Abstract
The goal of this study is to describe the establishment of an HIV testing and treatment programme in the Jamaican correctional system and to estimate the prevalence of HIV/sexually transmitted disease (STD) among adult incarcerated men in this country. A demonstration project was implemented by the Jamaican Department of Correctional Services and Ministry of Health in the nation’s largest correctional centre. All inmates were offered HIV and syphilis testing, and a subset was offered chlamydia, gonorrhoea and trichomoniasis testing. Cross-sectional data from the project were reviewed to determine the prevalence and correlates of HIV/STD. HIV test acceptance was 63% for voluntary testers (n = 1200). The prevalence of HIV was 3.3% (95% confidence interval [CI] 2.33–4.64) (n = 1017) and the prevalence syphilis was 0.7% (95% CI 0.29–1.49) (n = 967). Among the subset tested (n = 396) the prevalence of chlamydia was 2.5% (95% CI 1.22–4.49) and for trichomoniasis it was 1.8% (95% CI 0.01–3.60), but no cases of gonorrhoea were detected (n = 396). The prevalence of HIV was significantly higher at 25% (95% CI 13.64–39.60) for persons located in a separate section where individuals labelled as men who have sex with men (MSM) are separated. HIV/STD testing is important and feasible in Jamaica. A special focus should be placed on providing services to inmates labelled as MSM. Other Caribbean nations may also benefit from similar programmes.
Keywords: prisons, seroprevalence, HIV/STD testing, homosexual men, Jamaica
INTRODUCTION
Early diagnosis of HIV and provision of treatment is critical to improving the health of infected individuals and preventing further transmission.1 In order to effectively identify persons infected with HIV and facilitate their care, populations most vulnerable to transmission must be included in screening and treatment efforts. Incarcerated populations are vulnerable to HIV, and globally tend to have significantly higher HIV prevalence rates than non-incarcerated populations.2–5 The majority of persons who are incarcerated are in low and middle-income countries (6.25 million people).6,7 Yet, HIV programmes and data characterizing the epidemic among this group are sorely lacking in developing countries,3,4 including those in the Caribbean, the second most affected region in the world in terms of HIV prevalence.8,9 A focus on incarcerated populations is warranted given their increased vulnerability. There is potential to significantly impact the health of those incarcerated by offering testing and treatment services. An additional benefit, especially of counselling services, would be to prevent transmission in the community when individuals are released.1,3,10
In Jamaica, a high priority has been placed on the provision of HIV testing and treatment services for persons who are incarcerated. 11 Jamaica houses the fourth largest incarcerated population in the Caribbean after Cuba, Puerto Rico and the Dominican Republic, numbering 3833 persons in 2006.6,12 The adult HIV prevalence in Jamaica is estimated at 1.5% based on sentinel surveillance from antenatal clinic attendees,13 and is transmitted predominantly through heterosexual sex.14 HIV prevalence estimates are much higher among select groups including men who have sex with men (MSM) (31%)15 and commercial sex workers (10%).14 Estimates of the prevalence of HIV in Jamaican correctional centres are based on small non-representative convenience samples and range from 6%14 to 12%.16
The Jamaican Department of Correctional Services (DCS) and the Ministry of Health (MOH) developed an initiative to provide HIV/sexually transmitted disease (STD) testing, treatment and education as a part of the standard of care in correctional institutions. As part of this initiative, a demonstration project was conducted in the nation’s largest all-male maximum security correctional centre. This study presents data from the demonstration project including the uptake of testing and an estimate of the prevalence of HIV/STD in this institution.
METHODS
Data from a demonstration project conducted by the Jamaican DCS and MOH were reviewed. The correctional centre chosen for the demonstration project is the largest institution in Jamaica, housing approximately 43% of all inmates. It is a maximum security facility and one of two reception institutions. Preparation for the demonstration project included an educational campaign and the training of inmate peer educators. Physical changes were also made to the medical unit to facilitate on-site rapid testing, confidential counselling and follow-up treatment. Correctional medical officers were trained in HIV rapid test analysis. MOH counsellors from outside the DCS were recruited to provide counselling and testing services. HIV/STD testing for the demonstration project was conducted from March to October 2006. The provision of HIV testing and follow-up treatment is currently ongoing.
