Abstract
Purpose
The purpose of this Phase II randomized-controlled trial was to evaluate the safety and effect of administering several doses of lycopene to men with clinically localized prostate cancer, on intermediate endpoint biomarkers implicated in prostate carcinogenesis.
Methods
Forty-five eligible men with clinically localized prostate cancer were supplemented with 15, 30 or 45 mg of lycopene or no supplement from biopsy to prostatectomy. Compliance to study agent, toxicity, changes in plasma lycopene, serum steroid hormones, PSA and tissue Ki-67 were analyzed from baseline to completion of intervention.
Results
Forty-two of forty-five five subjects completed the intervention for approximately 30 days from the time of biopsy until prostatectomy. Plasma lycopene increased from baseline to post treatment in all treatment groups with greatest increase observed in the 45 mg lycopene-supplemented arm compared to the control arm without producing any toxicity. Overall, subjects with prostate cancer had lower baseline levels of plasma lycopene similar to those observed in previous studies in men with prostate cancer. Serum free testosterone decreased with 30 mg lycopene supplementation and total estradiol increased significantly with 30 mg and 45 mg supplementation from baseline to end of treatment, with no significant increases in serum PSA or tissue Ki-67. These changes were not significant compared to the control arm for this sample size and duration of intervention.
Conclusions
Although antioxidant properties of lycopene have been hypothesized to be primarily responsible for its beneficial effects, our study suggests that other mechanisms mediated by steroid hormones may also be involved.
Keywords: lycopene, prostate cancer, steroid hormones and PSA
Introduction
The American Cancer Society estimates that there will be about 218,890 new cases of prostate cancer (CaP) in the United States in 2007 and about 27,050 men will die of this disease.1 The initiation and progression of CaP is a multi-step process including several intermediate steps and may involve a complex series of both exogenous and endogenous factors.2–4 Although it is clear that clinical CaP incidence and mortality vary greatly between populations, the frequency of latent CaP is evenly distributed among populations, suggesting that external factors such as diet and other lifestyle factors are important in the transformation from latent into more aggressive clinical cancer.2–5 Recent epidemiological and laboratory studies have suggested that several nutrients, including lycopene, can reduce risk of prostate and other cancers.6–8 Lycopene is the most prevalent carotenoid in the Western diet and the most abundant carotenoid in human serum. It is a non-provitamin A carotenoid that ranks highest among major natural carotenoids in its capacity for quenching singlet oxygen and scavenging free radicals, and distributed primarily in the fatty tissue, liver, plasma and skin.8
Epidemiological studies have observed that populations with high intake of dietary lycopene have lower risk of CaP.9–14 While prospective and case control studies have shown lycopene to be significantly lower in serum and tissue of cancer patients than in controls,11,15–18 results of a large nested case-control study, found no association between serum lycopene and CaP.19 This variability in the experimental data obtained in these epidemiological studies may be related to lycopene source, exposure misclassification, lack of a dose response and other confounding lifestyle factors such as obesity, use of tobacco and alcohol, other dietary differences, varying standardization of quantities and compositions of lycopene, geographical location and genetic risk factors. Given these caveats, result based on epidemiological evidence should be interpreted with caution.
In vitro data have consistently shown that lycopene modulates cell cycle progression, proliferation,20 has an inhibitory effect on DNA synthesis.21 initiating up-regulation of gap-junction proteins and a reduction of local androgen signaling,22 impact IGIF-1 signaling,23 antioxidant24 and induction of apoptotic cell death,25 indicating that isoflavones are promising chemopreventive agents, with several cellular effects which are both genomic and non-genomic. On the other hand, lycopene has also been observed to up-regulate the expression of urokinase plasminogen activator that is known to be metastatic to the bone.26 Several laboratories have examined the effects of lycopene in prostate carcinogenesis in rodent models,25,27–30 observing that lycopene metabolism was modulated by androgens,27,30 as castrated rats accumulated twice the liver lycopene as compared to intact controls,27 interfering with local testosterone activation. Prostatic IGF-I and IL-6 expression was also found to be down-regulated by lycopene.28 A few clinical trials have reported reduction of tumor volume,31–32 and lower prostate specific antigen33–34 with lycopene supplementation. To date, the results of the initial early clinical trials appear promising, although they have included various lycopene preparations and relatively short and varying duration of interventions (ranged from 12 mg/day for 8 weeks to 150 mg/day for 7 days) and men at various stages of CaP, utilizing both intermediate and surrogate biomarkers to evaluate chemoprevention efficacy.
Collectively, these earlier findings support a hypothesis that lycopene may play a role in the modulation of prostate carcinogenesis. The specific aim of the Phase II randomized-controlled trial was to recruit and randomize men, with clinically localized CaP to receive various doses (15, 30 and 45 mg/day) of a standardized lycopene supplement (Lyc-O-MatoTM 15 mg soft gel capsules (LycoRed Natural Products Industries, Ltd. (Beer-Sheva, Israel)) vs. a control arm consuming a diet without this supplement in the pre-surgical period prior to radical prostatectomy and observing the effectiveness of the study agent in producing an increase in (a) plasma levels of lycopene and corresponding (b) modulation of steroid hormones (decrease in free testosterone, increase in sex-hormone-binding globulin and total estradiol) and (c) reduction or stabilization in serum total PSA and (d) tissue Ki-67, a nuclear antigen and molecular marker known to be associated with the progression of cancer. In addition, our aim was to evaluate (e) compliance to study agent and (f) dose-related toxicity. Our overall goal was to determine the best dose of lycopene that could be used in a future phase II randomized placebo-controlled clinical trial to examine the safety and effectiveness of lycopene, in addition to exploring the potential mechanism of action of lycopene in prostate carcinogenesis.
Materials and Methods
This was a controlled, randomized clinical trial conducted in a cohort of men recruited from member institutions of the Moffitt CCOP Research Base, approved by the institutional review boards at these institutions. Men between the ages of 45 and 80 with histologically proven localized CaP, from biopsy specimens with no prior or current therapy for CaP or history of cancer except non-melanoma skin cancer, scheduled for prostatectomy between 4 and 6 weeks after registration were eligible to participate in the study. Patients, who received neoadjuvant hormonal therapy, vegans and/or nutritional supplement users, as ascertained by baseline food records, were excluded from the study. Subjects with a known history of hepatic and/or renal disease, prostatitis, and urinary tract infection within 30 days of registration or with a Body Mass Index greater than 32 Kg/m2 were excluded from the study.
