Abstract
Background
Assessing function is a crucial element in the diagnosis of dementia. This information is usually obtained from key informants. However, reliable informants are not always available.
Methods
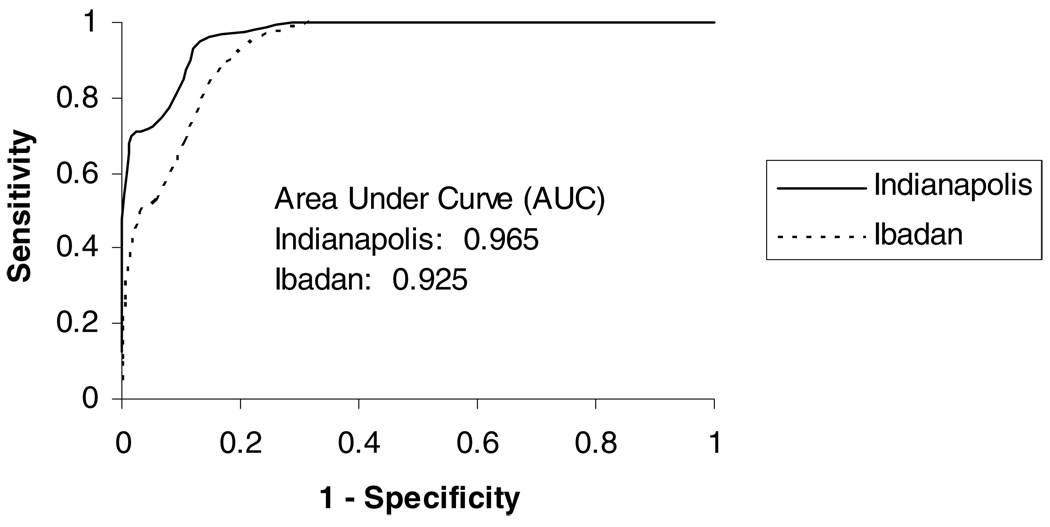
A 10-item semi-structured home interview (the CHIF, or Clinician Home-based Interview to assess Function) to assess function primarily by measuring instrumental activities of daily living directly was developed and tested for inter-rater reliability and validity as part of the Indianapolis–Ibadan dementia project. The primary validity measurements were correlations between scores on the CHIF and independently gathered scores on the Blessed Dementia Scale (from informants) and the Mini-mental State Examination (MMSE). Sensitivities and specificities of scores on the CHIF and receiver operator characteristic (ROC) curves were constructed with dementia as the dependent variable.
Results
Inter-rater reliability for the CHIF was high (Pearson’s correlation coefficient 0.99 in Indianapolis and 0.87 in Ibadan). Internal consistency, in both samples, was good (Cronbach’s α 0.95 in Indianapolis and 0.83 in Ibadan). Scores on the CHIF correlated well with the Blessed Dementia scores at both sites (−0.71, p < 0.0001 for Indianapolis and −0.56, p < 0.0001 for Ibadan) and with the MMSE (0.75, p < 0.0001 for Indianapolis and 0.44, p < 0.0001 for Ibadan). For all items at both sites, the subjects without dementia performed significantly better than those with dementia. The area under the ROC curve for dementia diagnosis was 0.965 for Indianapolis and 0.925 for Ibadan.
Conclusion
The CHIF is a useful instrument to assess function directly in elderly participants in international studies, particularly in the absence of reliable informants.
Keywords: dementia, ADL, IADL, African Americans, Yoruba
Introduction
A major criterion for the diagnosis of dementia is to establish cognitive deficits sufficient to cause significant impairment in the patient’s social or occupational functioning (APA, 1987; WHO, 1992). Most guidelines for diagnosing dementia recommend that information regarding the patient’s functioning and the ability to perform tasks of everyday living is best obtained from a reliable informant (Knopman et al., 2003; Morris et al., 1989; Richards and Hendrie, 1999). Unfortunately, reliable informants are not always available in community-based studies where significant proportions of elderly people live alone, at least in Western countries, even when they exhibit signs of dementia. For example, in the population-based Monongahela Valley Independent Elders Survey (MoVIES), approximately one-third of the subjects with dementia were living alone (Prescop et al., 1999) and approximately half of these subjects were unable to identify a caregiver. In our Indianapolis–Ibadan dementia project, approximately 50% of our African American elderly participants were unable or unwilling to identify an informant. This was much less of a problem for our Ibadan sample, where almost all the elderly Yoruba were living with extended families. However, even when informants were identified, questions about reliability of their information were sometimes raised at both sites.
