Abstract
Background
In spite of consistent evidence to suggest that being more physically active is associated with enhanced quality of life (QOL), there have been remarkably few attempts to determine the possible underlying mechanisms in this relationship.
Purpose
To prospectively examine the roles played by self-efficacy and physical and mental health status in the physical activity and quality of life relationship in older women.
Method
Older women (M age = 68.12 years) completed measures of physical activity, self-efficacy relative to balance, mental and physical health status, and global QOL at baseline (N = 249) and 24-month follow-up (N = 217). Demographics and general health information were assessed at baseline. A panel analysis within a covariance modeling framework was used to analyze the data.
Results
Analyses indicated that changes in physical activity over time were associated with residual changes in self-efficacy. Changes in self-efficacy were significantly associated with residual changes in physical and mental health status. Only changes in mental health status were significantly related to residual changes in global QOL.
Conclusion
Results from this study support the role of self-efficacy in the relationship between physical activity and QOL. Future physical activity promotion programs should include strategies to enhance self-efficacy for physical activity to be most effective for this population.
INTRODUCTION
A number of recent reviews in both the gerontological and the behavioral medicine literature have suggested a consistent association between physical activity and quality of life (QOL) in older adults (1–3). This relationship appears to hold across a broad spectrum of measures that have been used to represent the conceptualization of QOL (2). One approach to understanding QOL determinants is to treat QOL as a multidimensional or umbrella construct under which such dimensions as physical, social, psychological, and spiritual well-being may reside. Consistent with this perspective, Stewart and King (4) have conceptualized QOL as two broad categories, function and well-being, reflecting the framework provided by the Medical Outcomes Study (5). This framework is the fundamental basis for Health-Related Quality of Life (HRQL).
Using HRQL to conceptualize QOL has been the primary and accepted approach in the biomedical and behavioral medicine literature. However, the earlier social psychological literature would suggest that QOL as a global construct, rather than reflecting health status constructs, is represented by an overall satisfaction, or happiness, with one’s life (6,7). Physical functioning and physical health status variables are more proximal indicators of overall QOL (8,9,10).
Diener and his colleagues (11,12) have suggested that QOL reflects a “cognitive judgment of satisfaction with one’s life,” a perspective also taken by Rejeski and Mihalko (3). This approach permits comparative judgments, places importance on cognitive assessments, and has implications for theory testing and development (3). Indeed, if one adopts this approach, indicators such as physical and mental health status should be considered proximal QOL outcomes through which physical activity influences overall QOL (9). In a recent report, McAuley and his colleagues (13) presented evidence to support such a position. They argued that self-efficacy, the central component of social cognitive theory (14), has been consistently shown to be both a determinant and consequence of physical activity participation (15). Higher levels of self-efficacy have also been associated with a number of physical and mental health outcomes (14). In their cross-sectional analysis, McAuley et al.(13) hypothesized that physical activity initially influenced self-efficacy which, in turn, was associated with elements of mental and physical health status that were directly associated with satisfaction with life; a global measure of QOL. These hypotheses were supported and initially significant bivariate relationships between physical activity and health status and satisfaction with life were all rendered non-significant after controlling for the influence of self-efficacy. Thus, it would appear that a mediating role exists for self-efficacy in the physical activity-QOL relationship.
In their examinations of the cross-sectional relationships among physical activity, efficacy, health status, and global QOL, McAuley et al.(13) reported that the direction and strength of relationships were unaffected by important demographic variables such as age, race, income, education, and chronic health conditions. However, it is possible that such influences exert more explanatory power across time. For example, rates of sedentary behavior are higher among those of lower socioeconomic status (SES) (16) and lower SES neighborhoods have been reported to have significantly fewer facilities for physical activity (17). Finally, it is well-established that physical activity levels among minority populations are significantly less than those of their white counterparts (18), and Schutzer and Graves (19) have noted that chronic health conditions are associated with a sedentary lifestyle. Although these factors all reside outside the model hypothesized by McAuley et al. (13), it is important to determine whether they influence model relationships across time.
