Abstract
Background
In July 2007, a large Canadian teaching hospital realigned its general surgery services into elective general surgery subspecialty-based services (SUBS) and a new urgent surgical care (USC) service (also know in the literature as an acute care surgery service). The residents on SUBS had their number of on-call days reduced to enable them to focus on activities related to SUBS. Our aim was to examine the effect of the creation of the USC service on the educational experiences of SUBS residents.
Methods
We enrolled residents who were on SUBS for the 6 months before and after the introduction of the USC service. We collected data by use of a survey, WEB eVAL and recorded attendance at academic half days. Our 2 primary outcomes were residents’ attendance at ambulatory clinics and compliance with the reduction in the number of on-call days. Our secondary outcomes included residents’ time for independent study, attendance at academic half days, operative experience, attendance at multidisciplinary rounds and overall satisfaction with SUBS.
Results
Residents on SUBS had a decrease in the mean number of on-call days per resident per month from 6.28 to 1.84 (p = 0.006), an increase in mean attendance at academic half days from 65% to 87% (p = 0.028), at multidisciplinary rounds (p = 0.002) and at ambulatory clinics and an increase in independent reading time (p = 0.015), and they reported an improvement in their work environment. There was no change in the amount of time residents spent in the operating room or in their overall satisfaction with SUBS.
Conclusion
Residents’ education in the SUBS structure was positively affected by the creation of a USC service. Compliance with the readjustment of on-call duties was high and was identified as the single most significant factor in enabling residents to take full advantage of the unique educational opportunities available only while on SUBS.
Abstract
Contexte
En juillet 2007, un grand centre hospitalier universitaire canadien a réorganisé ses services de chirurgie générale en les subdivisant en deux éléments : un service de chirurgie générale élective (SCGE) basé sur les surspécialités et un nouveau service de chirurgie d’urgence (SCU) (qui porte dans la littérature l’appellation de service de chirurgie de soins actifs). On a réduit le nombre de jours de garde des résidents assignés au SCGE afin de leur permettre de se consacrer aux activités de ce service. Notre but était de mesurer l’effet de la mise sur pied d’un SCU sur l’expérience d’ap-prentissage des résidents assignés au SCGE.
Méthodes
Notre étude a porté sur les résidents assignés au SCGE pendant les six mois précédant et suivant la création du SCU. Nous avons recueilli les données au moyen du questionnaire WEB eVAL et nous avons enregistré les présences aux demi-journées de formation. Nos deux principaux paramètres étaient la participation des résidents aux cliniques ambulatoires et leur conformité à la réduction du nombre de leurs jours de garde. Nos paramètres secondaires incluaient le temps consacré par les résidents à la formation autonome, la participation aux demi-journées de formation, l’expérience chirurgicale, la participation aux tournées pluridisciplinaires et le degré général de satisfaction à l’endroit du SCGE.
Résultats
Chez les résidents assignés au SCGE, on a enregistré une baisse du nom-bre moyen de jours de garde par résident par mois, soit de 6,28 à 1,84 (p = 0,006), une augmentation de 65 % à 87 % de la participation moyenne aux demi-journées de formation (p = 0,028), aux tournées pluridisciplinaires (p = 0,002) et aux cliniques ambula-toires, de même qu’une augmentation du temps consacré à la formation autonome (p = 0,015); les résidents ont de plus fait mention d’une amélioration de leur environ-nement de travail. On n’a noté aucun changement quant au temps passé par les rési-dents au bloc opératoire ou quant à leur satisfaction globale à l’endroit du SCGE.
Conclusion
La mise sur pied du SCU a exercé un effet positif sur les résidents assignés au SCGE. Leur conformité à la réorganisation des tâches de garde a été élevée et s’est révélée être le facteur le plus significatif leur ayant permis de profiter au maximum de l’expérience didactique unique offerte exclusivement au SCGE.
