Abstract
Objectives:
Determine nursing home characteristics related to adherence to use of a hip protector (HP) to prevent fracture; also describe adherence and related resident characteristics.
Design:
A multi-center, randomized controlled trial of a HP in which adherence to wearing the HP was monitored by research staff three times a week for up to 21 months; data were collected by interviews and chart review.
Setting:
Thirty-five nursing homes in Boston, St. Louis, and Baltimore.
Participants:
A total of 797 eligible residents, 633 (79%) of whom passed the run-in period, 397 (63%) of whom remained in the study until the end of follow-up.
Intervention:
Residents wore a single HP on their right or left side.
Measurements:
In addition to regular monitoring of adherence, data were collected regarding facility characteristics, staffing, policies and procedures, perception of HPs and related experience, and research staff ratings of environmental and overall quality; and also resident demographic characteristics, and function, health, and psychosocial status.
Results:
Facility characteristics related to more adherence were not being chain-affiliated; less Medicaid case-mix; fewer residents wearing HPs; more paraprofessional staff training; more rotating workers; and having administrators who were less involved in meetings.
Conclusion:
Efforts to increase adherence to the use of HPs should focus on facilities with more Medicaid case-mix to reduce disparities in care, and those that have less of a culture of training. Staff may need support to increase adherence, and when adherence cannot be maintained, HP use should be targeted to those who remain adherent.
Keywords: hip fracture, nursing homes, compliance
INTRODUCTION
More than 340,000 hip fractures occur in the U.S. each year.1 These fractures typically follow a fall, and result in excess dependency and mortality.2,3 Their concern is especially notable in nursing homes (NHs), where 97% of residents have osteoporosis or osteopenia and their rate of hip fracture is 3-11 times that of age-matched community dwellers.4-6
Non-pharmacologic treatments such as hip protectors (HPs) are attractive options to reduce fractures as they avoid the expense and side-effects of medications and their effect is immediate. They are typically composed of a hard shell or dense foam, and fit into an undergarment that positions the HP over the trochanteric prominence. Depending on their style, HPs either absorb (foam) or divert (shell) the energy of a fall away from the greater trochanter to the soft tissue around the hip. Initial evidence regarding the efficacy of HPs was promising, although recent reviews and studies are equivocal; still, newer materials may prove effective in reducing fractures.7-9
One problem has plagued virtually all studies of HPs: low adherence. A recent review found adherence between 20-92% (median 56%), with reasons for non-use related to comfort, effort, incontinence, and physical difficulties.10 It is challenging to compare results across studies because some ask perceptions rather than use;11 some rely on focus groups;12 eligibility criteria and length of follow-up differ; and adherence is assessed using different respondents, timeframes, and strategies.9,13-18 Of note, only two of the latter studies were based in the U.S. and focused on a NH population, and both included only one NH each.17,18
In the U.S., 15,294 NHs with 1.6 million beds cared for 1.4 million residents in 2006.19-21 While information regarding characteristics related to HP adherence from single site studies is informative, it cannot inform facility-level characteristics that relate to adherence – many of which may be modifiable. The importance of facility-level characteristics is evident in other studies that found a relationship between resident outcomes and facility characteristics including ownership, affiliation, case-mix, staffing, services, administrative priorities, and family involvement.22-23
This study examined HP adherence in a large number of U.S. NHs and examined the facility-level predictors of adherence in a randomized trial. Further, it assessed resident-level characteristics related to adherence and delineated and compared residents who did and did not wear HPs at all, an area that has received less attention but is important if these devices are to have an effect on hip fracture incidence. The data derive from the Hip Impact Protection Project (HIP PRO), a randomized controlled clinical trial conducted by three clinical centers (Hebrew Rehabilitation Center, Boston, MA; University of Maryland, Baltimore, MD; Washington University, St Louis, MO) and a data coordinating center (Maryland Medical Research Institute, Baltimore, MD). Results of these analyses suggest how facility organization and leadership can increase adherence to HPs.
METHODS
Randomization, Eligibility, and Recruitment
HIP PRO corrected methodological limitations of other studies that randomized by facilities or by residents; instead, it randomized at the level of the hip, such that each resident had one protected and one non-protected hip. The administrators of eligible NHs agreed to this randomization, and the NH had to have at least 100 beds and be in proximity to a clinical center. Each NH was randomly selected to be a “right” or “left” sided facility, and all residents in that setting wore the HP on the same side. Doing so was assured by undergarments that had only one pocket to house the HP and which were clearly labeled to differentiate front from back. The first facility was enrolled October 2002 and data for these analyses were collected through October 2004.
Residents were eligible if they were 65 years of age or older; were long-stay; at least attempted to get out of the bed or chair or walk without human assistance in the past four weeks; and did not have a history of bilateral hip fractures or hip replacement surgery, a contagious disease necessitating isolation, pressure ulcers, blisters or skin tears over bony prominences that would be covered by the HP garment, hip circumference ≥ 49 inches, or staff recommendation not to enroll because of behaviors affecting adherence (e.g., not willing to wear undergarments). Power estimates to determine the efficacy of the HPs indicated a need to follow 546 residents. To obtain this number, residents who died, withdrew, or became ineligible (e.g., bedbound) were replaced. For these analyses, data from only those residents who were enrolled in the first nine months in each facility were used, to assure that the potential facility-level predictors collected at facility enrollment were timely.
Able residents provided their own consent and a responsible party provided consent for others while they provided assent. All residents participated in a two-week run-in trial to exclude those with poor adherence. During this time, research staff made six unannounced visits. If a resident was wearing the HP incorrectly at more than two visits, he/she was withdrawn. However, if the reason for non-adherence was staff or HP problems (e.g., no clean garments), an additional two-week run-in period was permitted after the problem was corrected.