Upon determination of eligibility and the granting of informed consent, patients were registered using a telephone based registration and randomization system41 determined by a pre-set algorithm. These assignments were stratified by Gleason score. Subjects were assigned to one of four arms: the intervention arm providing supplementation with lycopene supplied by Healthy Origins, Pittsburgh, Pennsylvania in the form of Lyc-O-MatoTM 15 mg soft gel capsules (LycoRed Natural Products Industries, Ltd. (Beer-Sheva, Israel), containing a natural tomato extract of standardized-content lycopene suspended in olive oil. Participants randomized to Arm 1–3 and instructed to consume 1 (Arm 1, 15 mg), 2 (Arm 2, 30 mg) or 3 (Arm 3, 45 mg) capsules daily. Subjects randomized to the control group received no supplementation. To avoid possible confounding due to Vitamin/mineral deficiencies and prevent the use of other non-standardized supplements, which may contain lycopene or other large doses of antioxidants, a standard formulation containing 100% USRDA for Vitamins (Pan American Lab Company, Miami, Florida—Multi Vita formula) was provided by the investigators to subjects in all groups, including the control group, during the entire study period. The duration of the intervention was from biopsy to prostatectomy (minimum of 4 and maximum of 6 weeks from biopsy/baseline), depending on duration between biopsy and prostatectomy. Subjects provided baseline demographic, anthropometric, medical and family history of cancer, alcohol, tobacco use and nutritional history including nutritional supplement use. Participants completed a weekly Two-Day Food Records to verify compliance to diet and instruction to avoid lycopene-rich foods. Diet records were analyzed using the University of Minnesota Nutrition Data System-Research version for analysis of nutrient composition at the Arizona Diet and Behavioral Assessment Center (www.azdiet-behavior.azcc.arizona.edu). Participants completed a daily Study Agent Intake and Symptom Log. An 85% compliance to supplements and completion of intake and symptom logs was required.
Non-fasting blood samples were drawn for analysis of (a) serum PSA (baseline and end of study); (b) serum free testosterone, total estradiol and SHBG [Extraction, chromatography, radioimmunoassay(RIA)] at baseline and end of study; (c) safety markers comprehensive metabolic panel (CMP), (Spectrophotometry, ion selective electrode (ISE) Hexokinase) and a complete blood count (CBC) (Electronic cell sizing sorting cytometry/microscopy) at LabCorp Diagnostic Laboratories in Tampa, Florida and (d) analysis of plasma total lycopene using HPLC, an extraction procedure developed by Craft Technologies, Inc (Wilson, North Carolina). Immunohistochemistry (Ki-67) was performed on paraffin embedded sections from prostate biopsies and prostatectomy tissues with prostate adenocarcinoma for evaluation of change in proliferation. Ki-67 antibody (clone MIB-1, DakoCytomation, Carpinteria, CA) was used at a dilution of 1:50. To enhance antigen retrieval citrate buffer was used. The antigen antibody reaction was detected using DAB chromogen. Change in percentage of Ki-67 positive tumor cells was evaluated. Although, we had initially planned to evaluate other tissue biomarkers including apoptosis, due to competition for representative prostate tissue sample from biopsy cores (diagnosis vs. research), we utilized an order of biomarkers to be examined (Ki-67, Apoptotic Index).
To evaluate and ensure subject safety, any change in medical condition and use of concomitant medications were monitored throughout the study period. All safety and compliance data were collected at baseline and end of study period. All adverse events (AEs) were reported on the Adverse Event CRF regardless of whether or not related to study drug. The severity of the events was determined using the NCI Common Terminology Criteria (CTC) for Adverse Events version 2.0 (CTCAE) (http://ctep.info.nih.gov). All AEs, including laboratory abnormalities that in the opinion of the study physicians are clinically significant, were followed according to good medical practices, and documented.
Statistical Methods
At the conclusion of the study, ANOVA was used to compare the four group mean change of plasma lycopene levels, serum steroid hormone levels, total PSA and tissue Ki-67 expression. Dunnett’s Tests for comparisons of multiple treatment arms against the control were also performed and ninety-five percent confidence intervals for the differences of these group means changes were formed. Paired t tests were, in addition, used to compare post-treatment versus pre-treatment changes for each group for plasma lycopene concentrations, serum steroid hormones and serum total PSA levels. These tests were two-sided at 0.05 significant levels. Although compliance was monitored, we employed “intent to treat principle” in all group comparisons. Subjects were analyzed according to the group into which they were randomized without regard to compliance or actual diet. Additional analyses have been done to compare apoptotic index and proliferative marker (Ki-67) at end of study by Dunnett’s Tests. Finally, the correlation between treatment-associated changes in plasma lycopene and changes in surrogate marker of disease progression (serum PSA), were obtained by Spearman’s non-parametric correlation method. In addition, we examined the possible role of age, smoking, alcohol use, and family history of cancer, presence of HGPIN, stage of disease and history of BPH on change plasma levels of lycopene. Categorical variables were compared by Pearson’s chi-square test. The continuous variables were tested by ANOVA for the differences in means. Prior to unblinding, the incidence of toxicity was evaluated. All the analysis was implemented in SAS version 9.
Results
Of men diagnosed with localized CaP, between the years 2004–2006, forty five (45) men met the eligibility criteria, consented and were consecutively admitted to the study. Forty two (42) men completed the intervention and were able to provide complete data pre- and post treatment including serum and plasma for analysis. Three subjects dropped out of the study including 1 from the placebo group and 2 from the lycopene-treated group. Reasons for dropping out of the study included cancellation of surgery (1 treatment arm) and 2 (1 control and 1 treatment arm) withdrew as these subjects did not wish to continue on study protocol. A 93.3% participant retention rate was achieved in the subjects recruited.
Initial comparison of baseline demographic variables such as age, race, and anthropometrics measurements such as height, weight body mass index (BMI), smoking history, family history of cancer and personal history of benign prostatic hyperplasia is displayed in Table 1. Although no significant differences were observed in the two groups on these variables, notably, overall, 66% of CaP patients were former or current smokers and had a mean BMI >25.
Table 1.
Demographic characteristics of subjects at baseline.
| Characteristics | Lycopene/15 mg | Lycopene/30 mg | Lycopene/45 mg | Control Group | P value |
|---|---|---|---|---|---|
| N | 10 | 10 | 14 | 11 | |
| Age(years) | 60.94(+/−7.05) | 57.54(+/−7.29) | 59.98(+/−6.46) | 60.30(+/−6.54) | 0.9358 |
| Weight(lbs) | 186.05(+/−19.90) | 193.37(+/−29.32) | 198.57(+/−26.17) | 181.56(+/−22.08) | 0.8341 |
| Height(in) | 68.95(+/−1.74) | 70.10(+/−3.41) | 67.58(+/−12.16) | 69.64(+/−3.27) | 0.9393 |
| BMI (lbs/in) | 27.52(+/−2.85) | 27.51(+/−2.09) | 28.11(+/−2.91) | 26.24(+/−1.95) | 0.3773 |
| Ethnicity | 0.6843 | ||||
| Hispanic | 1(10.00%) | 1(10.00%) | 0(0.00%) | 1(8.33%) | |
| Non-Hispanic | 9(90.00%) | 9(90.00%) | 14(100.00%) | 11(91.67%) | |
| Race | 0.1661 | ||||
| White | 9(90.00%) | 7(70.00%) | 13(92.86%) | 11(100.00%) | |
| Black | 0(0.00%) | 2(20.00%) | 1(7.14%) | 0(0.00%) | |
| Other | 1(10.00%) | 1(10.00%) | 0(0.00%) | 0(0.00%) | |
| Former or Current Smoker | 0.7785 | ||||
| yes | 7(70.00%) | 8(80.00%) | 8(57.14%) | 7(63.64%) | |
| no | 3(30.00%) | 2(20.00%) | 6(42.86%) | 4(36.36%) | |
| Former or Current Alcohol | 0.1999 | ||||
| yes | 6(60.00%) | 8(80.00%) | 5(35.71%) | 6(54.55%) | |
| no | 4(40.00%) | 2(20.00%) | 9(64.29%) | 5(45.45%) | |
| Family History of Cancer | 0.1465 | ||||
| yes | 10(100.00%) | 10(100.00%) | 14(100.00%) | 9(81.82%) | |
| no | 0(0.00%) | 0(0.00%) | 0(0.00%) | 2(18.18%) | |
| History of Benign Prostatic hyperplasia | 0.1389 | ||||
| yes | 7(70.00%) | 9(90.00%) | 14(100.00%) | 9(81.82%) | |
| no | 3(30.00%) | 1(10.00%) | 0(0.00%) | 2(18.18%) |
P value: ANOVA tests for the continuous variables and Fisher’s exact test for the categorical variables.
