Abstract
Self-efficacy is an important cognitive predictor of substance abuse treatment outcome. While measures of coping self-efficacy are related to substance use relapse in adults, their properties are not well known in adolescent populations. The present study examined 223 adolescents while in treatment for substance abuse and comorbid psychiatric disorders. Responses on the Drug-Taking Confidence Questionnaire (DTCQ; Sklar et al., 1997) were used to construct a 37-item, 5-factor version for use with adolescents. Exploratory and confirmatory factor analysis identified the following factors: 1) Negative Situations, 2) Social/Drugs, 3) Pleasant Emotions, 4) Testing Personal Control, and 5) Physical/Intimate. Data preliminarily support the construct, concurrent, and predictive validity of the revised instrument.
Keywords: Psychometrics, Self-efficacy, Comorbidity, Relapse prevention
Coping self-efficacy has been found to influence the course of treatment and patterns of relapse in the addictive behaviors. Defined by Bandura (1995) as “one's capacity to organize and execute courses of action required to manage prospective situations,” self-efficacy has been incorporated in cognitive-behavioral models of relapse to drug and alcohol use (Marlatt & Gordon, 1985; Brown & Ramo, 2006) as a key determinant of behavior in potential relapse situations. Within this theoretical framework, self-efficacy increases the probability that one will resist urges and pressures to relapse after a period of abstinence. Indeed, coping self-efficacy has been found to predict adult relapse to alcohol (e.g., Solomon & Annis, 1990) and drug (e.g., Burling, Reilly, Moltzen, & Ziff, 1989) use after treatment.
Cognitive-behavioral relapse theory assumes that characteristics of situations common to an individual's use prior to treatment represent characteristics that will pose the highest risk for relapse following treatment (Marlatt & Gordon, 1985). Based on the frequency of pretreatment substance use situations, Marlatt and colleagues (1985) developed a taxonomy of situations that pose the greatest risk for relapse among adults. The taxonomy identified two domains of situations, including intrapersonal (58% of Marlatt's original sample) and intrapersonal situations (42%). Within intrapersonal situations, situations were further classified as unpleasant emotions (UE; 37%), physical discomfort (PD; 4%), positive emotional states (PE; 6%), testing personal control (TPC; 4%) and urges and temptations to use (UT; 7%). Within interpersonal situations, specific conditions included interpersonal conflict (CO; 15%), social pressure (SP; 24%) and pleasant times with others (PT; 3%).
Currently, little is known regarding the appropriateness of adult-derived relapse classification systems to the patterns of adolescent addictive relapse. Previous work suggests that the majority of episodes of adult addiction relapse are associated with situations of anger or frustration, social pressure to drink, or interpersonal conflict (Marlatt & Gordon, 1985). In contrast, social situations comprise the majority of adolescent addictive relapse situations while negative affect is reported by few adolescents (Myers & Brown, 1990; Brown, Stetson & Beatty, 1989). In a recent study on the relapse characteristics of comorbid adolescents (Anderson, Frissell, Brown, in press), the vast majority (85%) of youth relapsed in the presence of others, when the main activity was socializing with peers. In the context of Marlatt's taxonomy for relapse situations, comorbid youth relapsed most often in situations involving temptation or to enhance a positive emotional state. Findings of developmental differences in relapse contexts suggest that adult-derived constructs may not accurately represent the adolescent experience, and highlight the importance of examining adolescent-specific factors (such as self-efficacy) that influence the addictive behavior relapse process.
As a key cognitive factor in the relapse process for adults (Marlatt, 1985), the measurement of coping self-efficacy has paralleled the situations most commonly associated with relapse in adults. The Drug-Taking Confidence Questionnaire (DTCQ; Sklar, Annis & Turner, 1997) is a measure of coping self-efficacy in 50 different situations. The measure has an 8-factor first order structure corresponding to Marlatt's (1985) taxonomy of high-risk situations, and a 3-factor second order structure consisting of Negative Situations (UE, PD, CO), Positive Situations (PE, PT) and Temptation Situations (TPC, UT, SP; Sklar et al., 1997). Research with the Inventory of Drinking Situations (IDS; Annis, 1982), a measure of likelihood of drinking in high risk situations, has suggested that while Marlatt's taxonomy seems to capture the major domains of potential relapse circumstances, there may be variation in how the most common situations cluster across adult samples (Cannon, Leeka, Patterson, & Baker, 1990; Isenhart, 1991).
The literature on coping self-efficacy with adults suggests that total scores across all areas predict the probability that an individual will relapse, and that the profile of subscores should predict the most likely types of situations associated with a return to substance use (Burling et al., 1989; Sklar et al., 1997; Solomon & Annis, 1990). Among youth, there is less evidence on the relationship between self-efficacy and relapse. Some recent work has suggested that self-efficacy may not serve as strong a protective role in relapse as it does for adults. Burleson and Kaminer (2005) examined self-efficacy as it related to drug use behavior in youth who were randomized to either a cognitive-behavior treatment or psychoeducation group therapy. They found that confidence to resist urges to use as measured by the Situational Confidence Questionnaire, a measure of situational self-efficacy paralleling the 3-factor structure of the DTCQ (negative affect situations, positive affect situations, urges and temptation situations), was not associated with substance use during treatment 3 months or 6 months following treatment in either condition. This finding may suggest that the structure of self-efficacy situations as applied to adults may not be appropriate for teens.
Ongoing neuromaturation throughout adolescence, concurrent with increasing exposure to alcohol and other drug use, suggest that substance-related cognitions would change in structure throughout development. For example, Christiansen, and colleagues (Christiansen, Goldman & Brown, 1985; Christiansen, Goldman, & Inn, 1982) found that responses to the Alcohol Expectancy Questionnaire-Adolescent Form, a measure of outcome expectations for drinking among youth, became more “crystallized” throughout adolescence because there was a tendency toward more homogenous item content within factors as adolescents matured into young adulthood. This suggested that expectancies about the effects of alcohol become more distinct as adolescents gain experience with alcohol. Thus, increased experience with alcohol use situations and/or quit attempts over time may lead adolescent beliefs about their ability to resist use to become more refined and solidified.