DCS HIV testing policy
Health service delivery within correctional centres in Jamaica is at the discretion of the DCS administration. The DCS adopted an HIV testing policy that required new admissions (persons incarcerated <6 months) and psychiatric patients to participate in mandatory opt-out testing, while current inmates (persons incarcerated >6 months) were offered HIV testing on a voluntary basis. Inmates in the mandatory opt-out group who actively refused testing were not forced to provide a blood sample. We refrain from describing this process as ‘routine’ testing because: (1) the term mandatory was used to describe the process to inmates; (2) inmates were not informed of an option to decline; and (3) perceived autonomy within a correctional centre is limited. True choice, as routine testing implies, would require a more thorough informed consent process similar to that followed for inmates offered voluntary testing.
The DCS policy on HIV testing was based on several factors. First, for psychiatric patients there was concern on the part of the DCS that inmates with impaired cognitive functioning may be more susceptible to sexual abuse while incarcerated and would thus benefit from services. The term ‘psychiatric patient’ refers to inmates who suffer mental illness to the extent that they are unable to provide informed consent for medical care. This determination is based on the evaluation of the institution psychiatrist. Medical care for these inmates is legally at the discretion of the Commissioner of Corrections in the same way that care outside the institution is relegated to a legal guardian. Second, for new admissions, the policy was adopted as a means of increasing the number of inmates who test for HIV. However, the DCS also noted the potential consequence of increased stigma for inmates who have not had access to heterosexual relationships for six months or longer. Thus, current inmates were offered voluntary testing.
Recruitment
Inmates were housed on five different sections. The ‘main’ section (58%), the ‘associate’ section (10%), the ‘labour’ section (17%), the ‘medical’ section (10%) and the ‘homosexual’ section (5%). Inmates were escorted by section to the counselling and testing area in groups of approximately 8–25 inmates. Each day an escort officer and inmate peer educator were given a list of persons on the section to recruit. New admissions participated on an ongoing basis as they entered the institution. Once in the counselling area, MOH counsellors facilitated a general introduction followed by one-on-one confidential counselling in private areas in accordance with national guidelines.17
Three hundred and ninety-six participants were also offered testing for chlamydia, gonorrhoea and trichomoniasis (the first 200 and a subsequent random sample of 196 participants). The prevalence of these types of infections among this subset was low (less than 3%), thus testing was not offered to remaining inmates. In addition to daily counselling and testing, a three-day mass testing event that followed the same protocol was conducted with additional personnel.
Counselling sessions were confidential. Unique identifiers were used to label specimens. A database linking patient information and identifiers was maintained by MOH counsellors. All patient information was stored in a locked file cabinet by MOH counsellors and shared only with medical personnel for the provision of follow-up treatment.
Specimen collection and analysis
Participants were given the option of testing for HIV through blood draw or by finger prick. Analysis of blood and serum samples for the presence of HIV-1 and/or HIV-2 antibodies was performed through use of the Determine HIV1/2 assay (Abbott Laboratories, Abbott Park, IL, USA) according to the manufacturer’s directions. Blood draw was required for syphilis testing and the serum samples were analysed using the nontreponemal TRUST assay (Toluidine Red Unheated Serum Test [New Horizons Diagnostics Inc., Columbia, MD, USA]). All positive HIV and reactive syphilis tests were sent to the national STD testing laboratory (Comprehensive Health Clinic [CHC]) for confirmation testing. A random specimen from every 10 blood samples collected for HIV and syphilis testing was analysed by the CHC laboratory for quality control.
The subset of participants tested for chlamydia, gonorrhea and trichomoniasis were asked to provide a sample of urine that was shipped to the Johns Hopkins International STD Research Laboratory in Baltimore, Maryland. The APTIMA Combo 2 kit (Gen-Probe, Inc., San Diego, CA, USA) was used to collect samples that were tested for the presence of Chlamydia trachomatis (CT), and Neisseria gonorrhoeae (NG), and Trichomonas vaginalis using the nucleic acid amplification test. The transcription – mediated amplification assay available as an analyte specific reagent through the Gen-Probe APTIMA COMBO 2 package was used to test for T. vaginalis (Gen-Probe APTIMA COMBO 2 package insert IN0037–04 Rev; Gen-Probe Inc., San Diego, CA, USA).
Follow-up care
Test results were reported to participants during post-test counselling with an MOH counsellor. Blood samples for confirmation of positive HIV results and CD4 tests were taken at the time of post-test counselling with permission of the participant. Follow-up treatment for HIV/STD including antiretroviral therapy was coordinated by the institution doctor. Confidential reporting forms were completed and submitted to the MOH for HIV-infected participants, in keeping with national reporting requirements.17
Ethics approval
Permission to link to programme information related to testing uptake and HIV/STD test results for statistical reporting and research purposes was granted by the MOH Medical Ethics Committee and the Johns Hopkins School of Medicine Internal Review Board.