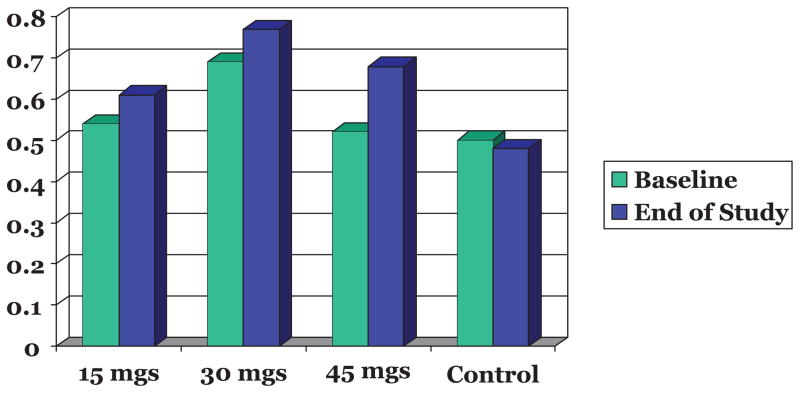
Subjects in all groups reported similar average intake of macronutrients and micronutrients at baseline and intake of these nutrients did not differ significantly between groups during the intervention. No significant changes in anthropometric variables such as weight and BMI were observed during the study period. Changes in plasma total lycopene levels (Table 2) from baseline to end of intervention were analyzed. Plasma lycopene increased with increasing dose of lycopene supplementation, with a maximum increase noted in the 45 mg supplemented group, compared to the plasma levels in the control arm where a decrease in plasma lycopene was observed (Fig. 1).
Table 2.
Plasma lycopene levels from biopsy to prostatectomy.
| Variable | Lycopene 15 mg (N = 10) |
Lycopene 30 mg (N = 10) |
Lycopene 45 kg (N = 14) |
Placebo Group (N = 11) |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | P* | Pre-treatment | Post-treatment | P* | Pre-treatment | Post-treatment | P* | Pre-treatment | Post-treatment | P* | |
| Plasma Total Lycopene umol/L | 0.54 (+/−0.16) | 0.61 (+/−0.16) | 0.324 | 0.69 (+/−0.39) | 0.77 (+/−0.22) | 0.555 | 0.52 (+/−0.20) | 0.68 (+/−0.16) | 0.229 | 0.50 (+/−0.20) | 0.48 (+/−0.26) | 0.706 |
P* paired t test comparing mean at baseline vs. final week within each group.
Figure 1.
Change in Plasma Lycopene (umol/L) levels from Baseline to post intervention by groups.
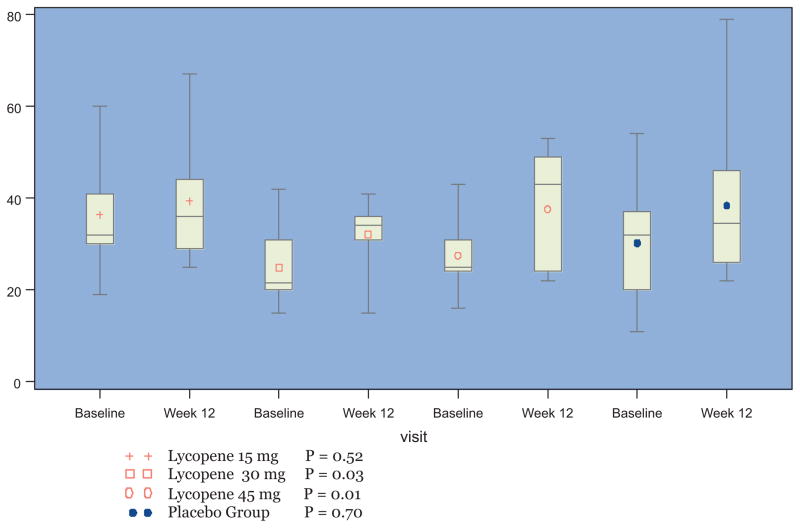
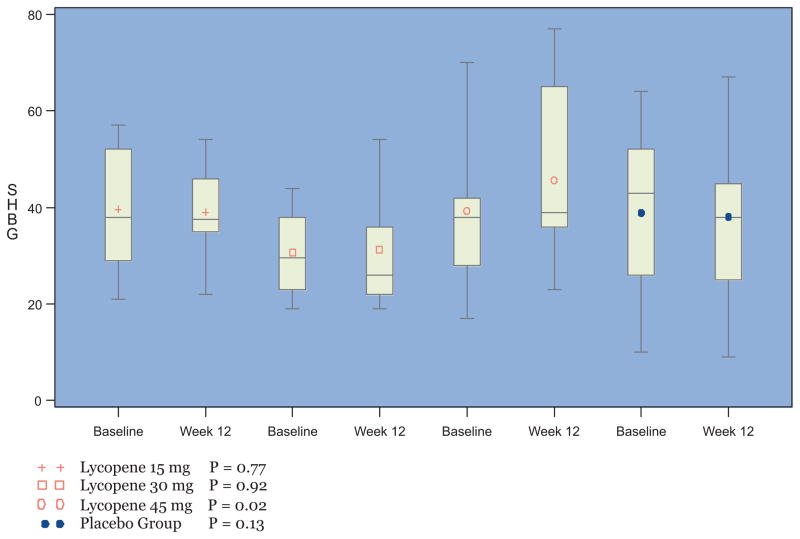
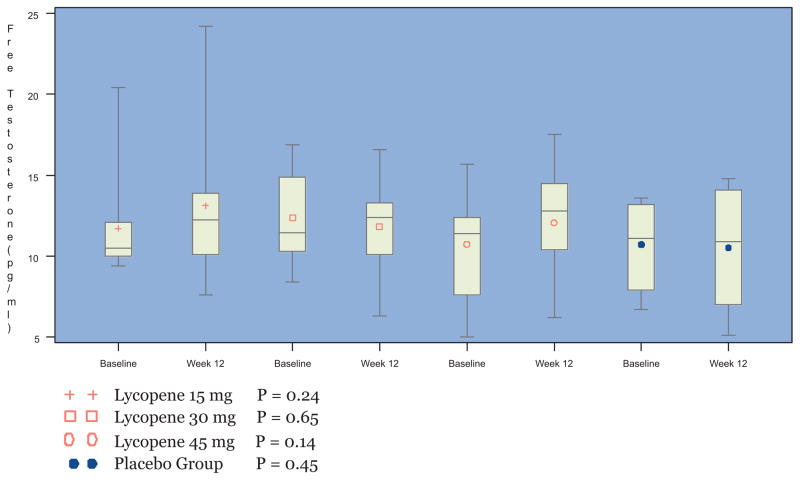
The baseline and final concentrations of serum free testosterone, SHBG and total estradiol for the four groups are displayed in Table 3. At the 30 mg lycopene dose level, a moderate decrease in mean free testosterone and a significant increase in mean plasma estradiol (Fig. 2) was observed [24.90 (+/−7.94) to 32.30 (+/−7.93), P = 0.02]. In addition, significant increase in serum SHBG [39.31 (+/−16.04) to 45.67 (+/−19.83), P = 0.022] (Fig. 3) and total estradiol [27.54 pmol/L (SD 7.82) to 37.64 pmol/L (SD12.65) [P = 0.006] was observed in the 45 mg/day lycopene supplemented group with no significant change in serum testosterone (Fig. 4). However, serum testosterone and SHBG levels in the control group remained unchanged.