To overcome this problem, we have developed a home-based interview for use by clinicians. The Clinician Home-based Interview to assess Function (CHIF) directly assesses function, defined as instrumental activities of daily living (IADL) in cognitively impaired elderly subjects who do not have reliable informants, and was used at both sites with the elderly African American and Yoruba populations. The interview is relatively brief, designed to be as non-intrusive as possible, but does require that the interviewer has some knowledge of the local environment. This paper describes the content of this interview, its properties, including inter-rater reliability, internal consistency, and factor structure at both sites. Its validity was estimated primarily by correlating the score derived from the CHIF with informant-based functional scores and cognitive test scores. In addition, specificity and sensitivity of the scores on the CHIF were calculated for the clinical diagnoses of dementia.
Method
Since 1992, researchers from Indiana University and the University of Ibadan have been conducting a longitudinal study of the prevalence and incidence of dementia and Alzheimer’s disease (AD) in elderly African Americans living in Indianapolis and Yoruba living in Ibadan, Nigeria. During the course of the study, prevalence and four incidence waves have been completed. The CHIF was designed and tested during the second incidence wave, 5 years following the prevalence study. The construction of study samples and the research design have been described in detail elsewhere (Hendrie et al., 2001). In brief, in Nigeria, the study was carried out on Yoruba, aged 65 years and over, living in the Idikan area in the city of Ibadan. A total population survey was carried out by means of door-to-door census, in a geographically defined area. In Indianapolis, the geographic target area used in the study consisted of 29 contiguous census tracts, in which African Americans represented 80% of the population in the 1990 census. Interviewers went door-to-door to randomly sampled addresses to invite African Americans aged 65 years and over to participate. Both prevalence and incidence waves followed a two-stage design, in which there was first an in-home screening using the Community Screening Instrument for Dementia (CSI-D), followed by a full diagnostic work-up of a subsample of the population selected on the basis of the performance on the screening test. Before the start of each wave of the study, informed consent was obtained from the participants and informants. The institutional review boards at both universities approved the study. Details of the development, content and scoring of the CSI-D have been published previously (Hall et al., 2000; Hendrie et al., 1993).
The clinical assessment was identical at both sites and included a structured interview with an informant, neuropsychological testing, and an examination by a physician. The informant interview was based on the Cambridge Mental Disorders of the Elderly Examination (Roth et al., 1986) and included a historical review of the participants and a review of their performance in everyday activities. The review of performance included the 11 items from the Blessed Dementia Scale (Blessed et al., 1968). The neuropsychological evaluation consisted of the Consortium to Establish a Registry for Alzheimer Disease (CERAD) battery (Morris et al., 1989). The test included the Mini-mental State Examination (MMSE), Animal Fluency Test, Boston Naming Test, Constructional Praxis, and Word List Learning Memory. The battery was translated and harmonized for use in Yoruba and normative values were available for both sites (Gureje et al., 1995; Unverzagt et al., 1996). Diagnoses were made at both sites after a consensus diagnostic conference involving the research clinicians. For diagnosis of dementia both DSM-III and ICD-10 criteria had to be satisfied (APA, 1987; WHO, 1992). NINCDS/ADRDA criteria were used to diagnose AD (McKhann et al., 1984).