Teaching hospitals across North America must deliver highly specialized elective surgical care and timely interventions in acute surgical illness while providing a supportive and high-quality learning environment for surgical residents. Several recent studies have described how changes in surgical service delivery can positively affect residents’ education. The introduction of a night-float system decreases resident fatigue and increases residents’ independent reading.1 Changing from traditional team-based services to apprenticeship, small team and night-float–based services results in residents experiencing increased operative time, increased satisfaction with their rotations and increased quality of life.2 Implementing surgical services that allow residents to develop goal-oriented work styles is associated with residents having increased operative exposure, increased work satisfaction and decreased mental stress.3
In recent years, many institutions have adopted acute care surgery models to meet the clinical challenges posed by complex and acute general surgical conditions and to balance the needs of diverse surgical staff with interests in subspecialty-based elective surgery and emergency general surgery. These surgery services have become the topic of intense interest and discussion in Canada and the United States. Studies and editorial comments have stated several proposed and observed benefits of acute surgery models, including improved patient care,4 increased job satisfaction for trauma surgeons,5 increased operative volume for surgeons performing elective procedures6 and development of educational programs.7 Although studies have carefully described acute care surgery services3,6,8 and evaluated fellowship training based on such services,8 none have evaluated how they affect the education of general surgery residents despite the fact that residents are directly affected by service realignments. Some authors have advocated for a need to study the effect of acute surgery models on resident education before these models are widely implemented in academic centres.9,10
We undertook this study to examine the effect of the introduction of urgent surgical care (USC) services at a large quaternary care teaching institution on the educational experience of general surgery residents in the elective general surgery subspecialty-based service (SUBS). We hypothesized that the USC model would enhance residents’ learning experiences on SUBS by enabling them to attend more operations, clinics, multidisciplinary conferences and educational rounds and by allowing them more time for independent study focused on their subspecialty.
Methods
The Vancouver General Hospital (VGH) is a quaternary care facility and a large teaching institution for the University of British Columbia. Until recently, the general surgery services at VGH had been divided into 4 SUBS. All residents and attending general surgeons provided on-call duties for general surgery, and emergency general surgery patients were admitted to the attending on-call’s SUBS team. This structure meant that during the daytime, residents on SUBS were not always able to participate fully in their staff surgeons’ operations, ambulatory clinics, multidisciplinary conferences or educational rounds because they were spending substantial portions of time in the emergency department, and, conversely, that emergency consultations were frequently delayed when on-call residents and staff were involved in elective surgical cases.
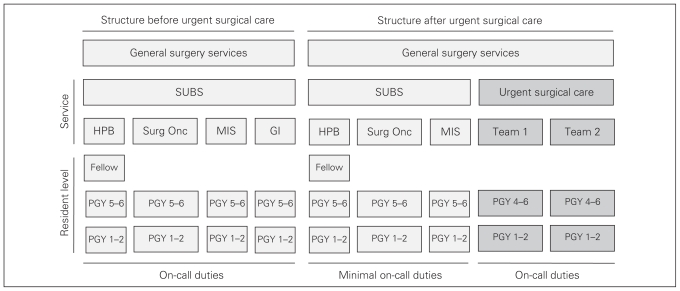
In July 2007, VGH introduced the USC service. The USC teams assumed responsibility for almost all urgent consultations and on-call duties following a float model and left elective subspecialty general surgery to the remaining 3 SUBS comprised of hepatobiliary, surgical oncology and minimally invasive surgery services (Fig. 1). Each SUBS was composed of 1 senior (postgraduate year [PGY] 4–6) resident, 1–2 junior (PGY 1–2) residents and 3–5 attending surgeons. The total number of residents at VGH increased from an average of 8.3 per month (6.8 general surgery residents and 1.5 off-service residents) before July 2007 to an average of 12 per month (9.7 general surgery residents and 2.4 off service residents) after July 2007. The number of on-call days per resident per month was purposefully reduced to 1–2 for residents on SUBS to enable them to focus on activities related to the subspecialty services. We performed this study to examine the feasibility of this new model and the effect of the reduction in the number of call days and the implementation of the USC service on residents’ educational experiences and workload while on SUBS. The Office of Research Services Behavioural Research Ethics Board at the University of British Columbia approved this study.
Fig. 1.
General surgery services structure before and after the implementation of the urgent surgical care (USC) service. Before the introduction of the USC service, the general surgery services consisted solely of the general surgery subspecialty-based services (SUBS) and all residents on SUBS performed on-call duties. After the introduction of the USC service, the general surgery services were divided into SUBS and USC services, and residents on SUBS did not perform on-call duties. GI = gastroenterology; HPB = hepatobiliary; MIS = minimally invasive surgery; PGY = postgraduate year; Surg Onc = surgical oncology.
Participants and study period
The experiences of 2 groups of residents were compared, first the cohort of general surgery residents on SUBS at VGH for the 6 months before the introduction of the USC service (January 2007 to June 2007), then the cohort of general surgery residents on SUBS at VGH for the 6 months after the introduction of the USC service (July 2007 to December 2007).