All procedures were approved by the Institutional Review Boards of the Clinical Centers and the Coordinating Center. Further details about the design can be found elsewhere.8,24
Measures
Data included those related to adherence and characteristics of facilities and residents that were examined in other studies of HP adherence and NH outcomes.
Adherence
Adherence was determined by research staff observation. Residents were visited unannounced by research staff three times per week across all shifts and days of the week. If the protector was not being worn or not being worn correctly, the resident was considered non-adherent. Depending upon when they were enrolled, residents were observed for adherence for between 1-21 months (mean 11.0, S.D. 6.1).
Facility characteristics
Data related to facility characteristics were obtained from interviews with the administrator, director of nursing (DON), and research staff. Information related to demographic characteristics (bedsize, years in operation, proprietary status, chain affiliation, and case-mix); staffing (administrator and DON years in the facility; use of universal, specialized, and rotating workers who work on more than one unit; staffing ratio, vacancy, turnover and temporary staffing of the DON, registered/licensed nurses, and certified nursing assistant positions; and an overall nurse staffing ratio); policies and procedures, and their perception of hip protectors and related experience. In reference to policies and procedures, organizational leadership was related to administrator and DON attendance in meetings with professional and non-professional staff and the director of physical therapy; it combined Likert scales to create an overall meeting frequency ranging from 3-12. Administrative priorities for the administrator and DON were obtained by reviewing the rank ordering of 12 activities used in prior work.23 Those that were ranked most important by at ≥ 25% of respondents included “treating residents respectfully” and “being aware of resident's medical status”. For each respondent, the twelve rankings were collapsed into three categories, and analyses examined whether respect and medical status awareness were ranked among those of highest priority (top four items), middle priority (next four items), or lower priority (last four items). The final policy and procedure items related to the number of and participation in in-service trainings in the last quarter and whether or not a falls prevention program was in place.23 Perception of hip protectors related to the administrator's and DON's perceptions regarding the extent to which protectors prevent fractures and how residents feel about wearing protectors, with a summative score of 0-4. The percent of residents enrolled in the trial (overall and of those eligible) was calculated as a measure of the intensity of facility exposure. Administrators and DONs also reported on related experience in the context of previous research involvement in the past year. Finally, research staff evaluated environmental quality using the Therapeutic Environment Screening Survey25 which creates a scale ranging from 12-38. Research staff also reported on facility commitment to protector use based upon whether mechanisms were in place to assure adherence such as consequences for lack of use, staff commitment to protector use (scored 1-4), quality of interaction between research and facility staff (scored 1-4), the general working environment (scored 1-5), and the quality of care (the mean of seven items [alpha 0.93] scored 1-5 that assess to what extent the administrator and DON have respect from the staff, the staffing ratio, the frequency of toileting, the response time to residents' requests, the quality of communication between staff and residents, and overall staff morale).
Resident characteristics
Chart data provided information about demographic characteristics (age, gender, race, marital status and education); functional status (behavioral symptoms including verbally abusive, physically abusive, socially inappropriate/disruptive, and resistant to care; wandering; depressed, sad or anxious mood; continence of bladder and bowel; mobility; and history of falls; and health status (osteoporosis, dementia, and depression diagnosis, history of hip fracture, number of medications, medications for osteoporosis, and body mass index). Data also were obtained from interviews with residents regarding cognitive function using the Short Blessed Test (with a score ≥ 12 indicative of cognitive impairment, which corresponds to a score of 19 on the Mini Mental Status Examination); 26 and regarding psychosocial characteristics with an eight item fear of falling measure27 (scored 1-5), and a measure of perceived need for and benefit of the HP (scored 1-4). The care provider who knew the resident best reported on the family's frequency of visits. In addition, research staff reported on each resident's body image shape by selecting one of nine images modified from a National Heart, Lung, and Blood Institute study;28 these ratings correlated 0.72 (p<.001) with resident ratings, and because there were less missing data from research staff, their data were used in analyses.
Statistical Methods
Descriptive statistics included means, standard deviations, and percentages for categorical variables. Monthly percent adherence, used as the outcome in the models described below, was calculated for each resident as the number of research staff visits on which the resident was wearing the HP correctly, divided by the total number of visits for the month, with the resulting proportion multiplied by 100.
To select variables for the multivariate models, each facility- and resident-level characteristic was included in a model with only that variable as the predictor of adherence. Variables that were significantly related to adherence (p<0.05) were included in multivariate models. Multivariate models were constructed by including all significant variables from the bivariate models in the full, initial model and stepping non-significant (≥0.05) variables out one at a time in a downward fashion. No interactions were tested. Initial models were constructed with related variables (such as demographic characteristics) included in a model. Significant variables from those models then were included in a combined model in which all significant variables from all conceptual areas (e.g., demographic characteristics, staffing, policies and procedures, hip protectors and related experience, research staff ratings) were included. P-values less than 0.05 are considered to be significant in these models. Since this is an exploratory analysis, no adjustment for multiplicity of testing was made. All models were tested using mixed model methodology29 because of the inherent correlation with observations (resident months) and the inherent correlation within NHs. This is especially true when including both facility- and resident-level characteristics in the models. All analyses were performed using SAS (SAS Institute, Inc., Cary, NC).
RESULTS
Of the 35 NHs participating in this project, almost one-half were for profit (46%), and not chain-affiliated (53%); their average bed size was 182 (SD 120). A total of 7152 NH residents were screened for participation. Of these, 3816 (53%) were not eligible, the majority because they never attempted to stand up (n=1909). Of the 3336 who were eligible, 68% (n=2268) refused to participate, and another 26 did not enter the run-in period for reasons such as subsequent ineligibility or death. The remaining 1042 residents entered the run-in, 797 of whom entered the study within the first nine months of facility enrollment. Of these, 164 (20%) did not pass the run-in, 236 (30%) passed the run-in but later dropped out, and 397 (50%) remained in study until follow-up data collection was completed.