Construction of CHIF
The CHIF was based upon the experiences of the senior physicians during the course of the physician home-based examination at both sites, from the prevalence and first incidence phases. The final semi-structured interview and scoring system was designed (by H.C.H.) after consultations between the research physicians and nurses at both sites. The semi-structured format was chosen to allow an experienced clinician the flexibility to rephrase questions and follow up probes to ensure maximum validity. It included areas normally measured in assessments of ADL and IADL, such as shopping and medication. The purpose of the instrument is to evaluate the participant’s higher cognitive function by assessing their knowledge of how to perform IADL, not whether they are physically capable of performing them. It was also designed to take advantage of the fact that the interview was being conducted at home. For example, an assessment of the state of the organization of the house and personal grooming could be made. Some allowances in scoring had to be made for most men’s relative inexperience in items such as cooking or shopping. However, in live-alone situations, men would be required to assume more of these responsibilities. It requires that interviewers have some geographic knowledge; for example, location of shopping centers and churches or mosques. For some items such as personal history, external validation is impossible, but the interviewer is asked to assess the coherence of the account and to note discrepancies in the order of events. Items were also selected that were common to both African Americans and Yoruba and could be assessed at both sites, although the details of each item might be quite different between sites, such as cooking arrangements and religious practices. The interview takes about 15 to 20 minutes to administer and collects information about 10 areas: personal history, cooking/food preparation, shopping, finances, medicines, religious attendance, communication with friends/relatives, social and family roles, organization of home/personal clothing, and recognition/awareness. Each item is scored from 0 to 2, with 2 indicating good performance. Total scores, calculated by summing the scores on all items, range from 0 to 20. The CHIF instrument is shown in the Appendix, published online attached to the electronic version of this paper at www.journals.cambridge.org/jid_IPG. A simple training plan, lasting approximately half a day, was established at both sites, where the senior physicians would review the items and the scoring system with the other participating physicians and nurses. During the testing of the CHIF, the clinicians administering the instrument were blind to information from the informant interview and from the results of the neuropsychological testing. The results from the CHIF were not presented or used in the diagnostic process. However, the clinicians who administered the CHIF also participated in the diagnostic process.
The CHIF was tested for inter-rater reliability during the course of the clinical assessment phase of the study on 12 consecutively scheduled Indianapolis subjects and 14 consecutively scheduled Ibadan subjects. One clinician conducted the interview and completed the instrument while a second clinician also scored the subject’s response independently. In Ibadan, both clinicians were physicians, and in Indianapolis, they were a physician and a nurse.
Statistical analysis