Data collection
We distributed a survey (Box 1) and consent forms to all eligible residents in July 2007 and January 2008 by placing them in their hospital mailboxes. The survey and consent forms were returned anonymously in unmarked envelopes to one of the investigator’s hospital mailbox.
Box 1.
Resident survey
For the following questions, please answer with 1–5 where: 1 = strongly disagree, 2 = disagree, 3 = neither agree nor disagree, 4 = agree and 5 = strongly agree.
While on service I had sufficient time for independent study.
While on service I was able to attend multidisciplinary conferences or rounds.
While on service I was able to attend day-care surgeries at sites other than VGH.
Please add any comments you have regarding the new structure of general surgery services at VGH.
VGH = Vancouver General Hospital.
We collected data from the survey, published on-call schedules, recorded attendance at academic half days (sign-in sheet) and WEB eVAL (Box 2), the electronic system that sends evaluations to residents on completion of a rotation. The general surgery program assistant collated the data from the sign-in sheets at academic half days and WEB eVALs with all identifiers removed and submitted the data to the investigators. The data for the cohort enrolled in the study before the implementation of the USC services were collected in July 2007, and the data for the cohort enrolled after were collected in January 2008.
Box 2.
Questions from the WEB eVAL
Did this service offer appropriate balance among ward, OR, consults and emergency and outpatient clinics?
| __Yes | __ No |
On average, how many hours per week did you attend clinic?
| __ 0 | __ < 2 | __ 2–4 | __ > 4 |
Was this an appropriate amount of time?
| __ Yes | __ No |
Monday to Friday: How many days did you spend in the OR?
| __ 1 | __ 2 | __ 3 | __ 4 | __ 5 |
Did your technical skills improve on this service?
| __ Yes | __ No |
Was the patient volume appropriate for your level?
| __ Too slow | __ Right volume | __ Too busy |
Overall rating
| __ Unsatisfactory | __ Marginal | __ Satisfactory | __ Good | __ Outstanding |
OR = operating room.
Outcomes
The 2 primary outcomes established a priori were residents’ attendance at ambulatory clinics and compliance with the reduction in number of on-call days. Our secondary outcomes, which were also established a priori, included residents’ time for independent study, attendance at academic half days, operative experience, attendance at service rounds and overall satisfaction with SUBS.
Data analysis
We analyzed residents’ comments collected from the survey and WEB eVAL to determine trends in general sentiments. We grouped residents’ comments about the impact of on-call and ward duties on their educational experiences into 3 categories: those related to their ability to attend scheduled teaching activities and the operating room, those related to their work environment and those related to ambulatory clinics. We then categorized the comments as negative if they contained negative words and expressions (e.g., “unable,” “pulled out,” “never able,” “rarely,” “unmanageable”) or as positive if they contained positive words and expressions (e.g., “reasonable,” “adequate,” “nice,” “great,” “supportive”).
We performed statistical analysis using SPSS version 15 software. We used independent samples t tests for parametric data and the Mann–Whitney U for nonparametric data.
RESULTS
There were 18 general surgery residents (8 senior and 10 junior) on SUBS before the implementation of the USC service and 16 general surgery residents (6 senior and 10 junior) after. The response rates for the survey and WEB eVAL were 65% (22/34) and 97% (33/34), respectively. The records of the academic half day attendance and call schedules were complete for both cohorts.
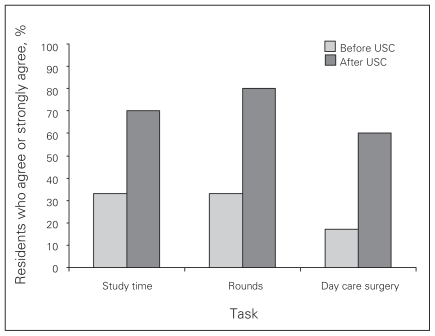
Survey
Residents on SUBS reported statistically significant increases in time for independent study (p = 0.015) and attendance at multidisciplinary conferences or rounds (p = 0.002; Fig. 2). There was no significant difference in reported time for attendance at day-care surgeries at sites other than VGH (p = 0.06) after the implementation of the USC service (Fig. 2).
Fig. 2.
Survey results for residents on the general surgery subspecialty-based service before and after the introduction of the urgent surgical care (USC) service at Vancouver General Hospital (VGH). This graph shows the proportion of residents who agreed or strongly agreed that they had adequate time for independent study, the ability to attend multidisciplinary rounds and the opportunity to attend day care surgeries at sites other than VGH.
