Abstract
Background
In the Rationing of Nursing Care in Switzerland Study, implicit rationing of care was the only factor consistently significantly associated with all six studied patient outcomes. These results highlight the importance of rationing as a new system factor regarding patient safety and quality of care. Since at least some rationing of care appears inevitable, it is important to identify the thresholds of its influences in order to minimize its negative effects on patient outcomes.
Objectives
To describe the levels of implicit rationing of nursing care in a sample of Swiss acute care hospitals and to identify clinically meaningful thresholds of rationing.
Design
Descriptive cross-sectional multi-center study.
Settings
Five Swiss–German and three Swiss–French acute care hospitals.
Participants
1338 nurses and 779 patients.
Methods
Implicit rationing of nursing care was measured using the newly developed Basel Extent of Rationing of Nursing Care (BERNCA) instrument. Other variables were measured using survey items from the International Hospital Outcomes Study battery. Data were summarized using appropriate descriptive measures, and logistic regression models were used to define a clinically meaningful rationing threshold level.
Results
For the studied patient outcomes, identified rationing threshold levels varied from 0.5 (i.e., between 0 (‘never’) and 1 (‘rarely’) to 2 (‘sometimes’)). Three of the identified patient outcomes (nosocomial infections, pressure ulcers, and patient satisfaction) were particularly sensitive to rationing, showing negative consequences anywhere it was consistently reported (i.e., average BERNCA scores of 0.5 or above). In other cases, increases in negative outcomes were first observed from the level of 1 (average ratings of rarely).
Conclusions
Rationing scores generated using the BERNCA instrument provide a clinically meaningful method for tracking the correlates of low resources or difficulties in resource allocation on patient outcomes. Thresholds identified here provide parameters for administrators to respond to whenever rationing reports exceed the determined level of ‘0.5’ or ‘1’. Since even very low levels of rationing had negative consequences on three of the six studied outcomes, it is advisable to treat consistent evidence of any rationing as a significant threat to patient safety and quality of care.
Keywords: Health care rationing, Nursing, Quality of heath care, Safety
What is already known about the topic?
Recent international evidence indicates a significant relationship between low nurse staffing and skill mix levels, negative characteristics of the nurse work environment and deteriorated patient and nurse outcomes.
Recent Swiss data suggests a connection between rationing of nursing care and adverse events in inpatients, as well as lower patient satisfaction with nursing care.
What this paper adds
A preliminary set of clinically meaningful thresholds for assessing rationing were identified. These can be used by nursing administrators to identify when action may be needed to protect patients from rationing-related adverse events.
The defined rationing threshold levels indicate that not all patient outcomes may be equally affected by implicit rationing of nursing care.
The findings indicate that it is advisable to avoid rationing to the greatest extent possible. Limiting the mean rationing levels on nursing units and across facilities respectively to ‘0.5’ and ‘1’ would minimize the negative consequences of rationing regarding patient outcomes.
1. Background
Implicit rationing of nursing care is the withholding of or failure to carry out all needed nursing interventions in the face of inadequate time, staffing or skill mix (Schubert et al., 2007). Cost-cutting managerial strategies have increased average acuity of hospital in-patients, along with the intensity of nursing services and reductions of nurse staffing and skill mixes (Aiken et al., 2001a,b; McCloskey and Diers, 2005; Norrish and Rundall, 2001). Combined with the growing nurse shortage (Buerhaus et al., 2007; Kingma, 2007; Simoens et al., 2005), such cutbacks are making rationing an increasingly prominent feature in health care. Although a number of authors have observed that prioritization and rationing are very common responses to limited nursing staff and related resources (Aiken et al., 2001a,b; Kalisch, 2006; Kuenzi and Schaer-Moser, 2002; West et al., 2005), to our knowledge, the relationship between rationing and patient outcomes was explicitly investigated for the first time in the Rationing of Nursing Care in Switzerland Study (RICH Nursing Study) (Schubert et al., 2008), which is an extension of the International Hospital Outcomes Study (IHOS) (Aiken et al., 2001a,b, 2002a,b).
In order to measure implicit rationing of nursing care, a conceptual model and the Basel Extent of Rationing of Nursing Care (BERNCA) instrument were developed (Schubert et al., 2007). This model drew upon theoretical and empirical work connecting staffing and work environments to care processes and patient outcomes, and includes factors empirically shown to influence decision-making and clinical judgment, prioritization of nursing care and patient and nurse outcomes. Implicit rationing of nursing care occurs when nurses providing care perceive that resources are insufficient to provide all of what they consider necessary services to all of the patients to whom they are assigned. The extent of rationing can be thought of in terms of the number of necessary nursing tasks omitted over a given period (Schubert et al., 2007).
Rationing is affected both by organizational factors and by individual nurses’ clinical decision-making and judgment. It is influenced by the available nursing resources (e.g., the adequacy of staffing and skill mix) to meet the patients’ care needs, as well as by characteristics of the involved nurses (e.g., experience, education) and patients (e.g., type and severity of illness, co-morbidities, acuity of patient conditions). Hospital characteristics (e.g., mission and budget), the nurse work environment, and the philosophy of care (e.g., priority setting, culture values, nursing care standards) influence the processes of nursing care, and, by extension, the rationing of that care (Schubert et al., 2007).
