Abstract
A sample of college students, oversampled for smoking (N = 127, 43% smokers), monitored daily experiences using electronic diaries over 14 days. We examined the frequency and correlates of liberally-defined hangover-like experiences (HLEs) using data from 1,595 person-days (1,325 following abstention from drinking, 270 following drinking, including 125 HLEs). More than 40% of the sample reported at least one HLE and nearly half of all drinking episodes were followed by HLE. Endorsement of HLE was more likely as the number of drinks increased and was associated with modest elevations of hangover symptoms. Gender did not predict rates of overall HLE endorsement, but males were less likely to report HLE after a drinking episode and showed a weaker relation between number of drinks and HLE. Smokers were more likely to report HLE, but there was no evidence that smoking status was associated with increased HLE susceptibility. Self-reported parental alcohol problems were associated with more frequent HLE and incrementally predicted HLE endorsement when number of drinks was covaried. The findings suggest HLE is a common outcome of college drinking and attest to the feasibility of using electronic diaries to assess its episode- and person-level correlates.
Keywords: alcohol, hangover, electronic diary, college students, gender, smoking
Hangover is one of the most prevalent negative consequences of binge drinking (Wiese, Shlipak & Browner, 2000). Hangover in college drinkers deserves further research attention. From a public health perspective, hangover is important because it has the potential to interfere with role functioning and scholastic achievement (e.g., Perkins, 2002). Hangover susceptibility has also been hypothesized to be a marker of either protection from or risk for later alcohol use disorder (AUD). Interestingly, suggestive evidence supporting both propositions can be found in the existing literature (cf. Earleywine, 1993; Newlin & Pretorious, 1990; Piasecki, Sher, Slutske, & Jackson, 2005; Slutske, Piasecki & Hunt-Carter, 2003; Span & Earleywine, 1999; Wall, Horn, Johnson, Smith & Carr, 2000; Wall, Shea, Luczak, Cook, & Carr, 2005; Yokoyama, et al., 2005). Thus, both practical considerations and theory suggest hangover in young drinkers deserves closer scrutiny. Toward this end, this study examined the frequency and predictors of hangover-like experiences reported by a sample of undergraduates during a two-week period of self-monitoring.
Little is known about how individual drinkers use the common-language term “hangover.” In this study, we used an assessment with a low implied threshold to enhance sensitivity and encourage students to report the presence of any aversive morning-after effects they attributed to drinking, even if these might not rise to the level of their personal definition of “hangover.” We use the term hangover-like experiences (HLE) hereafter to distinguish this inclusive, liberal assessment from potentially stricter assessments of “hangover” per se.
HLEs are complex, drinking-contingent outcomes. Conceivably, reports of naturally-occurring HLE may reflect factors associated with heavy drinking frequency (and, hence, opportunity to develop next-day symptoms), individual differences in susceptibility to HLE, or a blend of both processes. Diary monitoring is well-suited to disentangling these effects. By tracking drinking behaviors and HLE over a period of time, it is possible to identify individual difference factors related to the overall likelihood of endorsing HLE as well as factors that incrementally predict HLE endorsement after accounting for the degree of alcohol exposure in an episode.
We sought to characterize the frequency of HLE, determine the validity of the HLE assessment, and characterize the amount of alcohol typically consumed prior to HLE. Additional analyses focused on prediction of HLE from three individual difference variables related to risk for AUD and plausibly related to hangover: gender, smoking status, and parental alcohol problems. Males, smokers, and persons with a family history of alcoholism are all at elevated risk for developing AUD (e.g., Grant, et al., 2004; Hussong, Bauer, & Chassin, 2008; Jackson, Sher, Wood, & Bucholz, 2003). Prior research suggests women may be more susceptible to hangover at a given number of drinks (Jackson, 2008; Piasecki, et al., 2005; Slutske, et al. 2003). Smoking and nicotine administration alter subjective responses to alcohol (cf. Kouri, McCarthy, Faust, & Lukas, 2004; Madden, Heath, & Martin, 1997). Moreover, smoking and drinking covary across persons (e.g., Bobo & Husten, 2000) and across time within persons (e.g., Piasecki, McCarthy, Fiore & Baker, 2008). Thus, acute pharmacologic effects of smoking or trait/constitutional differences between smokers and nonsmokers could play a role in HLE. Some survey (Newlin & Pretorious, 1990; Piasecki, et al., 2005; Slutske, et al., 2003) and laboratory research (McCaul, Turkkan, Svikis & Bigelow, 1991; Span & Earleywine, 1999) suggests familial alcoholism is associated with increased hangover frequency and susceptibility, though failures to find such effects have also been reported (e.g. Earleywine, 1993; Howland, et al., 2008).
