaneous procedures to minimize CIT. The logistics are a challenge, and the use of hospital resources is substantial, but our view is that it is not only justified but also necessary if good outcomes are to be obtained.
Although the concept of DCD is an old one, it is new for most health care practitioners and hospital personnel because they were not directly involved in organ donation and transplantation more than 30 years ago. After DCD was initiated in our centre, we began institutional education sessions and seminars for ICU staff, OR personnel and administrators. We explained its nature and practice, familiarized individuals with the CCDT guidelines and addressed the concerns and questions from hospital staff. These sessions were invaluable in educating hospital personnel and helping them to understand a procedure that, for most, was entirely foreign. We are convinced that this education and support process is very important and can directly affect the acceptance and success of DCD.44 In addition, formal policies and standard operating procedures were developed and approved by our administration and Medical Advisory Committee.
Currently, there are about 4000 individuals on organ transplant waiting lists in Canada. The potential impact of DCD on increasing the supply of organs is estimated to be substantial. Over the last decade, there has been a 6-fold increase in the number of centres using organs from DCD donors in the Unites States.38 At selected centres, transplant activity has increased by up to 25%.39,45 Two analyses have examined the potential for increasing the number of kidneys available in Canada for transplantation if there was a concerted effort to use DCD organs. It has been estimated that DCD has the potential to increase kidney donation by up to 30%.46,47 During our first 18 months, we saw a 14% increase in organ donors in our program. We believe that this represents only a fraction of what can be accomplished. In our experience, we were fortunate to receive referrals from centres outside London, including regional hospitals that have no transplant programs. This collaboration brought a substantial number of donor organs that would otherwise have not been used. Donation after cardiac death is a concept that should be widely disseminated and taught in hospitals throughout Canada to reduce the number of patients dying of organ failure. This type of donation can be an important means of increasing the number of organs available for transplant, and the practice should be encouraged.
Acknowledgements
We thank Corinne Weernink for her assistance with manuscript preparation and constructive suggestions.
Footnotes
Competing interests: None declared.
Contributors: Drs. Hernandez-Alejandro, Caumartin, Ghent, Levstik and Wall designed the study. Drs. Hernandez-Alejandro, Caumartin, Marotta, Ghent, Levstik, Quan, Muirhead, House, Jevnikar and Wall acquired the data, which Drs. Hernandez-Alejandro, Caumartin, Levstik, McAlister, Luke and Wall analyzed. Drs. Hernandez-Alejandro, Caumartin and Wall wrote the article. All authors reviewed the article and approved its publication.
References
- 1.Cuende N, Cuende JI, Fajardo J, et al. Effect of population aging on the international organ donation rates and the effectiveness of the donation process. Am J Transplant. 2007;7:1526–35. doi: 10.1111/j.1600-6143.2007.01792.x. [DOI] [PubMed] [Google Scholar]
- 2.Institute of Medicine and National Academy of Sciences. Non-heartbeating organ transplantation: medical and ethical issues in procurement. Washington: National Academy Press; 1997. [Google Scholar]