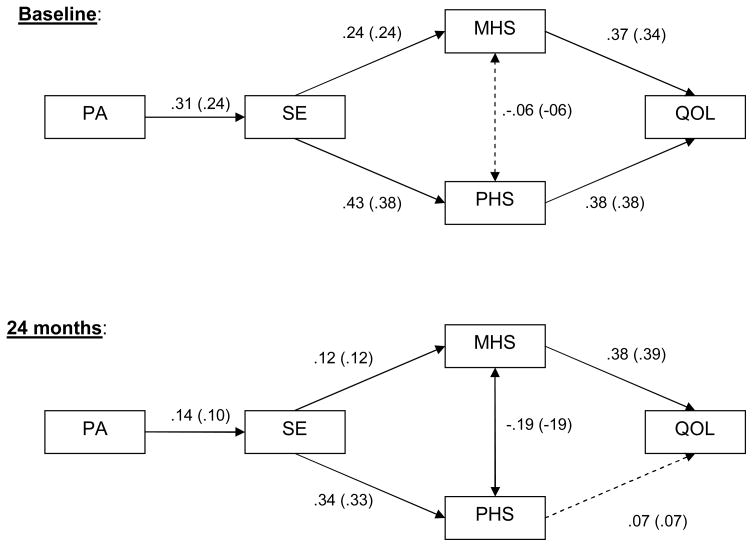
The present study further tested the model of physical activity and QOL proposed by McAuley et al. (13) in a 24-month prospective panel design in order to determine whether changes in the model constructs were related, as hypothesized, over time. In essence, it was hypothesized in the present study that decreases in physical activity across a 24-month period would be associated with decreases in self-efficacy. In turn, these changes in self-efficacy would be associated with changes in physical and mental health status, which would be directly related to changes in global QOL, as represented by satisfaction with life. These hypothesized relationships are depicted in Figure 1. Furthermore, we were interested in determining whether demographic factors and the presence of chronic health conditions influenced the hypothesized relationships.
Figure 1.
Panel model of relationships between physical activity, self-efficacy, mental and physical health status, and quality of life over time. Values in parentheses represent relationships after controlling for age, income, race, education, and chronic health conditions. Dashed lines indicate non-significant paths. Relationships at 24 months reflect changes over time. PA = physical activity; SE = self-efficacy; MHS = mental health status; PHS= physical health status; QOL = quality of life.
METHODS
Participants and Recruitment
Data were collected from an initial sample of 249 older (M age = 68.12 years, range 59–84 years) women at baseline of a prospective study beginning in 2002–2003, with 217 women available for follow-up data collection at 24 months in 2004–2005 (86.3% of total sample). All study procedures were approved by a University Institutional Review Board and each participant completed a written informed consent prior to study entry. Reasons for attrition at follow-up included personal illness/surgery/deceased (n = 14; 5.6%), lack of interest/time (n = 10; 4.0%), loss of contact or moved (n = 7; 2.9%), and family illness (n = 2; < 1.0%). Drop-outs were more likely to be older and African-American (p < .05). Study inclusion criteria, recruitment methods, and baseline characteristics have been reported elsewhere (20), as have health conditions at baseline and 24 months (21).
Measures
Demographic and health information
Information relative to age, race, education, and income, as well as health history data were collected by questionnaire. From this latter measure, an index of chronic health conditions was computed to reflect whether or not participants had cardiovascular disease, pulmonary disease, functional impairment of the musculoskeletal system, hypertension, or diabetes. Responses (1 for “Yes” and 0 for “No”) were aggregated to give a score ranging from 0–5.
Physical activity
To measure physical activity we used the Physical Activity Scale for the Elderly (PASE) (22), a valid and reliable self-report measure frequently used to assess physical activity in older adults (23,24). The PASE assesses activity counts based upon the frequency, duration, and metabolic equivalent value of self-reported activity.
Self-Efficacy
Although McAuley et al. (13), used measures of efficacy relative to physical activity and walking, we were interested in assessing self-efficacy relative to having control over one’s environment. As we age, limitations are imposed on instrumental activities necessary to lead an independent life such as negotiating stairs, avoiding falls, ambulating in crowded environments, and getting in and out of automobiles. Becoming or staying more active is likely to enhance such capabilities and being more efficacious in this regard should be associated with less fear and anxiety and better physical functioning. Thus, we used the Activity-Specific Balance scale (ABC) (25) to assess self-efficacy. This 16-item scale is measured on a 0 to 100% confidence scale; item ratings are summed and divided by the total number of items in the scale, resulting in a maximum possible efficacy score of 100. Validation work by Powell and Myers (25) indicates that this scale has adequate internal consistency, reliability and sensitivity for assessing balance confidence among high functioning elderly. Internal consistency for the ABC was excellent at both measurement points (α > .90).