All analyses were performed on each site separately. Baseline characteristics were compared between the participants with and without dementia using t-tests for continuous variables and Fisher’s exact tests for categorical variables. Pearson’s correlation coefficients were calculated between the CHIF and both the Blessed Dementia Scale and the MMSE. Logistic regression models with dementia vs. non-dementia as the dependent variable were fit for each site to see if CHIF was associated with dementia after adjusting for other demographic variables such as age, gender and education. For Ibadan, exact logistic regression was used as none of the dementia participants had any formal education and age was divided into three levels: 69–74, 75–84 and 85+. For Indianapolis, logistic regression models were conducted treating age as a continuous variable and also in the three age categories. Sensitivities and specificities for participants with and without dementia were determined for various cutpoints on the CHIF. In addition, receiver operator characteristic (ROC) curves were plotted and the area under the curve (AUC) was calculated.
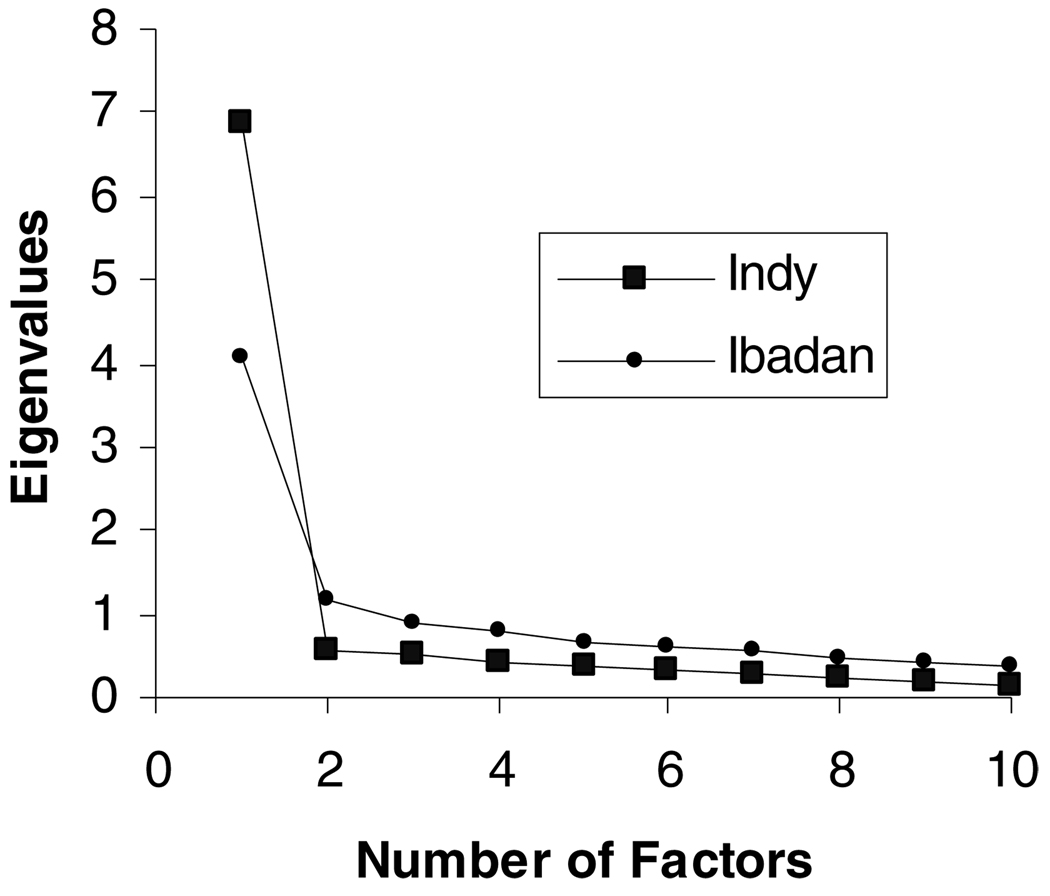
Factor analysis with varimax rotation was conducted for the CHIF. This included examining scree plots and the proportion of variance explained by each eigenvalue to identify major factors common to CHIF items.
Cronbach’s coefficient α of the CHIF was calculated using the entire sample from each site. Using the reliability samples, the percentage agreement between the two raters was calculated for each item on the CHIF. Pearson’s correlation coefficients were calculated between the total scores by the two raters.
All analyses were performed using SAS version 9.1.
Results
Reliability
Indices of inter-rater reliability were high at both sites. Pearson’s correlation coefficient between the two assessments was 0.99 (p < 0.0001) in Indianapolis and 0.87 (p < 0.0001) in Ibadan. Table 1 shows that the clinicians at the two sites scored the participants similarly on most of the items. Differences, when they did occur, were only one point in the scoring system. However, even a one-point difference could have clinical significance in a scale such as this, reinforcing the importance of conducting an initial training session.
Table 1.
Agreement of the two raters at each site using the reliability sample
| INDIANAPOLIS (n = 12) N (%) |
IBADAN (n = 14) N (%) |
|
|---|---|---|
| Personal History | 12 (100) | 13 (92.9) |
| Cooking/Food Preparation | 12 (100) | 13 (92.9) |
| Shopping | 12 (100) | 13 (92.9) |
| Finances | 11 (91.7) | 12 (85.7) |
| Medicines | 12 (100) | 12 (85.7) |
| Church/Mosque | 12 (100) | 8 (57.1) |
| Communication/Telephone | 12 (100) | 13 (92.9) |
| Roles | 12 (100) | 13 (92.9) |
| Organization of Home/Personal Clothing | 12 (100) | 13 (92.9) |
| Recognition | 10 (83.3) | 12 (85.7) |
Validity
There were 201 Indianapolis and 308 Ibadan participants who received a CHIF evaluation. Of the Indianapolis participants, 46 had missing items, leaving 155 (40 with dementia, 115 without) for whom all items on the CHIF were complete. Of these, 153 also had an MMSE score and 88 had a Blessed score. Of the Ibadan participants, only 13 had missing items. Thus, there were 295 Ibadan participants (38 with dementia and 257 without) for whom the CHIF was completed. Of these, 293 completed an MMSE and 294 a Blessed. Baseline characteristics of the subjects are shown in Table 2. In both sites, participants with dementia were significantly older that those without dementia (p = 0.0292 for Indianapolis and p = 0.0112 for Ibadan). In Ibadan, non-dementia participants had more education (p = 0.0124). In addition, in these sites, the participants without dementia functioned significantly better, as evidenced by the CHIF, Blessed and MMSE scores (all p-values < 0.0001). Table 3 shows that for all items on the CHIF in both sites, the participants without dementia functioned significantly better than those with dementia (p < 0.0001 for all).