In the RICH Nursing study, although the overall observed levels of implicit rationing were low, rationing was the only factor significantly associated with all of the six patient outcomes examined. Both before and after controlling for major organizational variables, higher rationing levels were significantly linked to higher frequencies of nurse-reported medication errors, patient falls, nosocomial infections, critical incidents and pressure ulcers, and lower levels of patient satisfaction with nursing care (Schubert et al., 2008). Of the major organizational variables evaluated as potential correlates of the patient outcomes studied, only the nursing work environment Adequacy of Resources dimension, measured with the Nursing Work Index-revised (NWI-R) (Aiken and Patrician, 2000; Lake, 2002) was a significant correlate of all of the six patient outcomes investigated except nosocomial infections. However, after controlling for rationing and patient-to-nurse ratio, none of these associations persisted. This could be because rationing, which takes place at the patient-nurse interface, is a strong marker of the impacts of resource adequacy and nurse practice environment quality on front-line care, and ultimately, on patient outcomes. However, few studies have measured conditions close to the actual delivery of care, as we have done to assess rationing. Therefore, the inconsistence which have arisen in the past two decades of research on the relationship between nurse staffing levels and rates of negative nurse-sensitive outcomes (Clarke and Donaldson, 2008a,b), might have resulted from the lack of closer measures of omitted care.
Rationing appears to be a new and potentially powerful indicator of care quality – one that reflects both organizational constraints and supports for nursing care in inpatient settings, and that appears, even at low levels, to have a pronounced effect on outcomes. Given the impossibility of avoiding rationing entirely, it is important to identify the exact levels at which it begins to affect patient outcomes. Knowing these thresholds would allow nursing administrators to monitor rationing levels and to react accordingly when they approached or exceeded predetermined tolerances.
The aims of this study were therefore (1) to describe the levels of implicit rationing of nursing care in a sample of Swiss acute care hospitals and (2) to identify clinically meaningful thresholds for scores on a rationing measurement tool by comparing the likelihoods of nurse-reported negative patient outcomes across rationing levels.
2. Methods
2.1. Design, setting and sample
Cross-sectional multi-hospital design data of the RICH Nursing study were used, incorporating data of 1338 working nurses and 779 hospitalized patients in a convenience sample of eight Swiss acute care hospitals (Schubert et al., 2008). The hospitals selected were located in the German (5) and French (3) speaking regions of Switzerland, had more than 100 beds each and had directors who provided written consents for their facilities to be included in the study. Nurses in these facilities working on medical, surgical or gynecological units were approached if they held Swiss nursing or equivalent foreign credentials, and had been working in direct patient care for a minimum of 3 months in the current hospital, including at least 1 month on their current unit. Student nurses, nursing assistants, and nurses assigned on a temporary basis to specific units (i.e., pool or float nurses) were specifically excluded. Patients approached had been hospitalized for at least 2 days on one of the selected units, understood and read either German or French and were deemed physically and mentally able to safely participate.
Approvals were obtained from seven local ethics committees responsible for the eight participating eight hospitals. Nurses and patients were surveyed voluntarily and anonymously. In each hospital, on a defined day, questionnaires were distributed to all eligible nurses and patients. Informed consent was implied by returning the completed questionnaires. Completed questionnaires were collected in closed boxes on each ward.
2.2. Variables and measurements
2.2.1. Nurse survey measures
Implicit rationing of nursing care was measured with the BERNCA instrument. On a 4-point Likert-type scale ranging from “never” to “often,” nurses reported how often in the past 7 working days they had been unable to carry out one or more of the 20 tasks listed. Initial validity and reliability of the BERNCA was established using survey data from German speaking Swiss hospital nurses (Schubert et al., 2007). Content validity was established via review by German nursing experts, who confirmed that the BERNCA items adequately represented the domain of implicit rationing of nursing care. Subscale structures were confirmed with explanatory factor analysis, which showed strong relationships between all individual items and one overall factor – that of rationing of nursing care. Construct validity was supported by significant correlations with nurse work environment variables, and independent of the related construct of patient-to-nurse ratio (used as a proxy for workload in the absence of other available standardized workload measures). As expected, the staffing and resource dimension of the nurse work environment correlated more strongly with rationing than with either of the other two dimensions of nursing leadership and professional development and interdisciplinary collaboration and competence. Internal consistency and homogeneity were confirmed by moderate to high inter-item correlations and a Cronbach’s alpha of 0.93. To calculate the average levels of implicit rationing of nursing care, individual nurses’ rationing scores were averaged over all 20 items (the range of total scores was 0–60, the range of mean item scores [reported in the analyses here] was 0–3.0) (Schubert et al., 2007).
The frequency of five adverse events and complications in inpatients, including the number of nurse reported (1) medication administration errors – medications administered at the wrong time, in the wrong dose and/or to the wrong patient, with or without consequences, over the past year; (2) patient falls, with and without injury, over the past year; (3) nosocomial infections contracted by patients over the past year (e.g., infections of the urinary tract, respiratory system, or wounds); (4) critical incidents which occurred in patients over the past year, e.g., acute post-operative bleeding, cardiac arrest or circulatory collapse (shock), and (5) pressure ulcers (stages 2–4) occurring in patients over the past year were assessed using questions based on items originally developed for the IHOS study (Aiken et al., 2001a,b, 2002a,b; Schubert et al., 2008). On a 4-point Likert-type scale ranging from “never” to “often,” nurses indicated the frequency of these adverse events in their patients over the past year.