Comparisons of those who refused to participate, did not pass the run-in, and subsequently dropped out provide information on the characteristics of residents willing to wear HPs. Those who agreed to participate versus those who refused did not differ in terms of age, gender, race, or ethnicity. Those who did or did not pass the trial did not differ in terms of behavior or depression, but those who did not pass were significantly more likely to be continent; mobile; not to have fallen in the preceding six months; and less likely to have a dementia diagnosis or be taking osteoporosis medicines.
Adherence
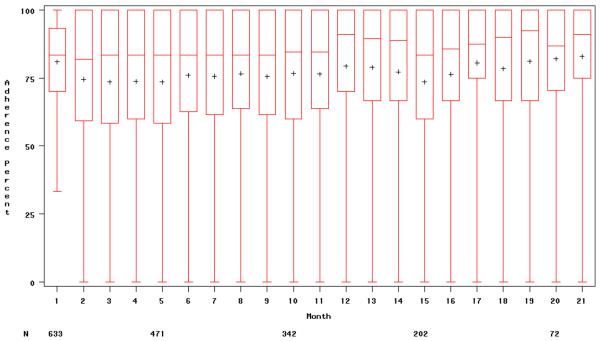
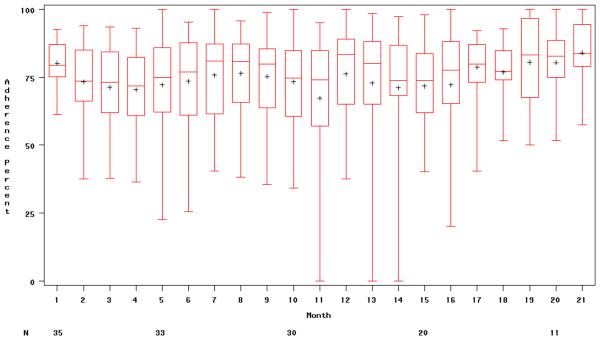
In total, 13,293 adherence observations were made of 633 subjects over 21 months. Figure 1 illustrates adherence by resident time in study (Figure 1a), and among NHs by NH time in study (Figure 1b). Figure 1a indicates that during each resident's first month of protector use, adherence averaged 81% (interquartile range 70-93%). Mean adherence remained at 75% or more, although the interquartile range was wider and extreme values lower after the residents' first month of participation. Across all months, adherence averaged 76% (range 0-100%; interquartile range 64-100%). Adherence in NHs by their own time in the study (Figure 1b) ranged between 0-100%, with an average of 78% (interquartile range 65-86%) and no significant change over time. Of note, the months in these figures cannot be compared, because, for example, a resident's first month in the study may not correspond to a facility's first month in the study due to rolling recruitment.
Figure 1.
Adherence by resident time in study (1a) and nursing home time in study (1b). The box indicates the interquartile range (25th-75th percentile); the plus sign inside of the interquartile range represents the mean; the line inside of the interquartile range represents the median; and the line extending from the box represents the extreme value.
Relationship of facility characteristics to adherence
Multivariate analyses comparing facility characteristics to adherence (see Table 2) found significant associations between the following variables and more adherence (p<.05): demographic characteristics of larger bed size, nonprofit status (i.e., adherence in non-profit facilities was 5.65% higher than in for-profit facilities), having fewer Medicaid residents, and not being affiliated with a chain (i.e., adherence was 5.8% higher in non-affiliated facilities); staffing characteristics of more use of rotating workers, a lower staffing ratio of professional nurses and paraprofessionals to number of residents, and more DON experience; policies and procedures including less organizational leadership (involvement in meetings with others), the DON prioritizing the need to treat residents respectfully (i.e., adherence was more than 15% higher compared to when respect was considered as least important), and a higher percent of nonprofessional staff attending in-service training; hip protector and related experience including fewer eligible residents enrolled and a history of both the administrator and DON being involved in research as opposed to only the DON; and research staff ratings of better environment quality, more RN commitment to protector use, better quality of interaction between the research and facility staff, and better quality of care.
Table 2.
Multivariate Relationship of Facility Characteristics to Adherencea
| Estimate | SE | P-value | |
|---|---|---|---|
| Demographics Characteristics (N=6522 observations) | |||
| Bedsize (per every 10 beds) | 0.20 | 0.04 | < 0.01 |
| Proprietary status, non-profit | 5.65 | 1.53 | < 0.01 |
| Case mix, percent of residents on Medicaid | −0.17 | 0.02 | < 0.01 |
| Affiliation , not chain-affiliated | 5.80 | 1.43 | < 0.01 |
| Staffing (N=4993 observations) | |||
| Percent rotating workers | 0.36 | 0.08 | < 0.01 |
| Nurses, registered and licensed (RN, LPN), Staffing ratio | −4.01 | 1.55 | <0.01 |
| Certified nursing assistants (CNA), Staffing ratio | −1.62 | 0.67 | 0.02 |
| DON, experience in facility | 0.03 | 0.01 | < 0.01 |
| Policies and Procedures (N=5700 observations) | |||
| Organizational leadership, Administrator index | −1.17 | 0.33 | < 0.01 |
| Organizational leadership, DON index | −1.29 | 0.38 | < 0.01 |
| Administrative priorities, DON | < 0.01 | ||
| Resident treated respectfully (reference = least important) | |||
| Somewhat important | 15.26 | 3.56 | < 0.01 |
| Most important | 15.05 | 3.11 | < 0.01 |
| In-service training last quarter, percent nonprofessionals attended | 0.19 | 0.04 | < 0.01 |
| Hip Protectors and Related Experience (N=6003 observations) | |||
| Percent of eligible residents enrolled in HIP PRO | −0.35 | 0.09 | <0.01 |
| Previous research involvement, past year (reference = both yes) | <0.01 | ||
| Administrator yes, DON no | 0.52 | 3.36 | 0.88 |
| Administrator no, DON yes | −13.74 | 3.35 | < 0.01 |
| Administrator and DON no | −3.10 | 2.32 | 0.18 |
| Research Staff Ratings (N=5781 observations) | |||
| Environmental quality (SCU-EQS score) | 0.41 | 0.13 | < 0.01 |
| Staff commitment to protector use (RN) | 3.05 | 1.11 | < 0.01 |
| Quality of interaction between research and facility staff | |||
| Facility staff approachable and responsive | 3.27 | 1.23 | < 0.01 |
| Quality of care | 3.96 | 1.15 | < 0.01 |
| Combined Demographic, Staffing, Policies/Procedures, Hip Protectors/Experience, and Staff Ratings (N=5496 observations) | |||
