Abstract
Background
The 2002-2003 Severe Acute Respiratory Syndrome (SARS) outbreak infected 8,422 individuals leading to 916 deaths around the world. However, there have been few epidemiological studies of SARS comparing epidemiologic features across regions. The aim of this study is to identify similarities and differences in SARS epidemiology in three populations with similar host and viral genotype.
Methods
We present a comparative epidemiologic analysis of SARS, based on an integrated dataset with 3,336 SARS patients from Hong Kong, Beijing and Taiwan, epidemiological and clinical characteristics such as incubation, onset-to-admission, onset-to-discharge and onset-to-death periods, case fatality ratios (CFRs) and presenting symptoms are described and compared between regions. We further explored the influence of demographic and clinical variables on the apparently large differences in CFRs between the three regions.
Results
All three regions showed similar incubation periods and progressive shortening of the onset-to-admission interval through the epidemic. Adjusted for sex, health care worker status and nosocomial setting, older age was associated with a higher fatality, with adjusted odds ratio (AOR): 2.10 (95% confidence interval: 1.45, 3.04) for those aged 51-60; AOR: 4.57 (95% confidence interval: 3.32, 7.30) for those aged above 60 compared to those aged 41-50 years. Presence of pre-existing comorbid conditions was also associated with greater mortality (AOR: 1.74; 95% confidence interval: 1.36, 2.21).
Conclusion
The large discrepancy in crude fatality ratios across the three regions can only be partly explained by epidemiological and clinical heterogeneities. Our findings underline the importance of a common data collection platform, especially in an emerging epidemic, in order to identify and explain consistencies and differences in the eventual clinical and public health outcomes of infectious disease outbreaks, which is becoming increasingly important in our highly interconnected world.
Background
The 2002-2003 SARS outbreak infected 8,422 individuals leading to 916 deaths in eight affected areas [1]. The first case was identified on 16 November 2002 in the southern Chinese city of Foshan [2]. The epidemic then spread within Guangdong province before a large superspreading event in Hong Kong seeded the global outbreak [3]. On 5 July 2003, the World Health Organization (WHO) announced the last affected area Taiwan to be transmission free and declared the last human-to-human transmission chain successfully interrupted [4]. Hong Kong, mainland China and Taiwan carried the largest disease burden as well as marked the most important milestones of the global outbreak. However, due to geo-political factors beyond the remit of public health, a consolidated account of their collective experience has not previously been documented.
Except for a few sporadic case reports mostly involving laboratory mishaps [5-7], there has not been sustained human-to-human transmission since 2003. However, the re-emergence of SARS remains a distinct possibility given that similar viruses continue to be isolated in potential animal reservoirs including bats [8,9] and palm civets [10], and trading of the latter continues in Guangdong province despite its official ban [11]. Moreover, reemergence in humans could result from an unknown animal reservoir, or via an intermediary animal host. In addition, among the three affected regions in Greater China, the disease had apparently different epidemiological characteristics whereas the populations share the same gene pool and the same viral clade [12]. These apparent epidemiologic heterogeneities despite similar host and viral genotypes as well as the preparedness imperative for a possible return of SARS motivated the present comparative analysis of the three regions, based on an integrated database of 3336 probable cases, which is the largest single repository of SARS patients constructed to date. We present comprehensive estimates of epidemiologic parameters of interest, and we also investigate potential explanations for the observed discrepancies between regions.
Methods
Sources of data
We analyzed a combined database of SARS patients from Hong Kong (n = 1755), Beijing (n = 917) and Taiwan (n = 664). Clinical, demographic and epidemiologic details for SARS patients from each region were collected, coded and anonymized for analysis. All analyses were based on patients who satisfied the WHO definition for 'probable cases' [13]. In Beijing, clinical presentation, exposure history, blood test, chest CT and X-ray scan were also reviewed in additional to the WHO definition.