Statistical analysis
The statistical software, Stata version 8.0 (StataCorp. LP, College Station, TX, USA) was used for data analysis. Frequencies were calculated and differences between categories were determined using chi-squared distribution. Logistic regression was used to explore correlations between dependent and independent variables. Contingency tables with unadjusted odds ratios (OR), adjusted odds ratios (AOR) and 95% confidence intervals (CI) were developed.
RESULTS
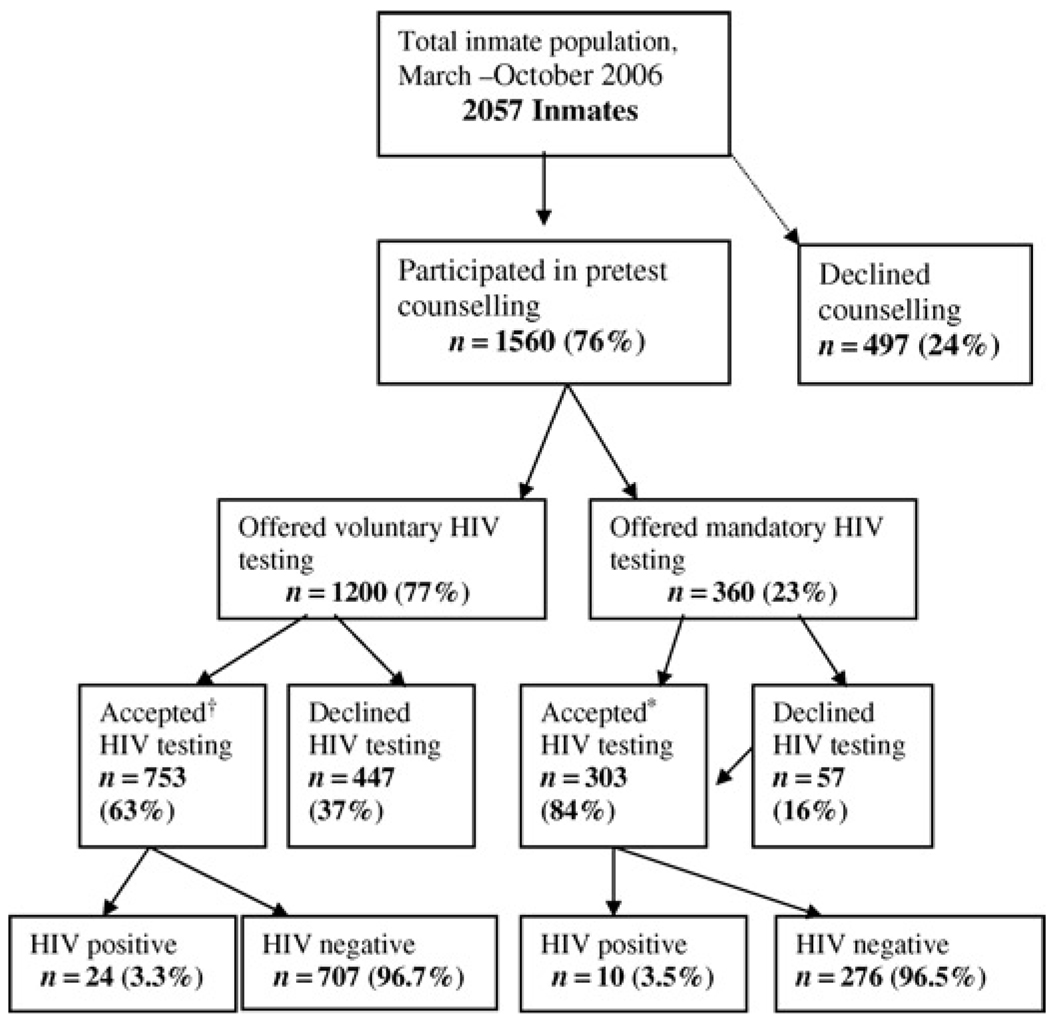
Figure 1 illustrates the participation of inmates in the demonstration project. Over the course of the project, 2057 inmates were incarcerated in the institution and were available for participation. This number exceeds the average daily population as it includes all admissions as well as current inmates transferred or released during the demonstration period. Of this number, a total of 1560 (76%) inmates participated in pretest counselling and 474 (24%) declined pretest counselling and participation in the programme altogether. Participation in pretest counselling, however, exceeded 70% across sections (range 70–82%).