| Case mix, percent of residents on Medicaid | −0.10 | 0.03 | < 0.01 |
| Affiliation , not chain-affiliated | 6.73 | 1.67 | < 0.01 |
| Percent rotating workers | 0.47 | 0.09 | < 0.01 |
| Organizational leadership, Administrator index | −1.15 | 0.32 | < 0.01 |
| Administrative priorities, DON | 0.05 | ||
| Resident treated respectfully (reference = least important) | |||
| Somewhat important | 8.13 | 3.82 | 0.03 |
| Most important | 7.44 | 3.21 | 0.02 |
| In-service training last quarter, percent nonprofessionals attended | 0.17 | 0.03 | < 0.01 |
| Percent of eligible residents enrolled in HIP PRO | −0.40 | 0.08 | < 0.01 |
Only those variables significantly associated with adherence in multivariate models are shown; variables that were significant in bivariate models but not in multivariate models were: demographic characteristics (years in operation and percent of residents on Medicare); staffing (DON staffing ratio, RN turnover ratio, and overall staffing ratio); policies and procedures (percent attendance of professionals at in-service training, and having a falls prevention program); hip protectors (administrator and DON positive perception of hip protectors); and research staff ratings (facility, administrator, DON, and certified nursing assistant commitment to protector use, quality of interaction between research and facility staff, and general working environment).
The final section of Table 2 provides the data for variables that remained significantly related to adherence when all significant demographic characteristics, staffing characteristics, policies and procedures characteristics, HP and related experience characteristics, and research staff ratings were entered into a multivariate model. Facility characteristics related to more adherence included proportionately fewer residents on Medicaid, not being chain-affiliated (related to 6.73% more adherence), having more rotating workers, less administrator involvement in meetings, the DON prioritizing respect for resident (related to 7.44-8.13% more adherence), more in-service training attended by nonprofessionals, and fewer eligible residents enrolled in HIP PRO.
Relationship of resident characteristics to adherence
Multivariate analyses comparing resident characteristics to adherence (Table 3) found significant associations between the following variables and more adherence (p<.05): demographic characteristics of white race and being married; functional status characteristics of no cognitive impairment, wandering, no consistent depression, bladder incontinence, bowel continence, and not being in a wheelchair; and health status characteristics of having an osteoporosis diagnosis.
Table 3.
Multivariate Relationship of Resident Characteristics to Adherencea
| Demographic Characteristics (N=6639 observations) | Estimate | SE | P-value |
|---|---|---|---|
| Race, non-white | −10.17 | 1.94 | <0.01 |
| Marital status, married | 5.06 | 1.92 | <0.01 |
| Functional Status (N=6635 observations) | |||
| Cognitive impairment (≥ 12 on the Blessed Test) | −7.34 | 1.90 | <0.01 |
| Wandering (reference = none) | <0.01 | ||
| Less than daily | −3.87 | 2.10 | 0.07 |
| Daily | 4.01 | 2.10 | 0.06 |
| Depressed, sad, or anxious mood (reference= no mood indicators) | 0.02 | ||
| Indicators present, easily altered | 1.26 | 1.53 | 0.41 |
| Indicators present, not easily altered | −4.89 | 2.12 | 0.02 |
| Incontinent, bladder (reference = always continent) | 0.04 | ||
| Sometimes incontinent | 5.07 | 2.04 | 0.01 |
| Frequently or always incontinent | 1.62 | 2.24 | 0.47 |
| Incontinent, bowel (reference = always continent) | 0.01 | ||
| Sometimes incontinent | −2.07 | 2.08 | 0.32 |
| Frequently or always incontinent | −6.30 | 2.09 | 0.01 |
| Mobility (reference = independent) | < 0.01 | ||
| Supervision or limited assistance | 0.13 | 1.94 | 0.95 |
| Extensive assistance or total dependence | 4.90 | 5.24 | 0.35 |
| Wheelchair | −7.08 | 1.61 | < 0.01 |
| Activity did not occur | −5.90 | 7.78 | 0.45 |
| Health Status (N=6651 observations) | |||
| Osteoporosis diagnosis | 5.71 | 1.74 | < 0.01 |
| Combined Demographic, Functional and Health Status (N=6618 observations) | |||
| Race, non-white | −8.76 | 1.92 | < 0.01 |
| Cognitive impairment (≥ 12 on the Blessed Test) | −6.63 | 1.87 | < 0.01 |
| Wandering (reference = none) | < 0.01 | ||
| Less than daily | −2.59 | 2.08 | 0.21 |
| Daily | 5.09 | 2.08 | 0.01 |
| Depressed, sad, or anxious mood (reference= no mood indicators) | 0.02 | ||
| Indicators present, easily altered | 0.17 | 1.52 | 0.91 |
| Indicators present, not easily altered | −5.40 | 2.11 | 0.01 |
| Incontinent, bladder (reference = always continent) | 0.02 | ||
| Sometimes incontinent | 5.44 | 2.00 | < 0.01 |
| Frequently or always incontinent | 1.73 | 2.20 | 0.43 |
| Incontinent, bowel (reference = always continent) | 0.02 | ||
| Sometimes incontinent | −2.64 | 2.05 | 0.20 |
| Frequently or always incontinent | −5.94 | 2.06 | < 0.01 |
| Mobility (reference = independent) | < 0.01 | ||
| Supervision or limited assistance | −0.28 | 1.91 | 0.88 |
| Extensive assistance or total dependence | 2.21 | 5.16 | 0.67 |
| Wheelchair | −7.08 | 1.59 | < 0.01 |
| Activity did not occur | −4.74 | 7.65 | 0.54 |
| Osteoporosis diagnosis | 4.78 | 1.67 | < 0.01 |
Only those variables significantly associated with adherence in multivariate models are shown; variables that were significant in bivariate models but not in multivariate models were: health status (taking medications for osteoporosis).