Our database on all 1755 probable cases in Hong Kong was derived from the Department of Health master list and the Hospital Authority eSARS system as previously described [14].
Data on 917 of the 2521 probable cases in Beijing [15], who were either directly admitted or transferred to Xiao Tang Shan Hospital (XTS Hospital, n = 680), the No. 302 People's Liberation Army Hospital (Hospital 302, n = 111) or the No. 309 People's Liberation Army Hospital (Hospital 309, n = 126) were included. Clinical information was reviewed by a panel of experts in the earlier stage of the epidemics and furthermore a standardized report form was used after May as previously described [15]. Data were extracted by detailed chart review in each hospital following a standard protocol. Hospital 309 admitted many of the earliest SARS patients and reached full capacity by early April. SARS patients were then sent to Hospital 302, a hospital specializing in infectious diseases. The severity and infectiousness of SARS prompted the Beijing government to build the XTS Hospital in eight days, opening on 1 May 2003. Data on comorbidities, and symptoms were unavailable for patients in Hospital 309.
Similarly, we captured the corresponding data from all 664 probable cases in Taiwan who provided the information through standardized screening questionnaires at emergency rooms and on admission. Data were collected from all hospitals and integrated into a dataset officially maintained by the Centers for Disease Control, Taiwan.
Statistical Analysis
We compared the characteristics of SARS patients by region in terms of demographic and clinical variables such as age, sex and health care worker (HCW) status, presence of pre-existing comorbid conditions (including ischemic heart disease, cerebrovascular disease, cancer, diabetes, chronic renal failure, chronic liver disease and asthma) and whether the patients were admitted before symptom onset. We estimated the case fatality ratios (CFRs) within subgroups of each of these characteristics. We calculated the age- and sex-standardized CFRs and associated exact binomial 95% confidence intervals based on the World Standard Population [16]. We fitted multivariable logistic regression models, controlled for variables such as sex, age, health care worker status, preexisting comorbid conditions and nosocomial infection, for each region on all data allowing us to estimate the adjusted odds ratios of mortality between regions. In the regression models we excluded all 126 patients from Hospital 309 for whom data on pre-existing comorbid conditions were not available and also other two, one and five patients from Hong Kong, Beijing and Taiwan respectively with unknown age, pre-existing comorbid conditions, onset date or admission date. To avoid extreme values in the adjusted odds ratio for the age effect, we chose the middle age group as the reference group. For Hong Kong patients, we also tested the effect of residence in Amoy Garden where a severe outbreak occurred in which many patients presented with diarrhea [17].
Incubation period was estimated on patients with dates of exposure to a potentially infected individual and a symptom onset date, using both non-parametric and parametric methods allowing for interval censoring [18]. We plotted the epidemic curves in each region, and examined the changes in onset-to-admission distribution over the course of the epidemic.
We identified factors which might have affected the onset-to-death and onset-to-discharge distribution and compared the differences across the regions. The onset-to-death and onset-to-discharge periods were firstly log-transformed and then fitted by linear regression separately to the same variables as in the previous model.
Finally, we examined regional differences in symptoms at presentation. All analyses were conducted in R version 2.3.1 [19].
Results
Additional file 1 shows patient characteristics by region and the associated crude CFRs. Patients in Hong Kong were on average older (mean = 43.5 years) than those in Beijing (34.7 years) but younger than those in Taiwan (47.2 years). Case fatality was consistently and strongly age-dependent. Approximately one-third of Taiwan SARS patients had pre-existing comorbid conditions, which was much greater than Hong Kong (20%) and Beijing (4%, based on available data), and in each region the CFRs were markedly elevated for those patients with comorbidities.
Overall, the crude CFRs differed substantially across regions (Additional file 1). After standardizing for age and sex, the case fatality ratios converged somewhat, suggesting that some of the crude differences were due to the different patient demographic profiles particularly in patients' ages between the three regions.
