Abstract
Acute eosinophilic pneumonia is a very rare disease that is characterized by acute febrile respiratory failure, diffuse bilateral infiltrates on chest X-ray, and eosinophilia in bronchoalveolar lavage fluid in the absence of infection. We present the case of a 15-year-old girl diagnosed with smoking-induced acute eosinophilic pneumonia. A previously healthy young girl with a 1-day history of fever presented with cough, dyspnea, and diffuse bilateral infiltrates on chest X-ray. She had started smoking only 3 weeks before presentation. She was diagnosed by bronchoalveolar lavage fluid tests and lung biopsy and dramatically improved after steroid treatment. We emphasize that acute eosinophilic pneumonia must be considered when acute pneumonia does not respond to broad-spectrum antibiotics. Effective treatment and prompt institution of therapy can obviate unnecessary morbidity and mortality.
Keywords: Pulmonary eosinophilia, smoking, adolescent, bronchoalveolar lavage fluid
INTRODUCTION
Since acute eosinophilic pneumonia was first described by Badesch1 and Allen2 in 1989, fewer than 150 cases have been reported worldwide. Acute eosinophilic pneumonia is extremely rare, especially in children.3 The current diagnostic criteria are as follows: fever, acute respiratory symptoms during a period of <1 week, diffuse bilateral infiltrates on chest X-ray, severe hypoxia, ≥25% eosinophilia in bronchoalveolar lavage fluid (BALF), or eosinophilic infiltrates in lung tissue biopsy and absence of definite causes of eosinophilic pneumonia such as drugs, infection, asthma, or atopy.4,5 This disease is similar clinically to acute interstitial pneumonitis or acute respiratory distress syndrome; therefore, its treatment is apt to fail if diagnosis is delayed without BALF tests. We experienced the case of a 15-year-old girl who recently started smoking and presented with the clinical and pathological features of acute eosinophilic pneumonia. To the best of our knowledge, this patient is the youngest among those reported with smoking-induced acute eosinophilic pneumonia in Korea. Recently, people have started smoking earlier, and it is difficult to obtain an accurate history of smoking. This is a case in which the history of smoking was inferred from the urine cotinine level.
CASE REPORT
A 15-year-old girl was admitted to our hospital with a 1-week history of fever as well as dry cough, dyspnea, and myalgia that started on the day of admission. She had been healthy prior to admission and had no notable history of respiratory or allergic disease. In her family history, her father was being treated for liver cirrhosis. She had started smoking 3-5 cigarettes daily 3 weeks before admission, but stopped smoking 1 week before admission due to discomfort after smoking. On admission, the patient had clear consciousness but appeared acutely ill. Her blood pressure was 112/70 mmHg, pulse rate 121/minute, respiratory rate 24/minute, and body temperature 36.4℃. The conjunctivae were pink, and the sclerae showed no sign of jaundice. No cervical lymph nodes were palpable. On physical examination, rales and coarse breathing sounds were audible, but heart sounds were normal. There were no abnormal findings in the abdomen.
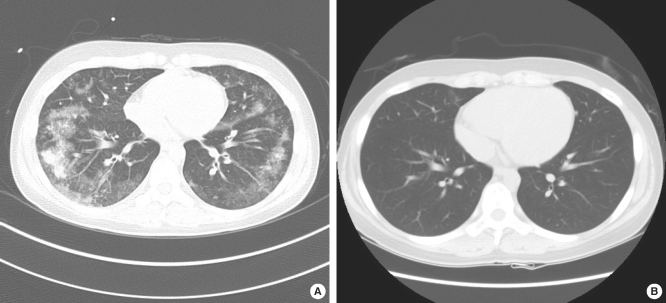
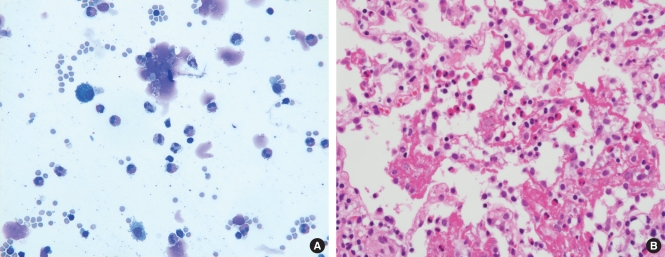