Figure 1.
Flowchart of recruitment, counselling and HIV testing. *Sample insufficient for testing n = 8, results not available at the time of analysis n = 13, inconclusive results n = 1. †Sample insufficient for testing n = 2, results not available at the time of analysis n = 14, inconclusive results n = 1
Out of the 1560 inmates who participated in pretest counselling, 1200 (77%) were current inmates and offered voluntary testing and 360 (23%) were offered mandatory opt-out testing. Of the 1200 inmates offered voluntary testing, 753 (63%) accepted HIV testing and 447 (37%) declined. From the specimens collected for the 753 who accepted HIV testing in the voluntary testing group, eight samples were insufficient for testing, 13 sample results were not available at the end of the study period and one sample result was inconclusive. Of the remaining 731 HIV tests from voluntary testers, 24 (3.3%) were HIV positive and 707 (97%) were HIV negative.
In the mandatory opt-out testing group, 303 (84%) inmates tested for HIV and 57 (16%) refused testing. Two samples were insufficient for testing, 14 sample results were not available at the end of the study period, and one test was inconclusive. Of the remaining 286 tests, 10 (3.5%) were HIV positive and 276 (96%) were HIV negative.
Persons who tested for HIV were similar to those who declined in terms of age. Inmates located on the ‘medical’ section were more likely to test than those on the ‘main’ section. A small number of participants were aware of their HIV-positive status prior to the demonstration project, but requested confirmation testing. These participants were not excluded from analysis. Thus, some participants who accepted testing may have known their HIV status.
Table 1 presents the number and percent testing positive for HIV, and the factors associated with a positive HIV test. The combined total of tests conducted and available for analysis from both the voluntary and mandatory opt-out testing was 1017. A total of 34 persons tested positive for HIV antibodies resulting in a prevalence estimate of 3.3% (95% CI 2.33–4.64%) for this population. Persons who tested positive for HIV and those who tested negative were similar in psychiatric status, admission status and age. However, the likelihood of a positive test result varied by section. The prevalence of HIV for persons located on the ‘homosexual’ section was 25% (95% CI 13.64–39.60) so that persons located on this section were 19.8 times more likely to test positive for HIV than those on the ‘main’ section (AOR 19.83, 95% CI 7.48, 52.58).
Table 1.
Number, percent HIV positive and correlates of HIV-positive test
| Variable | No. tested | No. HIV + (%: 95% CI) | OR (95% CI) (unadjusted) | OR (95% CI) (adjusted) |
|---|---|---|---|---|
| Total | 1017† | 34 (3.3%: 2.33–4.64) | – | – |
| Psychiatric patient | ||||
| No (ref.) | 882 | 31 (3.5%: 2.40–4.95) | ||
| Yes | 135 | 3 (2.2%: 0.46–6.36) | 0.62 (0.19–2.07) | 0.34 (0.08–1.50) |
| Admission | ||||
| No (ref.) | 866 | 27 (3.1%: 2.06–4.50) | ||
| Yes | 151 | 7 (4.6%: 1.88–9.32) | 1.51 (0.65–3.53) | 2.21 (0.82–5.95) |
| Age (17 missing) | ||||
| <25 (ref.) | 194 | 3 (1.6%: 0.32–4.45) | ||
| 26–30 | 265 | 7 (2.6%: 1.07–5.37) | 1.73 (0.44–6.77) | 1.41 (0.34–5.77) |
| 31–35 | 199 | 9 (4.5%: 2.09–8.41) | 3.02 (0.80–11.31) | 2.41 (0.60–9.66) |
| >35 | 342 | 14 (4.1%: 2.26–6.77) | 2.72 (0.77–9.58) | 1.93 (0.49–7.53) |
| Section (19 missing) | ||||
| Main (ref.) | 526 | 10 (1.9%: 0.92–3.47) | ||
| Associate | 115 | 1 (.0.9%: 0.02–4.75) | 0.45 (0.06–3.57) | 0.48 (0.06–4.01) |
| Homosexual | 48 | 12 (25.0%: 13.64–39.60) | 17.2 (6.96–42.50)* | 19.83 (7.48–52.58)* |
| Labour | 160 | 4 (2.5%: 0.69–6.28) | 1.32 (0.41–4.28) | 1.55 (0.46–5.24) |
| Medical | 149 | 4 (2.7%: 0.74, 6.73) | 1.42 (0.43–4.61) | 3.33 (0.82–13.54) |
OR = odds ratio; CI = confidence interval
Significant P < 0.001
Excludes two cases with inconclusive results
Of the 967 persons who tested for syphilis, seven persons or 0.7% (95% CI: 0.29–1.49) tested positive. Of the 396 persons who tested for chlamydia, gonorrhoea and trichomoniasis, 10 persons or 2.5% (95% CI 1.22–4.59) tested positive for chlamydia, and seven persons or 1.8% (95% CI 0.01–3.60) tested positive for trichomoniasis. No cases of gonorrhoea were detected. Of the 396 persons who tested for chlamydia, gonorrhoea and trichomoniasis, 337 also tested for HIV and syphilis. No cases of co-infection were found across any combination of infections. Psychiatric patients, and persons located on ‘labour’ and ‘medical’ sections were over-represented in this sub-sample. Admissions were under-represented in this group.
