Abstract
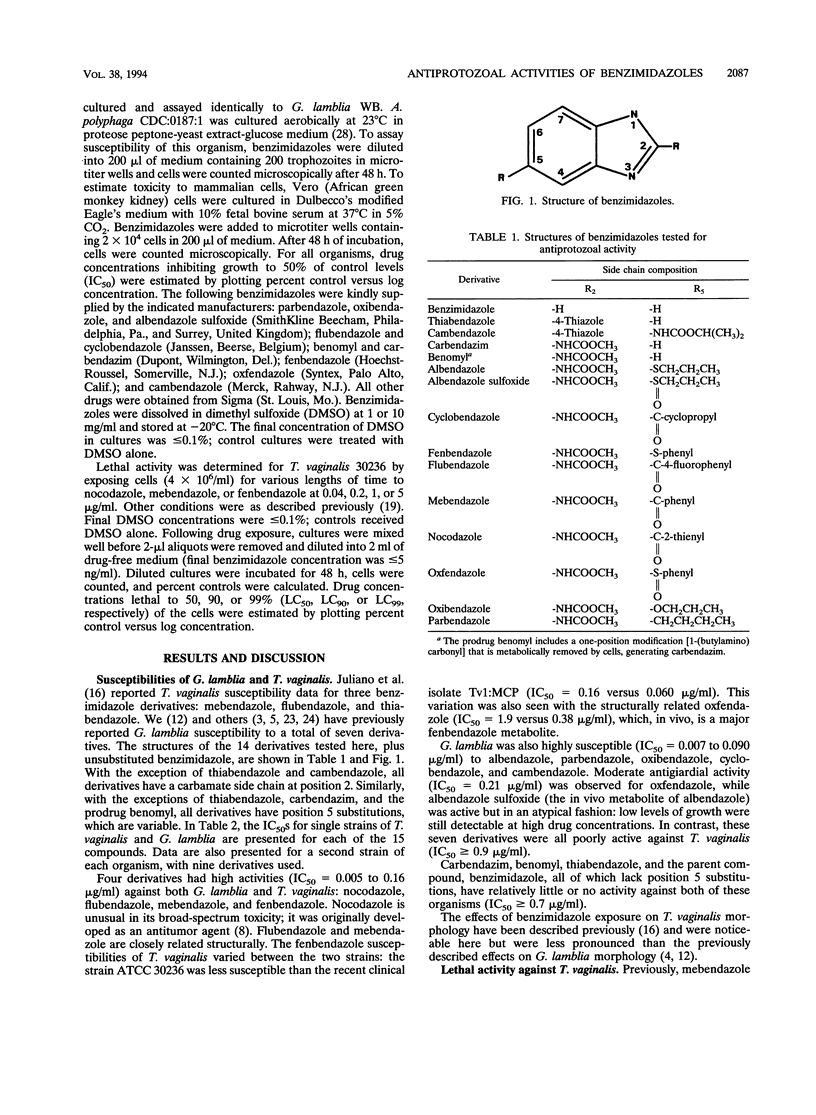
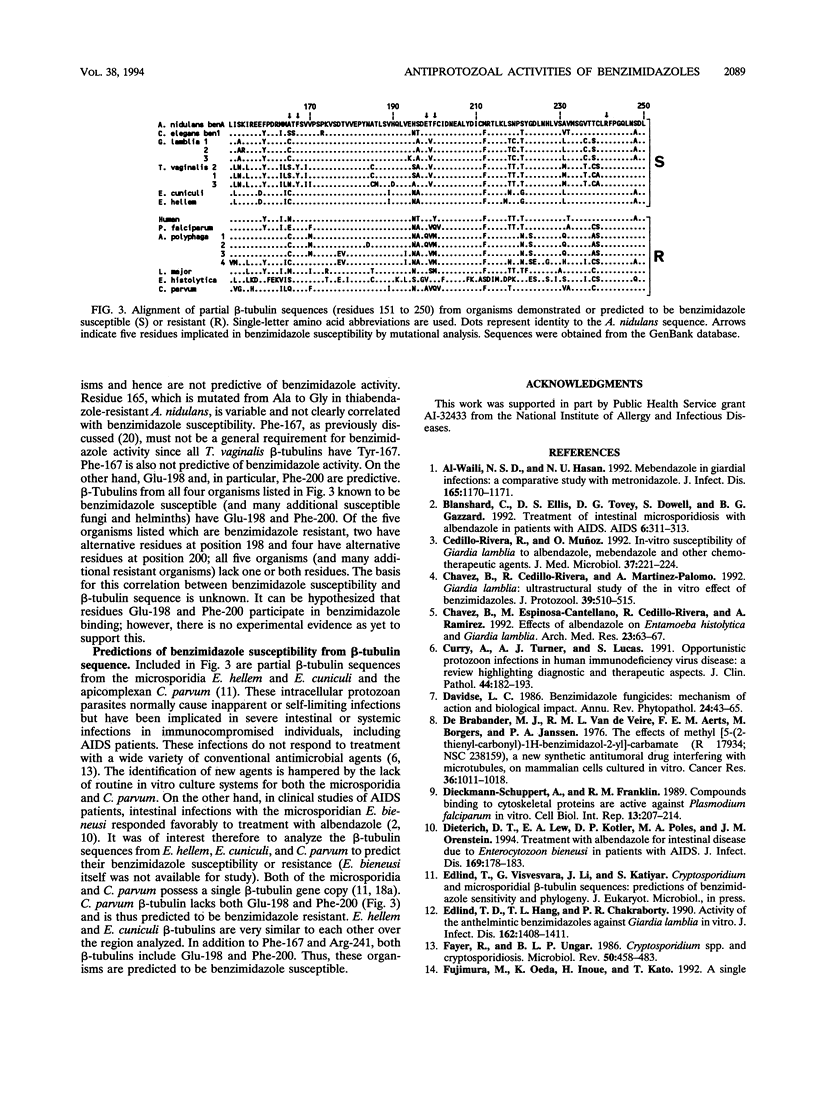
Benzimidazoles have been widely used since the 1960s as anthelmintic agents in veterinary and human medicine and as antifungal agents in agriculture. More recently, selected benzimidazole derivatives were shown to be active in vitro against two protozoan parasites, Trichomonas vaginalis and Giardia lamblia, and clinical studies with AIDS patients have suggested that microsporidia are susceptible as well. Here, we first present in vitro susceptibility data for T. vaginalis and G. lamblia using an expanded set of benzimidazole derivatives. Both parasites were highly susceptible to four derivatives, including mebendazole, flubendazole, and fenbendazole (50% inhibitory concentrations of 0.005 to 0.16 microgram/ml). These derivatives also had lethal activity that was time dependent: 90% of T. vaginalis cells failed to recover following a 20-h exposure to mebendazole at 0.17 microgram/ml. G. lamblia, but not T. vaginalis, was highly susceptible to five additional derivatives. Next, we examined in vitro activity of benzimidazoles against additional protozoan parasites: little or no activity was observed against Entamoeba histolytica, Leishmania major, and Acanthamoeba polyphaga. Since the microtubule protein beta-tubulin has been identified as the benzimidazole target in helminths and fungi, potential correlations between benzimidazole activity and beta-tubulin sequence were examined. This analysis included partial sequences (residues 108 to 259) from the organisms mentioned above, as well as the microsporidia Encephalitozoon hellem and Encephalitozoon cuniculi and the sporozoan Cryptosporidium parvum. beta-tubulin residues Glu-198 and, in particular, Phe-200 are strong predictors of benzimidazole susceptibility; both are present in Encephalitozoon spp. but absent in C. parvum.