Table 3.
Change in Serum Steroid Hormone Concentrations and Surrogate markers of Proliferation (PSA) from biopsy to prostatectomy.
| Variable | Lycopene 15 mg (N = 10) |
Lycopene 30 mg (N = 10) |
Lycopene 45 kg (N = 14) |
Placebo Group (N = 11) |
Lycopene arms vs. Placebo |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre- treatment | Post- treatment | P* | Pre- treatment | Post- treatment | P* | Pre- treatment | Post- treatment | P* | Pre- treatment | Post- treatment | P* | P** | |
| Total Estradiol pmo/L | 36.40 (+/−12.49) | 39.44 (+/−14.24) | 0.5155 | 24.90 (+/−7.94) | 32.30 (+/−7.93) | 0.0261 | 27.54 (+/−7.82) | 37.64 (+/−12.65) | 0.006 | 30.27 (+/−12.52) | 38.40 (+/−17.15) | 0.22 | 0.70 |
| SHBG nmol/L | 39.60 (+/−13.187) | 39.00 (+/−9.72) | 0.7654 | 30.70 (+/−8.67) | 31.33 (+/−12.26) | 0.9237 | 39.31 (+/−16.04) | 45.67 (+/−19.83) | 0.022 | 38.91 (+/−16.48) | 38.09 (+/−16.90) | 0.65 | 0.13 |
| Free testoster- one (pg/ml) | 11.71 (+/−3.24) | 13.12 (+/−5.00) | 0.2379 | 12.37 (+/−2.69) | 11.82 (+/−3.18) | 0.6487 | 10.75 (+/−3.45) | 12.07 (+/−3.72) | 0.135 | 10.72 (+/−2.44) | 10.53 (+/−3.44) | 0.85 | 0.45 |
| Total PSAng/dl | 6.46 (+/−2.74) | 6.70 (+/−3.39) | 0.5398 | 5.86 (+/−2.45) | 6.47 (+/−4.19) | 0.7355 | 5.97 (+/−4.00) | 6.39 (+/−3.46) | 0.55 | 5.48 (+/−3.38) | 5.12 (+/−1.86) | 0.73 | 0.28 |
P* paired t test comparing mean at baseline vs. final week within each group.
P** anova test result.
Figure 2.
Change in Mean Serum Total Estradiol (pmo/L) and Standard Deviations from baseline to post treatment by group.
Figure 3.
Change in Mean Serum SHBG (nmol/L) and Standard Deviations from baseline to post treatment by group.
Figure 4.
Change in Mean Serum free Testosterone (pg/ml) and Standard Deviations from baseline to post treatment by group.
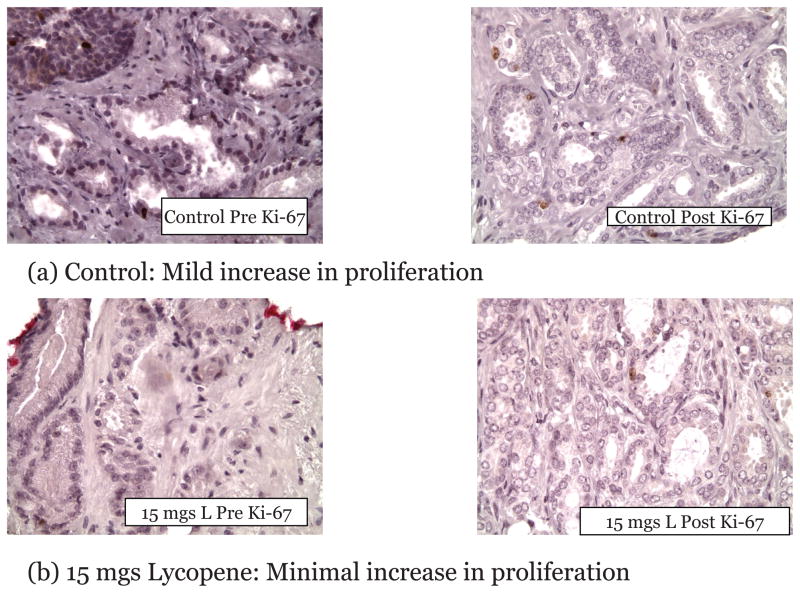
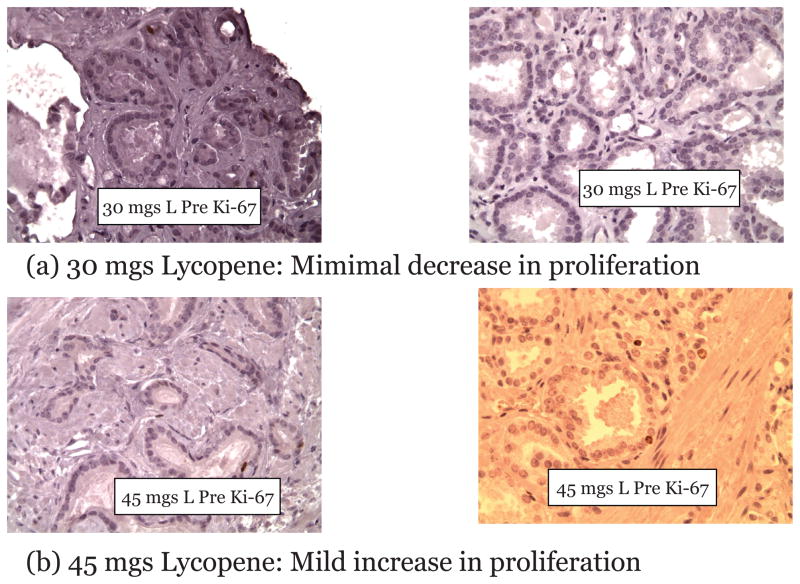
The baseline and final concentrations of serum total Prostate Specific Antigen (PSA) in the three treatment arms compared to the control arm is displayed in Table 3. All changes observed in the treated arms compared to control arm were not statistically significant. Evaluation to compare proliferative index in tumor biopsy to prostatectomy before and after receiving lycopene supplementation compared to controls was completed. The proliferative index measured by Ki-67 staining ranged between 0–7 percent in the cancer cells in all groups at baseline. Nineteen (19) of the 42 patients had matching post-surgical biopsy and histology specimens available for comparative analysis. Others were not included due to unavailability of baseline biopsy sample or inadequate staining of initial biopsy samples. The mean difference between groups receiving the lycopene supplementation observed a lower percentage of cells expressing Ki-67 compared to the control group (Table 4). Notably, 75% of subjects in the 30 mg lycopene supplemented group had a decrease in percent of cells expressing Ki-67 compared to the subjects in the control group where a 100% of the subjects observed an increase (Figs. 5 and 6).