Method
Participants
Students (n=127, 85% White, 61% female) enrolled in introductory psychology classes at the University of Missouri volunteered for a 14-day diary study of daily experiences in smokers and nonsmokers. Slightly more than half the sample were nonsmokers (n=72, 57%). Of the 55 smokers, 37 reported smoking daily. The smokers were not highly dependent; the average score on the Fagerström Test for Nicotine Dependence (FTND; Heatherton, Kozlowski, Frecker & Fagerström, 1991) was 0.94 and more than half of smokers (n=30) scored 0. The mean age was 18.8 years (range 18–32, median = 19). Participants received partial course credit and $75.
Procedure
Electronic diaries were implemented on personal digital assistants (PDAs; Palm Zire, Palm, Inc., Sunnyvale, CA) and questionnaires were administered via commercially-available software (Pendragon Forms version 3.2, Pendragon Software, Libertyville, IL). Signaling was controlled using reminder software (Bug Me, Electric Pocket, Ltd., Chepstow, UK). Four alarms per day were programmed to fire according to a predetermined, quasi-random schedule that changed each day for a given participant. Participants carried the PDAs in their natural environments for 14 days and began recording the day after an orientation and training session. All participants were instructed to respond to prompted assessments, and smokers were asked to complete entries before and after smoking. Participants visited the laboratory every 3–4 days so staff could download data, field questions, and encourage compliance. On average, analyzed participants provided at least one diary record on 13.3 days, and 94% provided at least one record 10 or more days.
Measures
Individual Differences
Gender and smoking status were determined from demographic and smoking history questionnaires. Following Slutske, et al. (2003), parental alcohol problems were assessed with the following screening item: “To your knowledge, has one or both of your biological parents ever had any of the following experiences related to the use of alcohol: problems fulfilling obligations at school or work, physical health or emotional problems, problems with family or friends, or legal problems (e.g., DUI, DWI)?” Ninety-two participants (73%) answered that neither biological parent had experienced one of these problems. Thirty-four participants (27%) were counted as reporting parental alcohol problems. Of these, 26 indicated problems had been experienced by the father, 3 by the mother, and 5 by both biological parents. A response to this item was missing for one participant.
Prior Night’s Drinking and HLE
In the first completed prompted assessment of each day, participants received questions about the drinking episode if they indicated they had consumed alcohol the night before. Participants were shown a screen saying “The next question asks the amount of alcohol you drank. A ‘standard drink’ is a can or bottle of beer, a glass of wine, or a shot of liquor.” Next, a numeric free response field was used to report the total number of standard drinks. A yes/no question about presence of HLE read: “Did you feel hungover this morning (even just a little) as a result of last night’s drinking?” A “yes” response was scored 1 and a “no” 0.
Hangover Symptoms
Prompted assessments included 5 items adapted from the Hangover Symptoms Scale (HSS; Slutske, et al., 2003). To minimize possible demand or carry-over effects, these items were embedded in a list of items tapping various subjective states, administered at every interview (i.e., not just drinking reports), and always presented prior to items about the drinking episode and HLE. Each item stem read: “Please rate how you’ve felt in the past 15 minutes.” The symptoms are listed in Table 1. Items were rated on a scale from 1 (not at all) to 5 (extremely).
Table 1.
Results of models testing differences in individual symptoms within first records of the day on post-drinking days with and without HLE relative to days following abstention.
| Abstention (Intercept)a |
Drinking Without HLE |
Drinking With HLE |
||||
|---|---|---|---|---|---|---|
| Symptom | Coefficient | 95% CI | Coefficient | 95% CI | Coefficient | 95% CI |
| More tired than usual | 1.89 | 1.80, 1.99 | −0.002 | −0.19, 0.19 | 0.35** | 0.11, 0.59 |
| Headache | 1.22 | 1.17, 1.26 | 0.05 | −0.07, 0.16 | 0.80*** | 0.60, 0.99 |
| Nauseous | 1.11 | 1.08, 1.14 | −0.001 | −0.08, 0.08 | 0.52*** | 0.39, 0.65 |
| Very weak | 1.22 | 1.18, 1.26 | −0.01 | −0.11, 0.09 | 0.53*** | 0.37, 0.68 |
| Extremely thirsty or dehydrated | 1.79 | 1.71, 1.87 | 0.15 | −0.02, 0.31 | 0.78*** | 0.55, 1.01 |
Note.
p<.01,
p<.001;
CI = confidence interval.