Nurse demographics reflects age, sex, experience (years as a nurse, in the current hospital, and on the current unit), education, nationality, and employment status (part-time vs. full time), which were used as control variables in the analyses (Aiken et al., 2002a,b).
2.2.2. Patient survey measures
Overall patient satisfaction with the care they received during their stay was assessed with one question using a 5-point Likert type scale (from very satisfied to very dissatisfied) (“Overall, how satisfied are you with the care you have received in this hospital?”). Data on patient Age, Sex and Health status were collected with additional questions on the patient satisfaction questionnaire (Schubert et al., 2008).
2.2.3. Hospital characteristics
Hospital characteristics such as size (number of beds), mission (university, cantonal, regional), and ownership (private, public) were obtained from hospital administrators and data provided by the Swiss Federal Office of Statistics for 2002 (http://www.bfs.admin.ch/bfs/portal/de/index/themen/14/04/01/data/01.html).
2.3. Data analysis
Variables were analyzed using descriptive statistical methods appropriate to the levels of measurement. Logistic regression models using robust (Huber–White) standard errors adjusted for clustering of observations by unit were fit, with implicit rationing of nursing care (BERNCA) scores as the independent variables and patient outcomes (frequency of nurse reported adverse events and complications in inpatients and patient satisfaction) as the dependent variables.
To define the thresholds at which rationing began to affect these outcomes negatively, BERNCA scores were recoded into 6 levels: 0, 0.5, 1.0, 1.5, 2.0, ≥2.5. Because of the skewed distribution of the adverse event measures (individual nurses’ responses regarding the frequencies of adverse events among their patients over the preceding year), two separate dichotomizations approaches were used to gain a fuller understanding of the underlying patterns. In the first reports of ‘rarely’, ‘sometimes’ and ‘often’ were contrasted against those of various events ‘never’ occurring in the second reports of ‘sometimes’ and ‘often’ were contrasted with those of ‘never’ and ‘rarely’. With the exception of the analyses involving patient satisfaction, all analyses were performed at the level of individual nurses (i.e. nurse-level measures of rationing were used as predictors of nurse-level reports of adverse events). Since the study’s design made it impossible to link individual nurse rationing data to individual patient satisfaction scores, unit level rationing measurements were used to define odds of individual patients expressing high satisfaction with their care. The level of significance was set at p < 0.05. Analyses were performed using SPSS 14 (SPSS for Windows, Version 14, 2005. Chicago: SPSS Inc.) and Stata 8 (StataCorp LP, College Station, TX).
3. Results
The characteristics of the hospitals, nurses and patients studied are presented in Table 1.
Table 1.
Summary of hospital, nurse and patients characteristics variable.
| Hospital characteristics | ||
| N | 8 | |
| Typology | University | 3 |
| Cantonal | 2 | |
| Regional | 3 | |
| Legal form | Public | 7 |
| Private/public | 1 | |
| Size | <300 beds | 2 |
| 300–600 beds | 3 | |
| >600 beds | 3 | |
| Included units | Surgical | 60 |
| Medical | 51 | |
| Gynaecological | 7 | |
| Nurse characteristics | ||
| N | 1338 | |
| Age (%) | 20–30 years | 42 |
| 31–40 | 31 | |
| 41–50 | 19 | |
| >50 | 8 | |
| Sex (%) | Female | 90 |
| Foreigners (%) | 31 | |
| Employment (%) | Full time: 100% | 39 |
| 80/90% | 33 | |
| Part-time: ≤70% | 28 | |
| Education (%) | Specialized | 31 |
| Graduate/postgraduate | 1 | |
| Years working | As a nurse | 10.3 (8.9) |
| – mean (S.D.) | In this hospital | 7.4 (7.4) |
| On this unit | 5.3 (6.0) | |
| Patient characteristics | ||
| N | 779 | |
| Age (%) | 14–20 years | 2 |
| 21–40 | 14 | |
| 41–60 | 30 | |
| 61–70 | 21 | |
| >71 | 33 | |
| Sex (%) | Female | 55 |
S.D.: standard deviation.
The frequency of nurse-reported adverse events over the past year and patient-reported satisfaction with care are shown in Table 2.
Table 2.
Frequency of nurse-reported adverse outcomes (N = 1338).
| Event type | Ever (rarely, sometimes, often) against never | Regularly (sometimes, often) against rarely, never |
|---|---|---|
| Medication errors (%) | 85 | 30 |
| Falls (%) | 89 | 44 |
| Nosocomial infection (%) | 93 | 58 |
| Critical incidents (%) | 67 | 16 |
| Pressure ulcers (%) | 82 | 24 |
3.1. Measured levels of implicit rationing of nursing care
Ninety-six percent of the 1338 nurses reported that they were unable to perform at least one of the listed nursing tasks at some point in the preceding week and therefore had resorted to rationing their care (rarely (1) sometimes (2) often (3)) in the last 7 working days. The mean nurse-level score suggested that, on average, tasks were omitted slightly less frequently than “rarely” (mean 0.82, SD 0.53, median 0.77, range 0–2.68). The six recoded cut-off points for individual nurse-level rationing scores (see Section 2.3) are shown in Table 3.
Table 3.