Table 4.
Tissue Ki-67% (Post Intervention) by Group.
| Arm | Number of Observations | Mean Ki-67(%) | SD |
|---|---|---|---|
| Lycopene 15 mgs | 8 | 2.63 | 1.41 |
| Lycopene 30 mgs | 10 | 3.51 | 1.43 |
| Lycopene 45 mgs | 11 | 3.64 | 1.9 |
| Control | 11 | 4.22 | 1.86 |
Figure 5.
Example of Change in Ki-67 expression from Baseline to Post intervention in a subject in the (a) Control arm and (b) 15 mgs Lycopene supplemented arm.
Figure 6.
Example of Change in Ki-67 expression from Baseline to Post intervention in a subject in the (a) 30 mgs and (b) 45 mgs Lycopene supplemented arm.
All anticipated and unanticipated, grades I to III, constitutional, dermatological, gastrointestinal (GI), metabolic and pain symptoms of adverse events (AEs) were documented on all subjects throughout the study period as displayed in Table 5. With the exception of 1 grade III AE (15 mg supplemented arm) determined to be unrelated to agent provided in the study, all other adverse events were grade I events in all groups. The reported Grade III event reported in the subject in the 15 mg dose group was gastrointestinal (indigestion) that lasted 10 days. Treatment was discontinued and restarted when symptoms resolved. Subject continued on the study without further incidence. Other grade I adverse events reported included gastrointestinal symptoms such as nausea, alteration in taste which were reported by 2 subjects (45 mg) and metabolic/laboratory changes in serum glucose, total proteins or albumin, ALT, increase in sodium, hyperphosphatomia and hyper and hypocalcemia, which were observed in all groups including the control arm, considered possibly related to study agent.
Table 5.
Adverse Events by Group, Grade, Anticipated, Causality and Symptoms.
| Treatment Group | Lycopene 15 mg |
Lycopene 30 mg |
Lycopene 45 mg |
Control Group |
|||||
|---|---|---|---|---|---|---|---|---|---|
| Category | Number of Subjects | Number of Events | Number of Subjects | Number of Events | Number of Subjects | Number of Events | Number of Subjects | Number of Events | P value** |
| ALL Adverse Events | 6 | 9 | 5 | 9 | 6 | 14 | 6 | 9 | |
| By Grade | 0.21 | ||||||||
| Grade 1 | 5 | 8 | 5 | 9 | 6 | 14 | 6 | 9 | |
| Grade 2 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Grade 3 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | |
| By Causality | 0.38 | ||||||||
| Unrelated | 2 | 2 | 1 | 1 | 0 | 0 | 1 | 1 | |
| Unlikely | 2 | 2 | 2 | 6 | 4 | 9 | 2 | 5 | |
| Possible | 3 | 4 | 1 | 1 | 4 | 4 | 3 | 3 | |
| Probable | 1 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | |
| By Expected | 0.12 | ||||||||
| Expected | 4 | 7 | 5 | 9 | 4 | 10 | 6 | 9 | |
| Unexpected | 0 | 0 | 0 | 0 | 3 | 3 | 0 | 0 | |
| By Symptom | 0.43 | ||||||||
| Endocrine | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | |
| Gastrointestinal | 1 | 1 | 0 | 0 | 2 | 3 | 0 | 0 | |
| Metabolic | 5 | 8 | 5 | 9 | 5 | 11 | 6 | 9 | |
P value: number of the episodes of adverse events, comparing all four Treatment groups.
Discussion
In this phase II trial, evaluation of the effectiveness of intervention was based on the magnitude of change in plasma levels of lycopene in the various doses of lycopene-supplemented groups compared to the control group and a corresponding stabilization or reduction in surrogate and intermediate endpoint biomarkers of proliferation (total PSA, Ki-67) and modulation of steroid hormones (free testosterone, estradiol and SHBG) that could be achieved, while preventing toxicities. In this phase II trial, we were able to demonstrate that in a cohort of men with localized CaP, compliance to a daily regimen of supplements and diet could be achieved, while maintaining weekly diet and symptom records and attendance to follow up visits, interviews and blood draws to monitor compliance, safety and toxicity. The retention rate of 93.3% indicates that this cohort was highly motivated and willing to participate in chemoprevention trials. Compliance to study agent is observed by the increase in plasma lycopene that was achieved in the lycopene-treated group compared to men in the control arm, although these increases were not significant. In addition, compliance to dietary restriction of lycopene-rich foods was observed by the unchanged, plasma levels of lycopene observed in the control group.
The mean level of lycopene consumption from foods reported in studies of the American population has been estimated at just over 8 mg/d.35 We established the selection of the product (purified standardized product) and dose of lycopene (15 mg, 30 mg and 45 mg, compared to a group with no supplementation) based on these previous data and including the 30 mg and 45 mg dose to be substantially higher than usual intake as the therapeutic dose levels. We observed the greater increases in plasma lycopene with increasing dose, with maximum increase in plasma observed with the 45 mg dose. No toxicities were observed at these dose levels compared to the control arm, including the 30 mg and 45 mg dose levels. However, these changes in plasma lycopene were not statistically significant compared to controls for this period of intervention and sample size. Similarly, previous intervention studies report that the relation between dietary intake of lycopene and plasma lycopene concentrations to be weak, with plasma rarely statistically correlated with estimated dietary intake.43–44 Other than in animal models, serial measurements of plasma lycopene has been observed in one other clinical trial in men with biochemical relapsed CaP where with a dose escalation from 15–120 mg/day, plasma lycopene levels increased, and plateaued after 3 months36 indicative of a trend towards stabilization of bio-available concentration of lycopene with time.
In addition, the mean plasma levels of lycopene in disease free populations has been reported to vary by gender, with plasma lycopene in males averaging 0.82 μmol/L35 compared to plasma lycopene of 0.56 μmol/L (SD 0.34–0.92) observed in the lowest quintile of men with CaP with aggressive disease.18 The range of baseline plasma lycopene observed in our clinical trial was similar to those observed in these studies, with plasma lycopene ranging from 0.50–0.69 μmol/L in the pre-surgical period prior to prostatectomy, thus validating the results of these previous findings.18 Although previous findings have implicated several factors that can potentially contribute to plasma lycopene levels in this cohort, multiple regression analysis of our data failed to demonstrate contributory effects of disease markers such as family history of cancer, stage of disease, presence of HGPIN, BPH history, PSA, in addition to environmental variables such as intake of other antioxidants, physical activity, BMI, smoking and alcohol use. Similarly, a large proportion of the variance in plasma lycopene, examined in previous studies has been unexplained and establishes the need for further investigations into the pharmacokinetics of lycopene in long-term clinical trials in disease-free, high-risk and cancer patient populations.
