Abstract
Objectives
To examine patient characteristics and outcomes of total knee replacement (TKR) in orthopaedic specialty hospitals.
Methods
We performed a retrospective cohort study in the US Medicare population. We defined specialty hospitals for TKR as centers: (1) that performed >75 TKRs in Medicare recipients in 2000; (2) in which TKR accounted for >7% of all Medicare discharges; and (3) that had <300 beds. We divided specialty hospitals into those with ≤100 beds and those with 101–299 beds. We compared preoperative characteristics and complications among patients undergoing TKR in specialty and nonspecialty centers. We stratified patients according to risk of complications and performed stratum-specific analyses.
Results
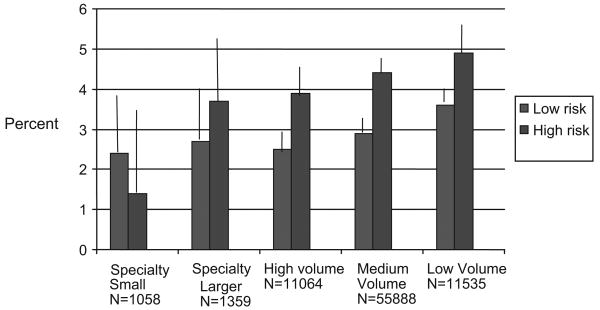
A total of 2417 patients received TKA in 19 specialty hospitals, accounting for 3% of all TKRs in 2000. The specialty hospitals had fewer patients with poverty level income. The smaller “boutique” specialty hospitals had lower complication rates than the larger specialty hospitals and the nonspecialty centers (P value for trend = 0.001). In analyses that adjusted for patient age and sex, low-risk patients had similar outcomes across all hospital categories. However, high-risk patients had statistically significantly greater benefit from treatment in smaller specialty hospitals, with the risk of any adverse event ranging from 1.4% (95% CI, 0%–3.5%) in smaller specialty hospitals to 4.9% (95% CI, 4.4%–5.5%) in low-volume centers.
Conclusions
Smaller specialty hospitals have low complication rates and are especially beneficial for high-risk patients. Further work should address functional outcomes, costs, and satisfaction in these specialty centers, and evaluate strategies to manage more high-risk patients in specialty centers.
Keywords: specialty hospitals, total knee replacement, complications
Surgical outcomes are optimized in centers with a higher volume of surgical procedures. In fact, procedure volume has been accepted as a key attribute of quality care.1–4 A unique type of high-volume hospital emerged in the last 15 years—the specialty hospital, which focuses on specific diagnoses or procedures, typically either cardiovascular or orthopaedic. The number of specialty hospitals in the United States increased 3-fold from 1997 to 2003.5
Recent reports have highlighted the lower risk of complications in cardiovascular specialty hospitals. Analyses that adjusted for procedure volume and case mix revealed no differences in outcomes between nonspecialty and specialty centers.6 However, Cram et al found that specialty orthopaedic centers had lower rates of complications following total hip and knee replacement than general hospitals, among both high- and low-risk patients, even after adjustment for case mix.7
Beyond the recent report by Cram et al,7 little is known about the case mix and outcomes in orthopaedic specialty hospitals. In particular, it is unclear whether specialty centers are especially beneficial for patients at highest risk for complications, and whether smaller “boutique” specialty centers deliver better outcomes than larger specialty centers. The literature on volume and outcomes would suggest that specialty hospitals would have excellent outcomes by virtue of their high volume of procedures.1–3,8,9 Beyond volume, specialization may provide the opportunity for specific investment and expertise that could further improve outcomes.
The objective of this report is to compare case mix and outcomes for high- and low-risk patients across different hospital types. We hypothesize that patients who have TKR in hospitals that focus intensively on TKR will have more favorable case mix and fewer complications, even after adjusting for case mix. Further, we hypothesize that specialty centers are especially beneficial in patients at highest risk for complications and that the benefits of specialty care are most evident in the smallest specialty hospitals.
Methods
Data Sources and Patient Sample
This study used Medicare claims submitted by hospitals (Medicare Part A) and surgeons (Medicare Part B). Additional hospital characteristics were obtained from the 2000 Annual Hospital Survey of the American Hospital Association.10 We focused on identifying and analyzing cases of TKR performed in the US Medicare population between January 1, 2000 and August 31, 2000. We did not analyze cases performed after August 30 to ensure complete ascertainment of outcomes within the first 3 postoperative months.