Full text
PDF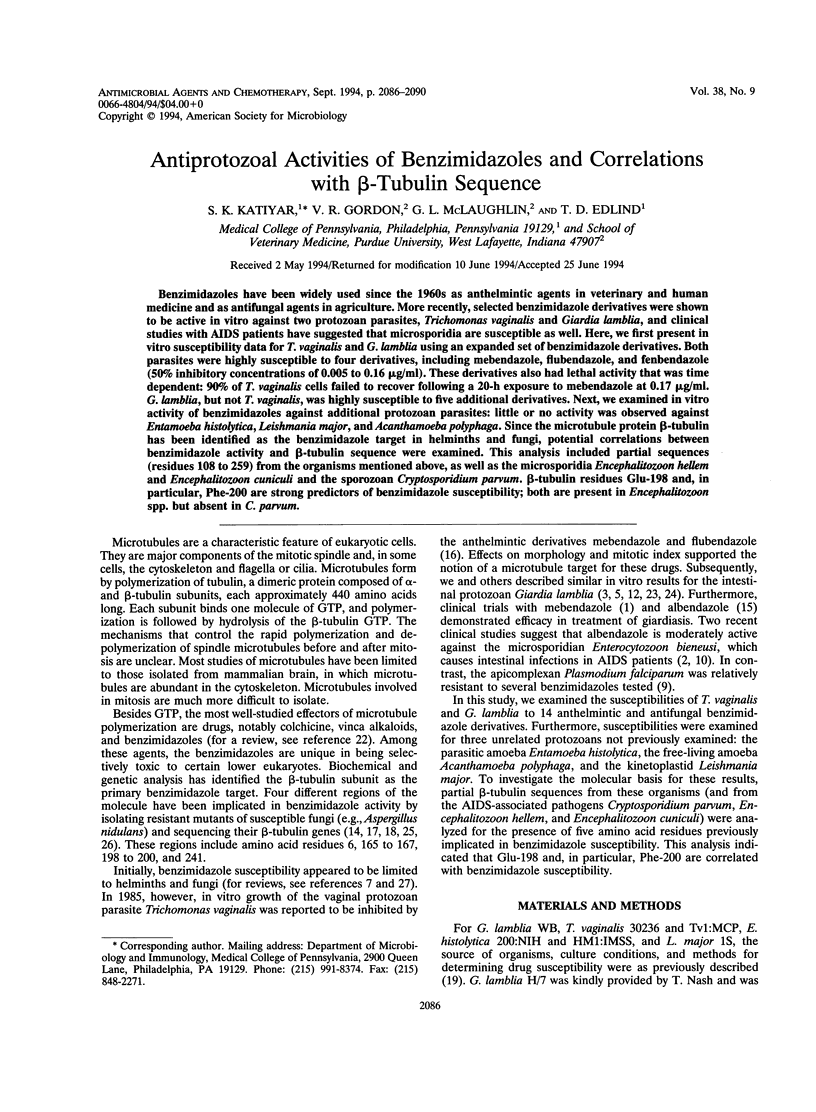

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Blanshard C., Ellis D. S., Tovey D. G., Dowell S., Gazzard B. G. Treatment of intestinal microsporidiosis with albendazole in patients with AIDS. AIDS. 1992 Mar;6(3):311–313. doi: 10.1097/00002030-199203000-00009. [DOI] [PubMed] [Google Scholar]
- Cedillo-Rivera R., Muñoz O. In-vitro susceptibility of Giardia lamblia to albendazole, mebendazole and other chemotherapeutic agents. J Med Microbiol. 1992 Sep;37(3):221–224. doi: 10.1099/00222615-37-3-221. [DOI] [PubMed] [Google Scholar]
- Chavez B., Cedillo-Rivera R., Martinez-Palomo A. Giardia lamblia: ultrastructural study of the in vitro effect of benzimidazoles. J Protozool. 1992 Jul-Aug;39(4):510–515. doi: 10.1111/j.1550-7408.1992.tb04841.x. [DOI] [PubMed] [Google Scholar]
- Chávez B., Espinosa-Cantellano M., Cedillo Rivera R., Ramírez A., Martínez-Palomo A. Effects of albendazole on Entamoeba histolytica and Giardia lamblia trophozoites. Arch Med Res. 1992;23(2):63–67. [PubMed] [Google Scholar]
- Curry A., Turner A. J., Lucas S. Opportunistic protozoan infections in human immunodeficiency virus disease: review highlighting diagnostic and therapeutic aspects. J Clin Pathol. 1991 Mar;44(3):182–193. doi: 10.1136/jcp.44.3.182. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dieckmann-Schuppert A., Franklin R. M. Compounds binding to cytoskeletal proteins are active against Plasmodium falciparum in vitro. Cell Biol Int Rep. 1989 Feb;13(2):207–214. doi: 10.1016/0309-1651(89)90067-2. [DOI] [PubMed] [Google Scholar]
- Dieterich D. T., Lew E. A., Kotler D. P., Poles M. A., Orenstein J. M. Treatment with albendazole for intestinal disease due to Enterocytozoon bieneusi in patients with AIDS. J Infect Dis. 1994 Jan;169(1):178–183. doi: 10.1093/infdis/169.1.178. [DOI] [PubMed] [Google Scholar]
- Edlind T. D., Hang T. L., Chakraborty P. R. Activity of the anthelmintic benzimidazoles against Giardia lamblia in vitro. J Infect Dis. 1990 Dec;162(6):1408–1411. doi: 10.1093/infdis/162.6.1408. [DOI] [PubMed] [Google Scholar]
- Fayer R., Ungar B. L. Cryptosporidium spp. and cryptosporidiosis. Microbiol Rev. 1986 Dec;50(4):458–483. doi: 10.1128/mr.50.4.458-483.1986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall A., Nahar Q. Albendazole as a treatment for infections with Giardia duodenalis in children in Bangladesh. Trans R Soc Trop Med Hyg. 1993 Jan-Feb;87(1):84–86. doi: 10.1016/0035-9203(93)90435-s. [DOI] [PubMed] [Google Scholar]
- Harris C. C., Frank A. L., van Haaften C., Kaufman D. G., Connor R., Jackson F., Barrett L. A., McDowell E. M., Trump B. F. Binding of (3H)benzo(a)pyrene to DNA in cultured human bronchus. Cancer Res. 1976 Mar;36(3):1011–1018. [PubMed] [Google Scholar]
- Juliano C., Martinotti M. G., Cappuccinelli P. "In vitro" effect of microtubule inhibitors on Trichomonas vaginalis. Microbiologica. 1985 Jan;8(1):31–42. [PubMed] [Google Scholar]