Notably, at the therapeutic dose levels a significant increase in serum estradiol and SHBG was observed with no significant changes in serum free testosterone. Androgens are required for the normal development and function of the prostate and are also necessary for the progression of CaP known to stimulate the proliferation, invasion and metastases.38 Administration of hormonal therapies has been shown to produce CaP in rodents, while castration and estrogen therapy can reduce the risk of CaP.27 It is clear from recent studies that testosterone and estradiol are dominant contributors of androgenic and estrogenic activity. Furthermore, sex-hormone binding globulin, because it binds to and sequesters testosterone and estradiol, controls the bioavailability of these steroid hormones. The high affinity of SHBG for binding to testosterone, also influences the circulatory levels of these sex steroids, their biodisposal to target cells as well as their mutual balance.25 Synergism between androgens and estrogens may be an important factor in the etiology of CaP.38–42 To date the modulation of steroid hormones by lycopene has not been examined nor reported in clinical trials with standardized lycopene supplementation, including measurement of plasma lycopene levels. In a single report of an epidemiological study which correlated intake of tomato products measured using food frequency questionnaire, a decrease in IGF-1 levels was observed.23 However, blood lycopene levels were not quantified in this study. Hirsh K et al.43 reported that each of the tested carotenoids (lycopene, phytoene, phytofluene, and beta-carotene) inhibited cancer cell proliferation induced by either E (2) and that the inhibition of cell growth by lycopene was accompanied by slow down of cell-cycle progression from G1 to S phase. These results suggest that dietary carotenoids inhibit estrogen signaling of both 17 beta-estradiol and can potentially attenuate their deleterious effect in hormone-dependent malignancies. Previous laboratory data27 identified alterations in lycopene metabolism in response to androgen ablation in rats, suggesting a possible diet/endocrine interaction. They observed that castrated rats accumulated approximately twice as much hepatic lycopene as did intact controls. In a later study, they27 observed that testosterone may indirectly modulate hepatic lycopene accumulation via influences on lipoprotein synthesis and secretion by liver and that a reduction in circulating androgens would thereby result in decreased lycopene metabolism and clearance, leading to an increase in tissue lycopene concentrations.27 Certainly, future large randomized case-control trials should confirm the potential specific pathways involved in lycopene metabolism mediated by steroid hormones, which might provide new dimensions not only to the prevention but also the treatment of CaP. Similar to observations with lycopene, steroid hormones also appear to alter the tissue concentrations of other antioxidants such as tocopherol, thought to modify CaP risk.44–46
Prostate Specific Antigen, or KLK3, is a member of the human kallikrein family of serine proteases secreted by the prostatic epithelium and the epithelial lining of the periurethral glands. Traditionally, clinicians have relied on PSA as a prognostic indicator in addition to tumor stage, grade and volume.47–49 Because the serum level of PSA is proportional to the volume of tumor present, PSA has become an integral part of disease management in this population with localized CaP. Freedland et al. reported that with each 2 point increase in PSA, the risk of biochemical progression increased approximately two-fold,48 even in men with PSA <10 ng/ml. Studies have demonstrated that a greater PSA level was associated with significantly more adverse pathological features and biochemical progression.47–49 Although we were targeting the intervention in men with CaP post biopsy and prior to radical prostatectomy, we included PSA as a surrogate marker of proliferation in this clinical trial.
Additionally, we examined tissue changes in Ki67 expression, which provides an accurate estimate of growth fraction and in many studies has been found to be a predictor of outcome for patients treated with radical prostatectomy. Ki-67 had significantly different levels of expression in normal prostate tissue, high-grade prostatic intraepithelial neoplasia (HGPIN), and prostate adenocarcinoma (PCA) and could potentially be applied as an intermediate endpoint biomarker of chemoprevention efficacy, although this has not been previously monitored serially in chemoprevention trials.50 Although, the sample size was small, and adequate pre/post treatment tissue was unavailable in our study, we observed a greater reduction in the percentage of cells expressing Ki-67 in the lycopene treated arms compared to the control arm.
Conclusion
Based on the compliance to supplementation achieved, toxicity profile, trends observed in the modulation of surrogate and intermediate endpoint biomarkers in this phase II clinical trial and absence of an increase in surrogate markers of proliferation, we recommend a standardized dose of 30 mg of lycopene formulation for a future definitive clinical trial, powered to examine the safety and effectiveness of lycopene in inhibiting the progression of CaP. Although the antioxidant properties of lycopene have been hypothesized to be primarily responsible for its beneficial effects, evidence is accumulating to suggest that other mechanisms may also be involved. Future studies must utilize a combination of validated prognostic biochemical, morphological and molecular intermediate endpoint biomarkers to evaluate chemoprevention efficacy. Until the results from larger well conducted phase III clinical trials have demonstrated efficacy and safety, it is critical for practitioners to exercise caution prior to recommending supplemental doses to their patients for cancer prevention or treatment.
Acknowledgments
The research study was funded by the National Institute of Health—National Cancer Institute U10 CA81920.
References
- 1.Facts and Figures. American Cancer Society; Atlanta, Georgia: 2007. Cancer. [Google Scholar]
- 2.Holmberg L, Bill-Axelson A, Garmo H, Palmgren J, Norlen BJ, Adami HO, Johansson JE. SPCG-4 Study Group. Prognostic markers under watchful waiting and radical prostatectomy. Hematol Oncol Clin North Am. 2006 Aug;20(4):845–55. doi: 10.1016/j.hoc.2006.03.007. [DOI] [PubMed] [Google Scholar]