Intercept values are provided for descriptive purposes; statistical tests not reported because they evaluate the difference from zero. Symptoms were rated on 1–5 scale (i.e., did not contain a zero value).
Data Selection
Analyses focused on the first prompted assessment of the day because, by design, these were the records in which information on drinking and HLE was collected. Of the 1,687 first daily records, 92 (5.5%) were excluded due to missing data or ambiguity in drinking-related reporting. In the remaining 1,595 records, 1,325 were from days on which the participant denied drinking the night before and 270 records contained reports of prior night’s drinking.
Statistical Analysis
A generalized estimating equations (GEE) approach was used to account for the clustered data structure. An AR(1) working correlation structure was specified for all models. Models predicting the dichotomous HLE item specified a binomial family and a logit link function. Because continuously-scaled variables (number of drinks, symptoms) were positively skewed, a gamma family and an identity link function were used.
Initial analyses explored the validity of the HLE item. First, HLE endorsement on post-drinking days was predicted from number of drinks in the episode. Next, each of the 5 diary-measured HSS symptoms was predicted from indicator variables indicating whether a given record was (a) from a day in which drinking but not HLE was endorsed or (b) a day for which both drinking and HLE were reported. Post-abstention days formed the reference category.
We explored relations between each of the individual difference variables and HLEs using a sequence of 4 models that differed with respect to consideration of drinking information. In Model 1, the individual difference variable was entered as the sole predictor of HLE endorsement in all morning diary records. This model assessed whether the predictor was associated with the overall likelihood of an HLE during the monitoring period, but did not consider whether any effects are attributable to different rates of drinking behavior. Model 2 again tested the individual difference factor as the sole predictor, but this time the analysis was limited to post-drinking records. This model tested whether the individual difference variable predicted HLE endorsement given the occurrence of drinking. In Model 3, number of drinks was added as a covariate to test whether the individual difference factor contributed incremental prediction beyond the amount of alcohol exposure in the episode. In Model 4, Model 3 was elaborated further to include an interaction term testing whether the individual difference variable moderated the relation between amount of alcohol consumed and the likelihood of HLE endorsement. Model 1 is conceptually related to HLE frequency while Models 2–4 test successively stricter conceptualizations of HLE susceptibility.
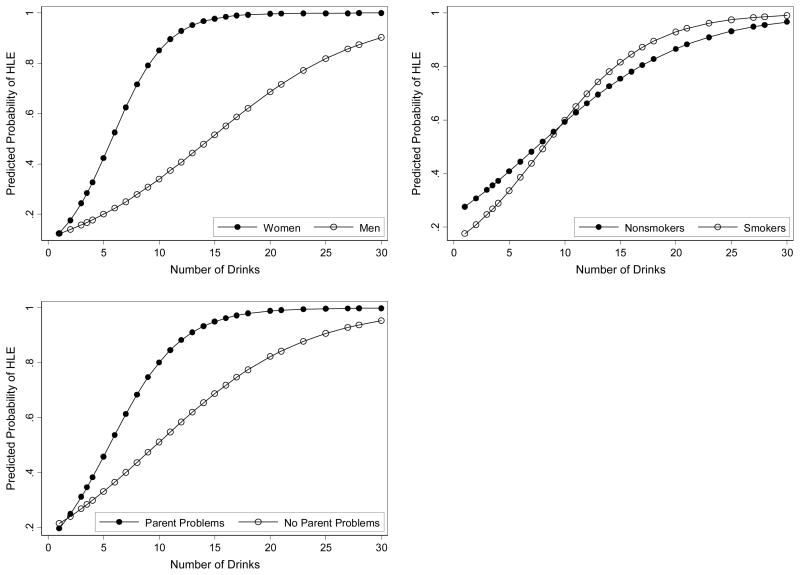
Supplemental models were performed to generate descriptive information. First, HLE endorsement was predicted from number of drinks in analyses stratified by each individual difference variable. Model-predicted probabilities were plotted by subgroup to illustrate potential HLE susceptibility effects. Second, model-based proportions were generated from Model 2 analyses to characterize the population-averaged rate of HLE endorsement on post-drinking days by subgroup. Finally, number of drinks was predicted from HLE endorsement and each individual difference variable in separate models. This permitted generation of population-averaged estimates of the mean drinks in non-HLE and HLE drinking episodes for each subgroup.