The present study represents an effort to better understand adolescent coping self-efficacy by examining the factor structure and psychometric properties of the Drug-Taking Confidence Questionnaire in a clinical sample of substance use disordered (SUD) youth. The factor structure of the DTCQ was expected to be less diversified (fewer factors) in this adolescent sample than the eight factor structure found for adults. To examine this possibility, confirmatory and exploratory factor analyses were used to test the number of factors present in our adolescent sample.
The Youth Relapse Model (Brown & Ramo, 2006), a form of Marlatt's cognitive-behavioral model of relapse adapted for youth, emphasizes the importance of motivation in the process of relapse, in that a desire to abstain is necessary in order to engage in a coping response when faced with a high risk situation. Because those youth who are motivated to abstain are more likely to use coping responses when faced with these situations, the model suggests their levels of coping self efficacy will also increase as they encounter more situations in which they do not use. As such, construct validity was examined in relation to situational appraisal variables on the Adolescent Relapse Coping Questionnaire (ARCQ; Myers & Brown, 1996) and motivation to abstain from using alcohol or drugs. Coping self-efficacy was predicted to have a negative relationship with the urge to use in a high-risk situation, and positive relationships with the importance of not using in the situation, the likelihood of avoiding use in the situation, and motivation to abstain from one's drug of choice. Discriminant validity was examined in relation to variables (ethnicity and family relationship functioning) that were not expected to have an association with situational coping self-efficacy. Concurrent validity was examined in relation to substance use characteristics of adolescents in treatment. Greater use histories were expected to be associated with lower confidence in resisting the urge to use in the future. Finally, predictive validity was assessed in reference to substance use outcomes 6 months after treatment. Since self-efficacy was expected to decrease vulnerability to relapse, higher self-efficacy scores while in treatment were predicted to be associated with more positive use outcomes.
Method
Participants
Participants for this study were 223 adolescents, age 13-17, recruited from four inpatient mental health/substance abuse treatment programs in southern California. The abstinence focused therapy milieu consisted of group, individual, and family therapy to address psychiatric and substance abuse issues. The average length of stay in each of these facilities was 2 weeks. Adolescents were an average age of 15.8 years (SD = 1.2); 50% were female; and a majority (70%) were Caucasian. Almost half (48%) of the participants' parents were married at the time of the first interview, 42% were divorced, 5% separated, 3% single and 2% were unmarried and living with a partner. Demographics, substance use, mental health diagnoses, and drugs of choice for the sample are presented in Table 1.
TABLE 1.
Demographic, Substance Involvement, and Mental Health Disorder Characteristics of Substance Use Disordered Adolescents (N=223)
| Gender | ||
| Male | 51% | |
| Female | 49% | |
| Ethnicity | ||
| Caucasian | 70.0% | |
| Hispanic | 18.3% | |
| African American | 5.8% | |
| Asian | 3.4% | |
| Other | 5.0% | |
| Age | 15.8 (1.2) | |
| Grade | 8.9 (1.2) | |
| Substance Use Diagnosis | ||
| Drug Use Disorder | 92% | |
| Alcohol Use Disorder | 79% | |
| Alcohol & Drug Use Disorder | 72% | |
| Mental Health Diagnosis | ||
| Internalizing and Disruptive | 72% | |
| Disruptive only | 15% | |
| Internalizing only | 9% | |
| SUD-only | 4% | |
| Drug of Choice | ||
| Marijuana | 47% | |
| Stimulants | 31% | |
| Alcohol | 13% | |
| Other Substance | 10% | |
Note. Values for Age and Grade are sample means (standard deviations).
Of the 223 adolescents assessed at intake, 45 did not complete in-person 6 month interviews and thus were not included in predictive validity analyses. We examined included (N=178) and excluded cases to determine any systematic baseline differences. There were no differences between those who had 6-month data compared to those who did not have follow-up data on gender (χ2 (1, N=223) = .55, n.s.), age (t (221) = 1.82, n.s.), ethnicity (χ2 (5, N=223) = .66, n.s.), or grades completed at intake (t (221) = 1.15, n.s.). At intake, those who were missing six month data had more DSM-IV substance dependence symptoms (9.3 vs. 8.1; t (221) = 2.43, p<.05).
Procedure
Consecutive admissions to the hospitals were screened for eligibility, which included presence of a current SUD (either abuse or dependence) in addition to any comorbid DSM-IV Axis I psychiatric disorders. Although not a requirement for participation in the study, co-occurrence of psychiatric disorders with SUDs was present in most of the participants (see Table 1). Adolescents were excluded if they lived more than 50 miles from the research facility, had a head injury with loss of consciousness longer than 2 minutes, exhibited psychotic symptoms prohibiting the acquisition of accurate information, or did not have a parent or guardian to corroborate information. For eligible participants, consent was obtained independently from adolescents and their parents/guardians. Each participant and parent or guardian completed a separate in-person interview while in treatment and six months following treatment. Following completion of both independent interviews, substance use and historical information from the adolescent and parent interviews was composited in a systematic manner to ensure accuracy in reporting. A random sample of 10% of participants completed a urine toxicology screen to verify use reports. With the exception of one case (cocaine), toxicology screens did not identify substances beyond those reported by youth.
Measures
Structured Clinical Interview (Brown, Creamer, & Stetson, 1987)
The clinical interview assesses demographics (e.g., age, sex, ethnicity, socioeconomic status, education, family characteristics), treatment history, and psychosocial functioning (e.g., academics, extracurricular activities, social functioning). Demographic and motivation variables from this interview were used in the present study.
Drug-Taking Confidence Questionnaire (DTCQ; Sklar et al., 1997)
This is a 50-item self-report questionnaire designed to assess self-efficacy in relation to an individual's perceived ability to cope effectively with high-risk for relapse situations. Participants are asked to indicate their drug of choice and rate their confidence that they can resist the urge to use this drug in each of 50 situations, rated on a 6-point scale (20% increments) from 0% (“not at all confident”) to 100% (“very confident”). The measure has been shown to have good psychometric properties for an adult sample (Sklar et al., 1997).
Customary Drinking and Drug Use Record (CDDR; Brown et al., 1998)
This structured interview provides reliable information about quantity, frequency, and patterns of alcohol and other drug consumption, withdrawal, and dependency symptoms (Brown et al., 1998). Variables used in this study were: 1) the average number of alcohol and drug use episodes per month in the 3 months before treatment; 2) the number of alcohol and drug physical withdrawal symptoms in the 3 months prior to treatment; 3) the number of DSM-IV alcohol/drug dependence symptoms; and 4) the total number of different drugs other than alcohol used in the 3 months prior to treatment. For concurrent validity analyses, substance use variables were divided by alcohol and drugs.