Table 2.
Baseline characteristics of subjects with and without dementia at both sites
| INDIANAPOLIS |
IBADAN |
|||||
|---|---|---|---|---|---|---|
| WITH DEMENTIA (N =40) |
WITHOUT DEMENTIA (N =115) |
p- VALUE | WITH DEMENTIA (N =38) |
WITHOUT DEMENTIA (N =257) |
p- VALUE | |
| Age | 83.4 ± 6.8 | 80.7 ± 6.4 | 0.0292 | 82.9±10.7 | 78.2 ± 6.6 | 0.0112 |
| Female gender, n (%) | 30 (75.0) | 81 (70.4) | 0.6857 | 33 (86.8) | 190 (73.9) | 0.1052 |
| Highest level of education/ attended school |
8.9 ± 2.5 | 9.3 ± 3.0 | 0.4668 | 0 (0.0%) | 35 (13.6%) | 0.0124 |
| Total CHIF | 9.6 ± 5.4 | 18.7 ± 2.1 | < 0.0001 | 14.2 ± 3.5 | 18.8 ± 1.7 | < 0.0001 |
| Blessed | 4.4 ± 3.0 | 1.1 ± 1.6 | < 0.0001 | 3.4 ± 2.3 | 1.2 ± 1.3 | < 0.0001 |
| MMSE | 18.4 ± 5.6 | 25.8 ± 2.8 | < 0.0001 | 12.3 ± 2.9 | 19.3 ± 4.5 | < 0.0001 |
CHIF = Clinician Home-based Interview to assess Function; Blessed = Blessed Dementia score; MMSE = Mini-mental State Examination score.
Table 3.
Comparison of subjects with and without dementia on CHIF items at both sites
| INDIANAPOLIS |
IBADAN |
|||||
|---|---|---|---|---|---|---|
| WITH DEMENTIA |
WITHOUT DEMENTIA |
p- VALUE | WITH DEMENTIA |
WITHOUT DEMENTIA |
TOTAL | |
| Personal History | 1.2 ± 0.7 | 2.0 ± 0.2 | < 0.0001 | 1.7 ± 0.5 | 2.0 ± 0.2 | < 0.0001 |
| Cooking/Food Preparation | 1.0 ± 0.7 | 1.9 ± 0.3 | < 0.0001 | 1.5 ± 0.6 | 1.9 ± 0.3 | < 0.0001 |
| Shopping | 0.8 ± 0.6 | 1.9 ± 0.4 | < 0.0001 | 1.2 ± 0.7 | 1.9 ± 0.3 | < 0.0001 |
| Finances | 0.9 ± 0.7 | 1.9 ± 0.4 | < 0.0001 | 1.3 ± 0.6 | 1.9 ± 0.3 | < 0.0001 |
| Medicines | 0.7 ± 0.6 | 1.8 ± 0.4 | < 0.0001 | 1.5 ± 0.6 | 1.9 ± 0.3 | < 0.0001 |
| Church/Mosque | 1.0 ± 0.7 | 1.9 ± 0.4 | < 0.0001 | 1.3 ± 0.5 | 1.7 ± 0.4 | < 0.0001 |
| Communication/Telephone | 1.3 ± 0.8 | 1.9 ± 0.3 | < 0.0001 | 1.4 ± 0.6 | 1.9 ± 0.3 | < 0.0001 |
| Roles | 0.9 ± 0.7 | 1.8 ± 0.4 | < 0.0001 | 1.1 ± 0.5 | 1.8 ± 0.4 | < 0.0001 |
| Organization of Home/ Personal Clothing |
1.1 ± 0.7 | 1.8 ± 0.4 | < 0.0001 | 1.6 ± 0.6 | 1.9 ± 0.4 | < 0.0001 |
| Recognition | 0.9 ± 0.7 | 1.9 ± 0.4 | < 0.0001 | 1.5 ± 0.6 | 1.9 ± 0.3 | < 0.0001 |
The Cronbach α coefficient was 0.95 for Indianapolis and 0.83 for Ibadan. The correlation coefficients between the Blessed and the CHIF were −0.71 for Indianapolis and −0.56 for Ibadan (p < 0.001 for both sites). The correlation coefficients between the MMSE and the CHIF were 0.75 for Indianapolis and 0.44 for Ibadan (p < 0.001 for both sites).