Health Status
Physical and mental health status was measured by the 12-Item Short Form Survey (SF-12) (26), a shortened version of the SF-36 Health Survey. The SF-36 is a 36-item scale developed to assess health functioning in large-scale studies (27). It contains eight scales (Physical Functioning, Role-Physical, Bodily Pain, General Health, Vitality, Social Functioning, Role-Emotional, and Mental Health) that are organized in a hierarchical manner to form summary measures of Physical and Mental Health. Each of the eight scales has been found to possess adequate reliability and validity across a number of studies and populations (26). The SF-12 provides a 12-item representative sampling of the content of the 8 health concepts and the various operational definitions of those concepts, including what respondents are able to do, how they feel, and how they evaluate their health status.
Quality of Life
The Satisfaction with Life Scale (SWLS) (28), a 5-item measure developed to assess life satisfaction in various age groups, was used to measure overall QOL. Each scale item is rated on a 7-point scale from strongly disagree (1) to strongly agree (7), with higher scores representing greater life satisfaction. In a review of SWLS research, Pavot and Diener (12) suggested that the measure successfully detects change in life satisfaction over time and the course of clinical interventions. The SWLS has demonstrated acceptable internal reliability and validity in older populations (28,29). Internal consistencies at baseline and follow-up in the present study were excellent (αs > .90).
Procedures
After telephone screening and study entry, participants were scheduled for a laboratory appointment during which they completed an approved Institutional Review Board written informed consent and all questionnaires including demographics, general health information, physical activity, self-efficacy, health status, and QOL. At 24-month follow-up, participants were once again contacted by telephone and upon assenting to continue participation, were scheduled to visit the laboratory and go through the same set of procedures. All participants were paid $15 for their completion of all measures, and transportation was provided for those unable to secure their own mode of travel to the laboratory.
Data Analysis
In order to examine the hypothesized relations between physical activity, self-efficacy, health status, and quality of life, a panel analysis within a covariance modeling framework was conducted. Panel analysis is a useful analytic procedure for testing theoretical relationships among constructs across time (30). As an example, in this model (see Figure 1), the relationship between mental health status and global QOL can be examined at time one (i.e., baseline) and due to repeated observations, it is possible to examine the relationship between changes in mental health status and changes in QOL, that are independent of the baseline relationship and other variables in the model. With 249 participants enrolled at baseline and 217 at 24-month follow-up and therefore the presence of missing data, the full-information maximum likelihood (FIML) estimator feature in Mplus V4.1 (31) was used. The FIML estimator is well documented as providing both accurate parameter estimates and fit indices with simulated missing data (32–34). Preliminary analyses of the data were conducted to confirm the missing at random (MAR) assumption therefore justifying use of FIML estimation. The extent of missing data for the following measures was: PASE (13.3%); exercise self-efficacy (12.9%); mental health status (12.9%); physical health status (12.9%) and SWLS (12.9%).
It should be noted, that in the original baseline test of our proposed model (13), we used a latent variable framework with multiple measures of each construct. We attempted to use a similar strategy for examining the hypotheses across time; however, we were unable to identify an admissible solution. Consequently, we adopted a strategy that selected the most reliable and conceptually relevant variables to represent the model constructs across time.
Model specification and fit
The hypothesized panel model tested is shown in Figure 1 and specified: (1) paths from physical activity to self-efficacy at both baseline and 24 months; (2) paths from self-efficacy to mental health status and physical health status at both baseline and 24 months; and (3) paths from mental health status and physical health status to SWLS at both baseline and 24 months. In addition, as McAuley et al. (13) reported a significant association between mental and physical health status, we estimated this association at baseline and follow-up. As is common in panel analysis, stability coefficients were also estimated (35). These coefficients represent correlations between the same variables (e.g., SWLS at baseline and 24 months) measured across time while controlling for the influence of other variables in the model. Overall, the stability coefficients were acceptable for physical activity (β = .50), efficacy (β =.68), mental health status (β =.48), physical health status (β = .55), and QOL (β = .51). For the sake of clarity, these paths are not shown in the figures.