Allocation of the six recoded rationing levels (BERNCA scores).
| Rationing level | ||
|---|---|---|
| 0.00= | Never – n (%) | 51 (4) |
| 0.50= | Very rarely – n (%) | 354 (29) |
| 1.00= | Rarely –n (%) | 381 (31) |
| 1.50= | Rarely/sometimes – n (%) | 291 (24) |
| 2.00= | Sometimes – n (%) | 120 (10) |
| ≥2.50= | More common than sometimes – n (%) (including rationing levels 2.50–3.00) | 23 (2) |
3.2. Threshold of implicit rationing of nursing care
Even very low levels of nurse-reported rationing (i.e., any score above 0) were associated with significantly elevated risks for five of the six reported negative events. Regression modelling suggested that the levels of rationing above which reports of negative events were distinctly elevated (i.e., the rationing thresholds) varied from ‘0.5’ to ‘2’ across the patient outcomes studied (Table 4).
Table 4.
Rationing threshold levels for selected patient outcomes using different dichotomization.
| Patient outcomes | Rationing:Lowest level |
Highest level |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| 0 | 0.5 |
1 |
1.5 |
2 |
2.5 |
||||||
| Odds (CI) | p-Value | Odds (CI) | p-Value | Odds (CI) | p-Value | Odds (CI) | p-Value | Odds (CI) | p-Value | ||
| Dichotomization ever (rarely, sometimes, often) versus never | |||||||||||
| Medication errorsa | Reference category | 1.81 (0.93, 3.52) | 0.08 | 4.62 (2.29, 9.33) | <0.001 | 4.60 (1.99, 10.66) | <0.001 | 6.30 (2.98, 13.30) | <0.001 | 11.33 (1.44, 89.38) | 0.02 |
| Fallsa | 0.80 (0.40, 1.60) | 0.52 | 2.04 (0.91, 4.57) | 0.08 | 1.96 (0.83, 4.67) | 0.13 | 5.35 (1.98, 14.43) | 0.001 | 3.91 (0.48, 31.53) | 0.20 | |
| Nosocom infectionsa | 2.32 (0.96, 5.61) | 0.06 | 6.19 (2.38, 16.10) | <0.001 | 4.44 (1.55, 12,75) | 0.006 | 4.91 (1.37, 17.58) | 0.014 | 5.79 (0.67, 50.23) | 0.11 | |
| Critical incidentsa | 1.55 (0.90, 2.69) | 0.12 | 2.50 (1.47, 4.26) | 0.001 | 4.46 (2.46, 8,10) | <0.001 | 8.79 (4.02, 19.20) | <0.001 | 8.79 (2.12, 36.47) | 0.003 | |
| Pressure ulcersa | 3.80 (1.93, 7.47) | <0.001 | 5.52 (2.87, 10.61) | <0.001 | 7.35 (3.60, 15.01) | <0.001 | 10.64 (4.53, 24.96) | <0.001 | 23.83 (2.84, 200.11) | 0.003 | |
| Dichotomization regularly (sometimes, often) versus rarely, never | |||||||||||
| Medication errorsa | Reference category | 1.55 (0.73, 3.33) | 0.26 | 1.92 (0.69, 4.13) | 0.10 | 2.24 (1.02, 4.93) | 0.05 | 2.22 (0.99, 4.98) | 0.05 | 4.56 (1.52, 13.68) | 0.01 |
| Fallsa | 0.66 (0.38, 1.15) | 0.14 | 0.73 (0.43, 1.24) | 0.24 | 0.83 (0.47, 1.45) | 0.51 | 1.25 (0.64, 2.45) | 0.51 | 2.00 (0.62, 6.47) | 0.25 | |
| Nosocom infectionsa | 1.06 (0.58, 1.95) | 0.84 | 2.12 (1.08, 4.14) | 0.03 | 2.36 (1.22, 4.94) | 0.02 | 3.05 (1.56, 6.00) | 0.001 | 2.41 (0.90, 6.45) | 0.08 | |
| Critical incidentsa | 1.04 (0.28, 3.81) | 0.95 | 2.6 (0.81, 8.33) | 0.11 | 5.51 (1.55, 19.55) | 0.008 | 7.29 (2.34, 22.70) | 0.001 | 5.65 (1.33, 28.14) | 0.04 | |
| Pressure ulcersa | 1.55 (0.68, 3.56) | 0.30 | 2.98 (1.33, 6.68) | 0.008 | 3.83 (1.62, 9.06) | 0.002 | 6.30 (2.52, 15.73) | <0.001 | 9.82 (2.53, 27.27) | <0.001 | |
| Patient satisfactionb very satisfied | 0.43 (0.21, 0.90) | 0.02 | 0.32 (0.16, 0.68) | 0.03 | |||||||
Notes: 95% CI – 95% confidence interval.
Nurse-reported outcome, predicted using nurse-level rationing scores.
Patient-reported outcome, predicted using unit-level aggregate rationing scores.
Using the first dichotomization approach for the nurse reported negative events regarding patient care (“rarely”, “sometimes”, “often” versus “never”); a rationing level of ‘0.5’ was significantly associated with more-than-doubled to nearly fourfold increases in the odds of nurses reporting nosocomial infections and pressure ulcers for the previous year. A rationing level of ‘1’ was significantly linked with an increase factor of from 2.50 to nearly 5 in the odds of nurses ever reporting critical incidents or medication errors. Levels of rationing above 1 were associated with heightened likelihood of nurse reported patient falls, while levels of ‘2’ and higher were associated with a large jump in the odds of patient falls (Table 4, Fig. 1).
Fig. 1.