Logistic regression models showed that, at both sites, the CHIF was significantly associated with dementia (p < 0.0001 for both) even after adjusting for age, gender and education. In Indianapolis, none of the covariates was significant (age p = 0.1725; gender p = 0.2569; and highest education level p = 0.4963). Treating age as three categories provided similar results. In Ibadan, both age and gender were also not significant (p = 0.7723 and 0.4228, respectively) but exact logistic regression showed that having any education was marginally significant (p = 0.0780).
The various scores on the CHIF and the corresponding sensitivities/specificities for dementia for both sites are shown in Table 4. Figure 1 shows the ROC curves for each site. The AUC was 0.965 for Indianapolis and 0.925 for Ibadan.
Table 4.
Sensitivity/specificity table on dementia for various CHIF scores for Indianapolis and Ibadan
| SCORE ON CHIF |
INDIANAPOLIS |
IBADAN |
||
|---|---|---|---|---|
| SENSITIVITY | SPECIFICITY | SENSITIVITY | SPECIFICITY | |
| 20 | 100.0 | 0.0 | 100.0 | 0.0 |
| 19 | 100.0 | 53.9 | 100.0 | 48.6 |
| 18 | 97.5 | 71.3 | 89.5 | 68.5 |
| 17 | 95.0 | 79.1 | 68.4 | 82.5 |
| 16 | 85.0 | 87.0 | 52.6 | 89.1 |
| 15 | 77.5 | 89.6 | 50.0 | 94.2 |
CHIF = Clinician Home-based Interview to assess Function.
Figure 1.
ROC curves for CHIF at both sites of dementia vs. non-dementia.
Factor analysis showed that one factor seemed appropriate for both sites. Figure 2 shows the scree plots of the two sites while Table 5 shows the factor loadings of the CHIF items at each site assuming one factor. The factor loadings range from 0.72 to 0.90 for Indianapolis and from 0.47 to 0.79 for Ibadan. Additionally, Table 5 shows all eigenvalues generated in the factor analyses. In Indianapolis, the first factor explained 69% of the total variation. Using the Ibadan data, the first factor explained 41% of the total variation while adding a second factor explained only an additional 12%.
Figure 2.
Scree plots of CHIF at both sites of dementia vs. non-dementia.
Table 5.
Factor analysis results for each site; factor loadings of the CHIF items as one factor and eigenvalues
| INDIANAPOLIS | IBADAN | |
|---|---|---|
| Factor loadings | ||
| Personal history | 0.85 | 0.53 |
| Cook food | 0.82 | 0.61 |
| Shopping | 0.90 | 0.79 |
| Finances | 0.83 | 0.71 |
| Medicine | 0.88 | 0.69 |
| Church | 0.81 | 0.55 |
| Communicate by telephone | 0.81 | 0.61 |
| Roles | 0.86 | 0.77 |
| Organization | 0.72 | 0.47 |
| Recognition | 0.81 | 0.55 |
| Eigenvalues | ||
| 1 | 6.89 | 4.05 |
| 2 | 0.56 | 1.16 |
| 3 | 0.51 | 0.91 |
| 4 | 0.41 | 0.79 |
| 5 | 0.39 | 0.65 |
| 6 | 0.35 | 0.63 |
| 7 | 0.29 | 0.56 |
| 8 | 0.24 | 0.47 |
| 9 | 0.20 | 0.42 |
| 10 | 0.16 | 0.37 |
CHIF = Clinician Home-based Interview to assess Function.