Cases of primary TKR were identified by searching for claims with International Classification of Diseases, 9th Clinical Modification (ICD-9-CM) code 81.54 or Current Procedural Terminology (CPT) code 27447. We excluded patients with codes indicating preexisting knee infection, metastatic cancer, or bone cancer. We also excluded patients enrolled in health maintenance organizations (HMOs) (because HMOs do not routinely file claims), as well as those not enrolled in both parts of Medicare, under 65, and non-US residents. Finally, we excluded patients who had bilateral TKRs in the same hospitalization. Fifteen percent of subjects were excluded, primarily because of bilateral TKR during the same hospitalization.
Categorization of Hospitals
Hospital volume was calculated as the number of primary plus revision TKRs performed by the institution in Medicare patients during 2000. We defined a high-volume hospital as one that performed at least 200 such TKRs. Total Medicare discharges were obtained from the 2000 American Hospital Association Survey of Hospitals.10
We defined specialty hospitals as centers that met each of the following criteria: (1) the hospital performed at least 75 TKRs among Medicare beneficiaries in 2000; (2) TKR accounted for at least 7% of all Medicare discharges in 2000; and (3) the hospital had fewer than 300 beds. We further divided specialty centers into those with especially small bed sizes (≤100) and those with more moderate bed sizes (101–299).
Using these definitions, we created 5 mutually exclusive and collectively exhaustive categories: specialty hospitals with bed size ≤100, specialty hospitals with bed size 101–299 beds, and nonspecialty hospitals in 3 volume strata: >200 TKRs per year; 26–200 TKR per year and <26 TKRs per year in the Medicare population.
Case Mix Variables
Medicare files provided information regarding age, gender, race (white, black, and other/unknown), Medicaid eligibility (an indicator of poverty level income), arthritis diagnosis (osteoarthritis, rheumatoid arthritis, avascular necrosis, and others), and comorbidity. The latter was calculated with an adaptation of the Charlson Index, which incorporates data on comorbid conditions documented in the admission for TKR and in admissions in the prior 6 months.11,12
Patient Outcomes
The 5 outcomes we studied were death, acute myocardial infarction, deep knee wound infection (requiring surgical debridement or prosthesis removal), pneumonia requiring hospitalization, and pulmonary embolus. These outcomes provide insight into general hospital care for TKR patients (eg, pneumonia, myocardial infarction) and care more particular to the procedure (eg, deep wound infection, pulmonary embolus). We examined all such outcomes occurring within 90 days of the admission for TKR. Pulmonary embolus was defined by a hospital ICD-9-CM code of 415.1–415.19. Acute myocardial infarction and pneumonia were defined using ICD-9-CM codes from hospital claims, with algorithms validated by the Agency for Healthcare Research and Quality.13 Acute conditions (pulmonary embolus, myocardial infarction, and pneumonia) were counted as complications if they were listed only on the index TKR admission. If they were listed on a previous admission they were considered comorbidities. Chronic conditions such as diabetes were counted as comorbidities whether they were noted on the index or an earlier admission. We examined each complication separately and also as a composite of any of the aforementioned complications.
Statistical Analyses
We compared the risk of any complication across the 5 hospital categories with multivariable logistic regression models that used generalized estimating equations (GEE) to account for clustering within hospitals. These models adjusted for age (using an ordinal variable in 5-year increments) and sex. Two factors associated with outcome included comorbidity and eligibility for Medicaid. We defined low-risk patients as those with Charlson comorbidity scores ≤1 and not receiving Medicaid, and high-risk patients as those either with Charlson scores >1 or receiving Medicaid. We performed separate analyses for low- and high-risk patients to examine the effect of hospital type on outcome in each group. We used the least squared means procedure to estimate the adjusted mean proportion of adverse events across the 5 hospital types and we used the Duncan multiple comparison test to determine whether any of the stratum-specific mean proportions differed across hospital types.
We also performed sensitivity analyses in which we varied aspects of the definition of a specialty hospital. Specifically, we varied the threshold TKR volume from the base case of 75 TKRs per year in the Medicare population to an alternative criterion of 100 per year. Similarly, we also varied the threshold proportion of all discharges that were TKRs from the base case of 7% to an alternative criterion of 10%. Analyses were performed using SAS statistical software (Cary, NC).