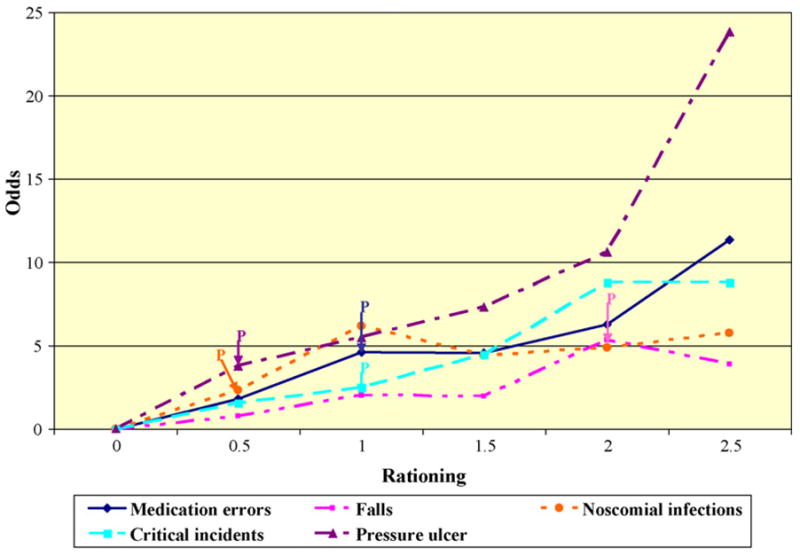
Rationing threshold levels for selected patient outcomes, as reported over the past year. Note: ‘p’ represents the rationing level at which the accepted level of significance <0.5 was reached and rationing began to affect the particular outcome negatively. Dichotomization of patient outcomes: ever (rarely, sometimes, often) versus never).
Repeating the modelling using the second dichotomization approach contrasting regularly (“sometimes or often”) versus “rarely or never” revealed the expected pattern. Fewer nurses reported that the negative events were as common, and a rationing level of ‘0.5’ was no longer significantly linked with any of the reported adverse events. In most cases, the thresholds associated with elevated risk of frequent adverse events were approximately 0.5 point higher. A rationing level of ‘1’ was now significantly associated with increases in the frequency of nosocomial infections and pressure ulcers, while a level of ‘1.5’ was significantly linked with increases in the frequency of critical incidents and medication errors. Using this dichotomization, no clear threshold could be defined for patient falls (Table 4, Fig. 2).
Fig. 2.
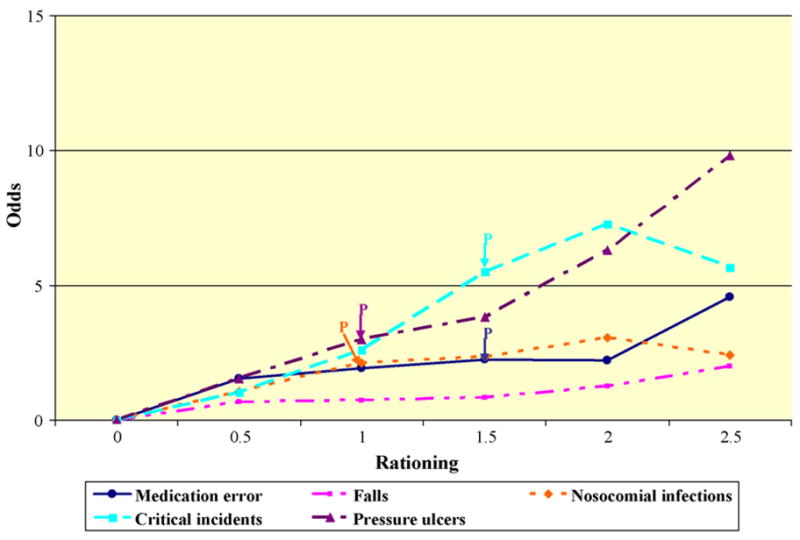
Rationing threshold levels for selected patient outcomes, regularly reported over the past year. Note: ‘p’ represents the rationing level at which the accepted level of significance <0.5 was reached and rationing began to affect the particular outcome negatively. Dichotomization of patient outcomes: regularly (sometimes, often) versus never, rarely)
At the same time, though, patient reported satisfaction with care was impacted significantly even by a rationing level of 0.5 (unit level measures), this accompanied a 57% decrease in the number of patients who reported being very satisfied with their care (Odds Ratio 0.43, 95% CI: 0.21, 0.90, p = 0.02). In summary, these results suggest that limiting rationing levels to either ‘0.5’ or ‘1’ would likely be associated with beneficial effects on patient satisfaction and the frequency of nurse reported negative events.
4. Discussion
This study used data from the RICH Nursing Study to define clinically meaningful thresholds at which implicit rationing of nursing care begins to affect nurse-reported patient outcomes negatively. Only four percent of participating nurses reported never having had to ration any of the 20 nursing measures listed in the tool over their last 7 working days. Although the average rationing levels were not high, as shown in a previous study (Schubert et al., 2008), rationing was significantly correlated with nurse-reported patient outcomes.
The nurse-reported patient outcomes of nosocomial infections, pressure ulcers and patient satisfaction appeared particularly sensitive to rationing, in that they showed significant increases whenever any consistent rationing was reported (average scores of 0.5). The rationing thresholds appear robust to differences in variable definitions and model specifications. Specifically, the two dichotomizations tested for the frequencies of negative outcomes yielded similar rationing thresholds.