The final section of Table 3 provides the data for the variables that remained significantly related to adherence when all significant demographic characteristics, functional status characteristics, and health status characteristics were entered into the multivariate model. Characteristics associated with more adherence include white race (related to 8.76% more adherence), no cognitive impairment (6.63% more adherence), daily wandering (5.09%), no consistent depression (5.4%), occasional bladder incontinence (5.44%), bowel continence, not being in a wheelchair (7.08%), and having an osteoporosis diagnosis (4.78%).
Relationship of facility and resident characteristics to adherence
Table 4 provides the data for the variables that remained significantly related to adherence when those from the combined facility and combined resident models were included in one multivariate analysis. Characteristics related to more adherence were fewer residents on Medicaid, not being chain-affiliated, have proportionately more rotating workers, less administrator involvement in meetings, more in-service training attended by nonprofessionals, and fewer eligible residents enrolled in HIP PRO; and residents who were cognitively intact, wandered on a daily basis, were not consistently depressed, had occasional bowel incontinence, and were not in a wheelchair.
Table 4.
Multivariate Relationship of Facility and Resident Characteristics to Adherence (N=5489 observations)
| Estimate | SE | P-value | |
|---|---|---|---|
| Facility Characteristics | |||
| Case mix, percent of residents on Medicaid | −0.10 | 0.03 | < 0.01 |
| Affiliation , not chain-affiliated | 5.05 | 1.66 | < 0.01 |
| Percent rotating workers | 0.36 | 0.08 | < 0.01 |
| Organizational leadership, Administrator | −1.06 | 0.30 | < 0.01 |
| In-service training last quarter, percent nonprofessionals attended | 0.17 | 0.03 | < 0.01 |
| Percent of eligible residents enrolled in HIP PRO | −0.47 | 0.08 | < 0.01 |
| Resident Characteristics | |||
| Cognitive impairment (≥ 12 on the Blessed Test) | −4.05 | 1.95 | 0.04 |
| Wandering (reference = none) | < 0.01 | ||
| Less than daily | −3.39 | 2.19 | 0.12 |
| Daily | 5.06 | 2.25 | 0.03 |
| Depressed, sad, or anxious mood (reference= no mood indicators) | < 0.01 | ||
| Indicators present, easily altered | 1.69 | 1.61 | 0.29 |
| Indicators present, not easily altered | −6.90 | 2.17 | < 0.01 |
| Incontinent, bladder (reference = always continent) | 0.01 | ||
| Sometimes incontinent | 1.78 | 1.99 | 0.08 |
| Frequently or always incontinent | −3.14 | 1.80 | 0.37 |
| Mobility (reference = independent) | < 0.01 | ||
| Supervision or limited assistance | 1.43 | 2.03 | 0.48 |
| Extensive assistance or total dependence | 3.24 | 5.27 | 0.54 |
| Wheelchair | −4.69 | 1.66 | < 0.01 |
| Activity did not occur | −5.48 | 7.57 | 0.47 |
DISCUSSION
This, the largest study of its type in the U.S., is the first to broadly examine the relationship of NH characteristics to HP adherence. It is of importance because it can help explain rates of adherence ranging from 20-92%,10 and provide guidance for organizational change to promote HP use. The final analytic model that combined significant facility- and resident-level characteristics identified six facility characteristics related to more adherence. One unfortunate finding is that adherence was lower in facilities with a higher Medicaid case-mix. This finding is consistent with reports of fewer resources and more health-related deficiencies in NHs with more Medicaid residents.30 Facilities with higher Medicaid case-mix also are more likely to serve African American residents, which may explain why this resident-level variable became non-significant in the combined model. Thus, it is possible that racial and socioeconomic disparities in adherence are less related to resident-level characteristics than to health system factors, and this is the first study to document the extension of that disparity to the use of HPs.
Not surprisingly, more paraprofessional training related to adherence, and NHs that better prepare staff for their work, in general, are likely to evidence higher adherence. Other studies also have demonstrated the positive effect of training on falls and hip fracture prevention.31,32 This study also found that having more rotating workers is related to more adherence. As such, it is the third study to run counter to prevailing wisdom in suggesting that permanent (non-rotating) staffing is not always beneficial to residents.33,34 In the case of adherence to HPs, it may be that new staff are especially vigilant to resident care plans due to their unfamiliarity with the resident. While the conclusions do not necessarily suggest the use of rotating workers, they do suggest that NHs focus on more frequent review of and attention to care plans. These two findings, related to training and diligence to care plans, may explain in part why adherence was higher in facilities in which administrators were less involved in meetings; that is, it may be that administrators are less involved when other procedures are in place to assure quality care. In support of this conclusion, administrators were less involved in meetings in NHs that had a falls prevention program (Pearsons r = −.39), commitment to HPs (r = −.37 to −.54), and better quality of care (r = −.63), and more involved in settings that evidenced more DON and RN staff turnover (r = .48 and .38). This interpretation provides hypotheses for further study.