Additional file 1 also displays the adjusted odds ratios of death for each predictor based on data from each region. The adjusted results confirm that older age, non-HCWs, presence of pre-existing comorbid conditions and admission before symptom onset were strongly associated with mortality. In the combined model (Additional file 2), the adjusted odds ratios (95% confidence intervals) of case fatality for Beijing and Taiwan were 0.18 (0.11 to 0.29) and 1.64 (1.29 to 2.07) compared to Hong Kong. When the XTS Hospital patients were excluded, the adjusted odds ratios (95% confidence intervals) of case fatality for Beijing was 0.98 (0.46 to 2.09) compared to Hong Kong. We also fitted a logistic regression analysis to test for any differential effects of sex, age, health care worker status, pre-existing comorbid conditions and nosocomial acquisition between Hospital 302 and XTS Hospital. All the first-order interaction effects were found to be insignificant. All main and interaction effects with residence in Amoy Garden were also found to be insignificant.
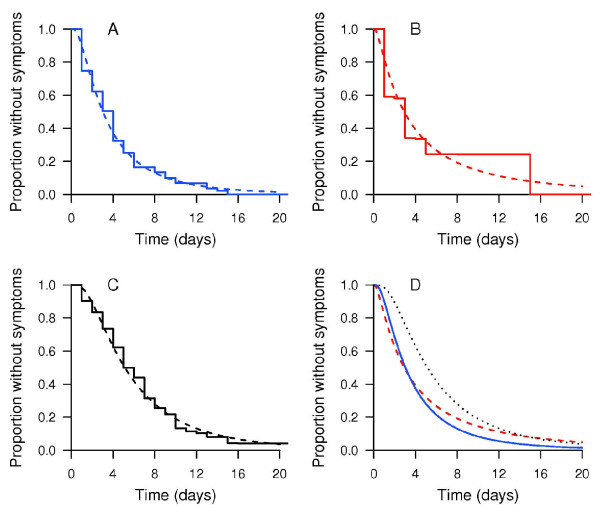
Data on exposure and onset times were available for 168 patients in Hong Kong, 97 patients in Beijing and 210 patients in Taiwan. Fitted lognormal distributions showed good fit compared to non-parametric estimates of the incubation distribution (Figure 1). Based on the lognormal distributions, the estimated means (standard deviations) of the incubation distributions were 4.4 days (4.6 days) in Hong Kong, 5.7 days (9.7 days) in Beijing and 6.9 (6.1 days) in Taiwan. The 25, 50, 75 and 95th percentiles were 2, 3, 5 and 12 days in Hong Kong, 1, 3, 6 and 20 days in Beijing and 3, 5, 9 and 18 days in Taiwan.
Figure 1.
Estimated incubation distribution. (A) Hong Kong (n = 168), (B) Beijing* (n = 97) and (C) Taiwan (n = 156) using a non-parametric method (solid line) and fitted to a lognormal distribution (dashed line). (D) Comparison of estimated incubation distributions fitted to a lognormal distribution in Hong Kong (solid line), Beijing (dashed line), and Taiwan (dotted line). *The large steps seen in the non-parametric estimate in Beijing are aretefacts due to the small sample size.