Patient falls appeared to be the least sensitive of the outcomes to rationing. While rationing of care may be involved in fall risk, the specific aspects of nursing care and patient characteristics affecting falls (such as risk assessment, surveillance, environmental modifications, ward design and patient dependency) may be somewhat different from those involved in other outcomes (Hurst, 2008; Roberts, 1985). However, the relation between nurse staffing, nursing intervention and patient falls is still under discussion (Lake and Cheung, 2006), as is the adequacy of the current methods for collecting patient fall data (Currie, 2008; White and McGillis Hall, 2003).
In interpreting these results, one must consider that, based on the results of the explorative factor analysis, which yielded only one strong factor, the mean rationing score of the scale was used for the definition of the thresholds, which weight all elements of the BERNCA equally. Further, given the low overall rationing levels, the mean score was recoded into 6, rather than 4 levels for the definition of the thresholds. For future work with the BERNCA, a refinement of the scaling is recommended. Considering the results of the evaluation of the reliability and validity of the BERNCA (described in Schubert et al., 2007), we have begun a refinement of the scale, which will also make allowances for scaling issues, e.g., by adding the answer category “was not necessary”.
This study has several strengths, but a number of weaknesses are also noteworthy. First, the cross-sectional design employed does not permit causal inferences regarding rationing and patient outcomes. Second, the geographic and cultural specificity of the sample (a convenience sample of eight Swiss acute care hospitals), and the hospital inclusion criteria, limit the generalizability of the findings, especially regarding smaller facilities (<100 beds). Officials at 11 of the 19 hospitals originally approached to participate in the RICH Nursing study declined to participate. They provided two general types of explanation for their decisions: limited resources and prior commitments to other projects, and “political” reasons (i.e., they did not wish their institutions to be involved in a study investigating rationing of care). Consequently, the levels of rationing in Swiss hospitals at large could actually be much higher than shown here. Because at the time of this article’s printing there is no complete list of nurses in Switzerland, it is impossible to select a random sample of the entire nurse population. However, the use of non-randomized samples is a common strategy in outcome research, as well as in cross-country studies (Clarke and Donaldson, 2008a,b).
A further weakness is that, with the exception of patient satisfaction, nurse reports of negative events in patient care, rather than outcome data generated by more objective sources, were used as the dependent variables here. Given the data situation in Switzerland, which is characterized by a lack of regular reporting of nurse sensitive patient outcomes (e.g., only two of the included hospitals regularly collected data on pressure ulcers), tightly-restricted research access to databases, and the lack of alternative data sources, this method offered the only possibility to collect similar outcome data in all participating hospitals. Due to the lack of other data sources, other authors have also used nurse-reported data in outcome research (Aiken et al., 1997; Sochalski, 2004). Nevertheless, at least one study building upon of the RICH Nursing study is currently underway to test the validity of nurse reported data against hospital patient outcome records. In one such study, nurse-reported patient fall data for a 1-year period and official fall incident reports for the same period were significantly correlated, for both falls with and without injury (Cina-Tschumi et al., 2008). However, further validation of nurse reports as measures of incidents is needed. Depending on the results obtained, clinician reported incidence of patient falls and other events may be a type of measure worth using more extensively in research in this area, due to the relative ease of implementing it on a large scale at reasonable cost.
Finally, the nurse reports of negative events in patient care and the rationing data refer to different time frames (the preceding year for outcomes versus the last 7 working days for rationing), which may have attenuated the associations observed.
However, these shortcomings are balanced by a number of strengths. First, the response rates for both nurses and patients in the upper range of those seen in voluntary surveys provide precise depictions of implicit rationing of nursing care and its associations with outcomes in the eight hospitals. Furthermore, analyses of data at the unit and individual levels, for patients and nurses, considerably increased the precision of linkages and probably the statistical power of the study as well.
From the results of these analyses, the following implications for clinicians, nurse administrators and researcher can be derived. First, rationing is an important empirical factor, which appears to be linked with patient safety and care quality. The defined rationing threshold levels, together with the BERNCA, can be used by nurse administrators and clinicians to monitor rationing levels regularly, e.g., to integrate the BERNCA into quality assurance processes in institutions and administer the BERNCA to randomly selected groups of nurses on different shifts every 3 months (or more often if practical) and to examine underlying causes and consider increasing staffing whenever rationing exceeds the threshold levels defined here. Over time, refinement of the instrument for use in specific clinical settings and further development of benchmarking statistics will increase the BERNCA’s usefulness for these purposes.
Because of the demonstrated importance of rationing and the lack of knowledge regarding the decision-making processes and allocation criteria nurses use to distribute scarce resources among their patients, along with the factors influencing implicit rationing of nursing (Bucknall, 2000; Hendry and Walker, 2004; Schubert et al., 2007), it is important to develop a deeper understanding of the underlying decisions and processes involved. This knowledge would help to determine which kinds of interventions are necessary when the measured rationing levels exceed the defined thresholds. Due to limitations in nursing resources and restrictions in nurse staffing levels in many hospitals, this would make it possible to develop other appropriate interventions or strategies, which could be used to reduce the rationing levels effectively, next to the adaptation of the nurse staffing and skill mix. Furthermore, this would help to define relevant indicators, which should be monitored additionally to rationing. This will require large representative studies with mixed methods approaches that incorporate prospectively collected longitudinal data on staffing and outcomes sensitive to nursing care. Such data will enable the linking of rationing, patient acuity and complexity levels with precise nurse staffing measures at the unit level, while allowing causal inferences about the identified associations and interrelations.