All study procedures were approved by the Human Research Committee of Brigham and Women's Hospital.
Results
Hospital Characteristics
A total of 3141 hospitals performed at least 1 TKR in the Medicare population in 2000, and were included in the American Hospital Association 2000 Survey. Forty-six percent of these hospitals were categorized as low volume and 0.6% (19) met our definition of specialty hospitals. Of these 19 specialty hospitals, 9 had ≤100 beds and 10 had > 100 beds (Table 1). A total of 80,904 TKRs met our entry criteria. Three percent of these procedures were performed in specialty hospitals (Table 1). Specialty hospitals had annual TKR procedure volumes comparable to high-volume centers, but lower bed sizes (Table 1). Eight of the 19 specialty hospitals (42%), were for-profit, as compared with 15% of the nonspecialty hospitals.
Table 1.
Hospital and Patient Characteristics of Specialty, High Volume, and Lower Volume Hospitals
| Smaller Specialty | Larger Specialty | High Volume >200 Cases/Yr | Moderate Volume 26–200 Cases/Yr | Low Volume <25 Cases/Yr | |
|---|---|---|---|---|---|
| Hospital characteristics | |||||
| No. hospitals (%) performing TKR (N = 3141) | 9 (0.3%) | 10 (0.3%) | 90 (3%) | 1,574 (50%) | 1,458 (46%) |
| Mean (SD) annual hospital volume TKR in Medicare population | 257 (171) | 319 (193) | 289 (91) | 72 (41) | 15 (30) |
| Mean (SD) hospital bed size | 50 (29) | 178 (52) | 606 (271) | 265 (173) | 144 (132) |
| Patient characteristics | |||||
| No. patients | 1058 | 1359 | 11,064 | 55,888 | 11,535 |
| Over 75 (%) | 59 | 62 | 59 | 59 | 57 |
| Female (%) | 65 | 67 | 66 | 67 | 67 |
| Nonwhite* (%) | 6.1 | 7.6 | 6.3 | 7.7 | 11 |
| Charlson comorbidity >1 (%) | 9.7 | 14 | 15 | 13 | 12 |
| Medicaid eligible* (%) | 4.6 | 5.6 | 5.3 | 8.2 | 13 |
Smaller specialty = <100 beds; larger specialty = >100 beds.
Test for trend: P < 0.005.
Patient Characteristics
Patient age and sex did not differ across the 5 hospital types (Table 1). Lower volume centers had the highest proportion of patients who were eligible for Medicaid, nonwhite, and who had higher comorbidity scores.
Patient Outcomes in Each Hospital Category
Low-volume hospitals had higher annual crude rates of most adverse outcomes (Table 2). The smaller specialty centers had lower annual rates of several outcomes types including mortality, pneumonia, pulmonary embolus, and the composite “any complication.” We performed multivariate analyses of the risk of any complication, adjusting for age, comorbidity, sex, and Medicaid eligibility. The smaller specialty hospital served as the reference group. The larger specialty hospitals had a somewhat higher risk of complications (OR, 1.5; 05% CI, 0.9%–2.4%), as did the high-volume centers (OR, 1.4; 95% CI, 1.0%–2.1%), medium-volume centers (OR, 1.6; 95% CI, 1.1%–2.4%), and low-volume centers (OR, 2.0; 95% CI, 1.3%–2.8%). The test for trend across the hospital categories was highly significant (P < 0.0001).
Table 2.
Crude Outcomes of Specialty, High Volume, and Lower Volume Hospitals
| Smaller Specialty N = 1058 | Larger Specialty N = 1359 | High Volume >200 Cases/Yr N = 11,064 | Moderate Volume 26–200 Cases/Yr N = 55,588 | Low Volume <25 Cases/Yr N = 11,535 | |
|---|---|---|---|---|---|
| Mortality (%) | 0.38 | 0.59 | 0.62 | 0.60 | 0.81 |
| Acute myocardial infarction (%) | 0.38 | 0.81 | 0.77 | 0.80 | 0.84 |
| Pulmonary embolus (%) | 0.47 | 1.2 | 0.70 | 0.78 | 0.88 |
| Hospitalized pneumonia* (%) | 0.76 | 1.0 | 1.1 | 1.4 | 1.7 |
| Deep knee infection† (%) | 0.19 | 0.15 | 0.24 | 0.37 | 0.49 |
| Any of the above* (%) | 2.1 | 3.1 | 3.0 | 3.5 | 4.2 |
Smaller specialty = ≤100 beds; larger specialty = 101–299 beds.