On admission, routine blood tests revealed white blood cells, 19,400/µL; hemoglobin, 14.4 g/dL; erythrocyte sedimentation rate, 17 mm/hour; platelets, 241,000/µL; neutrophils, 90.8%; lymphocytes, 3.7%; monocytes, 4.0%; and eosinophils, 1.4%. Arterial blood gas analysis performed in room air exhibited pH 7.45; PaCO2, 31 mmHg; PaO2, 64 mmHg; HCO3, 22.0 mEq/L; base excess, -1.4 mEq/L; and oxygen saturation, 93%. Blood biochemical tests showed total protein, 5.9 g/dL; albumin, 3.3 g/dL; aspartate aminotransferase, 17 IU/L; alanine aminotransferase, 8 IU/L; C-reactive protein, 4.22 mg/dL; total bilirubin, 1.1 mg/dL; blood urea nitrogen, 4.0 mg/dL; and creatinine, 0.4 mEq/L. Chest X-ray showed diffuse bilateral infiltrates, especially in the peripheral region (Fig. 1) and chest CT exhibited multiple nodular lesions with ground-glass appearance (Fig. 2). The patient was negative for rheumatoid factor, antinuclear antibody, anti-neutrophil cytoplasmic antibody (ANCA), antibody against Mycoplasma, and cold agglutinin. The levels of IgG, IgA, IgM, complement C3 and C4 were within the normal limits, and the total IgE level was 113 KU/L. Cultures of blood and sputum were negative for bacteria and fungi. Urine tests were negative for antigens of Legionella and Pneumococcus, and IgG tests against parasites were negative for Paragonimus westermani and Clonorchis sinesis. Stool examination was negative for parasite ova. Immediately after admission, ampicillin/sulbactam and cefotaxime, as well as oseltamivir, were administered under the suspicion of pandemic H1N1 infection, but hypoxia, dyspnea, and pneumonic infiltration on chest X-ray were aggravated abruptly. Non-invasive ventilation was maintained. On the second day in hospital, bronchoscopy revealed no abnormal findings, but BALF tests exhibited white blood cells, 280/µL; macrophages, 19%; neutrophils, 10%; lymphocytes, 26% eosinophils, 35% (eosinophilia); and basophils, 4% (Fig. 3A). BALF cultures were negative for bacteria and fungi. The patient was negative for PCR and culture of viruses, including respiratory syncytial virus, influenza virus, parainfluenza virus, adenovirus, and human metapneumovirus; real-time RT-PCR for the novel influenza virus H1N1; antigen tests for Aspergillus and Pneumocystis jiroveci; PCR and culture of cytomegalovirus and Chlamydia pneumonia; PCR of Epstein-Barr virus; and acid-fast bacillus smear. On the third day in hospital, thoracoscopy-assisted lung biopsy was performed in the middle and lower lobes of the left lung, which showed eosinophilic infiltrates suggestive of interstitial pneumonia (Fig. 3B). Based on these results, the patient was diagnosed with acute eosinophilic pneumonia. On the fifth day in hospital, urine cotinine level, which was determined to confirm smoking, was 47 ng/mL. Furthermore, routine blood test revealed white blood cells, 5,500/µL; neutrophils, 45.8%; lymphocytes, 26.0%; monocytes, 9.0%; and eosinophils (19.0%, eosinophilia). Methylprednisolone (125 mg) was administered every 6 hours. The day after methylprednisolone administration, hypoxia and dyspnea improved, and infiltrates on chest X-ray improved 2 days after drug administration (Fig. 1). Methylprednisolone was tapered from the fourth day of drug administration. The patient was discharged from the hospital on day 9 and was followed up periodically. At the time of discharge from the hospital, routine blood tests revealed white blood cells, 10,300/µL; neutrophils, 59.6%; lymphocytes, 31.5%; monocytes, 6.3%; and eosinophils, 2.4% (within the normal limits). There were no specific findings in pulmonary function, methacholine provocation, and skin prick tests. Methylprednisolone is being tapered at the outpatient clinic. On day 15 of follow-up, chest X-ray showed no infiltrates.
Fig. 1.
Serial chest X-ray on admission, hospital days 5, 6 and 7 showing dramatic improvement after the initiation of corticosteroids on hospital day 5.
Fig. 2.
Chest CT on admission (A) and follow-up after 2 months (B) reveals markedly improved ground glass opacity and air space consolidation in both lungs.
Fig. 3.