At the 6-month follow-up interview, CDDR data were used to classify adolescents by outcome status (see Brown, Vik, & Creamer, 1989) for detailed descriptions of these classifications): Abstainers had no more than one episode of alcohol or other drug exposure in the six months since treatment. Minor relapsers had limited alcohol or drug involvement (less than 3 consecutive days) and no associated problems or DSM-IV dependence symptoms during the 6 months after treatment. Adolescents who had more than 3 consecutive days of use and any associated problems or any dependence symptoms were classified as major relapsers. Major relapsers have been consistently shown to have more severe use patterns compared to minor relapsers in other samples using this classification system (e.g., Brown, D'Amico, McCarthy, & Tapert, 2001; Brown et al., 1994).
Adolescent Relapse Coping Questionnaire (ARCQ; Myers & Brown, 1996)
This reliable and validated questionnaire measures alcohol/drug related coping strategies in two common high risk situations for substance abusing adolescents (Myers & Brown, 1996). The ARCQ assesses primary and secondary appraisal (Folkman & Lazarus, 1988) of two relapse risk situations and use of a variety of coping strategies. Each participant is asked to consider two standard situations (Situation A: social pressure to use, Situation B: emotional distress), and indicate his/her urge to use, importance of not using, self-efficacy, and locus of control for each situation (scored on a 10-point Likert-type scale).
Family Environment Scale (FES; Moos & Moos, 1994)
This instrument measures the social and environmental characteristics of families. Adolescents were asked to rate whether a series of statements were true or false about their families (scored 0/1). For the present study, the Relationship dimension was used, which includes three 9-item scales measuring Cohesion, Expressiveness, and Conflict within families. The FES Relationship Dimension has been shown to predict treatment outcome in an adolescent substance abusing population (Friedman, Terras, & Kreisher, 1995).
Results
Missing Data Imputation
Prior to analyses, the 50 DTCQ items were examined using SPSS v. 14.0 for accuracy of data entry, missing values (range: 0%-5%) and distributional properties for confirmatory and exploratory factor analysis. Of the 223 participants, complete data on all items of the DTCQ were available for 175; there were no missing data on any of the demographic or substance use variables at intake. There were between zero and five missing values on 49 of the 50 DTCQ items. The final item, “If I felt that someone was trying to control me and I wanted to feel more independent,” had missing values on more than 5% of the cases (26 of 223 values). The SPSS Missing Value Analysis module was employed, whereby the DTCQ items were entered as predictors to impute values for missing items. The data imputation procedure yielded complete DTCQ data for all 223 participants. An exploratory factor analysis indicated no differences across analyses conducted on individuals with complete DTCQ data (N = 175) and individuals with complete and imputed data (N = 223). In addition, ten cases were identified through Mahalanobis distance as multivariate outliers with p < .001. Deletion of the ten cases did not affect any of the analyses and thus they were retained in analyses.
Confirmatory Factor Analysis (CFA) on DTCQ scales
A confirmatory factor analysis was conducted using Mplus v.2.13 software (Muthén & Muthén, 1999) to examine the fit of the 8-factor structure of the DTCQ in this sample of adolescents. All analyses were assessed using the maximum likelihood method with robust errors and the Satorra-Bentler chi-square statistic (Satorra & Bentler, 1994) to account for non-normal distribution of data. Assessment of the overall goodness-of-fit of each model was based upon five indices: (a) chi-square goodness-of-fit index; (b) the ratio of the chi-square to the degrees of freedom; (c) the comparative fit index (CFI; Bentler, 1990); (d) the root mean square error of approximation (RMSEA; Browne & Cudek, 1993); and (e) the standardized root mean square residual (SRMR). A cutoff value close to .06 for RMSEA and .08 for SRMR generally support the good fit of a model (Hu & Bentler, 1999). CFI of .90 was used as an adequate cutoff value (Bentler & Bonett, 1980) to limit concerns of Type I error rate when observed indicators are measured at the item level (Marsh, Hau, & Wen, 2004). As shown in Table 2, fit indices indicated a moderately good fitting model, however the previously specified CFI cutoff was not met (X2 = 2078, p<.0001; CFI = .88; RMSEA = .06; SRMR = .06).
TABLE 2.
Fit Indices of Models Tested (N=223)
| Model | X2 (df) | X2 /df | CFI | RMSEA | SRMR |
|---|---|---|---|---|---|
| 8-factor (50 items) | 2078.32* (1147) | 1.8 | .88 | .06 | .06 |
| 5-factor (37 items) | 1126.14* (619) | 1.8 | .91 | .06 | .051 |
| 1-factor (37 items) | 1858.57* (629) | 3.0 | .77 | .09 | .075 |
p< .0001
Because this CFA provided only a moderately good fit of the data, we conducted an Exploratory Factor Analysis (EFA) with the 50 items and then validated the solution with another CFA. Using exploratory factor analysis as a precursor to CFA has been found to be a practical heuristic strategy for model specification and development (Gerbing & Hamilton, 1996). We conducted principle axis factoring with promax rotation using SPSS FACTOR. Oblique rotation was selected based on the original development of the Inventory of Drug Taking Situations (Turner, Annis & Sklar, 1997) and the expectation of significant interscale correlations, in part because youth are less discriminating about alcohol and drug use situations than adults (Christiansen & Goldman, 1983). Of note, varimax (orthogonal) rotation produced the same factors, so the oblique results are presented here.
The number of factors to be retained was determined by scree tests, examination of factor loadings, and interpretability of the solution. Examination of these factors suggested a 5-factor solution. Of the original 50 items, 13 were eliminated due to loadings on multiple factors (i.e., secondary factor loading >.30) or not meeting the criterion of an item factor loading above .40 on any factor. The first factor explained 50% of the variance and each of the remaining four factors explained between 3% and 6% of the variance. As can be seen in Table 2, the final 5-factor solution fit indices fit Hu and Bentler's (1990) combinatorial rules and suggested a good fit for the hypothesized model. The scale names, means, alpha coefficients, and factor loadings for the final 37-item 5-scale measure are reported in Table 3. The PE, TPC, and P/I scales were significantly skewed, while the NS, S/D, TPC, P/I. and total scale scores were significantly kurtotic.