Standard model fit indices were calculated including the chi-square goodness of fit, the root mean square error of approximation (RMSEA), the Comparative Fit Index (CFI) and the standardized root mean square residual (SRMR). Full explanations of these fit indices are available elsewhere (36–39). It is commonly accepted (37) that a non-significant chi-square, values above .95 for the CFI in concert with values of .06 or less for the SRMR, and .08 or less for the RMSEA are indicative of good-fitting models.
Covariates
It is well-established that demographic and health variables are associated with a number of the constructs in this model (e.g, physical activity, self-efficacy, health status) and have the potential to differentially influence the hypothesized relationships. To address this possibility, following the initial test of the hypothesized model, an additional analysis of this model was conducted controlling for baseline assessments of age, race, income, education, and chronic health conditions.
RESULTS
Descriptive statistics for all variables included in the hypothesized model are shown in Table 1. Information relative to participants’ health conditions can be found elsewhere (21). As is evident in the table, there are modest reductions in all variables across the 24-month time period. Paired t-tests, however, indicated that these reductions were all significant, although the effect sizes are generally small with the exception of a moderate reduction in physical activity (see Table 1). The panel model analyzing the relationships proposed in Figure 1 resulted in a good fit for the data (χ2 = 40.37, df = 26, p <.05, RMSEA [90% CI] = .05 [.02–.10], CFI = 0.98, SRMR = .04). All of the hypothesized paths were significant (p < .05) with the exception of the path from changes in physical health status at 24-months to changes in satisfaction with life at 24-months and the correlation between baseline mental health and physical health status. At baseline, more active women were more efficacious (β = .31). More efficacious women reported higher physical (β = .43) and mental (β = .24) health status. Having higher physical and mental health status were associated with higher satisfaction with life or global QOL (β = .38; β = .37, respectively).
Table 1.
Descriptive statistics and effect sizes for changes across time for all model constructs.
| Variable (Range) | Baseline | 24-Month Follow-up | t | p | d |
|---|---|---|---|---|---|
| 1. Physical activity | 159.12 (68.10) [25–425.82] | 128.36 (59.89) [4.39–320.75] | 6.74 | .0001 | .49 |
| 2. Balance confidence (0–100%) | 91.97 (11.26) [11.25–10] | 90.13 (14.18) [16.25–100] | 2.45 | .01 | .17 |
| 3. Mental health (0–100) | 53.19 (8.24) [18.96–71.27] | 52.01 (8.74) [24.11–70.63] | 1.97 | .05 | .13 |
| 4. Physical health (0–100) | 47.64 (9.68) [15.26–62.78] | 46.13 (10.86) [17.66–64.62] | 2.65 | .008 | .18 |
| 5. Satisfaction with life (5–35) | 25.81 (6.19) [5–35] | 24.78 (6.84) [5–35] | 2.55 | .01 | .17 |
Note. Values are expressed as Mean (SD). The data presented for physical activity and activities balance confidence have been previously reported in McAuley et al.13
Range of scores for each variable at each timepoint are shown in brackets below the mean values.
Relative to relationships among changes in constructs over time, changes in physical activity were associated with residual changes in self-efficacy (β = .14). Changes in self-efficacy were significantly related to residual changes in physical health status (β = .34) and mental health status (β = 12). Only changes in mental health status were significantly associated with residual changes in global QOL (β =.38), as represented by satisfaction with life. Finally, there was a significant inverse correlation between mental and physical health status (β = −.19). The overall model accounted for 32% and 51% of the variance in satisfaction with life at baseline and follow-up, respectively.
A final set of analyses tested the model reported above but this time controlling for the potential influence of health conditions and demographic variables (i.e., education, income, age, race). This approach did not significantly improve the overall fit of the model or significantly change the direction, strength, or significance levels of the path coefficients, (χ2 = 32.03, df = 26 p = .16, RMSEA [90% CI] = 0.03 [0.00 – 0.06], CFI = .99, and SRMR = .02). This model accounted for 37% and 52% of the variance in QOL at baseline and follow-up, respectively. Most of the covariates demonstrated significant associations with some of the model constructs (p < .05). For example, older women were less active (β = −.17) and reported poorer mental health status and physical health status at baseline (β = −.12, − .12, respectively) and follow-up (β = −.13, −.14 respectively). Higher income was associated with higher levels of satisfaction with life (β = .26) whereas having a higher education was associated with being more active at baseline (β = .13) and having higher self-efficacy at follow-up (β = .11). Finally, women with more chronic health conditions were less active (β = −.10) and efficacious (β = −.21) and reported lower levels of physical health status (β = −.25) at baseline.