Results
Rates of Drinking and HLE Endorsement
Ninety-five participants (73.1%) reported at least one drinking episode in a first record of the day (range: 1 to 12, median = 2, mode =1). HLE was endorsed in 125 (46.3%) of the 270 post-drinking records. Fifty-three participants (40.8%) reported at least one HLE in a first record of the day (range: 1 to 7, median = 2, mode =1).
Number of Drinks and HLE
Across all drinking reports, the number of drinks ranged from 1 to 30 (M =7.7; median = 7). As would be expected, the number of drinks was a significant predictor of HLE (OR = 1.20, 95% CI = 1.13–1.29, p<.001).
Symptom Ratings
All 5 items derived from the HSS were elevated when participants endorsed HLE (Table 1). No symptom was higher on days for which drinking was reported but HLE denied.
Individual Differences
Table 2 gives results from Models 1–4 for each individual difference factor. Gender was unrelated to the overall likelihood of reporting HLE (Model 1). When only post drinking reports were considered, men were less likely than women to report HLE (Model 2). This effect held when number of drinks was covaried (Model 3), and was attributable to a weaker relation between number of drinks and HLE among men (Model 4). Smokers were more likely than nonsmokers to report HLE (Model 1) but this effect did not remain in Models 2–4 suggesting the overall effect was attributable to more frequent drinking by smokers. Parental alcohol problems predicted overall likelihood of HLE endorsement (Model 1) and this effect persisted when only post-drinking reports were examined (Model 2). Adjusting for number of drinks did not liquidate the effect (Model 3) but Model 4 revealed no main effect for parental alcohol problems and only a trend (p=.09) toward an interaction between family history and number of drinks.
Table 2.
Odds ratios and confidence intervals from models predicting HLE endorsement from individual difference variables.
| Model 1 | Model 2 | Model 3 | Model 4 | |
|---|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Gender | ||||
| Male | 0.72 (0.44–1.15) | 0.49* (0.25–0.96) | .17*** (0.07–0.38) | 1.02 (0.25–4.18) |
| Number of Drinks | -- | -- | 1.28*** (1.19–1.39) | 1.50*** (1.30–1.73) |
| Male × Number of Drinks | -- | -- | -- | 0.79** (0.66–0.93) |
| Smoking Status | ||||
| Smoker | 2.77*** (1.78–4.31) | 0.90 (0.47–1.71) | 0.83 (0.42–1.64) | 0.54 (0.17–1.75) |
| Number of Drinks | -- | -- | 1.21*** (1.13–1.29) | 1.16** (1.05–1.29) |
| Smoker × Number of Drinks | -- | -- | -- | 1.06 (0.93–1.22) |
| Parental Alcohol Problems | ||||
| Parent Problems | 2.18*** (1.40–3.39) | 2.70** (1.36–5.35) | 2.22* (1.08–4.59) | 0.79 (0.19–3.34) |
| Number of Drinks | -- | -- | 1.20*** (1.12–1.29) | 1.15*** (1.07–1.25) |
| Parent Problems × Number of Drinks | -- | -- | -- | 1.18 (0.97–1.42) |
Note.
p<.05,
p<.01,
p<.001;
HLE = Hangover-like experience. OR = Odds ratio, CI = confidence interval. See text for a description of each model.
Figure 1 illustrates the nature of these effects by plotting model-based estimates of HLE endorsement probability as a function of the number of drinks reported for subgroups defined by sex, smoking status, and parental problems. Table 3 summarizes model-based estimates of the number of drinks in HLE- and Non-HLE drinking episodes and the proportion of the drinking events followed by HLE for the full sample and each subgroup.
Figure 1.
Model-based estimates of the relation between number of drinks and the probability of HLE endorsement by gender (top left), smoking status (top right), and parental alcohol problems (bottom).
Table 3.
