Abstract
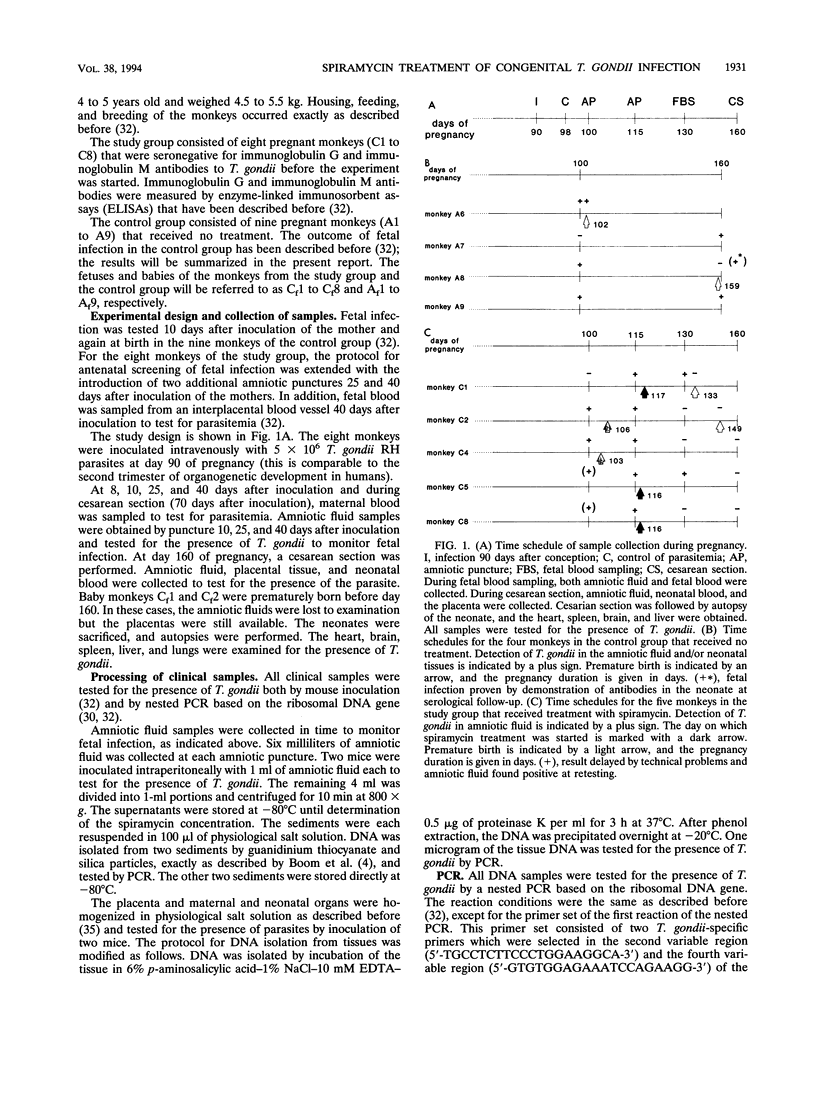
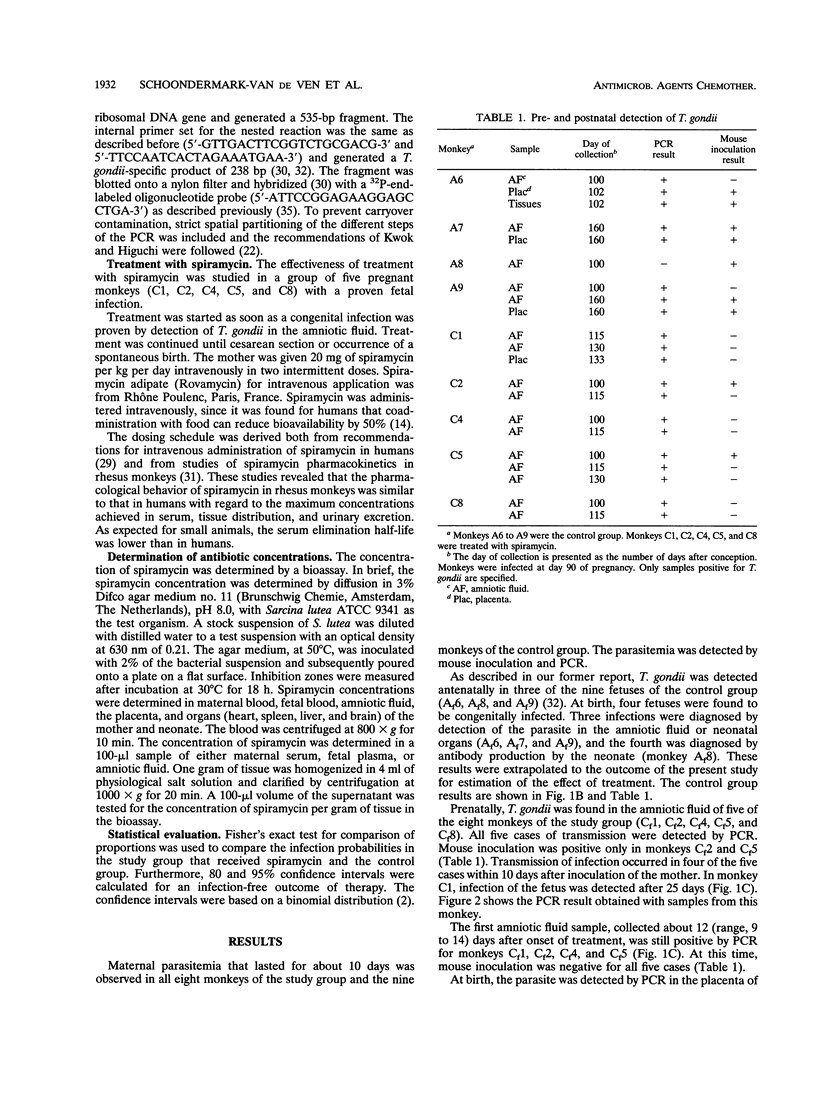
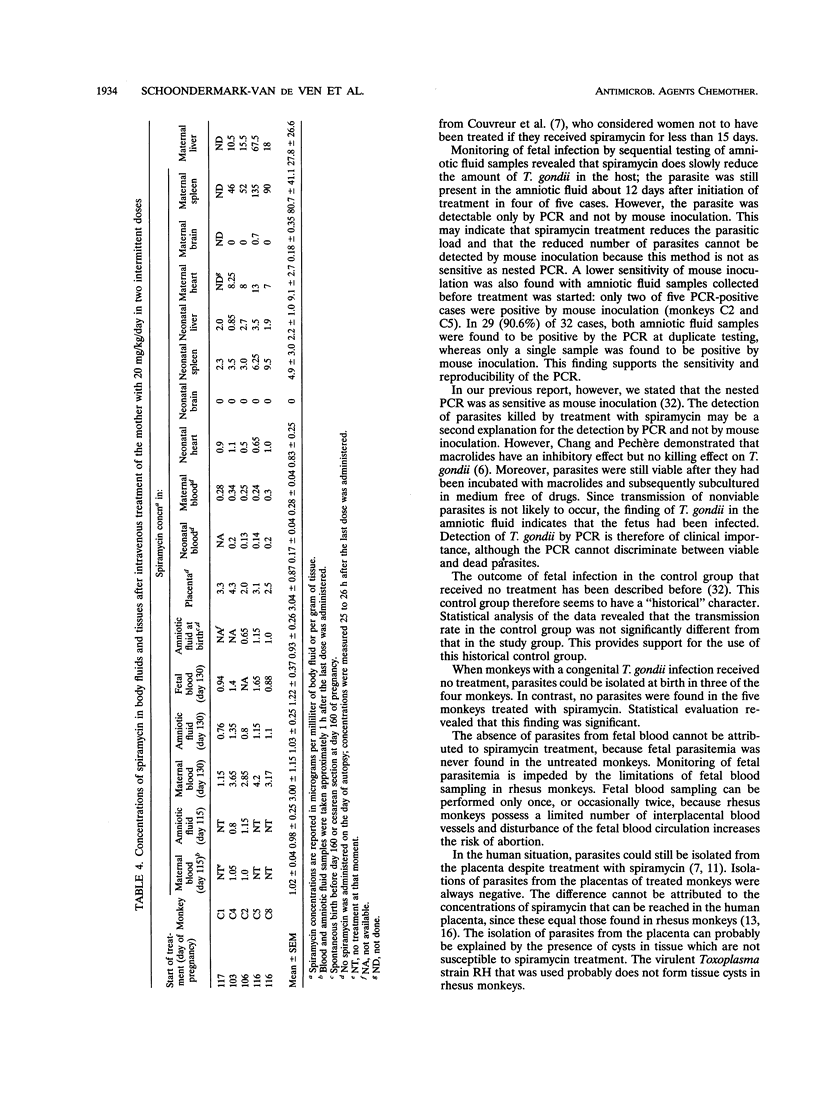
The effectiveness of spiramycin for the treatment of rhesus monkey fetuses congenitally infected with Toxoplasma gondii was studied. Eight monkeys were infected at day 90 of pregnancy. This is comparable to the second trimester of organogenetic development in humans. Transmission of infection was found prenatally in five of the eight monkeys by detection of the parasite in the amniotic fluid. Treatment with spiramycin (20 mg/kg/day in two intermittent doses given intravenously) was started as soon as fetal infection was proven and was continued until birth. Nine to 14 days after initiation of treatment, the parasite was still detectable in amniotic fluid samples from four of these five cases. However, the parasite was detected only by PCR and not by mouse inoculation. T. gondii was also detected only by PCR in the placenta of one monkey that delivered prematurely. This monkey received spiramycin treatment for only 2 weeks. In the four monkeys that received treatment for about 7 weeks, the parasite was not present at birth in the placenta nor in amniotic fluid or neonatal organs. Spiramycin accumulates mainly in maternal tissues. Although concentrations in neonatal tissue were found to be 5 to 28 times higher than the corresponding concentrations in neonatal serum, the concentrations in neonatal tissue were still 11 to 16 times lower than those found in the mothers. However, no spiramycin was found in the fetal brains. Early treatment with spiramycin may prevent transmission of infection to the fetus but most probably cannot interrupt an existing brain infection, which is the most severe outcome of congenital toxoplasmosis in humans.