(A) Bronchoalveolar lavage fluid showed more than 25% eosinophils. (Wright stain, ×400). (B) Lung biopsy specimen on the third day shows that many inflammatory cells are present in the alveolar spaces and septae, which are admixed with fibrous exudates. The majority of the infiltrated cells are eosinophils (Hematoxylin-eosin stain, ×400).
DISCUSSION
Acute eosinophilic pneumonia belongs to the eosinophilic lung diseases that are characterized by acute respiratory symptoms including fever, cough, dyspnea, diffuse bilateral infiltrates, and hypoxia. Eosinophilic lung disease includes a variety of infiltrative lung diseases that have marked eosinophilic infiltrates into the lung parenchyma, probably caused by eosinophils, and was first described by Löffler7 in 1932. Crofton et al.8 have classified this disease entity into five groups: simple pulmonary eosinophilia or Löffler's syndrome, prolonged pulmonary eosinophilia, pulmonary eosinophilia with asthma, topical eosinophilia, and pulmonary eosinophilia with polyarteritis nodosa. Carrington et al.9 have described chronic eosinophilic pneumonia that is characterized by high fever; night sweating; weight loss; respiratory symptoms such as severe dyspnea, diffuse infiltrates, and eosinophilia of the lung and peripheral blood; and dramatic responses to steroids, with frequent recurrence after their discontinuation. Badesch et al.1 have described acute eosinophilic pneumonia that is similar to chronic eosinophilic pneumonia, but different in that it shows symptoms during a period of <1 month, no association with asthma or other complications, absence of definite causes, and no recurrence after discontinuation of treatment. Allen et al.2 have reported four cases of acute eosinophilic pneumonia. Recently, eosinophilic lung diseases have been classified into three groups: (1) those with determined causes, including eosinophilic pneumonia due to parasites and other pathogens, drugs, toxins or radiation, as well as allergic bronchopulmonary aspergillosis; (2) those with undetermined causes, including simple pulmonary eosinophilia, acute eosinophilic pneumonia, chronic eosinophilic pneumonia, Churg-Strauss syndrome, and hypereosinophilic syndrome; and (3) miscellaneous lung diseases with possible associated eosinophilia.5,10
Although the pathophysiology of acute eosinophilic pneumonia has not yet been elucidated, it is thought to be caused by acute hypersensitivity to inhaled allergens.2 Most cases are idiopathic, but a few cases seem to be associated with recent smoking or nonspecific dust inhalation.11 Cases of acute eosinophilic pneumonia have continually been reported in new young smokers. When smokers continue to smoke, they may develop tolerance, but acute eosinophilic pneumonia can develop in current smokers who increase their amount of smoking.4,6,12-17 Subjects who restart smoking show clinical symptoms and signs similar to those of acute eosinophilic pneumonia.13-15 Watanabe et al.13 have reported that acute eosinophilic pneumonia that is probably caused by smoking can occur at a mean age of 19 years and a mean of 14.3 days after initiation of smoking. It has been reported in United States soldiers that the incidence of acute eosinophilic pneumonia was 9.1 soldiers per 10,000, and that all cases of acute eosinophilic pneumonia occurred in smokers, 78% of whom started smoking within 1 month of its occurrence.17 As the incidence of acute eosinophilic pneumonia is low compared to that of smoking, it is difficult to regard smoking as its single cause. Our case developed in a girl who started smoking (3-5 cigarettes daily) 3 weeks prior to admission. Acute eosinophilic pneumonia develops most frequently around the age of 30 years in healthy subjects without a past history of asthma or atopy, and more frequently in men.5,18 Clinical symptoms have an acute onset of <7 days, including fever, cough, tachypnea, and dyspnea, which may lead to a misdiagnosis of pneumonia.4,12,19 Because dyspnea is aggravated rapidly, it is difficult to discriminate acute eosinophilic pneumonia from acute respiratory distress syndrome or acute lung injury.4,12,19 Most patients show a fever of more than 38℃, 73% report chest pain, and a few patients complain of myalgia or abdominal pain. Chest auscultation reveals crackles in 80% of patients and normal breathing sounds in 20%.4,12,19 Chest X-ray shows reticulonodular density in the air spaces or interstitial tissues in both lung fields, especially peripheral fields, frequently accompanied by small amounts of pleural effusion.4,10,20 Chest CT exhibits bilateral ground-glass attenuation, interlobular septal thickening, thickening of bronchovascular bundles, bilateral pleural effusion without cardiomegaly, and random distribution.10,21 Although the number of