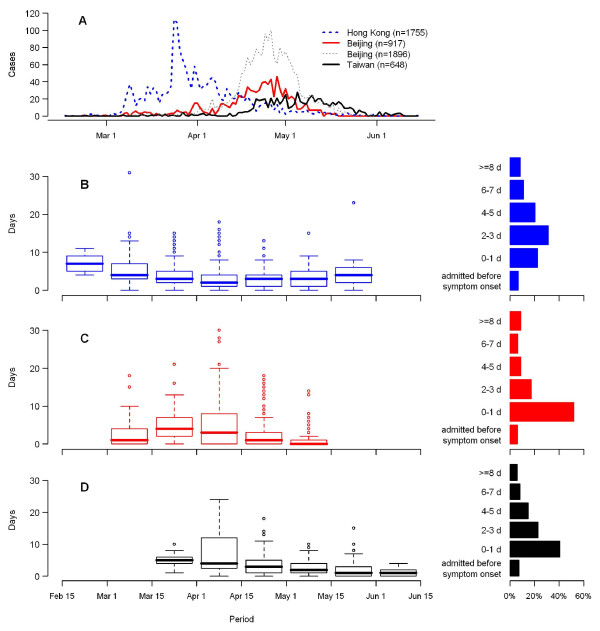
Figure 2A shows the epidemic curve in each region, supplemented with the overall epidemic curve in Beijing [15]. The epidemic in Hong Kong occurred mainly in late March and early April 2003, preceding the outbreaks in Beijing and Taiwan by approximately one month. Figure 2B, C and 2D show box plots of the time from onset to admission during different calendar time periods and the overall distributions of onset-to-admission intervals. Within each region, the onset-to-admission times decreased throughout the main part of all three epidemics, while onset-to-admission times appeared to increase towards the end of the Hong Kong epidemic. Excluding the patients admitted before symptom onset, the mean delay from onset to admission were 3.6, 2.7 and 2.8 days respectively for Hong Kong, Beijing and Taiwan. A relatively large proportion of patients were admitted to hospital within one day after symptom onset in both Beijing and Taiwan, and Taiwan had a higher proportion of patients admitted before symptom onset. In Hong Kong and Taiwan, patients admitted before symptom onset had a much higher CFR (53% and 70% respectively, see Additional files 3 and 4). Hong Kong and Taiwan showed a decreasing gradient with prolonged delay from first symptoms to hospitalization until about one week whereas the opposite appeared to be the case in Beijing. Within Beijing, there was a clear difference in both onset-to-admission distributions and CFRs among hospitals although the trends were mostly consistent (see Additional file 4).
Figure 2.
Epidemiological characteristics in Hong Kong, Beijing and Taiwan. (A) Epidemic curve for Hong Kong, Beijing (based on our data and those from a Beijing dataset [15]), and Taiwan. B-D*: Time from onset to admission distribution for each 2-week period and onset-to-admission distribution for (B) Hong Kong, (C) Beijing and (D) Taiwan. * Patients admitted before symptom onset and periods with fewer than 10 cases were excluded.
The median onset-to-death periods in Hong Kong, Beijing and Taiwan were 21, 24 and 10 days respectively, while the median onset-to-discharge periods were 23, 36 and 19 days respectively. We also examined factors affecting the length of these periods (see Additional file 5). Patients in the youngest age group and those who had acquired SARS nosocomially had significantly shorter onset-to-death periods, while non-health care workers and those with pre-existing comorbid conditions had marginally shorter onset-to-death periods. When comparing across the three regions, Hong Kong and Beijing patients had similar onset-to-death periods, but those of patients in Taiwan were significantly shorter. As a sensitivity analysis, we show the factors affecting onset-to-death and onset-to-discharge excluding data from XTS Hospital (see Additional file 6).
Regarding the onset-to-discharge period, younger patients were found to have shorter lengths of stay in hospital on average. We found statistically significant interaction effects between HCW status and location and between pre-existing comorbid conditions and location, where HCWs in Taiwan had longer onset-to-discharge periods (acceleration factor = 1.35, 95% CI: 1.17, 1.55), while those with pre-existing comorbid conditions in Taiwan had shorter periods (acceleration factor = 0.87, 95% CI: 0.75, 1.02). After adjustment for the above factors, Beijing had a significantly longer onset-to-discharge period comparing with Hong Kong, while Taiwan had a significantly shorter period.