DISCUSSION
The results of this study suggest that provision of HIV/STD testing and treatment services among the incarcerated population is both important and feasible in Jamaica. The overall prevalence of HIV among incarcerated men in this sample is 3.3%, twice the prevalence of 1.5% found in antenatal clinics,14 but lower than the prevalence suggested by previous non-representative convenience samples of incarcerated men in Jamaica.14,16 This is similar to estimates from Trinidad and Tobago where the HIV prevalence is estimated at 4.9% for the incarcerated population,4,18 compared with 2.6% HIV prevalence for the adult population aged 15–44.19 The prevalence of HIV among incarcerated versus non-incarcerated populations is higher in other regions of the world where injection drug use is more common.4,20 The data from Jamaica, and Trinidad and Tobago indicate that the provision of HIV testing services for incarcerated populations in the Caribbean may aid in identifying more cases of HIV infection in this region, but would not introduce an insurmountable burden to correctional health systems.
Although participants were not randomly selected, the 3.3% HIV prevalence in the sample serves as a strong estimate of the prevalence of HIV in the institution. The majority of inmates participated in pretest counselling (76%), and the majority of those who participated in pretest counselling also tested for HIV (66.9%, voluntary and mandatory opt-out groups combined). Participants were recruited in a systematic manner so that all sections are represented, and test acceptance was high across sections. Persons who chose to test were similar to those who declined testing in terms of age.
There is the potential for selection bias that would underestimate the true prevalence if persons who were HIV infected were less likely to participate in counselling and testing. This has been documented in other correctional centre contexts. 21–23 The use of antibody tests may also lead to a slight underestimate, as a recent seroconversion would not be detected. Additionally, this study included only male inmates in Jamaica, and higher rates of HIV infection among women have been documented in other countries.24
The HIV prevalence estimated among MSM was exceptionally high at 25%, and underscores the need to focus on this group. This higher rate among MSM inmates approaches the HIV prevalence rate of 31.8% estimated for MSM in Jamaica outside of correctional centres,15 and may reflect the higher HIV prevalence among MSM in the wider community. Transmission may also occur inside the institution; however, the cross-sectional nature of these data prohibits our ability to support or refute this hypothesis. Few studies have explored the rate of HIV transmission within correctional centres,25,26 as this remains a sensitive issue within correctional health care globally.
The high prevalence of HIV among MSM found in this study is consistent with other recent reports that suggest the need to refocus on MSM for HIV prevention and treatment in low and middle-income countries27–30 including those in Latin American and the Caribbean.8,15,31,32 The approach taken to address the needs of the MSM population, however, requires a contextually specific understanding of male homosexuality and homophobia. Otherwise, what seems appropriate from a public health standpoint may cause more harm than good for the intended beneficiaries.
Condom distribution within Jamaican correctional centres has been suggested as a means to prevent HIV transmission among MSM.33 However, proposed condom distribution provided the occasion for a 1997 prison riot that coincided with a period of conflict between DCS administration and warder labour unions. During this prison riot homosexual inmates were targeted and killed,34,35 which led the DCS to institute a policy of separating inmates labelled as homosexual. The 1997 prison riot also created a climate of fear related to the provision of HIV services within correctional institutions. Although the root cause of the prison riot may not have been directly related to these issues, stigma against HIV and homosexuality in this context provided an opportunity for the riots to occur. During the current demonstration project, a similar call for condom distribution in correctional centres from outside the DCS was made. This resulted in prison riot threats and the shutdown of the programme for a three-week period,36 as inmates were incensed that persons outside the institution would be given the perception that homosexual sex is common within the institution.