Model-based estimates of the mean number of drinks reported in the absence or presence of HLE endorsement and the proportion of drinking events followed by HLE.
| Group | Drinks without HLE |
Drinks with HLE |
Proportion of Post-Drinking Days with HLE |
|||
|---|---|---|---|---|---|---|
| Estimate | 95% CI | Estimate | 95% CI | Estimate | 95% CI | |
| Full Sample | 5.8 | 5.1, 6.6 | 10.1 | 8.7, 11.5 | .48 | .40, .56 |
| Gender | ||||||
| Men | 7.5 | 6.3, 8.9 | 15.1 | 11.8, 18.3 | .37 | .25, .50 |
| Women | 4.5 | 3.9, 5.2 | 8.2 | 7.1, 9.3 | .54 | .44, .64 |
| Smoking Status | ||||||
| Smokers | 5.9 | 4.8, 6.8 | 10.0 | 7.8, 12.3 | .47 | .37, .57 |
| Nonsmokers | 5.8 | 4.5, 7.1 | 10.1 | 8.4, 12.0 | .50 | .37, .62 |
| Parental Alcohol Problems | ||||||
| Endorsed | 5.2 | 3.7, 6.6 | 12.5 | 9.7, 15.2 | .65 | .51, .77 |
| Not Endorsed | 5.9 | 5.1, 6.8 | 8.7 | 7.2, 10.2 | .41 | .32, .50 |
Note. CI = confidence interval.
Discussion
Approximately 40% of the students reported at least one HLE during an arbitrary 14-day period. HLE was endorsed in nearly half of the drinking episodes reported. These are likely upper-bound estimates of hangover frequency because we attempted to maximize sensitivity for morning-after effects by using an assessment with a low implied threshold. Additionally, we used a convenience sample from one campus and oversampled smokers, so our findings cannot be construed as definitive population estimates of college HLE frequency. Clearly, however, HLEs are common outcomes of college drinking episodes deserving further investigation.
A diary item asking whether students experienced hangover, “even just a little,” appeared to be a valid method for identifying hangover-like experiences. When students endorsed HLE, they also reported higher scores on hangover symptoms. The degree of symptom elevation was modest, but this is also observed in laboratory studies of hangover involving administration of substantial doses of alcohol (e.g., Kruisselbrink, et al., 2006; Roehrs, Yoon & Roth, 1991; Rohsenow, et al., 2007). HLE endorsement was more likely as the number of drinks consumed increased. On average, students reported 5.8 drinks without HLE and 10.1 when endorsing HLE. These estimates accord with prior findings suggesting 8–10 drinks is an approximate hangover threshold in college drinkers (e.g., Jackson, 2008; Mallet, Lee, Neighbors, Larimer & Turrisi, 2006). This is notably higher than some definitions of binge drinking (e.g., 4–5 drinks; Wechsler & Nelson, 2001). Thus, even though the HLE assessment encouraged drinkers to use low subjective threshold for endorsement, HLE might still be considered a high-threshold event with reference to alcohol exposure.
The potential to identify factors associated with frequency or susceptibility to HLE is a strength of the diary monitoring approach. In this study, gender was most clearly associated with differential susceptibility to HLE. Smoking status was associated with HLE frequency but not susceptibility. A self-report of parental alcohol problems was associated with both more frequent HLE and possible increased susceptibility to HLE, though evidence for this was weaker than observed for gender (i.e., a main effect only). Some individual difference factors (e.g. cigarette use) may primarily predict HLE frequency because they are markers of disinhibition or impulsivity and a propensity to drink heavily (e.g., Jensen, et al., 2003; Reynolds, et al., 2007). Other factors (e.g., female gender) may be related to HLE susceptibility because they are associated with increased pharmacologic sensitivity to alcohol (e.g., Lieber, 1997). Finally, some characteristics (e.g., familial alcohol problems) may be associated with frequency and susceptibility via both routes (e.g., Sher, Brent, Walitzer, & Wood, 1991; Morzorati, Ramchandi, Fluri, Li, & O’Connor, 2002). It must be stressed that the current data are better-suited to stimulating than to resolving such questions. Alternative accounts, including method artifacts (e.g., group differences in willingness to endorse HLE or bias in reporting the number of drinks), could explain the findings. Future studies are needed to evaluate the replicability and potential mediators of the observed effects.