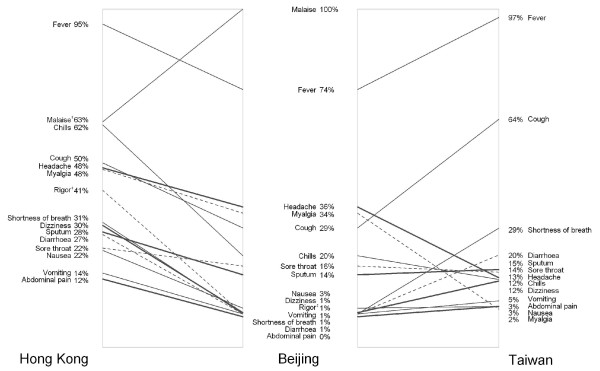
Figure 3 summarizes symptoms at the time of presentation in Hong Kong, Beijing (Hospital 302 only) and Taiwan. While the prevalence of the different symptoms were similar in Beijing and Taiwan, the occurrence of most symptoms was typically higher in Hong Kong. Fever was the most common presenting symptom in all three regions. Dizziness, rigor, shortness of breath as well as gastro-intestinal symptoms including diarrhea, vomiting and abdominal pain were rarely reported in Beijing, on the other hand every patient in Beijing reported malaise.
Figure 3.
Proportion of cases showing different symptoms on presentation in Hong Kong, Beijing (Hospital 302 only†) and Taiwan. * Labels on the vertical axis have been jittered for better presentation. † Detailed symptom data were missing for Hospital 309 patients. ‡ Malaise and rigor were not documented in Taiwan.
Discussion and Conclusions
This set of analyses is the most comprehensive to date, based on data accounting for 40% of the global case load. Simultaneously analysing data from various affected areas in Greater China together revealed consistencies and explained heterogeneities that would have otherwise remained unexplored. Our combined database is unique in that of the three regions, only mainland China is a member of the WHO whereas Hong Kong is an observer and Taiwan is a non-member. Such geo-political influences have posed an almost insurmountable challenge to official supranational agencies in pulling together the respective databases [20]. Database construction during an outbreak is critical to underpin analyses that will inform policy decisions regarding both disease control and treatment of infected patients. Key to the utility of such databases is their scope, format, accuracy and timeliness. While we have largely succeeded on the first two counts, the fact that we are only reporting results seven years after SARS receded into its animal reservoir points to an urgent deficiency in the global public health research infrastructure. Nevertheless, this report underscores the positive steps forward in recent years.
Our findings confirm the widely reported heterogeneous CFRs in the three regions [1,21,22]. However, discounting the highly selected XTS Hospital sample, the Beijing CFR approximated that of Hong Kong. On the other hand, Taiwan had a 64% higher adjusted case fatality compared to Hong Kong. Clearly one of the most important explanations for the observed low case fatality ratio in our subset of patients from Beijing is the inherent selection bias. While we studied 36% of the reported probable SARS cases in Beijing, from three of the largest SARS hospitals, our subset is by no means representative. The majority (74%) of our patients were from the XTS Hospital, a facility which was built especially to house SARS patients and opened halfway through the epidemic. Only one of the 680 inpatients was directly admitted, the remainder were transferred from other hospitals in Beijing. Although some of the XTS patients experienced symptom onset as early as the end of March, admission to XTS would have required survival until at least May 1, when XTS opened. Further, it is less likely that patients in serious condition (for example requiring mechanical ventilation) would have been transferred. As further confirmation of the systematic selection of the XTS sample, we found that patients admitted to XTS Hospital were epidemiologically biased, as shown by having shorter onset-to-admission periods and longer onset-to-discharge periods (data not shown).