- 3.Knoll GA, Mahoney JE. Non-heart-beating organ donation in Canada: Time to proceed. CMAJ. 2003;169:302–3. [PMC free article] [PubMed] [Google Scholar]
- 4.Shemie SD, Baker AJ, Knoll G, et al. National recommendations for donation after cardiocirculatory death in Canada. CMAJ. 2006;175:S1. doi: 10.1503/cmaj.060895. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lewis J, Peltier J, Nelson H, et al. Development of the University of Wisconsin Donation After Cardiac Death Evaluation Tool. Prog Transplant. 2003;13:265–73. doi: 10.1177/152692480301300405. [DOI] [PubMed] [Google Scholar]
- 6.Ethics Committee, American College of Critical Care Medicine; Society of Critical Care Medicine. Recommendations for nonheart-beating organ donation. Crit Care Med. 2001;29:1826–31. doi: 10.1097/00003246-200109000-00029. [DOI] [PubMed] [Google Scholar]
- 7.Abt P, Crawford M, Desai N, et al. Liver transplantation from controlled non-heart-beating donors: an increased incidence of biliary complications. Transplantation. 2003;75:1659–63. doi: 10.1097/01.TP.0000062574.18648.7C. [DOI] [PubMed] [Google Scholar]
- 8.D’Alessandro AM, Hoffmann RM, Knechtle SJ, et al. Liver transplantation from controlled non-heart-beating donors. Surgery. 2000;128:579–88. doi: 10.1067/msy.2000.108421. [DOI] [PubMed] [Google Scholar]
- 9.Fujita S, Mizuno S, Fujikawa T, et al. Liver transplantation from donation after cardiac death: a single center experience. Transplantation. 2007;84:46–9. doi: 10.1097/01.tp.0000267424.88023.7b. [DOI] [PubMed] [Google Scholar]
- 10.Cooper JT, Chin LT, Krieger NR, et al. Donation after cardiac death: the University of Wisconsin experience with renal transplantation. Am J Transplant. 2004;4:1490–4. doi: 10.1111/j.1600-6143.2004.00531.x. [DOI] [PubMed] [Google Scholar]
- 11.Reich DJ, Munoz SJ, Rothstein KD, et al. Controlled non-heart-beating donor liver transplantation: a successful single center experience, with topic update. Transplantation. 2000;70:1159–66. doi: 10.1097/00007890-200010270-00006. [DOI] [PubMed] [Google Scholar]
- 12.Tojimbara T, Fuchinoue S, Iwadoh K, et al. Improved outcomes of renal transplantation from cardiac death donors: a 30-year single center experience. Am J Transplant. 2007;7:609–17. doi: 10.1111/j.1600-6143.2007.01664.x. [DOI] [PubMed] [Google Scholar]
- 13.Whiting JF, Delmonico F, Morrissey P, et al. Clinical results of an organ procurement organization effort to increase utilization of donors after cardiac death. Transplantation. 2006;81:1368–71. doi: 10.1097/01.tp.0000179641.82031.ea. [DOI] [PubMed] [Google Scholar]
- 14.Casavilla A, Ramirez C, Shapiro R, et al. Experience with liver and kidney allografts from non-heart-beating donors. Transplantation. 1995;59:197–203. doi: 10.1097/00007890-199501000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Butterworth PC, Taub N, Doughman TM, et al. Are kidneys from non-heart-beating donors second class organs. Transplant Proc. 1997;29:3567–8. doi: 10.1016/s0041-1345(97)01143-3. [DOI] [PubMed] [Google Scholar]
- 16.Balupuri S, Buckley P, Snowden C, et al. The trouble with kidneys derived from the non heart-beating donor: a single center 10-year experience. Transplantation. 2000;69:842–6. doi: 10.1097/00007890-200003150-00029. [DOI] [PubMed] [Google Scholar]
- 17.Bernat JL, D’Alessandro AM, Port FK, et al. Report of a national conference on donation after cardiac death. Am J Transplant. 2006;6:281–91. doi: 10.1111/j.1600-6143.2005.01194.x. [DOI] [PubMed] [Google Scholar]
- 18.Doshi MD, Hunsicker LG. Short- and long-term outcomes with the use of kidneys and livers donated after cardiac death. Am J Transplant. 2007;7:122–9. doi: 10.1111/j.1600-6143.2006.01587.x. [DOI] [PubMed] [Google Scholar]