The current findings did not reveal consistent, unidirectional associations between known risk factors for AUD and HLE susceptibility. Being female is associated with lowered risk of AUD and parental alcohol problems are associated with heightened AUD risk, but both characteristics appeared to be related to HLE susceptibility in this study. One inference might be that hangover/HLE susceptibility is not a good candidate marker of AUD risk. Another could be that HLE susceptibility effects in different subpopulations may reflect qualitatively distinct causal mechanisms with varying implications for AUD development (e.g., Begleiter & Porjesz, 1999). A third possibility is that a more stringent criterion (i.e., “hangover” per se) might reveal more consistent associations with AUD risk factors. Finally, it is interesting that both women and offspring of alcoholics show “telescoping” of drinking problems (Hussong, et al., 2008; Randall, et al., 1999). Thus, it is possible that susceptibility to hangover/HLE might prove to be related to the course of incipient AUD rather than its occurrence per se. Although short-term ecological studies may play a valuable role in generating a set of worthy hypotheses, definitively addressing the relation (if any) between HLE/hangover susceptibility and AUD risk ultimately requires long-term prospective studies incorporating formal diagnostic assessments (e.g., Piasecki, et al., 2005).
Additional limitations should be noted. The observation period was brief. Participants provided a retrospective tally of the prior night’s drinks. Given the short duration of retrospection, these are likely to be reasonably accurate, but we cannot rule out rating bias. Students are known to overestimate the size of standard drinks (White, et al., 2005). As a result, self-reported drink totals may systematically underestimate the true amount of alcohol consumed in standard drink units. Participants’ body weights were not measured. This information would have been valuable for calculating estimated blood alcohol concentrations associated with HLE. Rates of alcohol-tobacco co-use during the drinking episode may play an important role in HLE; the data collected did not permit examination of this question.
The findings attest to the feasibility of assessing hangover or HLE in the stream of daily experience (see also Jackson, 2008; Muraven, Collins, Morsheimer, Shiffman & Paty, 2005). Valuable future avenues for daily monitoring studies include examination of possible near-term negative consequences of HLE (e.g., academic impairment; morning drinking) and further delineation of the person- and event-level correlates of hangover/HLE frequency and susceptibility.
Acknowledgments
Supported by NIH grants DA016330 and P50AA011998. We thank David Newlin for his thoughtful comments on an earlier draft and Alison Richardson for assistance with data collection.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/adb
References
- Begleiter H, Porjesz B. What is inherited in the predisposition toward alcoholism? A proposed model. Alcoholism: Clinical and Experimental Research. 1999;23:1125–1135. doi: 10.1111/j.1530-0277.1999.tb04269.x. [DOI] [PubMed] [Google Scholar]
- Bobo JK, Husten C. Sociocultural influences on smoking and drinking. Alcohol Research & Health. 2000;24:225–232. [PMC free article] [PubMed] [Google Scholar]
- Earleywine M. Personality risk for alcoholism covaries with hangover symptoms. Addictive Behaviors. 1993;18:415–420. doi: 10.1016/0306-4603(93)90058-h. [DOI] [PubMed] [Google Scholar]
- Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991–1992 and 2001–2002. Drug and Alcohol Dependence. 2004;74:223–234. doi: 10.1016/j.drugalcdep.2004.02.004. [DOI] [PubMed] [Google Scholar]
- Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: A revision of the Fagerström Tolerance Questionnaire. British Journal of Addiction. 1991;86:1119–1127. doi: 10.1111/j.1360-0443.1991.tb01879.x. [DOI] [PubMed] [Google Scholar]