TABLE 3.
Means (standard deviations) and factor loadings of revised Drug-Taking Confidence Questionnaire
| Variable | Factor | ||||
|---|---|---|---|---|---|
| 1 | 2 | 3 | 4 | 5 | |
| Scale 1: Negative Situations (NS); M = 48.45 (24.7); α = .97 | |||||
| If I started to feel guilty about something. | .86 | ||||
| If I felt that I had let myself down. | .85 | ||||
| If I were angry at the way things had turned out. | .85 | ||||
| If I were not getting along well with others at school or at work. | .85 | ||||
| If other people treated me unfairly or interfered with my plans. | .85 | ||||
| If I felt anxious or tense about something. | .85 | ||||
| If I felt that my family was putting a lot of pressure on me or that I couldn't measure up to their expectations. | .84 | ||||
| If someone were dissatisfied with my work or I felt pressured at school or on the job. | .83 | ||||
| If there were fights at home. | .82 | ||||
| If I felt confused about what I should do. | .81 | ||||
| If I were lonely. | .80 | ||||
| If I were depressed about things in general. | .80 | ||||
| If I felt overwhelmed and wanted to escape. | .76 | ||||
| If I felt there was nowhere left to turn. | .76 | ||||
| If I felt tense or uneasy in the presence of someone. | .75 | ||||
| If other people rejected me or didn't seem to like me. | .75 | ||||
| If I were unable to express my feelings to someone. | .71 | ||||
| Scale 2: Social/Drug Situations (S/D); M = 18.80 (12.4); α = .94 | |||||
| If I were out with friends and they kept suggesting we go somewhere and use these drugs. | .85 | ||||
| If I wanted to celebrate with a friend. | .85 | ||||
| If I were with friends and wanted to increase my enjoyment. | .85 | ||||
| If others in the same room were using these drugs and I felt hey expected me to join in. | .83 | ||||
| If I were with a group of people and everyone was using these drugs. | .80 | ||||
| If I began to think how good a rush or high had felt. | .78 | ||||
| If I unexpectedly found some of these drugs or happened to see something that reminded me of these drugs. | .78 | ||||
| If I were in a place where I had bought or used these drugs before. | .74 | ||||
| Scale 3: Positive Emotion (PE); M = 13.84 (5.5); α = .86 | |||||
| If I felt excited about something. | .81 | ||||
| If I were feeling content with my life. | .81 | ||||
| If I were confident and relaxed. | .79 | ||||
| If I were happy. | .71 | ||||
| Scale 4: Testing Personal Control (TPC); M = 12.30 (5.88); α = .87 | |||||
| If I wanted to test out whether I could be in places where these drugs were being used without using any. | .80 | ||||
| If I wanted to find out whether I could use these drugs occasionally without getting hooked. | .79 | ||||
| If I wanted to prove to myself that these drugs were not a problem for me. | .79 | ||||
| If I wanted to see whether I could use these drugs in moderation. | .76 | ||||
| Scale 5: Physical/Intimacy (P/I); M = 12.96 (6.0); α = .79 | |||||
| If I were with an intimate friend and wanted to feel even closer. | .80 | ||||
| If I were having a good time and wanted to increase my enjoyment. | .74 | ||||
| If I wanted to lose weight. | .61 | ||||
| If I wanted to stay awake, be more alert, or be more energetic. | .61 | ||||
Note. Factor loadings from final confirmatory factor model, maximum likelihood estimation, all factor loadings are significant at the p<.05 level
Finally, because of the magnitude of difference between the first and the four subsequent eigenvalues, we considered that a 1-factor solution might also fit the data well. As such, we conducted a CFA specifying a 37-item, 1-factor solution. The factor solution was not as good of a fit as the 5-factor model. Specifically, CFI = 78, RMSEA = .09, and SRMR = .08; consequently, the 5-factor version was used for all subsequent analyses.
DTCQ revised scale validation
Table 4 presents validity analyses for the 37-item, 5-factor version of the DTCQ for the entire sample, and use characteristics for youth whose substance of choice was an illicit drug (n=188) or alcohol (n=27). Spearman's rho was used as a measure of correlation in all validity analyses because DTCQ scale scores and some independent variables were not normally distributed. In order to control for Type I error across multiple analyses, an alpha level of .01 was used for each analysis.
TABLE 4.
Adolescent DTCQ Factor correlations (Spearman's rank) with validation variables by drug of choice
| NS | S/D | PE | TPC | P/I | DTCQ total | |
|---|---|---|---|---|---|---|
| Entire Sample (N = 223) | ||||||
| Urge to use in situation A | -.51* | -.20* | -.38* | -.39* | -.48* | |
| Importance of not using in situation A | .36* | .45* | .31* | .30* | .41* | |
| Liklihood of not using in situation A | .42* | .22* | .35* | .16 | .37* | |
| Urge to use in situation B | -.44* | -.36* | ||||
| Importance of not using in situation B | .25* | .27* | ||||
| Liklihood of not using in situation B | .34* | .34* | ||||
| Motivation | .37* | .47* | .34* | .30* | .19* | .43* |
| Self-esteem | .41* | .11 | .16 | .14 | .18 | .26 |
| Cohesion | .21 | .19 | .20 | .05 | .20 | .25 |
| Expressiveness | .30* | .25 | .22 | .08 | .25 | .31* |
| Conflict | -.16 | -.03 | -.18 | -.02 | -.20 | -.16 |
| Ethnicity (F) | .72 | 1.33 | .87 | .45 | .24 | .50 |
| Drug Sample (n=188) | ||||||
| Motivation to abstain from drugs | .39* | .52* | .38* | .35* | .24* | .46* |
| Drug use episodes /last 3 mos. | -.03 | -.13 | -.08 | -.07 | -.12 | -.08 |
| Drug withdrawal symptoms | -.20* | -.20 | -.04 | -.29* | -.23* | -.20* |
| DSM-IV drug dependence symptoms | -.03 | -.10 | -.05 | -.05 | -.08 | -.05 |
| # drugs used, last 3 mo. | -.10 | -.16 | -.13 | -.17 | -.26* | -.16 |
| Alcohol Sample (n = 27) | ||||||
| Motivation to abstain from alcohol | .47 | .42 | .14 | .32 | .11 | .43 |
| Alcohol use episodes /last 3 mos. | -.46 | -.33 | -.13 | -.24 | -.17 | -.42 |
| Alcohol withdrawal symptoms | -.75* | -.67* | -.50* | -.57* | -.51* | -.75* |
| DSM-IV alcohol dependence symptoms | -.18 | -.09 | -.17 | -.20 | -.32 | -.18 |
p< .01
Note. ANOVAs were used to test whether there were any differences between ethnic groups on the five scales or DTCQ total. Values in the table are F-tests, none of which were significant.