Test for trend: *P < 0.005; †P < 0.05.
We performed multivariate regression analyses separately in strata defined by low- and high-risk patients. The dependent variable was having any complication. This proportion formed a continuous range from 0 to 1.0, making it suitable for linear regression. The analyses were adjusted for patient age and sex. We examined the adjusted mean proportion of complications for each hospital type (Fig. 1). Among the low-risk patients, there was no statistically significant difference in the risk of complications across the 5 hospital types. However, among the high-risk patients the risk of complications was significantly lower in the small specialty hospitals (1.4%; 95% CI, 0%–3.5%) than in the other hospital types (range, 3.7%–4.9%). This difference in adjusted mean complications between the smaller specialty hospitals and the other hospital types was statistically significant at the 0.05 level.
FIGURE 1.
Adjusted mean proportion of adverse outcomes according to hospital type, stratified by low- and high-risk patients.
Error bars represent upper 95% confidence intervals around the adjusted mean proportion of adverse events.
A sensitivity analysis that used a criterion for specialty hospital designation of 100 TKR per year in the Medicare population, rather than 75, yielded the same associations between hospital type and outcome as the base case analysis. Similarly, a sensitivity analysis that required 10% of all Medicare discharges to be TKR, rather than 7%, also yielded the same associations between hospital type and outcome.
Discussion
We examined case mix and outcomes in 80,904 patients undergoing primary TKR in one of 5 types of hospitals in the United States in 2000. These included larger or smaller specialty hospitals with a dedicated focus on TKR, and 3 types of nonspecialty hospitals distinguished by annual Medicare volume of TKR. There were no substantial differences across the 5 hospital types in the distribution of patient age and sex. The smaller specialty hospitals had fewer patients who were nonwhite, nonpoor, and who had >1 comorbid conditions than the other centers. In general, the lower volume hospitals had a greater risk of perioperative complications than the higher volume hospitals, as anticipated based upon prior work.8 The hospital types are ordered in Tables 1 and 2 to emphasize the association between hospital type and outcome.
There was limited evidence of “cherry picking,” or favorable selection of low-risk patients into the larger specialty centers. However, the smaller specialty centers seemed to have more favorable case selection with respect to non-white race, Medicaid eligibility, and comorbidity.
As hypothesized, the smaller specialty hospitals with ≤100 beds had especially favorable outcomes, even with adjustment for age, sex, comorbidity, and poverty status. The benefit of having TKR in a smaller specialty hospital was especially apparent for high-risk patients (Fig. 1).
Case selection and outcomes of care in specialty hospitals have received relatively little study. Cram et al documented that cardiac specialty hospitals had lower case mix adjusted rates of complications than control centers, but that these differences were explained by hospital volume.6 On the other hand, these authors found that specialty orthopaedic hospitals had lower rates of complications, even after adjustment for case mix.7
We defined orthopaedic hospitals differently than Cram et al,7 who excluded teaching centers. We also based our determination of specialty status on the number of TKR admissions, rather than all orthopaedic admissions, to ensure that the centers had specialized expertise in TKR. Finally, we included all hospitals that performed TKR in our analyses, whereas Cram et al limited controls to nonspecialty hospitals in the same hospital service area as the specialty centers. Because specialty centers may locate where the competition is weak, this may have created a selection bias favoring the specialty hospitals. Our sensitivity analyses, which used alternative definitions of specialty hospital, yielded the same associations between hospital type and outcome.
Our study adds to existing literature by noting that low-risk patients had low rates of adverse events across all hospital types including specialty and nonspecialty centers. In contrast, patients at higher risk for medical complications benefited most from treatment in the specialty centers. Our results suggest that expanded use of specialty hospitals might be beneficial for high-risk patients. The financial and logistic implications of offering specialty hospital care for a large proportion of TKR recipients are profound and should prompt further study.
Despite the large number of TKRs in our sample, we had limited power to compare complication rates among specialty hospitals and the various high-volume hospitals because only 3% of patients had their TKR in a specialty center. Our study, as all claims-based analyses, is also limited by imprecision in the assessment of key case mix variables such as comorbidity and socioeconomic status. It is conceivable that some of the differences in outcome noted across hospital type may reflect residual confounding. Similarly, the distinction between complications and comorbidities is challenging and may result in some misclassification of these variables.