Full text
PDF



Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Araujo F. G., Shepard R. M., Remington J. S. In vivo activity of the macrolide antibiotics azithromycin, roxithromycin and spiramycin against Toxoplasma gondii. Eur J Clin Microbiol Infect Dis. 1991 Jun;10(6):519–524. doi: 10.1007/BF01963942. [DOI] [PubMed] [Google Scholar]
- Boom R., Sol C. J., Salimans M. M., Jansen C. L., Wertheim-van Dillen P. M., van der Noordaa J. Rapid and simple method for purification of nucleic acids. J Clin Microbiol. 1990 Mar;28(3):495–503. doi: 10.1128/jcm.28.3.495-503.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chamberland S., Kirst H. A., Current W. L. Comparative activity of macrolides against Toxoplasma gondii demonstrating utility of an in vitro microassay. Antimicrob Agents Chemother. 1991 May;35(5):903–909. doi: 10.1128/aac.35.5.903. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang H. R., Pechère J. C. In vitro effects of four macrolides (roxithromycin, spiramycin, azithromycin [CP-62,993], and A-56268) on Toxoplasma gondii. Antimicrob Agents Chemother. 1988 Apr;32(4):524–529. doi: 10.1128/aac.32.4.524. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Couvreur J., Desmonts G., Thulliez P. Prophylaxis of congenital toxoplasmosis. Effects of spiramycin on placental infection. J Antimicrob Chemother. 1988 Jul;22 (Suppl B):193–200. doi: 10.1093/jac/22.supplement_b.193. [DOI] [PubMed] [Google Scholar]
- Couvreur J., Thulliez P., Daffos F., Aufrant C., Bompard Y., Gesquière A., Desmonts G. In utero treatment of toxoplasmic fetopathy with the combination pyrimethamine-sulfadiazine. Fetal Diagn Ther. 1993 Jan-Feb;8(1):45–50. doi: 10.1159/000263746. [DOI] [PubMed] [Google Scholar]
- Daffos F., Forestier F., Capella-Pavlovsky M., Thulliez P., Aufrant C., Valenti D., Cox W. L. Prenatal management of 746 pregnancies at risk for congenital toxoplasmosis. N Engl J Med. 1988 Feb 4;318(5):271–275. doi: 10.1056/NEJM198802043180502. [DOI] [PubMed] [Google Scholar]
- Derouin F., Nalpas J., Chastang C. Mesure in vitro de l'effet inhibiteur de macrolides, lincosamides et synergestines sur la croissance de Toxoplasma gondii. Pathol Biol (Paris) 1988 Dec;36(10):1204–1210. [PubMed] [Google Scholar]
- Desmonts G., Couvreur J. Congenital toxoplasmosis. A prospective study of 378 pregnancies. N Engl J Med. 1974 May 16;290(20):1110–1116. doi: 10.1056/NEJM197405162902003. [DOI] [PubMed] [Google Scholar]
- Forestier F., Daffos F., Rainaut M., Desnottes J. F., Gaschard J. C. Suivi thérapeutique foetomaternel de la spiramycine en cours de grossesse. Arch Fr Pediatr. 1987 Aug-Sep;44(7):539–544. [PubMed] [Google Scholar]
- Frydman A. M., Le Roux Y., Desnottes J. F., Kaplan P., Djebbar F., Cournot A., Duchier J., Gaillot J. Pharmacokinetics of spiramycin in man. J Antimicrob Chemother. 1988 Jul;22 (Suppl B):93–103. doi: 10.1093/jac/22.supplement_b.93. [DOI] [PubMed] [Google Scholar]
- Garin J. P., Paillard B. Toxoplasmose expérimentale de la souris. Activité comparée de: clindamycine, midécamycine, josamycine, spiramycine, pyriméthamine-sulfadoxine, et triméthoprime-sulfaméthoxazole. Ann Pediatr (Paris) 1984 Nov;31(10):841–845. [PubMed] [Google Scholar]