- Howland J, Rohsenow DJ, Allesnworth-Davies D, Greece J, Almeida A, Minsky SJ, Arnedt JT, Hermos J. The incidence and severity of hangover the morning after moderate alcohol intoxication. Addiction. 2008;103:758–765. doi: 10.1111/j.1360-0443.2008.02181.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hussong A, Bauer D, Chassin L. Telescoped trajectories from alcohol initiation to disorder in children of alcoholic parents. Journal of Abnormal Psychology. 2008;117:63–78. doi: 10.1037/0021-843X.117.1.63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM. Heavy episodic drinking: Determining the predictive utility of five or more drinks. Psychology of Addictive Behaviors. 2008;22:68–77. doi: 10.1037/0893-164X.22.1.68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jackson KM, Sher KJ, Wood PK, Bucholz KK. Alcohol and tobacco use disorders in a general population: Short-term and long-term associations from the St. Louis Epidemiological Catchment Area Study. Drug and Alcohol Dependence. 2003;71:239–253. doi: 10.1016/s0376-8716(03)00136-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jensen MK, Sorenson TIA, Andersen AT, Thorsen T, Tolstrup JS, Gotfredsen NS, Gronbaek M. A prospective study of the association between smoking and later alcohol drinking in the general population. Addiction. 2003;98:355–363. doi: 10.1046/j.1360-0443.2003.00304.x. [DOI] [PubMed] [Google Scholar]
- Kouri EM, McCarthy EM, Faust AH, Lukas SE. Pretreatment with transdermal nicotine enhances some of ethanol’s acute effects in men. Drug and Alcohol Dependence. 2004;75:55–65. doi: 10.1016/j.drugalcdep.2004.01.011. [DOI] [PubMed] [Google Scholar]
- Kruisselbrink LD, Martin KL, Megeny M, Fowles JR, Murphy RJL. Physical and psychomotor functioning of females the morning after consuming low to moderate quantities of beer. Journal of Studies on Alcohol. 2006;67:416–420. doi: 10.15288/jsa.2006.67.416. [DOI] [PubMed] [Google Scholar]
- Lieber CS. Gender differences in alcohol metabolism and susceptibility. In: Wilsnack RW, Wilsnack SC, editors. Gender and alcohol: Individual and social perspectives. New Brunswick, NJ: Publications Division, Rutgers Center of Alcohol Studies; 1997. pp. 77–89. [Google Scholar]
- Madden PAF, Heath AC, Martin NG. Smoking and intoxication after alcohol challenge in women and men: Genetic influences. Alcoholism: Clinical and Experimental Research. 1997;21:1732–1741. [PubMed] [Google Scholar]
- Mallett KA, Lee CM, Neighbors C, Larimer ME, Turrisi R. Do we learn from our mistakes? An examination of the impact of negative alcohol-related consequences on college students’ drinking patterns and perceptions. Journal of Studies on Alcohol. 2006;67:269–276. doi: 10.15288/jsa.2006.67.269. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCaul ME, Turkkan JS, Svikis DS, Bigelow GE. Alcohol and secobarbital effects as a function of familial alcoholism: Extended intoxication and increased withdrawal effects. Alcoholism: Clinical and Experimental Research. 1991;15:94–101. doi: 10.1111/j.1530-0277.1991.tb00524.x. [DOI] [PubMed] [Google Scholar]
- Morzorati SL, Ramchandi VA, Flury L, Li TK, O’Connor S. Self-reported subjective perception of intoxication reflects family history of alcoholism when breath alcohol levels are constant. Alcoholism: Clinical and Experimental Research. 2002;26:1299–1306. doi: 10.1097/01.ALC.0000025886.41927.83. [DOI] [PubMed] [Google Scholar]
- Muraven M, Collins RL, Morsheimer ET, Shiffman S, Paty JA. The morning after: Limit violations and the self-regulation of alcohol consumption. Psychology of Addictive Behaviors. 2005;19:253–262. doi: 10.1037/0893-164X.19.3.253. [DOI] [PubMed] [Google Scholar]
- Newlin DB, Pretorious MB. Sons of alcoholics report greater hangover symptoms than sons of nonalcoholics: A pilot study. Alcoholism: Clinical and Experimental Research. 1990;14:713–716. doi: 10.1111/j.1530-0277.1990.tb01231.x. [DOI] [PubMed] [Google Scholar]
- Perkins HW. Surveying the damage: A review of research on the consequences of alcohol misuse in college populations. Journal of Studies on Alcohol, Suppl. 2002;14:91–100. doi: 10.15288/jsas.2002.s14.91. [DOI] [PubMed] [Google Scholar]