- 3.Johansson JE, Andren O, Andersson SO, Dickman PW, Holmberg L, Magnuson A, Adami HO. Natural history of early, localized prostate cancer. JAMA. 2004 Jun 9;291(22):2713–9. doi: 10.1001/jama.291.22.2713. [DOI] [PubMed] [Google Scholar]
- 4.Kelloff GJ, Leiberman R, Steele VE, Boone CW, et al. Chemoprevention of Prostate cancer. Eur Urol. 1999;35(5–6):342–50. doi: 10.1159/000019906. [DOI] [PubMed] [Google Scholar]
- 5.Klotz L. Active surveillance versus radical treatment for favorable-risk localized prostate cancer. Curr Treat Options Oncol Review. 2006;7(5):355–62. doi: 10.1007/s11864-006-0003-z. [DOI] [PubMed] [Google Scholar]
- 6.Gester H. The potential role of Lycopene for Human Health. Journal of American College of Nutrition. 1997;16:109–26. doi: 10.1080/07315724.1997.10718661. [DOI] [PubMed] [Google Scholar]
- 7.Stahl W, Sies H. Lycopene: A biologically important carotenoid for humans? Archives of Biochemistry and Biophysics. 1996;336 (1):1–9. doi: 10.1006/abbi.1996.0525. [DOI] [PubMed] [Google Scholar]
- 8.Nguyen ML, Schwartz SJ. Lycopene: Chemical and biological properties. Food Technology. 1999;53(2):38–45. [Google Scholar]
- 9.Giovannuci E. Tomato products, lycopene, and prostate cancer: a review of the epidemiological literature. J Nutr. 2005 Aug;135(8):2030S–1S. doi: 10.1093/jn/135.8.2030S. [DOI] [PubMed] [Google Scholar]
- 10.Giovannuci E. Tomatoes, tomato-based products, lycopene, and cancer: review of the epidemiologic literature. J Natl Cancer Inst. 1999 Feb 17;91(4):317–31. doi: 10.1093/jnci/91.4.317. [DOI] [PubMed] [Google Scholar]
- 11.Giovannuci E, Rimm EB, Liu Y, Stampfer MJ, Willett WC. A prospective study of tomato products, lycopene, and prostate cancer risk. J Natl Cancer Inst. 2002 Mar 6;94(5):391–8. doi: 10.1093/jnci/94.5.391. [DOI] [PubMed] [Google Scholar]
- 12.Wu K, Erdman JW, Schwartz SJ, Platz EA, Leitzmann M, Clinton SK, DeGroff V, Willett WC. Giovannucci E. Plasma and dietary carotenoids, and the risk of prostate cancer: a nested case-control study. Cancer Epidemiol Biomarkers Prev. 2004 Feb;13(2):260–9. doi: 10.1158/1055-9965.epi-03-0012. [DOI] [PubMed] [Google Scholar]
- 13.Etminan M, Takkouche B, Caamano-Isorna F. The role of tomato products and lycopene in the prevention of prostate cancer: a meta-analysis of observational studies. Cancer Epidemiol Biomarkers Prev. 2004 Mar;13(3):340–5. [PubMed] [Google Scholar]
- 14.Jian L, Du C, Lee AH, Binns CW. Do dietary lycopene and other carotenoids protect against prostate cancer? International Journal of Cancer. 2005;113:1010–4. doi: 10.1002/ijc.20667. [DOI] [PubMed] [Google Scholar]
- 15.Rao AV, Fleshner N, Agarwal S. Serum and tissue lycopene and biomarkers of oxidation in prostate cancer patients: a case-control study. Nutr Cancer. 1999;33(2):159–64. doi: 10.1207/S15327914NC330207. [DOI] [PubMed] [Google Scholar]
- 16.Lu QY, Hung JC, Heber D, Go VL, Reuter VE, Cordon-Cardo C, Scher HI, Marshall JR, Zhang ZF. Inverse associations between plasma lycopene and other carotenoids and prostate cancer. Cancer Epidemiol Biomarkers Prev. 2001 Jul;10(7):749–56. [PubMed] [Google Scholar]
- 17.Kirsh VA, Mayne ST, Peters U, Chatterjee N, Leitzmann MF, Dixon LB, Urban DA, Crawford ED, Hayes RB. A Prospective Study of Lycopene and Tomato Product Intake and Risk of Prostate Cancer. Cancer Epidemiology, Biomarkers and Prevention. 2006;15(1):92–8. doi: 10.1158/1055-9965.EPI-05-0563. [DOI] [PubMed] [Google Scholar]
- 18.Gann PH, Ma J, Giovannucci E, Willett W, Sacks FM, Hennekens CH, Stampfer MJ. Lower prostate cancer risk in men with elevated plasma lycopene levels: results of a prospective analysis. Cancer Res. 1999 Mar 15;59(6):1225–30. [PubMed] [Google Scholar]
- 19.Peters U, Leitzmann MF, Chatterjee N, Wang Y, Albanes D, Gelmann EP, Friesen MD, Riboli E, Hayes RB. Serum Lycopene, Other Carotenoids, and Prostate Cancer Risk: A Nested Case-Control Study in the Prostate, Lung, Colorectal and Ovarian Cancer Screening Trial. Cancer Epidemiol Biomarkers Prev. 2007 May;16(5):962–8. doi: 10.1158/1055-9965.EPI-06-0861. [DOI] [PubMed] [Google Scholar]
- 20.Obermuller-Jevic UC, Olano-Martin E, Corbacho AM, Eiserich JP, van der Vliet A, Valacchi G, Cross CE, Packer L. Lycopene inhibits the growth of normal human prostate epithelial cells in vitroJ. NutrNov. 2003;133(11):3356–60. doi: 10.1093/jn/133.11.3356. [DOI] [PubMed] [Google Scholar]
- 21.Barber NJ, Zhang X, Zhu G, Pramanik R, Barber JA, Martin FL, Morris JD, Muir GH. Lycopene inhibits DNA synthesis in primary prostate epithelial cells in vitro and its administration is associated with a reduced prostate-specific antigen velocity in a phase II clinical study. Prostate Cancer Prostatic Dis. 2006;9(4):407–13. doi: 10.1038/sj.pcan.4500895. Epub 2006;Sep 19. [DOI] [PubMed] [Google Scholar]
- 22.Goyal A, Delves GH, Chopra M, Lwaleed BA, Cooper AJ. Prostate cells exposed to lycopene in vitro liberate lycopene-enriched exosomes. BJU Int. 2006 Oct;98(4):907–11. doi: 10.1111/j.1464-410X.2006.06434.x. [DOI] [PubMed] [Google Scholar]
- 23.Chan JM, Stampfer MJ, Giovannucci E, Ma J, Pollak M. Insulin-like growth factor I (IGF-I), IGF-binding protein-3 and prostate cancer risk: epidemiological studies. Growth Horm IGF Res. 2000;10(Suppl A):S32–3. doi: 10.1016/s1096-6374(00)90015-7. [DOI] [PubMed] [Google Scholar]
- 24.Cohen LA. Nutrition and prostate cancer: a review. Ann N Y Acad Sci. 2002 Jun;963:148–55. doi: 10.1111/j.1749-6632.2002.tb04106.x. [DOI] [PubMed] [Google Scholar]
- 25.Tang L, Jin T, Zeng X, Wang JS. Lycopene inhibits the growth of human androgen-independent prostate cancer cells in vitro and in BALB/c nude mice. J Nutr. 2005 Feb;135(2):287–90. doi: 10.1093/jn/135.2.287. [DOI] [PubMed] [Google Scholar]
- 26.Forbes K, Gillette K, Sehgal I. Lycopene increases urokinase receptor and fails to inhibit growth or connexin expression in a metastatically passaged prostate cancer cell line: a brief communication. Exp Biol Med (Maywood) 2003 Sep;228(8):967–71. doi: 10.1177/153537020322800813. [DOI] [PubMed] [Google Scholar]
- 27.Boileau TW, Clinton SK, Zaripheh S, Monaco MH, Donovan SM, Erdman JW. Testosterone and food restriction modulate hepatic lycopene isomer concentrations in male F344 rats. J Nutr. 2001 Jun;131(6):1746–52. doi: 10.1093/jn/131.6.1746. [DOI] [PubMed] [Google Scholar]