- Garin J. P., Pellerat J., Maillard, Woehrle R., Hezez Bases théoriques de la prévention par la spiramycine de la toxoplasmose congénitale chez la femme enceinte. Presse Med. 1968 Dec 7;76(48):2266–2266. [PubMed] [Google Scholar]
- Harris C., Salgo M. P., Tanowitz H. B., Wittner M. In vitro assessment of antimicrobial agents against Toxoplasma gondii. J Infect Dis. 1988 Jan;157(1):14–22. doi: 10.1093/infdis/157.1.14. [DOI] [PubMed] [Google Scholar]
- Hohlfeld P., Daffos F., Thulliez P., Aufrant C., Couvreur J., MacAleese J., Descombey D., Forestier F. Fetal toxoplasmosis: outcome of pregnancy and infant follow-up after in utero treatment. J Pediatr. 1989 Nov;115(5 Pt 1):765–769. doi: 10.1016/s0022-3476(89)80660-2. [DOI] [PubMed] [Google Scholar]
- Horvath C., Tangapregassom A. M., Tangapregassom M. J., Trecul M., Boucher-Ehrensperger M., Compagnon A., Petter C. Pathogenesis of limb and facial malformations induced by pyrimethamine in the rat. Acta Morphol Hung. 1988;36(1-2):53–61. [PubMed] [Google Scholar]
- Jacobs L. Toxoplasma and toxoplasmosis. Adv Parasitol. 1967;5:1–45. doi: 10.1016/s0065-308x(08)60374-7. [DOI] [PubMed] [Google Scholar]
- Kwok S., Higuchi R. Avoiding false positives with PCR. Nature. 1989 May 18;339(6221):237–238. doi: 10.1038/339237a0. [DOI] [PubMed] [Google Scholar]
- Leport C., Vilde J. L., Katlama C., Regnier B., Matheron S., Saimot A. G. Failure of spiramycin to prevent neurotoxoplasmosis in immunosuppressed patients. JAMA. 1986 May 2;255(17):2290–2290. doi: 10.1001/jama.1986.03370170054013. [DOI] [PubMed] [Google Scholar]
- Mas Bakal P., Veld N in'T Postponed spiramycin treatment of acute toxoplasmosis in white mice. Trop Geogr Med. 1965 Sep;17(3):254–260. [PubMed] [Google Scholar]
- Nguyen B. T., Stadtsbaeder S. Comparative effects of cotrimoxazole (trimethoprim-sulphamethoxazole), pyrimethamine-sulphadiazine and spiramycin during avirulent infection with Toxoplasma gondii (Beverley strain) in mice. Br J Pharmacol. 1983 Aug;79(4):923–928. doi: 10.1111/j.1476-5381.1983.tb10537.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoondermark-Van de Ven E., Galama J., Camps W., Vree T., Russel F., Meuwissen J., Melchers W. Pharmacokinetics of spiramycin in the rhesus monkey: transplacental passage and distribution in tissue in the fetus. Antimicrob Agents Chemother. 1994 Sep;38(9):1922–1929. doi: 10.1128/aac.38.9.1922. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schoondermark-Van de Ven E., Melchers W., Galama J., Camps W., Eskes T., Meuwissen J. Congenital toxoplasmosis: an experimental study in rhesus monkeys for transmission and prenatal diagnosis. Exp Parasitol. 1993 Sep;77(2):200–211. doi: 10.1006/expr.1993.1077. [DOI] [PubMed] [Google Scholar]
- Stray-Pedersen B. Treatment of toxoplasmosis in the pregnant mother and newborn child. Scand J Infect Dis Suppl. 1992;84:23–31. [PubMed] [Google Scholar]
- van de Ven E., Melchers W., Galama J., Camps W., Meuwissen J. Identification of Toxoplasma gondii infections by BI gene amplification. J Clin Microbiol. 1991 Oct;29(10):2120–2124. doi: 10.1128/jcm.29.10.2120-2124.1991. [DOI] [PMC free article] [PubMed] [Google Scholar]