Future research with the BERNCA should incorporate representative samples of types of hospitals, as well as long-term facilities, where the scarcity of nursing resources is a continuous issue, and should include other nurse sensitive patient outcome data and sources (Van den Heede et al., 2007) to confirm the rationing thresholds defined here. Prospective designs should also be considered. Furthermore, studies with large, representative hospital samples would also help clarify the extent to which nursing processes and rationing may be similar or different across hospital types, and whether the relationship between rationing and outcomes is conditioned or affected by hospital type and ward designs feature. Particularly, the ward design feature seems to be a relevant factor related with workload, quality of care (Hurst, 2008). In this study, the small hospital sample, with closely linked inter-hospital characteristics did not allow us to control for this.
As described, data source issues, including access to data and the reliability of the data acquired, are enduring issues in this area of outcome research (Clarke and Donaldson, 2008a,b). In Switzerland, as in other countries, several hospitals have started to implement critical incident reporting systems on a national scale (CIRS). Although sensitivity of the information in these databases may make access to these data difficult at times and consistency of the data, particularly across hospitals, could prove challenging to verify, such datasets may become another suitable data source for outcomes research.
Given the sensitivity of the topic and not to harm patients, Randomized Control Trials (RCT) or Clinical Control Trials (CCT) on the unit levels with, e.g., deliberate omission of necessary nursing interventions in the intervention group, are unlikely to be practical. But natural experiments, in which system changes implemented in one group of facilities as a matter of policy, e.g., interventions for improving the safety culture and quality of the work environment are evaluated by comparing the facilities affected with control institutions, could help strengthen the evidence base related to rationing. Furthermore, linked with valid patient outcome data, the BERNCA could be used in future studies to evaluate different models of care or staffing approaches and their impacts on both with rationing and care endpoints.
5. Conclusions
With nurses in ever-shorter supply and the increasing acuity of hospital inpatients, the intensity of required nursing services is rising, while nurse staffing, skill mixes, and resources are on the decrease. As a result, rationing is becoming an increasingly prominent feature in health care. The results of this study highlight the relevance of rationing for patient safety and care quality, since all detectable rationing showed negative effects on three of the six studied patient outcomes.
Data here suggests that rationing scores generated using the BERNCA instrument could provide a clinically meaningful method for tracking the effects of low resources, or difficulties in allocating resources, on patient outcomes. The identified thresholds provide parameters for nursing administrators to monitor negative effects of rationing on patient outcomes, and to respond rapidly whenever rationing exceed tolerable levels.
Based on these results, it can be strongly recommended to avoid rationing to the greatest extent possible and to limit the mean rationing levels on nursing units and across facilities respectively to ‘0.5’ and ‘1’ (i.e., very low levels). This would prevent most, if not all, negative consequences of rationing to patient outcomes.
Acknowledgments
The authors thank the nurse leaders, resource nurses, staff nurses and patients in the study hospitals for their participation. The authors also acknowledge Chris Shultis for his work editing the article.
Funding
This study was funded by the Swiss Federal Office of Public Health.
Footnotes
Conflict of interest
No conflicts.
Ethical approval
Approvals were obtained from seven local ethics committees responsible for the participating eight hospitals.
Nurses and patients were surveyed voluntarily and anonymously. Informed consent was implied by returning the completed questionnaires. Additionally two ethics committees asked for a written informed consent from the patients.
References
- Aiken LH, Sloane DM, Klocinski JL. Hospital nurses’ occupational exposure to blood: prospective, retrospective, and institutional reports. Am J Public Health. 1997;87 (1):103–107. doi: 10.2105/ajph.87.1.103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM. Hospital restructuring: does it adversely affect care and outcomes? J Health Human Serv Admin. 2001a;23 (4):416–442. [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski JA, Busse R, Clarke H, Giovannetti P, Hunt J, Rafferty AM, Shamian J. Nurses’ reports on hospital care in five countries. Health Aff (Millwood) 2001b;20 (3):43–53. doi: 10.1377/hlthaff.20.3.43. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM. Hospital staffing, organization, and quality of care: cross-national findings. Int J Qual Health Care. 2002a;14 (1):5–13. doi: 10.1093/intqhc/14.1.5. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Clarke SP, Sloane DM, Sochalski J, Silber JH. Hospital nurse staffing and patient mortality, nurse burnout, and job dissatisfaction. JAMA. 2002b;288 (16):1987–1993. doi: 10.1001/jama.288.16.1987. [DOI] [PubMed] [Google Scholar]