The more eligible residents who were wearing HPs, the less the adherence. This finding persisted when resident-level characteristics were added to the model, suggesting it was the sheer number of residents, rather than their dependence, that related to adherence. One interpretation of this finding relates to the time required for staff to dress residents in the HP. Given the amount of care required by NH residents, the workforce shortages,35 and that over-burdened staff relegate optional tasks to a secondary status,36 these findings suggest three avenues of action. The first is to bolster the workforce, such as to involve families in promoting HP use. Indeed, family involvement is related to increased adherence.18 The second is to provide staff education about the risks and consequences of hip fracture. The third is to target the use of HPs to those most in need, and emphasize their use as an integral component of the care plan.
Finally, non-profit ownership and not being affiliated with a chain were related to almost 6% more adherence. There is abundant evidence that for-profit status is related to poorer quality care and outcomes23,37 and that the majority of for-profit NHs are affiliated with a chain while only a minority of non-profit NHs have a chain affiliation.38 Thus, findings from the current study add to what has been written about for-profit NHs by extending it to adherence with care practices.
This study also demonstrated that with careful attention to adherence, rates averaging 75% or more can be sustained for as long as two years. This figure is markedly higher than other studies (e.g., Kurrle obtained 53% adherence).13 Of course, this study used a run-in period which excluded those with poor adherence; also, as an efficacy study, neither this study nor others can assure that the observed adherence rates will be achieved in daily practice. On the other hand, being a research project and not a standard of care may have adversely affected adherence. It is in this context that this study provides guidance as to the types of facilities in which special efforts will be necessary to maximize the use of HPs – NHs that have a higher Medicaid and African American case-mix, less of a culture of staff training, and staff who are more burdened and may not be able to attend as closely as desired to resident care plans. In instances when staff cannot attend closely to all residents who might benefit from HPs, it is suggested that their use be targeted to those residents who are most likely to use them.10,18
Residents who passed the two-week run-in period were significantly more likely to be incontinent and not independently mobile; to have fallen in the preceding six months; and to have a dementia diagnosis or be taking osteoporosis medicines. However, for those who continued in the study, in models adjusted for resident status, having cognitive impairment was related to lower adherence. Other studies have found less39 and more16,18 adherence among those who are cognitively impaired; and less10 and more9,14 adherence among those who are incontinent. One study found a significant relationship between depression and lower adherence,18 although this was not significant in adjusted analyses. However, comparisons across studies are complicated by the fact that not all controlled for similar characteristics or defined variables similarly. There is evidence, however, that residents at risk of fracture are more likely to be adherent.9,10 In light of conflicting resident-level findings and facility characteristics that suggest a need to target HP use, it may be that the best approach is one that is individualized: offer HPs to all residents who are at risk, and encourage their use in residents who are willing to wear them. The success of this effort in reference to adherence should be evident by twelve weeks time.40 This focus on individualized care is consistent with the importance of treating residents respectfully, which was significantly related to adherence until the fully adjusted model was run.
Despite being the only study to examine facility-level predictors of adherence to HPs in U.S. NHs, this project has limitations. The most notable is that the HP was one-sided, raising concerns as to generalizability. Also, the project used a run-in period that results in higher adherence among those who remain in the study; similarly, research staff visited frequently to encourage adherence. Further, while a large number of facility- and resident-level characteristics were studied, not all were sufficiently powered for analyses. Still, findings that adherence is lower in NHs that have more Medicaid case-mix and African American residents and less training for certified nursing assistants, and in which staff are more burdened, can explain differences in adherence across studies and indicate settings in which special efforts are needed to encourage adherence with HPs to decrease fractures.
Table 1.
Characteristics of Eligible Residents Who Refused to Participate, Did not Pass the Trial, and Dropped Out, Through Nine Months Post Facility Randomizationa
| Refused (N=2268) Number (%) or Mean (SD) |
Agreed to Participate (N=797) | |||
|---|---|---|---|---|
| Did Not Pass Trial (N=164) Number (%) or Mean (SD) |
Passed Trial (N=633) | |||
| Dropped Out (N=236) Number (%) or Mean (SD) |
Did Not Drop Out (N=397) Number (%) or Mean (SD) |
|||
| Demographic Characteristics | ||||
| Age (mean, SD) | 85.2 (8.0) | 85.5 (7.1) | 85.9 (7.4) | 85.0 (7.3) |
| Gender, male | 492 (21.7) | 32 (19.5) | 52 (22.0) | 70 (17.6) |
| Race, non-white | 123 (11.6) | 22 (13.4) | 40 (17.0) | 51 (12.9) |
| Ethnicity, Hispanic | 11 (0.8) | 1 (0.6) | 3 (1.3) | 3 (0.8) |
| Marital status, not married | 140 (88.6) | 205 (87.6) | 339 (85.6) | |
| Functional Status | ||||
| No cognitive impairment (≥ 12 on the Blessed Test) | 38 (23.5) | 43 (18.3) | 70 (17.7) | |
| Aggressive behavior scale | 0.6 (1.5) | 0.7 (1.4) | 0.6 (1.3) | |
| Do not wander | 128 (81.0) | 180 (76.6) | 293 (73.8) | |
| No depressive indicators | 96 (60.8) | 138 (58.7) | 228 (57.4) | |
| Continent of bladder | 69 (43.7) | 62 (26.4) | 104 (26.2)*** | |
| Continent of bowel | 98 (62.0) | 113 (48.1) | 174 (43.8)*** | |
| Independently mobile | 66 (41.8) | 60 (25.5) | 120 (30.2)** | |
| No falls in last six months | 96 (61.2) | 113 (48.1) | 180 (45.3)* | |
| Health Status | ||||
| History of hip fracture | 10 (6.4) | 14 (6.0) | 29 (7.3) | |
| Osteoporosis diagnosis | 31 (19.8) | 39 (16.6) | 75 (18.9) | |
| Alzheimer's disease, dementia diagnosis | 89 (56.7) | 158 (67.2) | 274 (69.0)* | |
| Depression diagnosis | 67 (42.4) | 99 (42.1) | 179 (45.1) | |
| Number of medications | 8.8 (4.0) | 8.6 (3.6) | 8.5 (3.9) | |
| Taking medications for osteoporosis | 11 (7.0) | 27 (11.5) | 58 (14.7)* | |
| Body mass index | 25.0 (4.6) | 24.2 (4.4) | 24.8 (4.6) | |
Number missing: 4 (cognitive impairment); 7 (ethnicity, wandering, depressive indicators and depression diagnosis, incontinence, mobility); 8 (falls, osteoporosis diagnosis, Alzheimer's diagnosis, taking osteoporosis medications); 9 (marital status, history of hip fracture). Percents are column percents; using gender as an example, 21.7% of those who refused were male; 19.5% of those who did not pass the trial were male, 22.0% of those who dropped out were male, and 17.6% of those who did not drop out were male.
p <.05;
p < .01;
p<0.001 for comparisons across all groups.