An interesting related finding is that the relatively higher CFR also applied consistently to each subgroup including low risk groups such as younger patients and HCWs, which suggests that the presence of some common factors not included in our models (e.g. treatment protocols, hospital setting) may have independently increased CFRs in Taiwan. However, the treatment of choice in Hong Kong and Taiwan was the combined use of ribavirin and corticosteroids [14,23], and a large meta-analysis has shown that these treatments were likely ineffective [24]. We also observed similar patterns of CFRs for patients with the four most common comorbidities (diabetes, cardiovascular disease, ischaemic heart disease and chronic obstructive airways disease; data not shown) between Hong Kong and Taiwan and we did not observe exceptionally high case-fatality ratios among the patients with comorbidities in Taiwan. Hence the difference is probably not attributable to anti-viral or immunologic regimens but could have been related to different levels of general supportive care. Overall, our analysis found that age and pre-existing comorbid conditions were two major determinants of fatality, which is consistent with existing studies [14,25-30]. Male sex was significantly associated with increased risk of fatality in Hong Kong after adjustment for other important confounding factors, consistent with a previous study in Hong Kong that identified a sex effect in unadjusted analyses of aggregate data [31]. The reasons for an increase in risk of death among males remain unclear. In addition we found that admission before symptom onset, most likely due to nosocomial acquisition, was also significantly associated with higher fatality rate after adjustment for comorbidities in Taiwan [32].
In terms of epidemiologic parameters, the incubation period had mean 4.4, 5.7 and 6.9 days and a 95th percentile of 12.4, 19.7 and 17.9 days in Hong Kong, Beijing and Taiwan respectively, with some degree of variation between regions [18]. Together they can reliably inform the diagnostician the likelihood of SARS in a suspected case and advise the public health practitioner the appropriate period of quarantine. While most countries used a ten-day quarantine period, based on early estimates of the incubation period [33], our findings suggest that a longer period may be appropriate if SARS were to reemerge [29]. However differences between regions in the incubation distribution, as well as in the onset to discharge/death distributions discussed below, may be due to different interpretations of disease onset between the regions.
As would be expected, our results show that onset-to-admission periods shortened throughout the epidemic (Figure 2) as public awareness improved and public health interventions were implemented [14,34,35]. However, in the three regions, there was no evidence that shorter onset-to-admission period resulted in lower fatality (see Additional file 3), possibly due to the lack of effective treatment and that viremia only peaks after seven to ten days [26].
Taiwan's shorter onset-to-death distributions, indicating quicker deterioration, coupled with the consistently higher fatality ratios for most subgroups raises the possibility that the management of these patients did not compare favorably with those in the other two regions, especially if we assume the viral agent and host genetic susceptibility were similar throughout. However without more detailed clinical data, for example levels of viral load or as a proxy lactate dehydrogenase at admission reflecting initial illness severity [14,29], it is not possible to discern here whether management and treatment, or some other factors, were responsible for the higher fatality ratios in Taiwan. Alternatively, differences in environment may be responsible for some observed differences, given the known associations between for example smoking and respiratory disease [36,37]. The relatively longer onset-to-discharge periods in Beijing could likely be explained by different clinical or official protocols [38].
Our description of the variability between regions in symptoms at presentation (Figure 3) is the first such comparison in the literature. The higher rates in Hong Kong of almost every symptom could be due to differences in reporting (or asking) behavior. This again points to the need for a universal information supply chain, from case and symptom definitions to guidelines in history taking and data coding, for newly emerging or resurging diseases of supranational interest. As previously noted all three areas analyzed here shared the identical viral strain, as well as the same ethnic gene pool, so it is less likely that differences are due to the infective agent or host genetic factors. Although there are differences in the absolute rates of the various symptoms, we note that a previously derived clinical prediction rule for SARS [39] has been validated on patients from Taiwan [40].
Finally, a few limitations bear mention. As in most previous studies [14,29,41,42], our analysis was based on probable cases of SARS according to the WHO definition [13] rather than laboratory confirmed cases because the latter definition may be biased toward including more survivors, particularly among the earlier cases [14]. Furthermore, rapid diagnostic SARS tests were not available until fairly late in the epidemic and had poor sensitivity for detecting the disease [43,44]. The WHO case definitions may have been applied differently in the three regions, or a different percentage of probable cases might have been caused by other pathogens, which may have led to the observed differences. Furthermore, while SARS patients in Beijing were classified according to the WHO definition, but a more recent detailed case review has found that some reported 'probable' SARS cases may have been misclassified [45]. We note that odds ratios should be interpreted with caution since they may be a poor approximation to relative risks with outcomes that have a high prevalence. Asymptomatic and subclinical infections of SARS were not considered in our analysis, although there is strong evidence that very few existed [46]. A final limitation is that, as previously discussed, the Beijing patients in our database mostly were hospitalized in XTS Hospital and were found to be epidemiologically different from patients in other hospitals, which makes it difficult to generalize our results to all patients in Beijing.