In summary, hospitals with a specialty focus on TKR that had 100 beds or fewer exhibited favorable selection and had lower complication rates than other types of centers, even after adjustment for case mix. Further, these hospitals were more likely to attract low-risk patients. However, the small specialty centers seemed to be especially beneficial for high-risk patients. Further work is required to examine the full range of relevant outcomes in specialty hospitals, including patient functional status, satisfaction, and longevity of the prosthesis; to understand whether total knee replacement and other procedures are more cost-effective in specialty hospitals than in major high-volume centers; and to develop interventions to permit higher-risk patients to take advantage of specialty hospitals.
Acknowledgments
Drs. Katz and Losina had full access to the data and take responsibility for the integrity and accuracy of the analyses.
Supported by a grant from the New England Baptist Hospital and by NIH/NIAMS grants K24 AR02123 and P60 AR 47782.
The funding organizations (New England Baptist Hospital, NIH) did not have any role in design, analysis, or reporting of findings.
References
- 1.Birkmeyer JD, Siewers AE, Finlayson EV, et al. Hospital volume and surgical mortality in the United States. N Engl J Med. 2002;346:1128–1137. doi: 10.1056/NEJMsa012337. [DOI] [PubMed] [Google Scholar]
- 2.Dudley RA, Johansen KL, Brand R, et al. Selective referral to high-volume hospitals: estimating potentially avoidable deaths. JAMA. 2000;283:1159–1166. doi: 10.1001/jama.283.9.1159. [DOI] [PubMed] [Google Scholar]
- 3.Halm EA, Lee C, Chassin MR. Is volume related to outcome in health care? A systematic review and methodologic critique of the literature. Ann Intern Med. 2002;137:511–520. doi: 10.7326/0003-4819-137-6-200209170-00012. [DOI] [PubMed] [Google Scholar]
- 4.Birkmeyer JD, Finlayson EV, Birkmeyer CM. Volume standards for high-risk surgical procedures: potential benefits of the Leapfrog initiative. Surgery. 2001;130:415–422. doi: 10.1067/msy.2001.117139. [DOI] [PubMed] [Google Scholar]
- 5.Iglehart JK. The emergence of physician-owned specialty hospitals. N Engl J Med. 2005;352:78–84. doi: 10.1056/NEJMhpr043631. [DOI] [PubMed] [Google Scholar]
- 6.Cram P, Rosenthal GE, Vaughan-Sarrazin MS. Cardiac revascularization in specialty and general hospitals. N Engl J Med. 2005;352:1454–1462. doi: 10.1056/NEJMsa042325. [DOI] [PubMed] [Google Scholar]
- 7.Cram P, Rosenthal GE, Vaughan-Sarrazin MS, et al. A comparison of total hip and knee replacement in specialty and general hospitals. J Bone Joint Surg Am. 2007;89:1675–84. doi: 10.2106/JBJS.F.00873. [DOI] [PubMed] [Google Scholar]
- 8.Katz JN, Barrett J, Mahomed NN, et al. Association between hospital and surgeon procedure volume and the outcomes of total knee replacement. J Bone Joint Surg Am. 2004;86(-A):1909–1916. doi: 10.2106/00004623-200409000-00008. [DOI] [PubMed] [Google Scholar]
- 9.Katz JN, Phillips CB, Baron JA, et al. Association of hospital and surgeon volume of total hip replacement with functional status and satisfaction three years following surgery. Arthritis Rheum. 2003;48:560–568. doi: 10.1002/art.10754. [DOI] [PubMed] [Google Scholar]
- 10.American Hospital Association. Annual Hospital Survey. Chicago, IL: American Hospital Association; 2000. [Google Scholar]
- 11.Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373–383. doi: 10.1016/0021-9681(87)90171-8. [DOI] [PubMed] [Google Scholar]
- 12.Romano PS, Roos LL, Jollis JG. Adapting a clinical comorbidity index for use with ICD-9-CM administrative data: differing perspectives. J Clin Epidemiol. 1993;46:1075–1079. doi: 10.1016/0895-4356(93)90103-8. [DOI] [PubMed] [Google Scholar]
- 13.AHRQ Quality Indicators. Vol. 2006. Rockville, MD: Agency for Healthcare Research and Quality; 2006. Inpatient Quality Indicators Overview. [Google Scholar]