In summary, these findings support the perspective that the relationships between changes in physical activity and satisfaction with life follow pathways through self-efficacy and health status variables.
DISCUSSION
We report a prospective examination of a model of potential pathways from physical activity to QOL in a sample of older women. This model, initially proposed by McAuley et al. (13), hypothesized that physical activity influences global QOL indirectly through its effects on self-efficacy and physical and mental health status. It is important to note that the test of this model controlled for both baseline associations and stability of measures over time, as well as potential confounding variables such as demographics and self-reported chronic health conditions. The initial cross-sectional support for this model (13) was partially replicated in the present study in which relationships among changes in model constructs were examined across time.
Interestingly, the only hypothesized pathway not supported was between changes in physical health status and changes in global QOL over time. One might suggest that such a relationship may be more likely to be manifested in the context of a physical activity intervention in which changes in physical parameters (e.g., endurance, flexibility, strength, function) may be more salient to the individual or across greater periods of time when changes in health status become more apparent/observable to the individual. Indeed, this last assumption is supported by the findings of Stuifbergen and her colleagues (40) in a large, prospective study of exercise, functional limitations, and QOL in individuals with multiple sclerosis. It was reported that rate of change of exercise over a 5-year period was significantly correlated with rate of change of functional limitations (r = −.25) and QOL (r = .42) and that changes in the latter two variables were also correlated (r = −.50). These findings might suggest that increased activity leads to decreased functional limitations and enhanced QOL, although it is unclear from the reporting what the independent relationships between these changes were.
It is acknowledged that mental and physical health status could comprise a number of important constructs that are associated with physical activity, self-efficacy, and QOL. For example, physical health status might be addressed by measuring functional limitations, disability, and functional performance in addition to more global health status measures as used herein. Relative to mental health status, Elavsky et al. (9), have demonstrated that self-efficacy, and in particular, positive affect, were significant mediators of physical activity’s association with overall QOL in a one-year follow-up of a physical activity intervention for older adults. Importantly, Elavsky and her colleagues noted that when examining the relationship between physical activity and quality of life across a four year period, only changes in positive affect mediated this association. Such findings are in concert with Diener et al.’s (28) position that perceptions of life-satisfaction are molded by affective well-being. Recent data from Blane et al. (10) also suggest pathways to QOL through mental and physical health status in which depression and functional limitations mediated the relationships of physical health variables (i.e., blood pressure, body mass index, and lung function) on global QOL. Further, Kreitler, Peleg, and Ehrenfeld (41), in a recent study of cancer survivors, noted that individuals who were more efficacious also reported lower levels of perceived stress and, in turn, improved QOL. Thus, affective responses, perceived stress, self-esteem, and depression may be important components of a latent mental health status construct. Interventions that influence these factors may have the greatest potential for enhancing QOL.
We also note the importance of considering other types of self-efficacy in examining the physical activity-QOL relationship. We focused our measurement on activities considered to be important for exerting control over one’s environment and engaging in daily activities that are important for independent living. However, one might also consider including self-efficacy assessments relative to engaging in different activities or to overcoming barriers to activity in the environment. As well as issues relative to the measurement of the model constructs, the present study is also limited by the short time period and focus exclusively on women. Additionally, it is important to note that we focused on only two elements of function (mental/psychosocial and physical) that may explain the association between physical activity and QOL. Identifying and testing additional pathways representing other elements of function (e.g., cognitive and social function) may have further explanatory power (42).
As attempts to disentangle the complexity of the relationship between physical activity and QOL continue, it will be important to consider not just mediators of this relationship but also potential moderators. It has previously been noted that the perceived value of physical activity may have a role to play on this relationship (1,3). That is, do people who place a greater value on physical activity demonstrate a better quality of life? Diener et al. (43) have noted that domain satisfaction is an important component of overall life satisfaction. Certainly, the maintenance of an independent lifestyle is, in all probability, a valued element of the aging process. Whether physical activity is an equally valued component of older adults’ lives is of less certainty. As health promotion campaigns targeting older adults continue to stress physical activity as a key ingredient in a healthy lifestyle, physical activity is more likely to take on greater value and to be more strongly viewed as an important method of maintaining function and independence. Thus, the assessment of baseline value attributions and the development of strategies for changing perceived values relative to physical activity may be worthy of consideration.