- Aiken LH, Patrician PA. Measuring organizational traits of hospitals: the Revised Nursing Work Index. Nurs Res. 2000;49 (3):146–153. doi: 10.1097/00006199-200005000-00006. [DOI] [PubMed] [Google Scholar]
- Bucknall TK. Critical care nurses’ decision-making activities in the natural clinical setting. J Clin Nurs. 2000;9 (1):25–35. [PubMed] [Google Scholar]
- Buerhaus PI, Auerbach DI, Staiger DO. Recent trends in the registered nurse labor market in the U.S.: short-run swings on top of long-term trends. Nurs Econ. 2007;25(2):59–66. 55. quiz 67. [PubMed] [Google Scholar]
- Cina-Tschumi B, Schubert M, Kressig RW, De Geest S, Schwendimann R. Frequencies of falls in Swiss hospitals: Concordance between nurses’ estimates and fall incident reports. Int J Nurs Stud. 2008 doi: 10.1016/j.ijnurstu.2008.09.008. [DOI] [PubMed] [Google Scholar]
- Clarke S, Donaldson N. Nurse staffing and patient care quality and safety. In: Hughes R, editor. Patient Safety and Quality An Evidence-Based Handbook for Nurses. Agency for Healthcare Research and Quality; Rockville, MD: 2008a. pp. 1–25. [PubMed] [Google Scholar]
- Clarke SP, Donaldson NE. Staffing. In: Hughes RG, editor. Patient Safety and Quality Agency for Healthcare Research and Quality. An Evidence-Based Handbook for Nurses. Rockville, MD: 2008b. pp. 1–25. [PubMed] [Google Scholar]
- Currie L. Fall and injurie prevention. In: Hughes RG, editor. Patient Safety and Quality Agency for Healthcare Research and Quality. An Evidence-Based Handbook for Nurses. Rockville, MD: 2008. pp. 1–56. [PubMed] [Google Scholar]
- Hendry C, Walker A. Priority setting in clinical nursing practice: literature review. J Adv Nurs. 2004;47 (4):427–436. doi: 10.1111/j.1365-2648.2004.03120.x. [DOI] [PubMed] [Google Scholar]
- Hurst K. UK ward design: patient dependency, nursing workload, staffing and quality—an observational study. Int J Nurs Stud. 2008;45 (3):370–381. doi: 10.1016/j.ijnurstu.2006.09.007. [DOI] [PubMed] [Google Scholar]
- Kalisch BJ. Missed nursing care: a qualitative study. J Nurs Care Qual. 2006;21(4):306–313. doi: 10.1097/00001786-200610000-00006. quiz 314–305. [DOI] [PubMed] [Google Scholar]
- Kingma M. Nurses on the move: a global overview. Health Serv Res. 2007;42 (3 Pt 2):1281–1298. doi: 10.1111/j.1475-6773.2007.00711.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kuenzi K, Schaer-Moser M. The Labour Situation in Nursing in the Canton of Bern – Die Arbeitssituation im Pflegebereich im Kanton Bern (in German) Büro Bass, Büro & Co; Bern, Switzerland: 2002. pp. 1–81. [Google Scholar]
- Lake ET. Development of the practice environment scale of the Nursing Work Index. Res Nurs Health. 2002;25 (3):176–188. doi: 10.1002/nur.10032. [DOI] [PubMed] [Google Scholar]
- Lake ET, Cheung RB. Are patient falls and pressure ulcers sensitive to nurse staffing? West J Nurs Res. 2006;28 (6):654–677. doi: 10.1177/0193945906290323. [DOI] [PubMed] [Google Scholar]
- McCloskey BA, Diers DK. Effects of New Zealand’s health reengineering on nursing and patient outcomes. Med Care. 2005;43 (11):1140–1146. doi: 10.1097/01.mlr.0000182549.85761.cd. [DOI] [PubMed] [Google Scholar]
- Norrish BR, Rundall TG. Hospital restructuring and the work of registered nurses. Milbank Q. 2001;79(1):55–79. IV. doi: 10.1111/1468-0009.00196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Roberts F. Accidents in hospital. Learning from past mishaps. Nurs Times. 1985;81 (10):24–26. [PubMed] [Google Scholar]
- Schubert M, Glass TR, Clarke SP, Aiken LH, Schaffert-Witvliet B, Sloane DM, De Geest S. Rationing of nursing care and its relationship to patient outcomes: the Swiss extension of the International Hospital Outcomes Study. Int J Qual Health Care. 2008:1–11. doi: 10.1093/intqhc/mzn017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schubert M, Glass TR, Clarke SP, Schaffert-Witvliet B, De Geest S. Validation of the Basel Extent of Rationing of Nursing Care instrument. Nurs Res. 2007;56 (6):416–424. doi: 10.1097/01.NNR.0000299853.52429.62. [DOI] [PubMed] [Google Scholar]
- Simoens S, Villeneuve M, Hurst J. OECD Health Working Papers. OECD; Paris: 2005. Tackling Nurse Shortages in OECD Countries; pp. 1–58. [Google Scholar]
- Sochalski J. Is more better?: the relationship between nurse staffing and the quality of nursing care in hospitals. Med Care. 2004;42(2 Suppl):II67–II73. doi: 10.1097/01.mlr.0000109127.76128.aa. [DOI] [PubMed] [Google Scholar]
- Van den Heede K, Clarke SP, Sermeus W, Vleugels A, Aiken LH. International experts’ perspectives on the state of the nurse staffing and patient outcomes literature. J Nurs Scholarsh. 2007;39 (4):290–297. doi: 10.1111/j.1547-5069.2007.00183.x. [DOI] [PubMed] [Google Scholar]
- West E, Barron DN, Reeves R. Overcoming the barriers to patient-centred care: time, tools and training. J Clin Nurs. 2005;14 (4):435–443. doi: 10.1111/j.1365-2702.2004.01091.x. [DOI] [PubMed] [Google Scholar]
- White P, McGillis Hall L. Patient safety outcomes. In: Doran D, editor. Nurse-Sensitive Outcomes: State of the Science. Jones and Bartlett Puplishers; Sudbury, MA: 2003. pp. 211–242. [Google Scholar]