Discussion
Obtaining information about ADL from participants, in the absence of reliable informants, is a major problem for epidemiological studies. The semi-structured interview, the CHIF, was developed to meet this need by the Indianapolis and Ibadan researchers. The CHIF is relatively brief, easy to administer and score after a short training period, and adds minimally to participant burden. Our analyses demonstrate high degrees of reliability for most items at both sites, as well as good internal consistency (Cronbach’s α was 0.95 for Indianapolis and 0.83 for Ibadan). The factor analysis supports the concept that the interview was measuring a single domain with both the Yoruba and African Americans; the factor explained 69% of the variation in African Americans and 41% of the variation in Yoruba.
Our primary validity measurements were the subject-derived MMSE scores and the informant-based Blessed Dementia Scale scores, which were measured independently from, and blind to, the results from the CHIF. Highly significant correlations between the CHIF and both of these measures were demonstrated at both sites (Blessed Indianapolis −0.71; Blessed Ibadan −0.56; MMSE Indianapolis 0.75; MMSE Ibadan 0.44). While the results are consistently somewhat lower in the Ibadan cohort, they compare favorably with the application of other instruments to international sites (Jorm, 2004) and support the concept that the CHIF is a valid instrument for measuring function directly, at least in African American and Yoruba.
Data from the CHIF were also analyzed in association with clinical diagnoses of dementia/no dementia. However, in this regard, it should be pointed out that while the CHIF scores were not used for diagnostic purposes, the clinicians, who collected that information, also participated in the diagnostic conferences. It is possible that their experience with the CHIF influenced, in some way, their clinical judgments. Both mean total scores from the CHIF and scores from each item were significantly different between subjects with and without dementia, with subjects with dementia functioning at a lower level in all cases at both sites. We also determined the sensitivities and specificities of the CHIF scale with the diagnosis of dementia. The area under the ROC curve for dementia diagnoses was an impressive 0.965 for Indianapolis and 0.925 for Ibadan. The CHIF, which was originally designed for use by experienced clinicians, is currently in a semi-structured form. There would appear to be no reason, however, why it could not be administered by any skilled interviewer, but this would probably require transforming the interview to a more structured form and the use of a more rigorous training plan. The CHIF could also be added to traditional clinical interviews, obtaining medical and psychosocial information. The interview was originally intended to be used only when an informant was not available, but the information derived from it was deemed to be so useful by our study faculty that it is now administered to all participants, regardless of the availability of an informant. One other limitation of the interview is that it can only be administered as part of a home-based interview and requires the administrator to have local knowledge. A clinically-based version of the CHIF would require considerable modifications, but may be possible. It should also be pointed out that there are now available direct performance-based assessments from occupational therapy that have been used successfully with patients with dementia (Mahurin et al., 1991), but these assessments are usually lengthy and have not been used so far to any great extent in population-based studies.
The development and testing of the CHIF was designed specifically for use in the Indianapolis–Ibadan study. We are encouraged that these results demonstrate its utility in these two populations from very different socioeconomic and cultural backgrounds. We propose that this approach of collecting information on functioning directly from participants may be a useful addition to other international studies of dementia but would require further validation in the populations to be studied including the selection of the appropriate items to reflect the culture and social circumstances of the study population (Fillenbaum et al., 1999).
Acknowledgments
Supported for this work was provided by NIA Grant AG09965 and Alzheimer’s Association/F.M. Kirby Foundation Pilot Research Grant IRG-95-084.
Footnotes
Conflict of interest
None.