- 28.Siler U, Barella L, Spitzer V, Schnorr J, Lein M, Goralczyk R, Wertz K. Lycopene and vitamin E interfere with autocrine/paracrine loops in the Dunning prostate cancer model. FASEB J. 2004 Jun;18(9):1019–21. doi: 10.1096/fj.03-1116fje. Epub. 2004; Apr 14. [DOI] [PubMed] [Google Scholar]
- 29.Herzog A, Siler U, Spitzer V, Seifert N, Denelavas A, Hunziker PB, Hunziker W, Goralczyk R, Wertz K. Lycopene reduced gene expression of steroid targets and inflammatory markers in normal rat prostate. FASEB J. 2005 Feb;19(2):272–4. doi: 10.1096/fj.04-1905fje. Epub 2004 Nov 15. [DOI] [PubMed] [Google Scholar]
- 30.Campbell JK, Stroud CK, Nakamura MT, Lila MA, Erdman JW. Serum testosterone is reduced following short-term phytofluene, lycopene, or tomato powder consumption in F344 rats. J Nutr. 2006 Nov;136(11):2813–9. doi: 10.1093/jn/136.11.2813. [DOI] [PubMed] [Google Scholar]
- 31.Kucuk O, Sakr W, Sarkar FH, et al. Lycopene supplementation in men with localized prostate cancer (Pca) modulates grade and volume of PIN. and tumor, level of serum PSA and biomarkers of cell growth, differentiation and apoptosis. Proc AACR March 1999 [Google Scholar]
- 32.Kucuk O, Sarkar FH, Sakr W, Djuric Z, Pollak MN, Khachik F, Li YW, Banerjee M, Grignon D, Bertram JS, Crissman JD, Pontes EJ, Wood DP. Phase II randomized clinical trial of lycopene supplementation before radical prostatectomy. Cancer Epidemiol Biomarkers Prev. 2001 Aug;10(8):861–8. [PubMed] [Google Scholar]
- 33.Ansari MS, Gupta NP. A comparison of lycopene and orchidectomy vs orchidectomy alone in the management of advanced prostate cancer. BJU Int. 2004 Sep;94(4):678. doi: 10.1111/j.1464-410x.2003.05067_4.x. [DOI] [PubMed] [Google Scholar]
- 34.Ansari MS, Gupta NP. Lycopene: a novel drug therapy in hormone refractory metastatic prostate cancer. Urol Oncol. 2004 Sep–Oct;22(5):415–20. doi: 10.1016/j.urolonc.2004.05.009. [DOI] [PubMed] [Google Scholar]
- 35.Porrini M, Riso P. What are typical lycopene intakes? J Nutr. 2005 Aug;135(8):2042S–5S. doi: 10.1093/jn/135.8.2042S. Review. [DOI] [PubMed] [Google Scholar]
- 36.Clark PE, Hall MC, Borden LS, Miller AA, Hu JJ, Lee WR, Stindt D, D’Agostino R, Lovato J, Harmon M, Torti FM. Phase I–II prospective dose-escalating trial of lycopene in patients with biochemical relapse of prostate cancer after definitive local therapy. Urology. 2006 Jun;67(6):1257–61. doi: 10.1016/j.urology.2005.12.035. [DOI] [PubMed] [Google Scholar]
- 37.Paetau I, Khachik F, Brown ED, Beecher GR, Kramer TR, Chittams J, Clevidence BA. Chronic ingestion of lycopene-rich tomato juice or lycopene supplements significantly increases plasma concentrations of lycopene and related tomato carotenoids in humans. Am J Clin Nutr. 1998 Dec;68(6):1187–95. doi: 10.1093/ajcn/68.6.1187. [DOI] [PubMed] [Google Scholar]
- 38.Parsons JK, Carter HB, Platz EA, Wright EJ, Landis P, Metter EJ. Serum testosterone and the risk of prostate cancer: potential implications for testosterone therapy. Cancer Epidemiol Biomarkers Prev. 2005 Sep;14(9):2257–60. doi: 10.1158/1055-9965.EPI-04-0715. [DOI] [PubMed] [Google Scholar]
- 39.Boileau TW, Clinton SK, Erdman JW., Jr Tissue lycopene concentrations and isomer patterns are affected by androgen status and dietary lycopene concentration in male F344 rats. J Nutr. 2000 Jun;130(6):1613–8. doi: 10.1093/jn/130.6.1613. [DOI] [PubMed] [Google Scholar]
- 40.Carruba G. Estrogens and mechanisms of prostate cancer progression. Ann N Y Acad Sci. 2006 Nov;1089:201–17. doi: 10.1196/annals.1386.027. [DOI] [PubMed] [Google Scholar]
- 41.Adlercreutz H, Mazur W, Bartels P, Elomaa V, Watanabe S, Wahala K, Landstrom M, Lundin E, Bergh A, Damber JE, Aman P, Widmark A, Johansson A, Zhang JX, Hallmans G. Phytoestrogens and prostate disease. J Nutr. 2000 Mar;130(3):658S–9S. doi: 10.1093/jn/130.3.658S. [DOI] [PubMed] [Google Scholar]
- 42.Kumar NB, Cantor A, Allen K, Riccardi D, Besterman-Dahan K, Seigne J, Helal M, Salup, Powsang J. The Specific Role of Isoflavones in Reducing Prostate Cancer Risk. Prostate. 2004;59:2. doi: 10.1002/pros.10362. [DOI] [PubMed] [Google Scholar]
- 43.Hirsch K, Atzmon A, Danilenko M, Levy J, Sharoni Y. Lycopene and other carotenoids inhibit estrogenic activity of 17beta-estradiol and genistein in cancer cells. Breast Cancer Res Treat. 2007 Aug;104(2):221–30. doi: 10.1007/s10549-006-9405-7. Epub 2006;Oct 19. [DOI] [PubMed] [Google Scholar]
- 44.Feingold IB, Longhurst PA, Colby HD. Regulation of adrenal and hepatic alpha-tocopherol content by androgens and estrogens. Biochim Biophys Acta. 1993 Mar 10;1176(1–2):192–6. doi: 10.1016/0167-4889(93)90196-v. [DOI] [PubMed] [Google Scholar]
- 45.Feingold IB, Colby HD. Sex differences in adrenal and hepatic alpha-tocopherol concentrations in rats. Pharmacology. 1992;44(2):113–6. doi: 10.1159/000138880. [DOI] [PubMed] [Google Scholar]
- 46.Hartman TJ, Dorgan JF. Woodson. Effects of long-term alpha-tocopherol supplementation on serum hormones in older men. Prostate. 2001 Jan 1;46(1):33–8. doi: 10.1002/1097-0045(200101)46:1<33::aid-pros1005>3.0.co;2-6. [DOI] [PubMed] [Google Scholar]
- 47.Loeb S, Gonzalez CM, Roehl KA, Han M, Antenor JA, Yap RL, Catalona WJ. Pathological characteristics of prostate cancer detected through prostate specific antigen based screening. The Journal of Urology. 2006;175(3 Pt 1):902–6. doi: 10.1016/S0022-5347(05)00327-7. [DOI] [PubMed] [Google Scholar]
- 48.Freedland SJ, Mangold LA, Walsh PC, Partin AW. The prostatic specific antigen era is alive and well: prostatic specific antigen and biochemical progression following radical prostatectomy. The Journal of Urology. 2005;174(4 Pt 1):1276–1281. doi: 10.1097/01.ju.0000173907.84852.ec. discussion 1281; author reply 1281. [DOI] [PubMed] [Google Scholar]
- 49.Thompson IM, Ankerst DP, Chi C, Goodman PJ, Tangen CM, Lucia MS, Feng Z, Parnes HL, Coltman CA. Assessing prostate cancer risk: results from the Prostate Cancer Prevention Trial. Journal of the National Cancer Institute. 2006;98(8):529–34. doi: 10.1093/jnci/djj131. [DOI] [PubMed] [Google Scholar]
- 50.Mucci NR, Rubin MA, Strawderman MS, Montie JE, Smith DC, Pienta KJ. Expression of Nuclear Antigen Ki-67 in Prostate Cancer Needle Biopsy and Radical Prostatectomy Specimens. Journal of the National Cancer Institute. 2000 Dec 6;92(23):1941–2. doi: 10.1093/jnci/92.23.1941. [DOI] [PubMed] [Google Scholar]