eosinophils is usually normal at the initial stage, it frequently increases over time.19 The IgE level varies between normal and extremely high.19 The BALF tests are the core measures for the diagnosis of acute eosinophilic pneumonia and show that the numbers of eosinophils, lymphocytes and neutrophils increase by 37-54%, 20%, and 15%, respectively.4,12 These findings are different from those for chronic eosinophilic pneumonia, which show normal cell fractions, except for eosinophils. Acute eosinophilic pneumonia can be diagnosed presumptively if the proportion of eosinophils in BALF is ≥25%, and it can be diagnosed definitively if that value is ≥40%.18 Although lung biopsy is not usually needed to diagnose acute eosinophilic pneumonia, it can be used in cases that are difficult to diagnose, such as immunodeficiency in which fungal infections cannot be ruled out. Pathological examination exhibits eosinophilic infiltrates in the interstitial tissue and alveolar space, and diffuse alveolar injury.6,10 Pulmonary function tests are not pathognomonic and show that about 50% of patients have restrictive patterns and the remaining 50% have obstructive patterns.18
Although our case showed clinical features of acute eosinophilic pneumonia, such as severe dyspnea, pulmonary infiltrates were observed in the bilateral peripheral fields. Broad-spectrum antibiotics were administered due to the progression of infiltration, but the infiltration did not improve. BALF tests revealed an increase in eosinophils and other inflammatory cells. In our patient, differential leukocyte counts of peripheral blood showed that eosinophils accounted for 1.4% of the total leukocytes on admission, but increased to 19% on the fifth day in hospital, which suggests that most eosinophils migrated to the lung. We could not perform pulmonary function tests because of severe dyspnea, but the tests performed 8 days after the initiation of steroid administration revealed normal findings.
Our female adolescent patient reported at first that she had not smoked. However, when a thorough history was taken under clinical suspicion of acute eosinophilic pneumonia, she reported that she had smoked for 2 weeks and then stopped during the week prior to admission. This was thought to be an adolescent case of acute eosinophilic pneumonia that was induced by smoking. Recently, the onset of smoking has occurred at a younger age, and the incidence has increased.22 As adolescents try to avoid reporting that they smoke, an accurate history of smoking is difficult to obtain. Therefore, when smoking habits are suspected strongly, physicians should make an effort to take a thorough history of smoking. To screen smokers, many tests have been used. Among these, measurement of urine cotinine concentration is a noninvasive method and yields better results than saliva cotinine concentration does. Cotinine has a half-life of approximately 19 hours and has high sensitivity, based on the response to questionnaires.23 Much controversy exists regarding the cutoff value of cotinine. A previous study with 130 Korean high-school students has shown that the mean urine concentrations of cotinine were 9.9 and 644.5 ng/mL, respectively, in non-smokers and subjective smokers during the previous month and that urine cotinine concentration became higher as the frequency of smoking increased.23 Our patient showed a urine cotinine concentration of 47 ng/mL, which was not significantly high. This result may be due to the following reasons: (1) the half-life of cotinine is 19 hours; (2) the patient stopped smoking the week before admission; and (3) the test was performed on day 5 in hospital. Therefore, follow-up with urine cotinine concentration will help detect smoking in adolescent patients.
Acute eosinophilic pneumonia should be discriminated from clinically similar lung diseases, especially pulmonary infections. In our case, laboratory tests for parasites, viruses, bacteria, and fungi were negative. Drugs were excluded as a cause of acute eosinophilic pneumonia, and the possibility of connective tissue diseases was judged to be low from the tests. Churg-Strauss syndrome was ruled out based on the absence of extrapulmonary symptoms and negativity for ANCA. Other allergic diseases or allergic bronchopulmonary aspergillosis were ruled out based on the absence of a previous history of bronchial asthma and negative skin reactions to offending allergens. Acute eosinophilic pneumonia rather than chronic eosinophilic pneumonia was suggested based on the following findings: (1) absence of a previous history of bronchial asthma; (2) onset at young age; (3) abrupt onset of respiratory symptoms; (4) no eosinophilia in peripheral blood; and (5) an increased proportion of eosinophils, lymphocytes, and neutrophils in BALF.