Description of authors’ roles
H. C. Hendrie, K. Hall, F. W. Unverzagt, O. Ogunniyi, O. Baiyewu, O. Gureje and R. Evans participated in the study concept and design, acquisition of data analysis and interpretation of data, and drafting of the manuscript. S. Gao and K. A. Lane provided statistical expertise, participated in the analysis and interpretation of data and critical revision of the manuscript. V. Smith-Gamble and M. Pettaway participated in the acquisition and interpretation of the data and the critical revision of the manuscript.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 3rd ed. revised. Washington, DC: American Psychiatric Association; 1987. [Google Scholar]
- Blessed G, Tomlinson BE, Roth M. The association between quantitative measures of dementia and of senile change in the cerebral grey matter of elderly subjects. British Journal of Psychiatry. 1968;114:797–811. doi: 10.1192/bjp.114.512.797. [DOI] [PubMed] [Google Scholar]
- Fillenbaum GG, et al. Development of an activities of daily living scale to screen for dementia in an illiterate rural older population in India. Age and Ageing. 1999;28:161–168. doi: 10.1093/ageing/28.2.161. [DOI] [PubMed] [Google Scholar]
- Gureje O, et al. The CERAD neuropsychological test battery: norms from a Yoruba speaking Nigerian sample. West African Journal of Medicine. 1995;14:29–33. [PubMed] [Google Scholar]
- Hall KS, Gao S, Emsley CL, Ogunniyi AO, Morgan O, Hendrie HC. Community Screening Interview for Dementia (CSID); performance in five disparate study sites. International Journal of Geriatric Psychiatry. 2000;15:521–531. doi: 10.1002/1099-1166(200006)15:6<521::aid-gps182>3.0.co;2-f. [DOI] [PubMed] [Google Scholar]
- Hendrie HC, et al. Alzheimer’s disease is rare in Cree. International Psychogeriatrics. 1993;5:5–14. doi: 10.1017/s1041610293001358. [DOI] [PubMed] [Google Scholar]
- Hendrie HC, et al. Incidence of dementia and Alzheimer disease in 2 communities: Yoruba residing in Ibadan, Nigeria, and African Americans residing in Indianapolis, Indiana. JAMA. 2001;285:739–747. doi: 10.1001/jama.285.6.739. [DOI] [PubMed] [Google Scholar]
- Jorm AF. The Informant Questionnaire on Cognitive Decline in the Elderly (IQCODE): a review. International Psychogeriatrics. 2004;16:275–293. doi: 10.1017/s1041610204000390. [DOI] [PubMed] [Google Scholar]
- Knopman DS, Boeve BF, Petersen RC. Essentials of the proper diagnoses of mild cognitive impairment, dementia, and major subtypes of dementia. Mayo Clinic Proceedings. 2003;78:1290–1308. doi: 10.4065/78.10.1290. [DOI] [PubMed] [Google Scholar]
- Mahurin RK, DeBettignies BH, Pirozzolo FJ. Structured assessment of independent living skills: preliminary report of a performance measure of functional abilities in dementia. Journal of Gerontology. 1991;46:P58–P66. doi: 10.1093/geronj/46.2.p58. [DOI] [PubMed] [Google Scholar]
- McKhann G, Drachman D, Folstein M, Katzman R, Price D, Stadlan EM. Clinical diagnosis of Alzheimer’s disease: report of the NINCDS-ADRDA Work Group under the auspices of Department of Health and Human Services Task Force on Alzheimer’s Disease. Neurology. 1984;34:939–944. doi: 10.1212/wnl.34.7.939. [DOI] [PubMed] [Google Scholar]
- Morris JC, et al. The Consortium to Establish a Registry for Alzheimer’s Disease (CERAD). Part 1. Clinical and neuropsychological assessment of Alzheimer’s disease. Neurology. 1989;39:1159–1165. doi: 10.1212/wnl.39.9.1159. [DOI] [PubMed] [Google Scholar]
- Prescop KL, Dodge HH, Morycz RK, Schulz RM, Ganguli M. Elders with dementia living in the community with and without caregivers: an epidemiological study. International Psychogeriatrics. 1999;11:235–250. doi: 10.1017/s1041610299005803. [DOI] [PubMed] [Google Scholar]
- Richards SS, Hendrie HC. Diagnosis, management, and treatment of Alzheimer disease: a guide for the internist. Archives of Internal Medicine. 1999;159:789–798. doi: 10.1001/archinte.159.8.789. [DOI] [PubMed] [Google Scholar]
- Roth M, et al. CAMDEX: a standardized instrument for the diagnosis of mental disorder in the elderly with special reference to the early detection of dementia. British Journal of Psychiatry. 1986;149:698–709. doi: 10.1192/bjp.149.6.698. [DOI] [PubMed] [Google Scholar]
- Unverzagt FW, et al. Effects of age, education, and gender on CERAD neuropsychological test performance in an African American sample. The Clinical Neuropsychologist. 1996;10:180–190. [Google Scholar]
- World Health Organization. Geneva: World Health Organization; The ICD-10 Classification of Mental and Behavioral Disorders: Clinical Descriptions and Diagnostic Guidelines. 1992