Competing interests
The authors declare that they have no competing interests.
Authors' contributions
BJC and GML conceived and designed the study. EHYL, CAH and BJC performed the statistical analysis. EHYL, CAH, BJC and GML analyzed and interpreted the data. EHYL and BJC drafted the manuscript. CHC, TT and CWC provided the study materials or patient data. CAH, CAD and GML obtained the funding. CHC, LMH and CWC collected and collated the data. All authors critically reviewed the manuscript, read and approved the final manuscript.
Pre-publication history
The pre-publication history for this paper can be accessed here:
Supplementary Material
Characteristics of SARS patients in Hong Kong, Beijing and Taiwan. The associated case-fatality ratios and adjusted odds ratios (95% confidence intervals) are also reported. CFR, case fatality ratio; AOR, adjusted odds ratio; CI, confidence interval. * Patients with unknown age, pre-existing comorbid conditions or admission date were excluded. † Adjusted for sex, age, health care worker status, preexisting comorbid conditions and nosocomial infection. ‡ Data on final outcome were not available for 12 patients in Taiwan and were excluded for analysis. § The estimates were not shown as there was not more than 2 deaths in these age groups out of a relatively large number of patients. || Based on the WHO World Standard Population distribution [16].
Characteristics of SARS patients in Hong Kong, Beijing and Taiwan (pooled data). The associated case-fatality ratios and adjusted odds ratios (95% confidence intervals) are also reported. CFR, case fatality ratio; AOR, adjusted odds ratio; CI, confidence interval. * Data on final outcome were not available for 12 patients in Taiwan and were excluded for analysis. Patients with unknown age, pre-existing comorbid conditions or admission date were excluded from multivariable logistic regression models. † Adjusted for sex, age, health care worker status, preexisting comorbid conditions, nosocomial infection and region. ‡ Based on the WHO World Standard Population distribution [16].
Case fatality ratio by different onset-to-admission periods, Hong Kong, Beijing and Taiwan. CFR, case fatality ratio; CI, confidence interval. * Excluding 16 patients with unknown admission dates or discharge outcome.
Case fatality ratio by different onset-to-admission periods in Beijing, XTS Hospital, Hospital 302 and Hospital 309. CFR, case fatality ratio; CI, confidence interval.
Factors affecting the onset-to-death and onset-to-discharge period of SARS patients in Hong Kong, Beijing and Taiwan. CI, confidence interval. * The acceleration factor is computed as exp(β). It indicates the relative increase (>1) or decrease (<1) in the median time from onset of symptoms to death or discharge. † also adjusted for interaction between location with admission before symptom onset. ‡ also adjusted for interaction between location with health care worker and pre-existing comorbid conditions.
Factors affecting the onset-to-death and onset-to-discharge period of SARS patients in Hong Kong, Beijing (restricted to Hospitals 302 and 309 only and Taiwan. CI, confidence interval. * The acceleration factor is computed as exp(β). It indicates the relative increase (>1) or decrease (<1) in the median time from onset of symptoms to death or discharge. † also adjusted for interaction between location with admission before symptom onset. ‡ also adjusted for interaction between location with health care worker and pre-existing comorbid conditions.
Contributor Information
Eric HY Lau, Email: ehylau@hku.hk.
C Agnes Hsiung, Email: hsiung@nhri.org.tw.
Benjamin J Cowling, Email: bcowling@hku.hk.
Chang-Hsun Chen, Email: leonardo@cdc.gov.tw.