Another consideration worthy of future research consideration is the extent to which differential changes in physical activity bring about differential changes in QOL and other model components. For example, we note a relatively large decline in physical activity across time but relatively small changes in the other constructs. Whether larger increases in physical activity brought about by interventions show smaller or more substantial increases in elements of QOL remains to be determined. Indeed, such questions may well be tied to changes in value that individuals associate with physical activity.
Strengths of the present study include a relatively large sample followed over a 24-month period, a high rate of retention, and the use of a well-established theoretical framework to examine some potential pathways from physical activity to QOL. In spite of the numerous studies and reviews (2,3)of this relationship in the literature, it is believed that these data represent one of the first attempts at testing potential mediators of this relationship that are theoretically-grounded and that have implications for how physical activity interventions might be structured to maximize increases in QOL. That is, these findings indicate that self-efficacy plays an important role in explaining the bivariate associations between physical activity, physical and mental health status, and global QOL. This underscores the necessity of structuring physical activity interventions and programs to provide experiences, feedback, and information that serve to enhance perceptions of capabilities. Failing to take into consideration this important, modifiable factor is likely to result in reduced effort and adherence, which is likely to lead to the erosion of self-efficacy (44). Ultimately, as these data suggest, this will have implications for reduced QOL.
As previously noted (13), the physical activity and QOL relationship is clearly more complex than is often painted in the literature and appears to involve influencing modifiable, more proximal outcomes (e.g., self-efficacy) as an initial step in the process. Although we view QOL as a more global construct reflecting overall satisfaction or happiness with life (6), we do not suggest that those constructs comprising HRQL be accorded a necessarily lesser status. Indeed, assessing physical, social, and mental health status appears to be an important element in the development of QOL. Moreover, they represent important outcomes associated with physical activity. Subsequent research endeavors might consider examining the relationship and the pathways proposed over longer periods of time, as a function of interventions, and in diseased populations. In closing, in spite of living longer lives, there is limited evidence to suggest that older adults are living better lives. Understanding the manner in which physical activity influences QOL, an important indicator of well-being, is clearly of public health importance.
Acknowledgments
This manuscript was prepared with the support of grant # AG20118 from the National Institute on Aging.
References
- 1.McAuley E, Elavsky S. Physical activity, aging, and quality of life. In: Zhu W, Chodzko-Zajko W, editors. Measurement issues in aging and physical activity. Champaign: Human Kinetics; 2006. [Google Scholar]
- 2.Netz Y, Wu M. Physical activity and psychological well-being in advanced age: A meta-analysis of intervention studies. Psychol Aging. 2005;20(2):272–284. doi: 10.1037/0882-7974.20.2.272. [DOI] [PubMed] [Google Scholar]
- 3.Rejeski WJ, Mihalko SL. Physical activity and quality of life in older adults. J Gerontol. 2001;56A(Special Issue II):23–35. doi: 10.1093/gerona/56.suppl_2.23. [DOI] [PubMed] [Google Scholar]
- 4.Stewart AL, King AC. Evaluating the efficacy of physical activity for influencing quality of life outcomes in older adults. Ann Behav Med. 1991;13(3):108–116. [Google Scholar]
