McLaren et al.1 review two developments in critical thinking about the continued relevance of Rose’s seminal population health strategy and concluded that Rose’s original ideas, now over 25 years old, hold firm. Our commentary will focus on their critique of the suggestion to more widely use multivariate risk algorithms in the population setting.2 We also draw connections between the use of risk algorithms and the authors’ central concerns about the role of social inequalities in relation to intervention or policy coverage. We argue that understanding a population’s baseline risk is a cornerstone of population health planning as articulated by Rose, and therefore it is inexcusable not to use improved methods of baseline risk assessment. Rather than be complacent with Rose’s original method of assessing population risk, we should look forward and further develop multivariate risk algorithms in the population setting.
Population risk assessment is a cornerstone of Rose’s population health strategy
Too often, advocates for a particular population health strategy quote Rose’s principle that ‘shifting the curve is the best approach’ without his required caveat, ‘when risk is diffused in the population’.3 Diffusion of population risk is described by plotting the range and distribution of baseline risk. Too often, we assume that risk is widely distributed without actually assessing it, let alone using an appropriately discriminating risk assessment method such as multivariate risk algorithms. Furthermore, as Rose stated, ‘All policy (including treatment) decisions should be based on absolute measures of risk (baseline risk, in other words); relative risk is strictly for researchers only’.4 Equation (1) shows that policy decisions can be further informed by combining baseline risk with other information to estimate population health benefit or community efficacy.
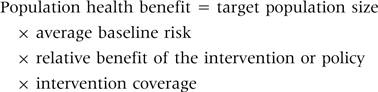 |
(1) |
A problem with terminology may be contributing to this debate. Despite the distinctions offered by McLaren et al. and Frohlich and Potvin,5 the concept of high- or low-baseline risk should not be equated with individual risk factors or associated only with medical or behavioural risk factors. Indeed, strength of multivariate risk algorithms is their recognition that baseline risk results from multiple contributions such as socio-economic position, biologic, demographic and other factors including those that may even begin at or before birth. High-baseline risk populations share similarities with ‘vulnerable populations’, with the additional concept that vulnerable people may have lower coverage (or ‘uptake’ or ‘response’) to interventions or policies.
Community effectiveness and the link between baseline risk, intervention coverage and health inequity
Reducing health inequity is a function of two critical components: baseline risk and intervention coverage. Although McLaren et al. and Frohlich and Potvin rightly focus on the role of coverage in addressing health inequities, improved risk assessment also contributes in two ways. First, discriminating methods (multivariate risk algorithms) of assessing baseline risk allow us to quantify important differences between social groups. With non-discriminating methods (used by Rose), the potential for health inequalities will falsely appear small or non-existent.
Secondly, baseline risk is essential to assessing the potential for policies or interventions to reduce inequities. When we can tease apart the elements of a policy and see how they each contribute to community effectiveness (using an approach such as the ‘equity effectiveness loop’), we can see which components need to be addressed to reduce inequities.6 For example, baseline risk differences can be so large that health inequities can be reduced even when there are inequities in coverage.7 Similarly, when there are large differences in baseline risk, interventions with a low relative benefit will make a small impact in reducing inequities, even if they are ‘radical’ in their focus on upstream prevention or cover the population completely.
Multivariate risk algorithms are a discriminating and accurate method of assessing baseline risk
The main advantage of multivariate risk prediction algorithms over older methods of baseline risk assessement is their improved ability to discriminate risk. Discrimination is defined as the ability to differentiate between those who are high risk and those who are low risk—or in other words distinguishing who will and will not experience the outcome. An algorithm with high discrimination does well at rank-ordering subjects in terms of likelihood of experiencing the event. Calibration or accuracy is another property of a risk algorithm that describes how well the predicted probability of disease closely agrees with the observed outcome. Risk discrimination and risk prediction are intimately related to the description of risk diffusion (Rose’s term) in populations. Take a hypothetical example of a community of 100 000 people where 1000 people will die of heart disease over the next 10 years. In an ideal setting, we would have a perfect ability to discriminate risk and can predict exactly which 1000 people will die. Because population risk is not at all diffused, we could then target only these 1000 people with preventive interventions, resulting in an extremely efficient and effective health strategy. Targeting the remaining 99 000 people with an intervention, even if it was radical, would have no preventive benefit. In public health, we rarely have such a clear knowledge of risk, though our tools are improving.
Twenty-five years ago, we had poor risk prediction tools and so heart disease appeared diffused. To achieve a reduction in heart disease, it appeared that programmes needed to target most of the population. Today, risk prediction tools using multiple risk factors (such as the Framingham algorithm) can identify over a 100-fold difference in heart disease risk between individuals in developed countries.2,7 Population risk for heart disease is much less diffused than previously believed, meaning there are large inequities. Since the inequities are so large for heart disease in many populations, it may be that focused prevention and treatment could be more effective and efficient for reducing inequities than radical interventions that cover the entire population. For maximum benefit, however, health inequities in heart disease and elsewhere are usually best addressed using multiple interventions that include both high-risk and population strategies.