- 19.Locke JE, Segev DL, Warren DS, et al. Outcomes of kidneys from donors after cardiac death: implications for allocation and preservation. Am J Transplant. 2007;7:1797–807. doi: 10.1111/j.1600-6143.2007.01852.x. [DOI] [PubMed] [Google Scholar]
- 20.Leichtman AB, Cohen D, Keith D, et al. Kidney and pancreas transplantation in the United States, 1997–2006: the HRSA Breakthrough Collaboratives and the 58 DSA Challenge. Am J Transplant. 2008;8:946–57. doi: 10.1111/j.1600-6143.2008.02173.x. [DOI] [PubMed] [Google Scholar]
- 21.Saidi RF, Elias N, Kawai T, et al. Outcome of kidney transplantation using expanded criteria donors and donation after cardiac death kidneys: realities and costs. Am J Transplant. 2007;7:2769–74. doi: 10.1111/j.1600-6143.2007.01993.x. [DOI] [PubMed] [Google Scholar]
- 22.Shoskes DA, Cecka JM. Deleterious effects of delayed graft function in cadaveric renal transplant recipients independent of acute rejection. Transplantation. 1998;66:1697–701. doi: 10.1097/00007890-199812270-00022. [DOI] [PubMed] [Google Scholar]
- 23.Quiroga I, McShane P, Koo DD, et al. Major effects of delayed graft function and cold ischaemia time on renal allograft survival. Nephrol Dial Transplant. 2006;21:1689–96. doi: 10.1093/ndt/gfl042. [DOI] [PubMed] [Google Scholar]
- 24.Brook NR, White SA, Waller JR, et al. Non-heart beating donor kidneys with delayed graft function have superior graft survival compared with conventional heart-beating donor kidneys that develop delayed graft function. Am J Transplant. 2003;3:614–8. doi: 10.1034/j.1600-6143.2003.00113.x. [DOI] [PubMed] [Google Scholar]
- 25.Pratschke J, Neuhaus P, Tullius SG. What can be learned from brain-death models. Transpl Int. 2005;18:15–21. doi: 10.1111/j.1432-2277.2004.00018.x. [DOI] [PubMed] [Google Scholar]
- 26.Roodnat JI, Mulder PG, Van Riemsdijk IC, et al. Ischemia times and donor serum creatinine in relation to renal graft failure. Transplantation. 2003;75:799–804. doi: 10.1097/01.TP.0000056632.00848.8D. [DOI] [PubMed] [Google Scholar]
- 27.Beiras-Fernandez A, Chappel D, Thein E, et al. Impact of small variations of ischemia time after polyclonal antithymocyte globulins in a nonhuman primate model of ischemia-reperfusion injury. Transplant Proc. 2004;36:2579–82. doi: 10.1016/j.transproceed.2004.09.049. [DOI] [PubMed] [Google Scholar]
- 28.Moustafellos P, Hadjianastassiou V, Roy D, et al. The influence of pulsatile preservation in kidney transplantation from non-heart-beating donors. Transplant Proc. 2007;39:1323–5. doi: 10.1016/j.transproceed.2006.11.026. [DOI] [PubMed] [Google Scholar]
- 29.Wight J, Chilcott J, Holmes M, et al. The clinical and cost-effectiveness of pulsatile machine perfusion versus cold storage of kidneys for transplantation retrieved from heart-beating and non-heart-beating donors. Health Technol Assess. 2003;7:1–94. doi: 10.3310/hta7250. [DOI] [PubMed] [Google Scholar]
- 30.Boros P, Bromberg JS. New cellular and molecular immune pathways in ischemia/reperfusion injury. Am J Transplant. 2006;6:652–8. doi: 10.1111/j.1600-6143.2005.01228.x. [DOI] [PubMed] [Google Scholar]
- 31.Wasowska BA, Lee CY, Halushka MK, et al. New concepts of complement in allorecognition and graft rejection. Cell Immunol. 2007;248:18–30. doi: 10.1016/j.cellimm.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Beiras-Fernandez A, Thein E, Hammer C. Induction of immunosuppression with polyclonal antithymocyte globulins: an overview. Exp Clin Transplant. 2003;1:79–84. [PubMed] [Google Scholar]