- 5.Tarlov AR, Ware JEJ, Greenfield S, et al. The medical outcomes study: An application of methods for monitoring the results of medical care. JAMA. 1989;262:925–930. doi: 10.1001/jama.262.7.925. [DOI] [PubMed] [Google Scholar]
- 6.Frisch MB. Quality of life therapy and assessment in health care. Clinical Psychology: Science and Practice. 1998;5(1):19–40. [Google Scholar]
- 7.Lawton MP. Housing characteristics and the well-being of elderly tenants in federally assisted housing. J Gerontol. 1975;30(5):601–606. doi: 10.1093/geronj/30.5.601. [DOI] [PubMed] [Google Scholar]
- 8.Scogin F, Morthland M, Kaufman A, Burgio L, Chaplin W, Kong G. Improving quality of life in diverse rural older adults: A randomized trial of a psychological treatment. Psychol Aging. 2007;22(4):657–665. doi: 10.1037/0882-7974.22.4.657. [DOI] [PubMed] [Google Scholar]
- 9.Elavsky S, McAuley E, Motl R, et al. Physical activity enhances long-term quality of life in older adults: Efficacy, esteem and affective influences. Ann Behav Med. 2005;30(2):138–145. doi: 10.1207/s15324796abm3002_6. [DOI] [PubMed] [Google Scholar]
- 10.Blane D, Netuveli G, Montgomery SM. Quality of life, health and physiological status and change at older ages. Soc Sci Med. doi: 10.1016/j.socscimed.2007.12.021. In press. [DOI] [PubMed] [Google Scholar]
- 11.Diener E. Subjective well-being. Psychol Bull. 1984;95:542–575. [PubMed] [Google Scholar]
- 12.Pavot W, Diener E. Review of the satisfaction with life scale. Psychol Assess. 1993;5(2):164–172. [Google Scholar]
- 13.McAuley E, Konopack JF, Motl R, et al. Physical activity and quality of life in older adults: Influence of health status and self-efficacy. Ann Behav Med. 2006;31(1):99–103. doi: 10.1207/s15324796abm3101_14. [DOI] [PubMed] [Google Scholar]
- 14.Bandura A. Self-Efficacy: The Exercise of Control. New York: W.H. Freeman; 1997. [Google Scholar]
- 15.McAuley E, Blissmer B. Self-efficacy determinants and consequences of physical activity. Exerc Sport Sci Rev. 2000;28(2):85–88. [PubMed] [Google Scholar]
- 16.Sproston K, Primatesta P. Health Survey for England Volume 2: Risk Factors for Cardiovascular Disease. TSO; London: 2004. [Google Scholar]
- 17.Estabrooks PA, Lee RE, Gyurcsik NC. Resources for physical activity participation: Does availability and accessibility differ by neighborhood socioeconomic status? Ann Behav Med. 2003;25(2):100–104. doi: 10.1207/S15324796ABM2502_05. [DOI] [PubMed] [Google Scholar]
- 18.U.S. Physical Activity Statistics. [Accessibility verified October 25, 2007];State Comparison by Demographics. Centers for Disease Control and Prevention (online) Available at http://apps.nccd.cdc.gov/PASurveillance/DemoCompareResultV.asp?State=0&Cat=4&Year=2005&Go=GO#result.
- 19.Schutzer KA, Graves BS. Barriers and motivations to exercise in older adults. Prev Med. 2004;39(5):1056–1061. doi: 10.1016/j.ypmed.2004.04.003. [DOI] [PubMed] [Google Scholar]
- 20.McAuley E, Konopack JF, Motl RW, et al. Measuring disability and function in older women: Psychometric properties of the late life function and disability instrument. J Gerontol A Biol Sci Med Sci. 2005;60:901–909. doi: 10.1093/gerona/60.7.901. [DOI] [PubMed] [Google Scholar]
- 21.McAuley E, Morris KS, Doerksen SE, et al. Physical activity change effects on functional limitations in older women: Mediating roles of functional performance and self-efficacy. J Am Geriatr Soc. 2007;55:1967–1973. doi: 10.1111/j.1532-5415.2007.01469.x. [DOI] [PubMed] [Google Scholar]
- 22.Washburn RA, Smith KW, Jette AM, et al. The physical activity scale for the elderly (PASE): Development and evaluation. J Clin Epidemiol. 1993;46(2):153–162. doi: 10.1016/0895-4356(93)90053-4. [DOI] [PubMed] [Google Scholar]
- 23.Martin KA, Rejeski WJ, Miller ME, et al. Validation of the PASE in older adults with knee pain and physical disability. Med Sci Sports Exerc. 1999;31(5):627–633. doi: 10.1097/00005768-199905000-00001. [DOI] [PubMed] [Google Scholar]