In examining construct validity, Scale 1 (NS) was correlated with appraisal variables from the ARCQ situation in which adolescents find themselves angry and frustrated after a fight with their parents (Situation B), whereas the other four scales were correlated with appraisal variables from a social gathering and drug offering risk situation (Situation A). The total score on the revised 37-item DTCQ was correlated with appraisal variables from both situations. Results showed significant relationships between DTCQ scales and all three appraisal variables in the hypothesized directions. Abstinence motivation was related to all DTCQ scales and the total score in the full sample (rs range: .19 to .47, all p<.01) and in the subsample of teens whose substance of choice was a drug (n=188; rs range: .24 to .52, all p<.01).
Discriminant validity of the DTCQ factors was examined in relation to ethnicity and family cohesion, expressiveness, and conflict. Due to a predominance of Caucasian participants, ethnicity was examined both as a dichotomous variable (Caucasian/non-Caucasian), as well as the original five groups. Regardless of the ethnicity variable used, ethnicity was significantly correlated with neither any of the scales nor the DTCQ total score (F range: .24 to 1.30, all n.s.). The FES Expressiveness scale was associated with self-efficacy in Negative Situations (DTCQ NS scale; rs = .30, p<.01) and the total self-efficacy (DTCQ total score: rs = .31, p<.01).
Considering concurrent criterion validity, all drug use variables were negatively related to DTCQ scales and the full measure. Significant relationships were also seen between drug withdrawal symptoms and the NS (rs = -.20, p<.01), TPC (rs = -.29, p<.01), P/I (rs = -.23, p<.01), and Total scores (rs = -.20, p<.01), and between the number of drugs used in the 3 months prior to treatment and the TPC (rs = -.17, p<.05) scale. Among the adolescents who identified alcohol as their substance of choice (n=27), alcohol use variables were negatively correlated with all scale scores and the full scale score. Significant negative relationships were observed between alcohol withdrawal symptoms and all five scales and the DTCQ Total (rs range: -.50 to.-.75., all p<.01).
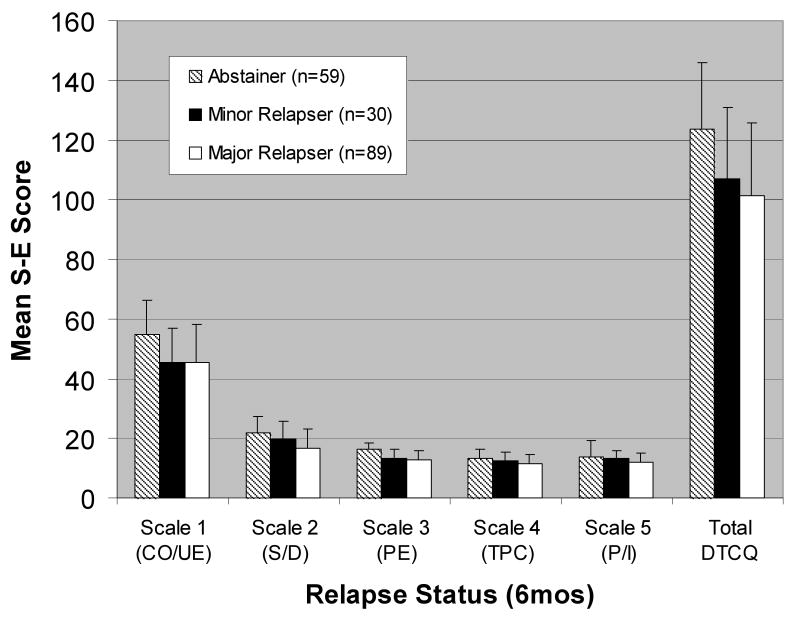
To evaluate predictive validity, separate univariate analyses of variance (ANOVA), using p = .01 to account for multiple analyses, were conducted comparing scores on each scale and the total DTCQ score with the outcome status of adolescents six months after treatment (abstainer, minor relapser, major relapser). Means for each scale and the total score for each of the three relapse categories are presented in Figure 1. As hypothesized, there was a significant linear trend of self-efficacy across the outcome categories for Scale 2 (F(2, 175) = 5.83, p<.05), Scale 3 (F(2, 175) = 13.67, p<.001, and the DTCQ Total score (F(2, 175) = 8.00, p<.01, such that those who went on to abstain had the highest levels of self-efficacy during treatment, followed by minor relapsers and major relapsers. While not showing a significant linear trend, the means for Scales 1, 4, and 5 were in the hypothesized direction.
Figure 1.
Mean situational self-efficacy score as a function of relapse status 6 months after treatment.
Discussion
The present study examined the factor structure and psychometric properties of the adult-based Drug-Taking Confidence Questionnaire (Sklar et al., 1997) in a clinical sample of adolescent substance abusers. A 5-factor, 37-item version was optimal. The factors identified for adolescents were Negative Situations, Social/Drug, Pleasant Emotions, Testing Personal Control, and Physical/Intimacy. This 5-factor model was a better fit for youth compared to the original 8-factor model (Sklar et al, 1997) and a 1-factor model. Present findings provide initial evidence for the validity of the revised DTCQ for SUD adolescents.