ACKNOWLEDGEMENT
Funded by National Institutes of Health, National Institute on Aging grant R01 AG018461 and supported in part by the Lawrence J. and Anne Cable Rubenstein Charitable Foundation.
The authors thank Linda Ball, PhD, Washington University School of Medicine, St. Louis, MO, for her insights related to variable construction. They also thank the project coordinators and data collectors across all three clinical centers and the staff of the data coordinating center whose diligent efforts allowed this work to be conducted.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflict of Interest: The authors have no financial or personal conflicts of interest related to the work reported in this manuscript.
REFERENCES
- 1.US Department of Health and Human Services . Hospital Inpatient Statistics 1996-1999. Agency for Health Care Policy and Research; Rockville, MD: 1999. AHCPR Publication 99-0034. [Google Scholar]
- 2.Magaziner J, Fredman L, Hawkes W, et al. Changes in functional status attributable to hip fracture: a comparison of hip fracture patents to community-dwelling aged. Am J Epidemiol. 2003;157:1023–1031. doi: 10.1093/aje/kwg081. [DOI] [PubMed] [Google Scholar]
- 3.Magaziner J, Lydick E, Hawkes W, et al. Excess mortality attributable to hip fracture in white women aged 70 years and older. Am J Public Health. 1997;87(10):1630–6. doi: 10.2105/ajph.87.10.1630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zimmerman S, Girman CJ, Buie VC, et al. The prevalence of osteoporosis in nursing home residents. Osteoporos Int. 1999;9:151–157. doi: 10.1007/s001980050129. [DOI] [PubMed] [Google Scholar]
- 5.Ooms ME, Vlasman P, Lips P, et al. The incidence of hip fractures in independent and institutionalized elderly people. Osteoporos Int. 1994;4:6–10. doi: 10.1007/BF02352254. [DOI] [PubMed] [Google Scholar]
- 6.Rudman ID, Rudman D. High rate of fractures for men in nursing homes. Am J Phys Med Rehabil. 1989;68:205. doi: 10.1097/00002060-198902000-00002. [DOI] [PubMed] [Google Scholar]
- 7.Parker MJ, Gillespie WJ, Gillespie LD. Hip protectors for preventing hip fractures in older people. (Art. No.: CD001255).Cochrane Database of Systematic Reviews. 2005;(3) doi: 10.1002/14651858.CD001255.pub3. DOI: 10.1002/14651858.CD001255.pub3. [DOI] [PubMed] [Google Scholar]
- 8.BLINDED FOR REVIEW.
- 9.Cryer C, Knox A, Stevenson E. Factors associated with hip protector adherence among older people in residential care. Injury Prevention. 2008;14:24–29. doi: 10.1136/ip.2007.016899. [DOI] [PubMed] [Google Scholar]
- 10.van Schoor NM, Deville WL, Bouter LM, et al. Acceptance and compliance with external hip protectors: a system review of the literature. Osteoporosis Int. 2002;13:917–924. doi: 10.1007/s001980200128. [DOI] [PubMed] [Google Scholar]
- 11.Myers AH, Michelson JD, Van Natta M, et al. Prevention of hip fractures in the elderly: receptivity to protective garments. Arch Gerontol Geriatr. 1995;21:179–189. doi: 10.1016/0167-4943(95)00637-z. [DOI] [PubMed] [Google Scholar]
- 12.Cameron ID, Quine S. External hip protectors: likely non-compliance among high risk elderly people living in the community. Arch Geront Geriatr. 1994;19:273–281. doi: 10.1016/0167-4943(94)00573-7. [DOI] [PubMed] [Google Scholar]
- 13.Kurrle SE, Cameron ID, Quine S. Predictors of adherence with the recommended use of hip protectors. Journal of Gerontology Medical Science. 2004;59:958–961. doi: 10.1093/gerona/59.9.m958. [DOI] [PubMed] [Google Scholar]
- 14.Warnke A, Meyer G, Bender R, et al. Predictors of adherence to the use of hip protectors in nursing home residents. JAGS. 2004;52:340–345. doi: 10.1111/j.1532-5415.2004.52103.x. [DOI] [PubMed] [Google Scholar]
- 15.Lauritzen JB, Petersen MM, Lund B. Effect of external hip protectors on hip fractures. The Lancet. 1993;34:11–13. doi: 10.1016/0140-6736(93)92480-h. [DOI] [PubMed] [Google Scholar]
- 16.O'Halloran PD, Murray LJ, Cran GW, et al. The effect of type of hip protector and resident characteristics on adherence to use of hip protectors in nursing and residential homes – an exploratory study. Int J Nurs Studies. 2005;42:387–397. doi: 10.1016/j.ijnurstu.2004.09.010. [DOI] [PubMed] [Google Scholar]
- 17.Burl JB, Centola J, Bonner A, et al. Hip protector compliance: a 13-month study on factors and cost in a long-term care facility. J Am Med Dir Assoc. 2003;4:245–250. doi: 10.1097/01.JAM.0000083382.28795.9B. [DOI] [PubMed] [Google Scholar]
- 18.Honkanen LA, Monaghan N, Reid MC, et al. Can hip protector use in the nursing home be predicted? JAGS. 2007;55:350–356. doi: 10.1111/j.1532-5415.2007.01015.x. [DOI] [PubMed] [Google Scholar]
- 19.Statehealthfacts.org. United States: Total Number of Certified Nursing Facilities. 2006 (online). Available at: http://www.statehealthfacts.org/profileind.jsp?ind=411&cat=8&rgn=1. Accessed July 12, 2008.