- 24.Washburn RA, McAuley E, Katula J, et al. The physical activity scale for the elderly (PASE): Evidence for validity. J Clin Epidemiol. 1999;52:643–651. doi: 10.1016/s0895-4356(99)00049-9. [DOI] [PubMed] [Google Scholar]
- 25.Powell LE, Myers AM. The Activities-specific Balance Confidence (ABC) Scale. J Gerontol A Biol Sci Med Sci. 1995;50A(1):M28–M34. doi: 10.1093/gerona/50a.1.m28. [DOI] [PubMed] [Google Scholar]
- 26.Ware JE, Kosinski M, Keller SD. A 12-Item Short-Form Health Survey: Construction of scales and preliminary tests of reliability and validity. Med Care. 1996;34(3):220–233. doi: 10.1097/00005650-199603000-00003. [DOI] [PubMed] [Google Scholar]
- 27.Ware JE, Kosinski M, Keller SD. SF-36 Physical and Mental Health Summary Scales: A User’s Manual. Boston, MA: The Health Institute, New England Medical Center; 1994. [Google Scholar]
- 28.Diener E, Emmons R, Larsen R, et al. The satisfaction with life scale. J Pers Assess. 1985;49:71–75. doi: 10.1207/s15327752jpa4901_13. [DOI] [PubMed] [Google Scholar]
- 29.Pavot WG, Diener E, Colvin CR, et al. Further validation of the satisfaction with life scale: Evidence for the cross-method convergence of well-being measures. J Pers Assess. 1991;57:149–161. doi: 10.1207/s15327752jpa5701_17. [DOI] [PubMed] [Google Scholar]
- 30.Halaby CN. Panel models in sociological research: Theory into practice. Annu Rev Sociol. 2004;30:507–544. [Google Scholar]
- 31.Muthén LK, Muthén BO. Mplus user’s guide. Los Angeles: Muthén & Muthén; 2004. [Google Scholar]
- 32.Arbuckle JL. Full information estimation in the presence of incomplete data. In: Marcoulides GA, Schumacker RE, editors. Advanced structural equation modeling: Issues and techniques. Mahwah, NJ: Lawrence Erlbaum Associates; 1996. pp. 243–278. [Google Scholar]
- 33.Enders CK. The impact of nonnormality on full information maximum-likelihood estimation for structural equation models with missing data. Psychol Methods. 2001;6:352–370. [PubMed] [Google Scholar]
- 34.Enders CK, Bandalos DL. The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling. 2001;8:430–457. [PubMed] [Google Scholar]
- 35.Kessler RC, Greenberg DF. Linear panel analysis. Models of quantitative change. New York: Academic; 1981. [Google Scholar]
- 36.Bentler PM. Comparative fix indexes in structural models. Psychol Bull. 1990;107(2):238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- 37.Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- 38.Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing structural equation models. Newbury Park, CA: Sage; 1993. pp. 136–162. [Google Scholar]
- 39.Bentler PM, Bonett DG. Significance tests and goodness fit in the analysis of covariance structures. Psychol Bull. 1980;88:588–606. [Google Scholar]
- 40.Stuifbergen AK, Blozis SA, Harrison TC, et al. Exercise, functional limitations, and quality of life: A longitudinal study of persons with multiple sclerosis. Arch Phys Med Rehabil. 2006;87:935–943. doi: 10.1016/j.apmr.2006.04.003. [DOI] [PubMed] [Google Scholar]
- 41.Kreitler S, Peleg D, Ehrenfeld M. Stress, self-efficacy and quality of life in cancer patients. Psychooncology. 2007;16(4):329–341. doi: 10.1002/pon.1063. [DOI] [PubMed] [Google Scholar]
- 42.McAuley E, Morris KS. Advances in physical activity and mental health: Quality of life. American Journal of Lifestyle Medicine. 2007;1(5):389–396. [Google Scholar]
- 43.Diener E, Oishi S, Lucas RE. Personality, culture, and subjective well-being: Emotional and cognitive evaluations of life. Annu Rev Psychol. 2003;54:403–25. doi: 10.1146/annurev.psych.54.101601.145056. [DOI] [PubMed] [Google Scholar]
- 44.Seeman TE, Unger JB, McAvay G, et al. Self-efficacy beliefs and perceived declines in functional ability: MacArthur studies of successful aging. J Gerontol B Psychol Sci Soc Sci. 1999;54B(4):214–222. doi: 10.1093/geronb/54b.4.p214. [DOI] [PubMed] [Google Scholar]