- Jung M. K., Oakley B. R. Identification of an amino acid substitution in the benA, beta-tubulin gene of Aspergillus nidulans that confers thiabendazole resistance and benomyl supersensitivity. Cell Motil Cytoskeleton. 1990;17(2):87–94. doi: 10.1002/cm.970170204. [DOI] [PubMed] [Google Scholar]
- Jung M. K., Wilder I. B., Oakley B. R. Amino acid alterations in the benA (beta-tubulin) gene of Aspergillus nidulans that confer benomyl resistance. Cell Motil Cytoskeleton. 1992;22(3):170–174. doi: 10.1002/cm.970220304. [DOI] [PubMed] [Google Scholar]
- Katiyar S. K., Edlind T. D. Enhanced antiparasitic activity of lipophilic tetracyclines: role of uptake. Antimicrob Agents Chemother. 1991 Nov;35(11):2198–2202. doi: 10.1128/aac.35.11.2198. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kirk-Mason K. E., Turner M. J., Chakraborty P. R. Evidence for unusually short tubulin mRNA leaders and characterization of tubulin genes in Giardia lamblia. Mol Biochem Parasitol. 1989 Aug;36(1):87–99. doi: 10.1016/0166-6851(89)90204-1. [DOI] [PubMed] [Google Scholar]
- Lacey E. The role of the cytoskeletal protein, tubulin, in the mode of action and mechanism of drug resistance to benzimidazoles. Int J Parasitol. 1988 Nov;18(7):885–936. doi: 10.1016/0020-7519(88)90175-0. [DOI] [PubMed] [Google Scholar]
- Meloni B. P., Thompson R. C., Reynoldson J. A., Seville P. Albendazole: a more effective antigiardial agent in vitro than metronidazole or tinidazole. Trans R Soc Trop Med Hyg. 1990 May-Jun;84(3):375–379. doi: 10.1016/0035-9203(90)90324-8. [DOI] [PubMed] [Google Scholar]
- Morgan U. M., Reynoldson J. A., Thompson R. C. Activities of several benzimidazoles and tubulin inhibitors against Giardia spp. in vitro. Antimicrob Agents Chemother. 1993 Feb;37(2):328–331. doi: 10.1128/aac.37.2.328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Orbach M. J., Porro E. B., Yanofsky C. Cloning and characterization of the gene for beta-tubulin from a benomyl-resistant mutant of Neurospora crassa and its use as a dominant selectable marker. Mol Cell Biol. 1986 Jul;6(7):2452–2461. doi: 10.1128/mcb.6.7.2452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas J. H., Neff N. F., Botstein D. Isolation and characterization of mutations in the beta-tubulin gene of Saccharomyces cerevisiae. Genetics. 1985 Dec;111(4):715–734. doi: 10.1093/genetics/111.4.715. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Van den Bossche H., Rochette F., Hörig C. Mebendazole and related anthelmintics. Adv Pharmacol Chemother. 1982;19:67–128. doi: 10.1016/s1054-3589(08)60021-6. [DOI] [PubMed] [Google Scholar]
- Visvesvara G. S., Balamuth W. Comparative studies on related free-living and pathogenic amebae with special reference to Acanthamoeba. J Protozool. 1975 May;22(2):245–256. doi: 10.1111/j.1550-7408.1975.tb05860.x. [DOI] [PubMed] [Google Scholar]
- al-Waili N. S., Hasan N. U. Mebendazole in giardial infection: a comparative study with metronidazole. J Infect Dis. 1992 Jun;165(6):1170–1171. doi: 10.1093/infdis/165.6.1170. [DOI] [PubMed] [Google Scholar]