In order to address homophobia, and the barrier it presents to effectively preventing and treating HIV, a focus should be placed on social and structural change that would create the context within which environmental interventions, such as condom distribution, may some day be implemented. Examples of actions that would lead to this type of change include policy advocacy aimed at laws that criminalize homosexual sex and the documentation and prosecution of hate crimes against homosexuals. An additional approach would be to assign social advocates for inmates who are MSM from human rights and non-governmental organizations that partner with the DCS. These advocates would document the health needs of MSM inmates, and may also document and address other issues related to stigma and discrimination experienced by this group such as social isolation leading to limited visitation and potential difficulties with community re-entry because of MSM stigma. The challenge of homophobia should not lead to inaction in terms of HIV prevention and treatment. Rather, what is required is an incremental approach that addresses homosexual stigma, and may ultimately lead to a supportive policy environment for health promotion among this group.
Proponents of mandatory testing suggest that this policy will result in the identification of a greater number of undiagnosed cases and thereby facilitate earlier treatment.37–40 However, voluntary testing may be a more appropriate method within correctional centres where there is potential for inmates to mistrust the motives of the institution. HIV test acceptance among those offered voluntary testing in this programme was 63%. This relatively high rate of test acceptance for a correctional centre context21–23 was achieved by ensuring confidentiality, providing HIV education and engendering the trust of inmates. Thus, even in a correctional context with a history of violence related to HIV and homophobia, a significant number of inmates were willing to test for HIV given the appropriate programme components.
The prevalence of syphilis (0.7%) was slightly lower than the prevalence estimated in the general population (1.4%).41 The prevalence estimated for other STDs including chlamydia (2.5%) and trichomoniasis (1.8%) was higher than the prevalence of urethral discharge syndromes reported among the non-incarcerated population in Jamaica (urethral discharge syndrome 6.5 per 100042). The inclusion of mostly psychiatric patients, who are less likely to be sexually active, and few new admissions may underestimate the true prevalence. A limitation of the study is that it did not include estimates of the prevalence of hepatitis B nor C. Further research that focuses on admissions and inmates prior to release, as well as incarcerated women, may be warranted.
The ability to provide comprehensive and confidential HIV services in Jamaican correctional centres was the direct result of the collaborative partnership between the DCS and MOH. Both agencies contributed to the development of the programme, invested staff and financial resources, and pledged ongoing support for expansion of the programme islandwide. This partnership may serve as a model for other countries.
ACKNOWLEDGEMENTS
We are grateful to the inmates who participated in the demonstration project and thereby contributed to this research study. Additionally, we would like to thank Genprobe, Inc. for their donation of test kits for chlamydia, gonorrhoea and trichomoniasis testing and their support for this project, as well as the Johns Hopkins Laboratories for conducting test analysis. We would also like to thank Claudette Pious and the volunteers of Children First for their support of this programme and dedication to the inmates of Jamaica. Finally, we would like to thank the counsellors, correctional officers and medical orderlies who made the demonstration project possible.
Declarations: This research was funded by the Hopkins AIDS Fogarty International Training Research Group, the US Fulbright Program and NIMH research fellowship F31MH073442-02. Funding and medical supplies for HIV testing for the demonstration project were provided by the Jamaican Ministry of Health through The Global Fund to Fight AIDS, Tuberculosis and Malaria.
REFERENCES
- 1.Centers for Disease Control and Prevention (CDC) Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR. 2006;55:1–17. [PubMed] [Google Scholar]
- 2.United Nations Office on Drugs and Crime (UNODC) [Downloaded 21 September, 2007];HIV/AIDS prevention, care, treatment and support in prison settings: a framework for an effective national response. 2006 Available from http://www.unodc.org/pdf/HIV-AIDS_prisons_July06.pdf.
- 3.United Nations Joint Programme on HIV/AIDS (UNAIDS) [Downloaded 21 September 2007];2006 Report on the Global AIDS Epidemic. Chapter 5: At Risk and Neglected: Four Key Populations. 2006 :104–122. Available from http://www.unaids.org/en/HIV_data/2006GlobalReport/default.asp.
- 4.Dolan K, Kite B, Black E. HIV in prison in low-income and middle-income countries. Lancet Infect Dis. 2007;7:32–41. doi: 10.1016/S1473-3099(06)70685-5. [DOI] [PubMed] [Google Scholar]
- 5.Okie S. Sex, drugs, prisons, and HIV. N Engl J Med. 2007;356:105–108. doi: 10.1056/NEJMp068277. [DOI] [PubMed] [Google Scholar]
- 6.Walmsley R. [(last checked 9 October 2008)];King’s College London, International Centre for Prison Studies; World Prison Population List. (6th edn.). 2006 Available from http://www.kcl.ac.uk/deposta/rel/icps/world-prison-populations-list-2005.pdf.