Current challenges in developing and using multivariate risk algorithms in a population setting
The use of predictive risk algorithms in population settings is fairly new, and several methodological challenges may contribute to their limited use. To encourage forward thinking and debate about how best to estimate population risk, we briefly discuss three of these issues here.
Can routinely collected data accurately discriminate risk at the level of populations?
Simple predictive measures such as age and self-reported weight and smoking have been shown to have discriminating power equal to that of detailed clinical data, often with improved accuracy.8,9 To improve the practical use of algorithms, we need to further develop and validate them using only population data such as routinely collected health administrative data or population health surveys.10
What is the right balance between discrimination and accuracy?
Clinicians are chiefly concerned about the discriminating property of a predictive risk tool, but predictive accuracy has proven to be equally important in our collaboration with population health planners. The challenge, as Diamond outlined, is that discrimination and accuracy (or calibration) mathematically compete with each other.11 In population health, we need to better understand what the right balance is and how best to measure and report discrimination and accuracy.
Can population risk algorithms accurately estimate the contribution of individual risk predictors?
Another desirable application of population risk algorithms is to assess the contribution of individual risk factors (including behavioural or social risks) to predictive risk. Risk algorithms are ideal for re-estimating baseline risk under scenarios where individual risk factors are modified. However, there are important interpretive cautions to consider and it is challenging to combine aetiognostic and prognostic research methods.
Conclusion
McLaren et al. acknowledge that multivariate risk algorithms are a more discriminating and accurate risk assessment approach than was available in Rose’s day, but they discount their use by wrongly associating them with only high-risk populations and the health benefits of medical treatment. To the contrary, multivariate risk algorithms can be used to more accurately discriminate risk in any population, including low-risk groups, and can help describe the benefits of all preventive health strategies, including those that are radical or upstream. A high-baseline risk strategy does not mean it focuses on downstream or medical treatment. Even when population risk is concentrated in high-risk groups, population prevention can be used to address underlying causes of disease as well as health inequities. Indeed, upstream interventions that target high-risk groups are extremely common worldwide. An example is means-tested social programmes.
The methods to assess population health strategies should not stand still. Multivariate risk algorithms support Rose’s attention to population risk assessment and can improve the description of risk diffusion and other concepts that are central to population health planning. The single largest challenge is to move beyond the clinical setting to develop and validate risk algorithms especially for population health planning.
Acknowledgements
D.G.M. holds a Chair in Applied Public Health from the Canadian Institute for Health Research and the Public Health Agency of Canada. The opinions, results and conclusions reported in this article are those of the author and are independent from the funding or employment sources.
Conflict of interest: None declared.
References
- 1.McLaren L, McIntyre L, Kirkpatrick S. Rose's; population strategy of prevention need not increase social inequalities in health. Int J Epidemiol. 2010;39:372–77. doi: 10.1093/ije/dyp315. [DOI] [PubMed] [Google Scholar]
- 2.Manuel DG, Lim J, Tanuseputro P, et al. Revisiting Rose: strategies for reducing coronary heart disease. Br Med J. 2006;332:659–62. doi: 10.1136/bmj.332.7542.659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rose G. Sick individuals and sick populations. 1985. Bull World Health Organ. 2001;79:990–96. [PMC free article] [PubMed] [Google Scholar]
- 4.Rose G. Environmental health: problems and prospects. J R Coll Physicians Lond. 1991;25:48–52. [PMC free article] [PubMed] [Google Scholar]
- 5.Frohlich KL, Potvin L. Transcending the known in public health practice: the inequality paradox: the population approach and vulnerable populations. Am J Public Health. 2008;98:216–21. doi: 10.2105/AJPH.2007.114777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Tugwell P, de Savigny D, Hawker G, Robinson V. Applying clinical epidemiological methods to health equity: the equity effectiveness loop. Br Med J. 2006;332:358–61. doi: 10.1136/bmj.332.7537.358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Anderson GM, Bronskill SE, Mustard CA, Culyer A, Alter DA, Manuel DG. Both clinical epidemiology and population health perspectives can define the role of health care in reducing health disparities. J Clin Epidemiol. 2005;58:757–62. doi: 10.1016/j.jclinepi.2004.10.020. [DOI] [PubMed] [Google Scholar]
- 8.Lindstrom J, Tuomilehto J. The diabetes risk score: a practical tool to predict type 2 diabetes risk. Diabetes Care. 2003;26:725–31. doi: 10.2337/diacare.26.3.725. [DOI] [PubMed] [Google Scholar]
- 9.Mainous AG, III, Koopman RJ, Diaz VA, Everett CJ, Wilson PW, Tilley BC. A coronary heart disease risk score based on patient-reported information. Am J Cardiol. 2007;99:1236–41. doi: 10.1016/j.amjcard.2006.12.035. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Rosella L, Manuel D. A population-based risk algorithm for the development of physician-diagnosed diabetes mellitus. Am J Epidemiol. 2006;163:S182. [Google Scholar]
- 11.Diamond GA. What price perfection? Calibration and discrimination of clinical prediction models. J Clin Epidemiol. 1992;45:85–89. doi: 10.1016/0895-4356(92)90192-p. [DOI] [PubMed] [Google Scholar]