- 20.Statehealthfacts.org. United States: Certified Nursing Facility Beds. 2006 (online). Available at: http://www.statehealthfacts.org/profileind.jsp?ind=413&cat=8&rgn=1. Accessed July 12, 2008.
- 21.Statehealthfacts.org. United States: Total Number of Residents in Certified Nursing Facilities. 2006 (online). Available at: http://www.statehealthfacts.org/profileind.jsp?rgn=1&cat=8&ind=408. Accessed July 12, 2008.
- 22.Zimmerman S, Gruber-Baldini AL, Hebel JR, et al. Nursing home characteristics related to Medicare costs for residents with and without dementia. Am J Alzheimers Dis Other Demen. 2008;(1):57–65. doi: 10.1177/1533317507308778. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Zimmerman S, Gruber-Baldini AL, Hebel JR, et al. Nursing home facility risk factors for infection and hospitalization: importance of registered nurse turnover, administration, and social factors. J Am Geriatr Soc. 2002;50(12):1987–95. doi: 10.1046/j.1532-5415.2002.50610.x. [DOI] [PubMed] [Google Scholar]
- 24.BLINDED FOR REVIEW.
- 25.Sloane PD, Mitchell CM, Weisman G, et al. The therapeutic environment screening survey for nursing homes (TESS-NH): an observational instrument for assessing the physical environment of institutional settings for persons with dementia. Journal of Gerontology Social Science. 2002;57:69–78. doi: 10.1093/geronb/57.2.s69. [DOI] [PubMed] [Google Scholar]
- 26.Thal LJ, Grundman M, Golden R. Alzheimer's disease: a correlational analysis of the Blessed Information-Memory-Concentration Test and the Mini-Mental State Exam. Neurology. 1986;36(2):262–264. doi: 10.1212/wnl.36.2.262. [DOI] [PubMed] [Google Scholar]
- 27.Lach H, Ball L, Birge S. Validation of a measure of fear of falling for nursing home residents. The Gerontologist. 2002;421(1):171. [Google Scholar]
- 28.The National Heart, Lung, and Blood Growth and Health Study Research Group Obesity and cardiovascular risk factors in black and white girls: the NHLBI growth and health study. Amer. Journal of Public Health. 1992;82(12):1613–1620. doi: 10.2105/ajph.82.12.1613. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Laird NM, Ware JH. Random-effects models for longitudinal data. Biometrics. 1982;38(4):963–974. [PubMed] [Google Scholar]
- 30.Mor V, Zinn J, Angelelli J, et al. Driven to tiers: socioeconomic and racial disparities in the quality of nursing home care. Milbank Q. 2004;82(2):227–256. doi: 10.1111/j.0887-378X.2004.00309.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Cox H, Puffer S, Morton V, et al. Educating nursing home staff on fracture prevention: a cluster randomized trial. Age Ageing. 2008;37(2):167–172. doi: 10.1093/ageing/afm168. [DOI] [PubMed] [Google Scholar]
- 32.Jensen J, Lundin-Olsson L, Nyberg L, et al. Fall and injury prevention in older people living in residential care facilities. A cluster randomized trial. Ann Intern Med. 2002;136(10):733–741. doi: 10.7326/0003-4819-136-10-200205210-00008. [DOI] [PubMed] [Google Scholar]
- 33.Zimmerman S, Sloane PD, Williams CS, et al. Dementia care and quality of life in assisted living and nursing homes. The Gerontologist. 2005;45:133–146. doi: 10.1093/geront/45.suppl_1.133. [DOI] [PubMed] [Google Scholar]
- 34.Burgio LD, Fisher SE, Fairchild JK, et al. Quality of care in the nursing home: effects of staff assignment and work shift. The Gerontologist. 2004;44:368–377. doi: 10.1093/geront/44.3.368. [DOI] [PubMed] [Google Scholar]
- 35.Stearns SC, D'Arcy LP. Staying the course: facility and professional retention among nursing assistants in nursing homes. G Gerontol B Psychol Sci Soc Sci. 2008;63(3):113–121. doi: 10.1093/geronb/63.3.s113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Hartig MT. Expert nursing assistant care activities. West J Nurs Res. 1998;20(5):584–601. doi: 10.1177/019394599802000506. [DOI] [PubMed] [Google Scholar]
- 37.Spector WD, Selden TM, Cohen JW. The impact of ownership type on nursing home outcomes. Health Econ. 1998;7:639–653. doi: 10.1002/(sici)1099-1050(1998110)7:7<639::aid-hec373>3.0.co;2-0. [DOI] [PubMed] [Google Scholar]
- 38.Rhoades JA, Potter DE, Krauss NA. Characteristics of nursing homes in 1996. Abstr Book Assoc Health Serv Res Meet. 1997;14:303–4. Available at: http://gateway.nlm.nih.gov/MeetingAbstracts/ma?f=102233852.html. [Google Scholar]
- 39.Chan DK, Hillier G, Coorre M, et al. Effectiveness and acceptability of a newly designed hip protector: a pilot study. Archives of Gerontoloty and Geriatrics. 2000;30:25–34. doi: 10.1016/s0167-4943(99)00048-5. [DOI] [PubMed] [Google Scholar]
- 40.Villar MT, Hill P, Inskip H, et al. Will elderly rest home residents wear hip protectors? Age Ageing. 1998;27(2):195–198. doi: 10.1093/ageing/27.2.195. [DOI] [PubMed] [Google Scholar]