- 7.World Bank. [(last checked 9 October 2008)];Data and Statistics: Country Groups. Available from http://web.worldbank.org/WBSITE/EXTERNAL/DATASTATISTICS/0,,contentMDK:20421402~pagePK:64133150~piPK:64133175~theSitePK:239419,00.html.
- 8.Figueroa JP. The HIV epidemic in the Caribbean: meeting the challenges of achieving universal access to prevention, treatment and care. West Indian Med J. 2008;57:195–203. [PubMed] [Google Scholar]
- 9.United Nations Joint Programme on HIV/AIDS (UNAIDS) [(last checked 9 October 2008)];Caribbean Fact Sheet. 2006 Available from http://data.unaids.org/pub/GlobalReport/2006/200605-FS_Caribbean_en.pdf.
- 10.Freudenberg N. Jails, Prisons, and the health of urban populations: A review of the impact of the correctional system on community health. J Urban Health. 2001;78:214–235. doi: 10.1093/jurban/78.2.214. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Ministry of Health Jamaica (MOH) Kingston, Jamaica, West Indies: Jamaica HIV/AIDS National Strategic Plan 2002–2006. 2001 October;
- 12.Department of Correctional Services, Ministry of National Security Jamaica (DCS) [(last checked 19 December 2008)];Kingston, Jamaica: Custodial Statistics. 2006 Jan–Dec; Available from http://www.dcsj.net/p/stats.htm.
- 13.Ministry of Health Jamaica (MOH) [Downloaded 16 April 2007];National HIV/STI Prevention and Control Program Facts and Figures: HIV/AIDS Epidemic Update January to June 2006. Available from http://www.jamaica-nap.org/AIDS_DATA_Jan-June_06final.pdf.
- 14.Figueroa JP. An overview of HIV/AIDS in Jamaica: strengthening the response. West Indian Med J. 2004;53:277–282. [PubMed] [Google Scholar]
- 15.Figueroa JP, Weir SS, Jones-Cooper C, et al. High HIV prevalence among hard to reach gay men in Jamaica is associated with high social vulnerability; XVII International AIDS Conference; 3–8 August 2008; Mexico City, Mexico. Abstract # 7427. [Google Scholar]
- 16.Bloomfield B. Teaching SRH in Jamaican prisons: breaking the violence, breaking the silence; International Conference on AIDS; 2004. Jul, pp. 11–16. Abstract No. WePeE6698. [Google Scholar]
- 17.Ministry of Health, Jamaica. National HIV/STD Control Programme. HIV Testing in Jamaica. 2005 June [Google Scholar]
- 18.Lee R, Edwards J, Wagner U. Evaluation of HIV/AIDS/STD Surveillance Trinidad and Tobago, Port of Spain. National Surveillance Unit, Ministry of Health, Caribbean Epidemiology Centre; 1997. [Google Scholar]
- 19.United Nations Joint Programme on HIV/AIDS (UNAIDS) [(last checked 20 November 2007)];Trinidad and Tobago country data. Available at http://www.unaids.org/en/Regions_Countries/Countries/trinidadandtobago.asp.
- 20.United Nations Joint Programme on HIV/AIDS (UNAIDS) [(last checked 20 November 2007)];United States of America Country Data. Available at http://www.unaids.org/en/Regions_Countries/Countries/united_states_of_america.asp.
- 21.Behrendt C, Kendig N, DAmbita C, et al. Voluntary testing for human immunodeficiency virus (HIV) in a prison population with a high prevalence of HIV. Am J Epidemiol. 1994;139:918–926. doi: 10.1093/oxfordjournals.aje.a117098. [DOI] [PubMed] [Google Scholar]
- 22.Hoxie N, Vergeront J, Frisby H, et al. HIV seroprevalence and the acceptance of voluntary HIV testing among newly incarcerated male prison inmates in Wisconsin. Am J Public Health. 1990;80:1129–1131. doi: 10.2105/ajph.80.9.1129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hoxie N, Chen M, Prieve A, et al. HIV seroprevalence among male prison inmates in the Wisconsin Correctional System. WMJ. 1997;97:28–31. [PubMed] [Google Scholar]
- 24.Maruschak LM. HIV in prisons, 2004. [Downloaded 16 April 2007];Bureau of Justice Statistics Bulletin. 2006 November; Available from http://www.ojp.usdoj.gov/bjs/pub/pdf/hivp04.pdf.