The differences in factor structure between the adult and adolescent forms of the DTCQ are consistent with previous literature suggesting that the structure of cognitions associated with alcohol and drug involvement changes as adolescents gain more experience with substance use (e.g., Christiansen et al., 1985; Deas, Riggs, Langenbucher, Goldman, & Brown, 2000; Dunn & Goldman, 1998). The reduced number of factors in the revised DTCQ presented here suggests that situational self-efficacy is less differentiated among adolescents than in previous samples of adults. For example, the Social/Drugs factor, comprised of items from the adult Social Pressure, Urges and Temptations, and Pleasant Times with Others subscales, suggests that adolescents may perceive situations in which they have a desire to use, in which peers and drugs or alcohol are present and in which substances are offered to them as related, and they construct self-efficacy for future use around such experiences. Similarly, the Physical/Intimacy factor may represent that adolescents perceive physical relapse precipitants (i.e., wanting to stay awake, wanting to lose weight), in the same context as those linked to their intimate interactions with others and that their confidence in these physical situations is related to their confidence to resist using in social situations (being with intimate friends, having a good time) rather than other negative physical states that may arise more often in adulthood (e.g., feeling nauseous, having a headache, having trouble sleeping). These results are consistent with studies showing that the immediate risks for teens are social situations paired with strong positive affect, rather than negative situations such as physical problems or conflict (e.g., Brown, Stetson et al., 1989; Brown, Vik et al., 1989).
The 5-factor structure found in this study differs from previous findings in an adolescent sample using the Situational Confidence Questionnaire (Annis & Graham, 1988), a questionnaire measuring situational self-efficacy to cope in drinking-related situations. Kirisci and colleagues (Kirisci & Moss, 1997; Kirisci, Moss & Tarter, 1996) confirmed an 8-factor structure corresponding to Marlatt's high-risk situations in a sample of adolescents. Several factors may account for differences between these findings and those reported here. First, prior studies used confirmatory factor analysis and item response theory to assess the adequacy of an 8-factor model in an adolescent sample. Since exploratory analyses were not conducted in either study with the SCQ, it is not clear whether a 5-factor model would have been a better fit than an 8-factor model in a community sample. Of note, in the present study, an 8-factor model did come close to meeting the model fit criteria; however this solution was not as good a fit as the five-factor model which emerged based on our exploratory factor analysis. Second, the SCQ measures coping self-efficacy to resist drinking rather than drug use, and adolescents may have had more varied experiences with drinking, corresponding to a more detailed set of coping self-efficacy constructs than for drug use.
Validation analyses were consistent with our predictions and provide support for the utility of the shortened and revised DTCQ scales. As hypothesized for construct validity, high confidence for coping in negative situations (Scale 1) was associated with urges to use (negative), the importance of not using (positive), and likelihood of resisting use (positive) in a situation related to interpersonal and intrapersonal conflict. Coping self-efficacy in the other four situations represented in the revised DTCQ (Scales 2-5) was significantly associated with appraisal variables in a social situation. These results suggest that the revised DTCQ does measure situation specific aspects of self-efficacy.
Motivation to abstain from alcohol and drugs following treatment was associated with youth self-efficacy. Relationships were slightly stronger between self-efficacy and motivation to abstain from drugs, rather than alcohol, which is consistent with research suggesting that motivation for abstinence varies across types of substances (Brown, Tapert, Tate, & Abrantes, 2000). These findings highlight the importance of considering motivation when evaluating cognitive constructs associated with youth relapse (Brown & Ramo, 2006). Youth entering treatment programs commonly have little motivation to abstain even though they may be motivated to resolve substance-related problems (Brown, 1999). Since motivation will dictate the extent to which youth make effortful coping responses in relapse risk situations, which in turn influences beliefs about ability to cope, it is expected that coping self-efficacy will be associated with motivation in a developmentally-specific cognitive-behavioral model of relapse (Brown & Ramo, 2006).
Coping self-efficacy appears to be relatively independent of ethnicity and family relationship functioning. The exception to this discriminant validity was the significant relationship between family expressiveness, and self-efficacy to resist the urge to use substances in negative situations. This finding suggests that adolescents who have a higher level of interpersonal communication within their families may have greater protection against relapse in negative interpersonal or intrapersonal states. This hypothesis, however, requires further validation.
Concurrent validity was examined in relation to substance use at intake and substances of choice. Modest but significant relationships were found between self-efficacy and quantity/frequency of use (use episodes), DSM-IV dependence symptoms and the number of substances used. Correlations found in this study were comparable to those reported for the DTCQ in an adult sample (Sklar et al., 1997). Relationships were strongest between self-efficacy and alcohol/drug withdrawal symptoms across all DTCQ scales, especially in the subsample of adolescents whose substance of choice was alcohol. This relationship suggests that intervention efforts for increasing self-efficacy may be most needed among adolescents who present with the greatest physical addiction symptoms.
Finally, it is useful to note that self-efficacy in two of the five situation clusters and total self-efficacy was predictive of substance use outcome 6 months after treatment. High self-efficacy was found to protect against a return to substance use and experiencing substance use-related problems after treatment. This is consistent with the adult literature demonstrating that lower coping self-efficacy predicts relapse after treatment for alcohol and drug abuse (e.g., Goldbeck, Myatt, & Aitchison, 1997; Solomon & Annis, 1990). Prospective findings such as these highlight the clinical utility of self-efficacy in understanding and preventing relapse in adolescents (Brown & Ramo, 2006; Marlatt, Baer, & Quigley, 1995). There were three situation clusters that were not predictive of relapse status after treatment (negative situations, testing personal control, and physical/intimacy). This is consistent with Burleson and Kaminer's (2005) finding that situational self-efficacy was not predictive of substance use outcome in a treatment sample of adolescents. These scales may represent types of high-risk situations which youth have not encountered as often as social/drug-related situations or positive emotion situations, and thus they tend to rate their confidence at a consistently high level. It is also possible that other cognitive and behavioral constructs included in the Youth Relapse Model (such as coping skills, motivation) interact with self-efficacy to predict substance use outcome. These hypotheses need to be examined more fully in future research.
This investigation utilized a sample of youth with SUDs and comorbid DSM-IV Axis I psychopathology. As such, the generalizability of these findings to other youth samples is unknown. Given the high rate of comorbidity of SUDs and Axis I psychiatric disorders among clinical samples of youth (Grella, Hser, Joshi, & Rounds-Bryant, 2001), we expect that this scoring system for the DTCQ is likely to extend to the broader population of adolescents in treatment for SUDs. Understanding the patterns of responses on the DTCQ in clinical samples of youth is critical for treatment planning; however, it will also be useful to examine whether these response patterns differ across community and clinical samples of youth and future work should address this.
Self-efficacy was not evaluated across gender, nor psychiatric symptoms in this study, and these issues should be examined in future investigations of the adolescent revised DTCQ. Considering that the factors predicting treatment outcomes differ for adult men and women (Grella & Joshi, 1999), and Axis I psychiatric disorders affect outcome from treatment (Grella et al. 2001; Tomlinson, Brown, & Abrantes, 2004), the role of self-efficacy in these relationships should be clarified in further research with this revised DTCQ for adolescents.