- Piasecki TM, McCarthy DE, Fiore MC, Baker TB. Alcohol consumption, smoking urge, and the reinforcing effects of cigarettes: An ecological study. Psychology of Addictive Behaviors. 2008;22:230–239. doi: 10.1037/0893-164X.22.2.230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Piasecki TM, Sher KJ, Slutske WS, Jackson KM. Hangover frequency and risk for alcohol use disorders: Evidence from a longitudinal high-risk study. Journal of Abnormal Psychology. 2005;114:223–234. doi: 10.1037/0021-843X.114.2.223. [DOI] [PubMed] [Google Scholar]
- Randall CL, Roberts JS, Del Boca FK, Carroll KM, Connors GJ, Mattson ME. Telescoping of landmark events associated with drinking: A gender comparison. Journal of Studies on Alcohol. 1999;60:252–260. doi: 10.15288/jsa.1999.60.252. [DOI] [PubMed] [Google Scholar]
- Reynolds B, Patak M, Shroff P, Penfold RB, Melanko S, Duhig AM. Laboratory and self-report assessments of impulsive behavior in adolescent daily smokers and nonsmokers. Experimental and Clinical Psychopharmacology. 2007;15:264–271. doi: 10.1037/1064-1297.15.3.264. [DOI] [PubMed] [Google Scholar]
- Roehrs T, Yoon J, Roth T. Nocturnal and next-day effects of ethanol and basal level of sleepiness. Human Psychopharmacology. 1991;6:307–311. [Google Scholar]
- Rohsenow DJ, Howland J, Minsky SJ, Greece J, Almeida A, Roehrs TA. The Acute Hangover Scale: A new measure of immediate hangover symptoms. Addictive Behaviors. 2007;32:1314–1320. doi: 10.1016/j.addbeh.2006.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sher KJ, Walitzer KS, Wood PK, Brent EE. Characteristics of children of alcoholics: Putative risk factors, substance use and abuse, and psychopathology. Journal of Abnormal Psychology. 1991;100:427–448. doi: 10.1037//0021-843x.100.4.427. [DOI] [PubMed] [Google Scholar]
- Slutske WS, Piasecki TM, Hunt-Carter EE. Development and initial validation of the Hangover Symptoms Scale: Prevalence and correlates of hangover in college students. Alcoholism: Clinical and Experimental Research. 2003;27:1442–1450. doi: 10.1097/01.ALC.0000085585.81711.AE. [DOI] [PubMed] [Google Scholar]
- Span SA, Earleywine M. Familial risk for alcoholism and hangover symptoms. Addictive Behaviors. 1999;24:121–125. doi: 10.1016/s0306-4603(98)00002-1. [DOI] [PubMed] [Google Scholar]
- Wall TL, Horn SM, Johnson ML, Smith TL, Carr LG. Hangover symptoms in Asian Americans with variants in the aldehyde dehydrogenase (ALDH2) gene. Journal of Studies on Alcohol. 2000;61:13–17. doi: 10.15288/jsa.2000.61.13. [DOI] [PubMed] [Google Scholar]
- Wall TL, Shea SH, Luczak SE, Cook TAR, Carr LG. Genetic associations of alcohol dehydrogenase with alcohol use disorders and endophenotypes in white college students. Journal of Abnormal Psychology. 2005;114:456–465. doi: 10.1037/0021-843X.114.3.456. [DOI] [PubMed] [Google Scholar]
- Wechsler H, Nelson TF. Binge drinking and the American college student: What’s five drinks? Psychology of Addictive Behaviors. 2001;15:287–291. doi: 10.1037//0893-164x.15.4.287. [DOI] [PubMed] [Google Scholar]
- White AM, Kraus CL, Flom JD, Kestenbaum LA, Mitchell JR, Shah K, Swatzwelder HS. College students lack knowledge of standard drink volumes: Implications for definitions of risky drinking based on survey data. Alcoholism: Clinical and Experimental Research. 2005;29:631–638. doi: 10.1097/01.alc.0000158836.77407.e6. [DOI] [PubMed] [Google Scholar]
- Wiese JG, Shlipak MG, Browner WS. The alcohol hangover. Annals of Internal Medicine. 2000;132:897–902. doi: 10.7326/0003-4819-132-11-200006060-00008. [DOI] [PubMed] [Google Scholar]
- Yokoyama M, Yokoyama A, Yokoyama T, Funazu K, Haman G, Kondo S, Yamashita T, Nakamura H. Hangover susceptibility in relation to aldehyde dehydrogenase-2 genotype, alcohol flushing, and mean corpuscular volume in Japanese workers. Alcoholism: Clinical and Experimental Research. 2005;29:1165–1171. doi: 10.1097/01.alc.0000172457.62535.ee. [DOI] [PubMed] [Google Scholar]