Because two-thirds of patients with acute eosinophilic pneumonia have respiratory failure that requires mechanical ventilation, early diagnosis and appropriate treatment are mandatory.6 Steroid administration markedly improves clinical symptoms within 24-48 hours.6 Spontaneous improvement has been reported in a few cases of acute eosinophilic pneumonia.12,24 In cases of respiratory failure, methylprednisolone (60-125 mg) is administered every 6 hours until respiratory failure improves, and thereafter, oral prednisolone (40-60 mg/day) is administered and tapered progressively.6,25 In a previous study, methylprednisolone (2 mg/kg) was administered every 6 hours to pediatric patients.26 Steroid dosage must be decided by considering the patient's body weight. Most patients with acute eosinophilic pneumonia can be treated successfully with steroid therapy for 2-12 weeks, without recurrence or sequalae.6
We experienced the case of a 15-year-old girl who had acute eosinophilic pneumonia due to the onset of smoking 3 weeks prior to admission. She was diagnosed based on BALF tests/lung biopsy and was treated successfully with steroids. A history of smoking should be taken in adolescent patients. To exclude the possibility of chronic eosinophilic pneumonia, identification of recurrence after discontinuation of steroid therapy is needed through long-term follow-up.
Footnotes
There are no financial or other issues that might lead to conflict of interest.
References
- 1.Badesch DB, King TE, Jr, Schwarz MI. Acute eosinophilic pneumonia: a hypersensitivity phenomenon? Am Rev Respir Dis. 1989;139:249–252. doi: 10.1164/ajrccm/139.1.249. [DOI] [PubMed] [Google Scholar]
- 2.Allen JN, Pacht ER, Gadek JE, Davis WB. Acute eosinophilic pneumonia as a reversible cause of noninfectious respiratory failure. N Engl J Med. 1989;321:569–574. doi: 10.1056/NEJM198908313210903. [DOI] [PubMed] [Google Scholar]
- 3.Oermann CM, Panesar KS, Langston C, Larsen GL, Menendez AA, Schofield DE, Cosio C, Fan LL. Pulmonary infiltrates with eosinophilia syndromes in children. J Pediatr. 2000;136:351–358. doi: 10.1067/mpd.2000.103350. [DOI] [PubMed] [Google Scholar]
- 4.Pope-Harman AL, Davis WB, Allen ED, Christoforidis AJ, Allen JN. Acute eosinophilic pneumonia. A summary of 15 cases and review of the literature. Medicine (Baltimore) 1996;75:334–342. doi: 10.1097/00005792-199611000-00004. [DOI] [PubMed] [Google Scholar]
- 5.Cottin V, Cordier JF. Eosinophilic pneumonias. Allergy. 2005;60:841–857. doi: 10.1111/j.1398-9995.2005.00812.x. [DOI] [PubMed] [Google Scholar]
- 6.Son C. Eosinophilic pneumonia. Tuberc Respir Dis. 2008;64:177–186. Korean. [Google Scholar]
- 7.Löffler W. Zur differential-diagnose der lungeninfiltrierungen. Il uber fluchtige succedan-infiltrate (mit eosinophilie) Beitr Klin Tuberk. 1932;79:368–392. [Google Scholar]
- 8.Crofton JW, Livingstone JL, Oswald NC, Roberts AT. Pulmonary eosinophilia. Thorax. 1952;7:1–35. doi: 10.1136/thx.7.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Carrington CB, Addington WW, Goff AM, Madoff IM, Marks A, Schwaber JR, Gaensler EA. Chronic eosinophilic pneumonia. N Engl J Med. 1969;280:787–798. doi: 10.1056/NEJM196904102801501. [DOI] [PubMed] [Google Scholar]
- 10.Jeong YJ, Kim KI, Seo IJ, Lee CH, Lee KN, Kim KN, Kim JS, Kwon WJ. Eosinophilic lung diseases: a clinical, radiologic, and pathologic overview. Radiographics. 2007;27:617–637. doi: 10.1148/rg.273065051. discussion 37-9. [DOI] [PubMed] [Google Scholar]