On-call days
The mean number of on-call days per month per resident decreased significantly from 6.28 to 1.94 call (p < 0.001). The mean number of call days per month per resident dropped for both senior and junior residents, and these drops were statistically significant: from 6.28 to 1.57 (p < 0.001) for senior residents and 6.40 to 2.0 (p < 0.001) for junior residents.
Attendance at academic half days
Residents’ mean attendance at academic half days increased significantly from 65% to 87% (p = 0.028). The attendance rate increased for both senior (from 60% to 79%, p = 0.26) and junior residents (from 70% to 91%, p = 0.08); however, these increases were not statistically significant. It was clear from the subgroup analyses that the significant increase in academic half day attendance for the group as a whole was driven by the junior residents.
WEB eVAL
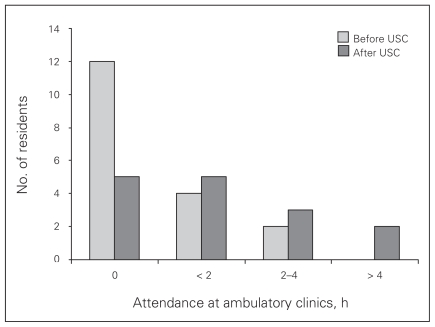
Residents reported a statistically significant increase (p = 0.04) in the amount of time spent at ambulatory clinics (Fig. 3). Before the implementation of the USC service, most residents (12/18) reported spending 0 hours per week at ambulatory clinics, whereas after implementation of the service, most residents reported spending more than 0 hours per week in clinics (10/15). The number of residents who felt that they were spending an appropriate amount of time at ambulatory clinics increased significantly (from 5/17 to 8/12, p = 0.028).
Fig. 3.
Mean number of hours spent at ambulatory clinics by residents on the general surgery subspecialty-based service before and after the introduction of an urgent surgical care (USC) service at Vancouver General Hospital.
After the introduction of the USC service, the proportion of residents on SUBS who felt that their surgical service offered an appropriate balance among ward work, operating room time, time spent seeing patients in consultation and in the emergency department, and time spent at out-patient clinics increased from 67% (12/18) to 93% (14/15); however, this increase was not significant (p = 0.07).
Most residents on SUBS felt that patient volume was appropriate both before and after the introduction of the USC service (67% [12/18] v. 53% [8/15]). The proportion of residents who felt that patient volume was too high declined from 22% (4/18) to 0% (0/15), whereas the proportion of residents who felt the patient volume was too low increased significantly from 11% (2/18) to 47% (7/15, p = 0.008).
After the introduction of the USC service, residents reported no change in their overall satisfaction with SUBS, the number of days per week spent in the operating room or improvement of technical skills.
Qualitative analysis
The proportion of residents who made positive comments related to the effect of on-call and ward duties on their ability to read, attend scheduled teaching activities and the operating room increased from 28% (3/11) to 63% (5/8) after introduction of the USC service. The proportion of residents who made positive comments about the effect of on-call and ward duties on their work environment increased from 17% (1/6) to 100% (5/5). A similar proportion of residents in both cohorts commented that they would like more time to attend ambulatory clinics (60% [3/5] before USC v. 75% [3/4] after USC). Two residents commented that patient volume on their SUBS was too low after the introduction of the USC service (Table 1, Table 2).
Table 1.
Sample comments from the survey and WEB eVAL of residents on the subspecialty-based surgical service before the introduction of the urgent surgical care service
| Category of residents’ comments; effect of on-call and ward duties on: | Negative comments | Positive comments |
|---|---|---|
| Ability to attend scheduled teaching activities and the operating room | “I was never able to attend teaching activities because of ward commitments.” “… pulled out of other teaching/half day repeatedly” “I rarely got to go to the OR, and I never had a full day in the OR.” |
“A lot of OR time.” |
| Work environment | “On-call schedules … place a huge burden on the residents.” “Workload prevents learning at this level.” |
“A well-rounded rotation.” |
| Ability to attend ambulatory clinics | “Clinic was never an option.” | “Organizing clinic time could be a good learning opportunity.” |
OR = operating room.
Table 2.