- 25.Krebs CP, Simmons M. Intraprison HIV transmission: an assessment of whether it occurs, how it occurs, and who is at risk. AIDS Educ Prev. 2002;14(5 Suppl B):53–64. doi: 10.1521/aeap.14.7.53.23865. [DOI] [PubMed] [Google Scholar]
- 26.Centers for Disease Control and Prevention. HIV transmission among male inmates in a state prison system – Georgia, 1992–2005. MMWR. 2006;55:421–426. [PubMed] [Google Scholar]
- 27.Ki-Moon B, Piot P, Soto-Ramirez L, Chan M. Opening Plenary; XVII International AIDS Conference; 3 August 2008; Mexico City, Mexico. [(last checked 9 October 2008)]. Available at http://www.kaisernetwork.org/health_cast/uploaded_files/080308_ias_opening_transcript.pdf. [Google Scholar]
- 28.The Foundation for AIDS Research (amFAR) [(last checked 9 October 2008)];MSM, HIV, and the road to universal access-how far have we come? 2008 August; Available from http://www.amfar.org/binary-data/AMFAR_PUBLICATION/download_file/000/000/54-1.pdf. [Google Scholar]
- 29.Baral S, Sifakis F, Cleghorn F, Beyrer C. Elevated risk for hiv infection among men who have sex with men in low- and middle-income countries 2000–2006: a systematic review. [(last checked 9 October 2008)];PLoS Med. 2007 4 doi: 10.1371/journal.pmed.0040339. Available from http://medicine.plosjournals.org/perlserv/?request=get-document&doi=10.1371/journal.pmed.0040339&ct=1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cáceres CF, Konda K, Segura E, Lyerla R. Epidemiology of male same-sex behaviour and associated sexual health indicators in low-and middle-income countries: 2003–2007 estimates. Sex Transm Infect. 2008;84 Suppl. I:49–56. doi: 10.1136/sti.2008.030569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Schwarländer B, Roel C, Luiz L. The HIV/AIDS epidemic in the Latin America and Caribbean region. AIDS. 2002;16 Suppl. 3:S1–S2. [Google Scholar]
- 32.Cáceres CF. HIV among gay and other men who have sex with men in Latin America and the Caribbean: a hidden epidemic? AIDS. 2002;16 Suppl. 3:S23–S33. doi: 10.1097/00002030-200212003-00005. [DOI] [PubMed] [Google Scholar]
- 33.Gray V. [(last checked 2 January 2008)];“No Condoms in Prisons” Full Stop – a narrow minded and backward response. 2006 Available from http://www.nacjamaica.com/images/content/article%20for%20sunday%20gleaner%20-%20about%20condoms%20in%20prisons_07-08-30.pdf. [Google Scholar]
- 34.Gleaner, The Jamaican. Brawl at GP. 1997 August 21;Vol. 163(194) [Google Scholar]
- 35.Gleaner, The Jamaican. Prison riots spread. 1997 August 22;Vol. 163(195) [Google Scholar]
- 36.Gleaner, The Jamaican. [(last checked 2 January 2008)];Riot alert – prison unrest looms over condom dispute. 2006 June 27; Available from http://www.jamaica-gleaner.com/gleaner/20060627/lead/lead2.html. [Google Scholar]
- 37.Ramratnam B, Rich J, Parikh A. Former prisoners’ views on mandatory HIV testing during incarceration. J Correctional Health Care. 1997;4:155–164. [Google Scholar]
- 38.Amankwaa A, Amankwaa L, Ochie C. Revisiting the debate of voluntary versus mandatory HIV/AIDS testing in US prisons. J Health Hum Serv Adm. 1999;22:220–236. [PubMed] [Google Scholar]
- 39.Braithwaite R, Arriola K. Male prisoners and HIV prevention: a call for action ignored. Am J Public Health. 2003;93:759–763. doi: 10.2105/ajph.93.5.759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Basu S, Smith-Rohrberg D, Hanck S, et al. HIV testing in correctional institutions: evaluating existing strategies, setting new standards. AIDS Public Pol J. 2005;20:3–24. [PubMed] [Google Scholar]
- 41. [(last accessed 26 November 2009)];Ministry of Health National Strategic Plan 2006–2010. Available from URL: http://www.moh.gov.jm/general/publication.
- 42.National AIDS Committee Jamaica (NAC) [Downloaded: 16 April 2007];Sexually Transmitted Infections Facts and Figures 2000 & 1999. 2000 Available from http://www.nacjamaica.com/sti/facts.htm.