- 33.Beiras-Fernandez A, Chappell D, Hammer C, et al. Influence of polyclonal anti-thymocyte globulins upon ischemia-reperfusion injury in a non-human primate model. Transpl Immunol. 2006;15:273–9. doi: 10.1016/j.trim.2006.02.003. [DOI] [PubMed] [Google Scholar]
- 34.Goggins WC, Pascual MA, Powelson JA, et al. A prospective, randomized, clinical trial of intraoperative versus postoperative Thymoglobulin in adult cadaveric renal transplant recipients. Transplantation. 2003;76:798–802. doi: 10.1097/01.TP.0000081042.67285.91. [DOI] [PubMed] [Google Scholar]
- 35.Manzarbeitia CY, Ortiz JA, Jeon H, et al. Long-term outcome of controlled, non-heart-beating donor liver transplantation. Transplantation. 2004;78:211–5. doi: 10.1097/01.tp.0000128327.95311.e3. [DOI] [PubMed] [Google Scholar]
- 36.Feng S, Goodrich NP, Bragg-Gresham JL, et al. Characteristics associated with liver graft failure: the concept of a donor risk index. Am J Transplant. 2006;6:783–90. doi: 10.1111/j.1600-6143.2006.01242.x. [DOI] [PubMed] [Google Scholar]
- 37.Mateo R, Cho Y, Singh G, et al. Risk factors for graft survival after liver transplantation from donation after cardiac death donors: an analysis of OPTN/UNOS data. Am J Transplant. 2006;6:791–6. doi: 10.1111/j.1600-6143.2006.01243.x. [DOI] [PubMed] [Google Scholar]
- 38.Pomfret EA, Fryer JP, Sima CS, et al. Liver and intestine transplantation in the United States, 1996–2005. Am J Transplant. 2007;7:1376–89. doi: 10.1111/j.1600-6143.2007.01782.x. [DOI] [PubMed] [Google Scholar]
- 39.Foley DP, Fernandez LA, Leverson G, et al. Donation after cardiac death: the University of Wisconsin experience with liver transplantation. Ann Surg. 2005;242:724–31. doi: 10.1097/01.sla.0000186178.07110.92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Cutrin JC, Cantino D, Biasi F, et al. Reperfusion damage to the bile canaliculi in transplanted human liver. Hepatology. 1996;24:1053–7. doi: 10.1002/hep.510240512. [DOI] [PubMed] [Google Scholar]
- 41.Fung JJ, Eghtesad B, Patel-Tom K. Using livers from donation after cardiac death donors — a proposal to protect the true Achilles heel. Liver Transpl. 2007;13:1633–6. doi: 10.1002/lt.21388. [DOI] [PubMed] [Google Scholar]
- 42.Mangus RS, Fridell JA, Vianna RM, et al. Comparison of histidine-tryptophan-ketoglutarate solution and University of Wisconsin solution in extended criteria liver donors. Liver Transpl. 2008;14:365–73. doi: 10.1002/lt.21372. [DOI] [PubMed] [Google Scholar]
- 43.Lee KW, Simpkins CE, Montgomery RA, et al. Factors affecting graft survival after liver transplantation from donation after cardiac death donors. Transplantation. 2006;82:1683–8. doi: 10.1097/01.tp.0000250936.73034.98. [DOI] [PubMed] [Google Scholar]
- 44.D’Alessandro AM, Peltier JW, Phelps JE. Increasing organ donations after cardiac death by increasing DCD support among health care professionals: a case report. Am J Transplant. 2008;8:897–904. doi: 10.1111/j.1600-6143.2008.02155.x. [DOI] [PubMed] [Google Scholar]
- 45.Punch JD, Hayes DH, LaPorte FB, et al. Organ donation and utilization in the United States, 1996–2005. Am J Transplant. 2007;7:1327–38. doi: 10.1111/j.1600-6143.2007.01779.x. [DOI] [PubMed] [Google Scholar]
- 46.Campbell GM, Sutherland FR. Non-heart-beating organ donors as a source of kidneys for transplantation: a chart review. CMAJ. 1999;160:1573–6. [PMC free article] [PubMed] [Google Scholar]
- 47.Lacroix JD, Mahoney JE, Knoll GA. Renal transplantation using non-heart-beating donors: a potential solution to the organ donor shortage in Canada. Can J Surg. 2004;47:10–4. [PMC free article] [PubMed] [Google Scholar]