Sample comments from the survey and WEB eVAL of residents on the subspecialty-based surgical service after the introduction of the urgent surgical care service
| Category of residents’ comments; effect of on-call and ward duties on: | Negative comments | Positive comments |
|---|---|---|
| Ability to attend scheduled teaching activities and the operating room | “Service needs more operating time” | “New urgent surgical team allowed elective teams more time for teaching and study; this was a very positive change.” “Given that the team is no longer on intake, the list is very reasonable thus allowing for time in the OR.” “Adequate reading time” |
| Work environment | “Good balance between service and education” “Can’t overstate how much richer a learning environment this has become without the average 36 hours of call every few days” |
|
| Ability to attend ambulatory clinics | “My one regret was not attending clinic during this rotation.” | “I would like to attend outpatient clinics as I feel these are a valuable learning experience.” |
OR = operating room.
Discussion
This study examined the effect of the realignment of general surgery services on the educational experiences of surgical residents. To the best of our knowledge, this is the only study to examine the effect of the creation of urgent surgical services on residents’ education, despite the fact that many North American institutions have been developing and adopting these types of models. The results of this study add to the body of literature that describes how program structure relates to educational experiences and can guide teaching institutions in the development and improvement of urgent and acute surgical services.
We feel that our data are representative of the general surgery resident body because the response rates for both the survey and WEB eVAL were good, included residents from all postgraduate year levels and represented a large portion of the total number of residents in the general surgery program. We observed significant positive changes in our primary and secondary outcomes. We demonstrated through our qualitative analysis that the decrease in residents’ on-call duties was associated with an increase in their sense of balance between ward duties, operating room attendance and educational opportunities. Residents’ comments such as “the beauty of the new team structure is that without the general surgery call, one has time to stay for all the after-hours HPB [hepatobiliary] cases, thereby optimizing the educational experience of this subspecialty team” emphasize that the implementation of the USC model achieved the predetermined goal of enhancing residents’ learning experiences on SUBS by freeing them of on-call duties. Residents on SUBS chose to attend after-hour operations for their team’s patients, thus increasing their operative exposure and increasing continuity of patient care. By staying for after-hour cases, residents on SUBS may also have improved the experience of residents and the care of patients on the USC service, because the USC residents could focus exclusively on emergency general surgery patients.
Other studies from American centres that have examined the effect of night-float models have found similar results in that shifting on-call duties to dedicated night-time teams results in decreased fatigue, increased independent reading and increased satisfaction among surgical residents.1,2 The results of this study support Gamelli’s hypothesis that the creation of acute surgery models ensures that elective surgical services are not overwhelmed by consults to which they cannot respond promptly and that acute surgical models greatly enhance academic departments.7
A potential criticism of the USC model10 is that residents on SUBS might experience decreased operating room time and decreased exposure to emergency general surgery because they are not performing on-call duties. This did not prove to be the case in this study; residents reported no change in the amount of time spent in the operating room. One study that evaluated a night-float system found that residents on the night teams had decreased operating room time because they were only on service at night.2 In the USC model examined in this study, residents’ on the USC service staffed both daytime and nighttime teams and, thus, should have equal access to the operating room as their colleagues on SUBS. Additionally, because all residents on SUBS services eventually rotate through the USC service, they have concentrated and dedicated exposure to emergency general surgery rather than having decreased exposure to emergency general surgery, which is the ideal situation as highlighted by Gamelli.7
Although we did not specifically examine the experiences of residents on the USC service, we collected some preliminary data in January 2008 after the USC service had been in place for 6 months. On the USC service, each resident covered a mean of 5.76 on-call days per month. Residents on the USC service had a lower attendance at academic half days compared with residents on SUBS (57% v. 87%). This preliminary data may suggest that residents on the USC service are overburdened by on-call duties and are not able to attend scheduled teaching rounds. However, 50% (3/6) of the residents on the USC service agreed that they had sufficient time for independent study and 67% (4/6) agreed that they had sufficient time to attend multidisciplinary conferences or rounds. We received positive comments from residents on the USC service, such as “great potential for enhancing resident experience at VGH in terms of teaching, operative experience, concentrated exposure to acute general surgery,” as well as critical ones, such as “the challenge appeared to be to balance a heavy work load.” These comments suggest that new challenges have arisen, such as communication, balancing work load with the number of residents per team, availability of operating room time and the development of good working relationships with allied health professionals such as nurse practitioners.
Our qualitative analysis demonstrated that residents’ reported a less hectic patient-related workload and an improved work environment but a continued desire to attend more ambulatory clinics. A minority of residents commented that patient volume was too low. When the USC service was initiated, the structure of SUBS was not formally changed other than to decrease the number of on-call days for residents on SUBS. This study has highlighted that the implementation of USC services decreases work load for residents on elective surgical services, thus creating a unique opportunity to enhance the educational activities of residents on the elective services, as suggested by previous authors.7 Residents in this study suggested that the issue of decreased patient volume could be addressed by having fewer junior residents on certain SUBS, formalizing attendance at ambulatory clinics, and taking one more call shift per month.