- 11.Rom WN, Weiden M, Garcia R, Yie TA, Vathesatogkit P, Tse DB, McGuinness G, Roggli V, Prezant D. Acute eosinophilic pneumonia in a New York City firefighter exposed to World Trade Center dust. Am J Respir Crit Care Med. 2002;166:797–800. doi: 10.1164/rccm.200206-576OC. [DOI] [PubMed] [Google Scholar]
- 12.Philit F, Etienne-Mastroianni B, Parrot A, Guerin C, Robert D, Cordier JF. Idiopathic acute eosinophilic pneumonia: a study of 22 patients. Am J Respir Crit Care Med. 2002;166:1235–1239. doi: 10.1164/rccm.2112056. [DOI] [PubMed] [Google Scholar]
- 13.Watanabe K, Fujimura M, Kasahara K, Yasui M, Myou S, Kita T, Watanabe A, Nakao S. Acute eosinophilic pneumonia following cigarette smoking: a case report including cigarette-smoking challenge test. Intern Med. 2002;41:1016–1020. doi: 10.2169/internalmedicine.41.1016. [DOI] [PubMed] [Google Scholar]
- 14.Shintani H, Fujimura M, Ishiura Y, Noto M. A case of cigarette smoking-induced acute eosinophilic pneumonia showing tolerance. Chest. 2000;117:277–279. doi: 10.1378/chest.117.1.277. [DOI] [PubMed] [Google Scholar]
- 15.Shin JH, Kwon YE, Yoon SH, Lee SI. Two cases of cigarette smoking-induced acute eosinophilic pneumonia. J Asthma Allergy Clin Immunol. 2007;27:277–282. Korean. [Google Scholar]
- 16.Uchiyama H, Suda T, Nakamura Y, Shirai M, Gemma H, Shirai T, Toyoshima M, Imokawa S, Yasuda K, Ida M, Nakano Y, Inui N, Sato J, Hayakawa H, Chida K. Alterations in smoking habits are associated with acute eosinophilic pneumonia. Chest. 2008;133:1174–1180. doi: 10.1378/chest.07-2669. [DOI] [PubMed] [Google Scholar]
- 17.Shorr AF, Scoville SL, Cersovsky SB, Shanks GD, Ockenhouse CF, Smoak BL, Carr WW, Petruccelli BP. Acute eosinophilic pneumonia among US Military personnel deployed in or near Iraq. JAMA. 2004;292:2997–3005. doi: 10.1001/jama.292.24.2997. [DOI] [PubMed] [Google Scholar]
- 18.Yong SJ. Diagnosis of eosinophilic lung disease. Tuberc Respir Dis. 2008;64:75–79. Korean. [Google Scholar]
- 19.Allen J. Acute eosinophilic pneumonia. Semin Respir Crit Care Med. 2006;27:142–147. doi: 10.1055/s-2006-939517. [DOI] [PubMed] [Google Scholar]
- 20.King MA, Pope-Harman AL, Allen JN, Christoforidis GA, Christoforidis AJ. Acute eosinophilic pneumonia: radiologic and clinical features. Radiology. 1997;203:715–719. doi: 10.1148/radiology.203.3.9169693. [DOI] [PubMed] [Google Scholar]
- 21.Daimon T, Johkoh T, Sumikawa H, Honda O, Fujimoto K, Koga T, Arakawa H, Yanagawa M, Inoue A, Mihara N, Tomiyama N, Nakamura H, Sugiyama Y. Acute eosinophilic pneumonia: Thin-section CT findings in 29 patients. Eur J Radiol. 2008;65:462–467. doi: 10.1016/j.ejrad.2007.04.012. [DOI] [PubMed] [Google Scholar]
- 22.Korea Center for Disease Control and Prevention (KCDC) Results of Korea youth risk behavior web-based survey (KYRBWS) 2006. Available from: http://healthy1318.cdc.go.kr/ [Google Scholar]
- 23.Park SW, Kim JY. Validity of self-reported smoking using urinary cotinine among vocational high school students. J Prev Med Public Health. 2009;42:223–230. doi: 10.3961/jpmph.2009.42.4.223. [DOI] [PubMed] [Google Scholar]
- 24.Hayakawa H, Sato A, Toyoshima M, Imokawa S, Taniguchi M. A clinical study of idiopathic eosinophilic pneumonia. Chest. 1994;105:1462–1466. doi: 10.1378/chest.105.5.1462. [DOI] [PubMed] [Google Scholar]
- 25.Jantz MA, Sahn SA. Corticosteroids in acute respiratory failure. Am J Respir Crit Care Med. 1999;160:1079–1100. doi: 10.1164/ajrccm.160.4.9901075. [DOI] [PubMed] [Google Scholar]
- 26.Buchheit J, Eid N, Rodgers G, Jr, Feger T, Yakoub O. Acute eosinophilic pneumonia with respiratory failure: a new syndrome? Am Rev Respir Dis. 1992;145:716–718. doi: 10.1164/ajrccm/145.3.716. [DOI] [PubMed] [Google Scholar]