The present study provides initial evidence for the utility of a 37-item form of the DTCQ as a measure of coping self-efficacy for alcohol and drug dependent adolescents. There are several differences between the scales in the revised form (5-factors) and the original form (8-factors), which appear to reflect that the self-efficacy construct is associated with the relapse experiences adolescents have most often. This form can be used in both clinical and research settings that wish to include self-efficacy into broader cognitively-based models of substance use in adolescents. It may also help clinicians understand risk perceptions of youth and target areas of strengths and weaknesses for teens in treatment for alcohol and drug abuse.
Acknowledgments
This research was supported by National Institute on Alcohol Abuse and Alcoholism grants AA0703 and AA12171 to Sandra A. Brown and National Institute on Drug Abuse grants R29 DA09181 and K02 DA17652 to Mark G. Myers.
Contributor Information
Danielle E. Ramo, San Diego State University/University of California, San Diego Joint Doctoral Program in Clinical Psychology, Department of Psychology, San Diego State University and Department of Psychiatry, University of California, San Diego
Mark G. Myers, University of California San Diego and Veteran's Affairs San Diego Healthcare System.
Sandra A. Brown, University of California, San Diego and Veteran's Affairs San Diego Healthcare System.
References
- Anderson KG, Frissell KC, Brown SA. Contexts of post-treatment use for substance abusing adolescents with comorbid psychopathology. Journal of Child & Adolescent Substance Abuse. doi: 10.1300/J029v17n01_04. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Annis HM. Inventory of drinking situations. Addiction Research Foundation of Ontario; Toronto: 1982. [Google Scholar]
- Annis HM, Graham JM. Situational Confidence Questionnaire (SCQ-39): User's Guide. Addiction Research Foundation; Toronto: 1988. [Google Scholar]
- Bandura A. Exercise of personal and collective efficacy in changing societies. In: Bandura A, editor. Self-efficacy in changing societies. New York: Cambridge University Press; 1995. pp. 355–394. [Google Scholar]
- Bentler PM. Comparative fit indexes in structural models. Psychological Bulletin. 1990;107:238–246. doi: 10.1037/0033-2909.107.2.238. [DOI] [PubMed] [Google Scholar]
- Bentler PM, Bonett DG. Significance tests and goodness of fit in the analysis of covariance structures. Psychological Bulletin. 1980;88:588–606. [Google Scholar]
- Brown SA. Treatment of adolescent alcohol problems: Research review and appraisal. In: National Institute on Alcohol Abuse and Alcoholism extramural scientific advisory board, editor. Treatment. Bethesda: NIAAA; 1999. pp. 1–26. [Google Scholar]
- Brown SA, Creamer VA, Stetson BA. Adolescent alcohol expectancies in relation to personal and parental drinking patterns. Journal of Abnormal Psychology. 1987;96:117–121. doi: 10.1037//0021-843x.96.2.117. [DOI] [PubMed] [Google Scholar]
- Brown SA, D'Amico EJ, McCarthy DM, Tapert SF. Four-year outcomes from adolescent alcohol and drug treatment. Journal of Studies on Alcohol. 2001;62:381–388. doi: 10.15288/jsa.2001.62.381. [DOI] [PubMed] [Google Scholar]
- Brown SA, Myers MG, Lippke L, Tapert SF, Stewart DG, Vik PW. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR); A measure of adolescent alcohol and drug involvement. Journal of Studies on Alcohol. 1998;59:427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- Brown SA, Ramo DE. Clinical course of youth following treatment for alcohol and drug problems. In: Liddle H, Rowe C, editors. Treating Adolescent Substance Abuse: State of the Science. New York: Cambridge University Press; 2006. pp. 79–103. [Google Scholar]
- Brown SA, Stetson BA, Beatty P. Cognitive and behavioral features of adolescent coping in high risk drinking situations. Addictive Behaviors. 1989;14:43–52. doi: 10.1016/0306-4603(89)90015-4. [DOI] [PubMed] [Google Scholar]
- Brown SA, Tapert SF, Tate SR, Abrantes AM. The role of alcohol in adolescent relapse and outcome. Journal of Psychoactive Drugs. 2000;32:107–115. doi: 10.1080/02791072.2000.10400216. [DOI] [PubMed] [Google Scholar]
- Brown SA, Vik PW, Creamer VA. Characteristics of relapse following adolescent substance abuse treatment. Addictive Behaviors. 1989;14:291–300. doi: 10.1016/0306-4603(89)90060-9. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Newbury Park: Sage; 1993. pp. 136–162. [Google Scholar]
- Burleson JA, Kaminer Y. Self-efficacy as a predictor of treatment outcome in adolescent substance use disorders. Addictive Behaviors. 2005;30:1751–1764. doi: 10.1016/j.addbeh.2005.07.006. [DOI] [PubMed] [Google Scholar]
- Burling TA, Reilly PM, Moltzen JO, Ziff DC. Self-efficacy and relapse among inpatient drug and alcohol abusers: A predictor of outcome. Journal of Studies on Alcohol. 1989;50:354–360. doi: 10.15288/jsa.1989.50.354. [DOI] [PubMed] [Google Scholar]
- Cannon DS, Leeka JK, Patterson ET, Baker TB. Principal components analysis of the Inventory of Drinking Situations: Empirical categories of drinking by alcoholics. Addictive Behaviors. 1990;15:265–269. doi: 10.1016/0306-4603(90)90069-a. [DOI] [PubMed] [Google Scholar]
- Christiansen BA, Goldman MS. Alcohol-related expectancies versus demographic/background variables in the prediction of adolescent drinking. Journal of Consulting & Clinical Psychology. 1983;51:249–257. doi: 10.1037//0022-006x.51.2.249. [DOI] [PubMed] [Google Scholar]
- Christiansen BA, Goldman MS, Brown SA. The differential development of adolescent alcohol expectancies may predict adult alcoholism. Addictive Behaviors. 1985;10:299–306. doi: 10.1016/0306-4603(85)90011-5. [DOI] [PubMed] [Google Scholar]