Our analysis demonstrated that most residents had improved educational experiences on SUBS after the introduction of the USC service. Additionally, there was no statistically significant change in the amount of time residents spent in the operating room or in residents’ overall satisfaction with SUBS. These results demonstrate that the USC model enhances residents’ learning and educational experiences.
Conclusion
Program and service structure relates to the quality of general surgery residents’ education. The introduction of a USC service made favourable quantitative and qualitative differences in residents’ education on subspecialty services. However, residency training programs and institutions must plan carefully when implementing USC services. They must anticipate workload and administrative challenges that naturally arise out of the creation of USC services so that any potential adverse educational impacts on the residents on SUBS or USC services can be addressed through thoughtful allocation of residents and the creation of well-defined learning objectives and academic curricula. To fully evaluate the effect of an USC model on all general surgery residents, a similar study focusing on the educational experiences of residents on USC service should be undertaken.
Footnotes
The results of this study were presented at the British Columbia Surgical Society Annual Spring Meeting at Delta Sun Peaks Resort, Sun Peaks, BC, Mar. 20–22, 2008, and at the 31st Annual Residents’ Research Day for the Division of General Surgery, University of British Columbia, in Vancouver, BC, Apr. 24, 2008.
Competing interests: None declared.
Contributors: Drs. Wood, Hameed and Buczkowski designed the study. Drs. Wood and Hameed acquired and analyzed data and wrote and reviewed the article. Drs. Buczkowski, Sidhu and Panton also analyzed the data. All authors reviewed the article and approved its publication.
References
- 1.Goldstein MJ, Kim E, Widmann WD, et al. A 360 degrees evaluation of a night-float system for general surgery: a response to mandated work-hours reduction. Curr Surg. 2004;61:445–51. doi: 10.1016/j.cursur.2004.03.013. [DOI] [PubMed] [Google Scholar]
- 2.Schneider JR, Coyle JJ, Ryan ER, et al. Implementation and evaluation of a new surgical residency model. J Am Coll Surg. 2007;205:393–404. doi: 10.1016/j.jamcollsurg.2007.05.013. [DOI] [PubMed] [Google Scholar]
- 3.Chung RS, Ahmed N. How surgical residents spend their training time: the effect of a goal-oriented work style on efficiency and work satisfaction. Arch Surg. 2007;142:249–52. doi: 10.1001/archsurg.142.3.249. [DOI] [PubMed] [Google Scholar]
- 4.Earley AS, Pryor JP, Kim PK, et al. An acute care surgery model improves outcomes in patients with appendicitis. Ann Surg. 2006;244:498–504. doi: 10.1097/01.sla.0000237756.86181.50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kim PK, Dabrowski GP, Reilly PM, et al. Redefining the future of trauma surgery as a comprehensive trauma and emergency general surgery service. J Am Coll Surg. 2004;199:96–101. doi: 10.1016/j.jamcollsurg.2004.02.025. [DOI] [PubMed] [Google Scholar]
- 6.Austin MT, Diaz JJ, Jr, Feurer ID, et al. Creating an emergency general surgery service enhances the productivity of trauma surgeons, general surgeons and the hospital. J Trauma. 2005;58:906–10. doi: 10.1097/01.ta.0000162139.36447.fa. [DOI] [PubMed] [Google Scholar]
- 7.Gamelli RL. Organization of faculty practice and resident training in acute care surgery in an academic medical center. Surgery. 2007;141:302–3. doi: 10.1016/j.surg.2007.01.005. [DOI] [PubMed] [Google Scholar]
- 8.Diaz JJ, Jr, Miller RS, May AK, et al. Acute care surgery: a functioning program and fellowship training. Surgery. 2007;141:310–6. doi: 10.1016/j.surg.2007.01.010. [DOI] [PubMed] [Google Scholar]
- 9.Kaplan LJ, Frankel H, Davis KA, et al. Pitfalls of implementing acute care surgery. J Trauma. 2007;62:1264–70. doi: 10.1097/TA.0b013e318053dfd8. [DOI] [PubMed] [Google Scholar]
- 10.Valentine RJ. Acute care surgery: the surgery program director’s perspective. Surgery. 2007;141:307–9. doi: 10.1016/j.surg.2006.09.014. [DOI] [PubMed] [Google Scholar]