- Christiansen BA, Goldman MS, Inn A. Development of alcohol-related expectancies in adolescents: Separating pharmacological from social learning influences. Journal of Consulting & Clinical Psychology. 1982;50:336–344. doi: 10.1037//0022-006x.50.3.336. [DOI] [PubMed] [Google Scholar]
- Deas D, Riggs P, Langenbucher J, Goldman M, Brown S. Adolescents are not adults: Developmental considerations in alcohol users. Alcoholism: Clinical and Experimental Research. 2000;24:232–237. [PubMed] [Google Scholar]
- Dunn ME, Goldman MS. Age and drinking-related differences in the memory organization of alcohol expectancies in 3rd-, 6th-, 9th-, and 12th-grade children. Journal of Consulting and Clinical Psychology. 1998;66:579–585. doi: 10.1037//0022-006x.66.3.579. [DOI] [PubMed] [Google Scholar]
- Folkman S, Lazarus RS. Manual for the Ways of Coping Questionnaire. Consulting Psychologists Press; Palo Alto: 1988. [Google Scholar]
- Friedman AS, Terras A, Kreisher C. Family and client characteristics as predictor of outpatient treatment outcome for adolescent drug abusers. Journal of Substance Abuse. 1995;7:345–56. doi: 10.1016/0899-3289(95)90027-6. [DOI] [PubMed] [Google Scholar]
- Gerbing DW, Hamilton JG. Viability of exploratory factor analysis as a precursor to confirmatory factor analysis. Structural Equation Modeling. 1996;3:62–72. [Google Scholar]
- Goldbeck R, Myatt P, Aitchison T. End-of-treatment self-efficacy: A predictor of abstinence. Addiction. 1997;92:313–324. [PubMed] [Google Scholar]
- Grella CE, Hser Y, Joshi V, Rounds-Bryant J. Drug treatment outcomes for adolescents with comorbid mental and substance use disorders. Journal of Nervous & Mental Disease. 2001;189:384–392. doi: 10.1097/00005053-200106000-00006. [DOI] [PubMed] [Google Scholar]
- Grella CE, Joshi V. Gender differences in drug treatment careers among clients in the National Drug Abuse Treatment Outcome Study. American Journal of Drug & Alcohol Abuse. 1999;25:385–406. doi: 10.1081/ada-100101868. [DOI] [PubMed] [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indices in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling. 1999;6:1–55. [Google Scholar]
- Isenhart CE. Factor structure of the Inventory of Drinking Situations. Journal of Substance Abuse. 1991;3:59–71. doi: 10.1016/s0899-3289(05)80006-9. [DOI] [PubMed] [Google Scholar]
- Kirisci L, Moss HB. Reliability and validity of the Situational Confidence Questionnaire in an adolescent sample: Confirmatory factor analysis and item response theory. Measurement and Evaluation in Counseling and Development. 1997;30:146–155. [Google Scholar]
- Kirisci L, Moss HB, Tarter RE. Psychometric Evaluation of the Situational Confidence Questionnaire in adolescents: Fitting a graded item response model. Addictive Behaviors. 1996;21:303–317. doi: 10.1016/0306-4603(95)00060-7. [DOI] [PubMed] [Google Scholar]
- Marlatt GA, Baer JS, Quigley LA. Self-efficacy and addictive behavior. In: Bandura A, editor. Self-efficacy in Changing Societies. New York: Cambridge University Press; 1995. pp. 289–315. [Google Scholar]
- Marlatt GA, Gordon JR. Relapse prevention: Maintenance strategies in the treatment of addictive behaviors. Guilford Press; New York: 1985. [Google Scholar]
- Marsh HW, Hau KT, Wen Z. In search of golden rules: Comment on hypothesis-testing approaches to setting cutoff values for fit indexes and dangers in overgeneralizing Hu and Bentler's (1999) findings. Structural Equation Modeling. 2004;11:320–341. [Google Scholar]
- Moos R, Moos B. Family Environment Scale Manual: Development, Applications, Research - Third Edition. Palo Alto, CA: Consulting Psychologist Press; 1994. [Google Scholar]
- Muthén BO, Muthén LK. Mplus (Version 2.13) [Computer software] Statmodel.com.; Los Angeles: 1999. [Google Scholar]
- Myers MG, Brown SA. Coping responses and relapse among adolescent substance abusers. Journal of Substance Abuse. 1990;2:177–189. doi: 10.1016/s0899-3289(05)80054-9. [DOI] [PubMed] [Google Scholar]
- Myers MG, Brown SA. The adolescent relapse coping questionnaire: Psychometric validation. Journal of Studies on Alcohol. 1996;57:40–46. doi: 10.15288/jsa.1996.57.40. [DOI] [PubMed] [Google Scholar]
- Satorra A, Bentler PM. Corrections to test statistics and standard errors in covariance structure analysis. In: von Eye A, Clogg CC, editors. Latent variables analysis: Applications for developmental research. Thousand Oaks, CA: Sage Publications; 1994. pp. 399–419. [Google Scholar]
- Sklar SM, Annis HM, Turner NE. Development and validation of the Drug-Taking Confidence Questionnaire: A measure of coping self-efficacy. Addictive Behaviors. 1997;22:655–670. doi: 10.1016/s0306-4603(97)00006-3. [DOI] [PubMed] [Google Scholar]
- Solomon KE, Annis HM. Outcome and efficacy expectancy in the prediction of post-treatment drinking behaviour. British Journal of Addiction. 1990;85:659–665. doi: 10.1111/j.1360-0443.1990.tb03528.x. [DOI] [PubMed] [Google Scholar]
- Tomlinson KL, Brown SA, Abrantes A. Psychiatric comorbidity and substance use treatment outcomes of adolescents. Psychology of Addictive Behaviors. 2004;18:160–169. doi: 10.1037/0893-164X.18.2.160. [DOI] [PubMed] [Google Scholar]
- Turner NE, Annis HM, Sklar SM. Measurement of antecedents to drug and alcohol use: Psychometric properties of the Inventory of Drug-Taking Situations (IDTS) Behavior Research & Therapy. 1997;35:465–483. doi: 10.1016/s0005-7967(96)00119-2. [DOI] [PubMed] [Google Scholar]
- Witkiewitz K, Marlatt GA. Relapse prevention for alcohol and drug problems: That was Zen, this is Tao. American Psychologist. 2004;59:224–235. doi: 10.1037/0003-066X.59.4.224. [DOI] [PubMed] [Google Scholar]