Lai-Ming Ho, Email: lmho@hku.hk.
Thomas Tsang, Email: thomas_tsang@dh.gov.hk.
Chiu-Wen Chang, Email: ccwen@cdc.gov.tw.
Christl A Donnelly, Email: c.donnelly@imperial.ac.uk.
Gabriel M Leung, Email: gmleung@hku.hk.
Acknowledgements
The authors thank all their colleagues in the Hong Kong Department of Health, the Hong Kong Hospital Authority, the 301, 302 and 309 hospitals in Beijing, and the Taiwan Center for Disease Control and National Health Research Institutes in Taiwan who were involved with the public health control of the SARS epidemics and data collection and processing. We thank Dr Baoxing Fan and colleagues at 301 Hospital of the PLA, Beijing, for abstracting and sharing the data on Beijing SARS patients as part of the SARSTRANS international collaboration. We also thank Steve Chan, Keith Tin and Pauline Woo for technical assistance. This work was supported in part through a commissioned research grant from the Research Fund for the Control of Infectious Diseases of the Health, Welfare, and Food Bureau of the Hong Kong Special Administrative Region Government (grant no. HKU-AA-17); by the University of Hong Kong SARS Research Fund; by the Taiwan Center for Disease Control SARS Research Fund; by the UK Medical Research Council; and by the EU Sixth Framework Programme for research for policy support (contract SP22-CT-2004-511066).
References
- Summary of probable SARS cases with onset of illness from 1 November 2002 to 7 August 2003. http://www.who.int/csr/sars/country/country2003_08_15.pdf
- Zhong NS, Zheng BJ, Li YM, Poon XZH, Chan KH, Li PH, Tan SY, Chang Q, Xie JP, Liu XQ. Epidemiology and cause of severe acute respiratory syndrome (SARS) in Guangdong, People's Republic of China, in February, 2003. Lancet. 2003;362:1353–1358. doi: 10.1016/S0140-6736(03)14630-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- CDC SARS Investigative Team. Update: outbreak of severe acute respiratory syndrome--worldwide, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:269–272. [PubMed] [Google Scholar]
- SARS outbreak contained worldwide. http://www.who.int/mediacentre/news/releases/2003/pr56/en/
- Escudero IH, Chen MI, Leo YS. Surveillance of severe acute respiratory syndrome (SARS) in the post-outbreak period. Singapore Med J. 2005;46:165–171. [PubMed] [Google Scholar]
- Watts J. SARS under control, but lab-safety questions remain. Lancet. 2004;363:1780. doi: 10.1016/S0140-6736(04)16344-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Heymann DL, Aylward RB, Wolff C. Dangerous pathogens in the laboratory: from smallpox to today's SARS setbacks and tomorrow's polio-free world. Lancet. 2004;363:1566–1568. doi: 10.1016/S0140-6736(04)16234-X. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chu DK, Poon LL, Chan KH, Chen H, Guan Y, Yuen KY, Peiris JS. Coronaviruses in bent-winged bats (Miniopterus spp.) J Gen Virol. 2006;87:2461–2466. doi: 10.1099/vir.0.82203-0. [DOI] [PubMed] [Google Scholar]
- Li W, Shi Z, Yu M, Ren W, Smith C, Epstein JH, Wang H, Crameri G, Hu Z, Zhang H. Bats are natural reservoirs of SARS-like coronaviruses. Science. 2005;310:676–679. doi: 10.1126/science.1118391. [DOI] [PubMed] [Google Scholar]
- Wang M, Yan M, Xu H, Liang W, Kan B, Zheng B, Chen H, Zheng H, Xu Y, Zhang E. SARS-CoV infection in a restaurant from palm civet. Emerg Infect Dis. 2005;11:1860–1865. doi: 10.3201/eid1112.041293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Civet cats found at restaurants again. http://www.chinadaily.com.cn/china/2007-02/14/content_808890.htm
- Liu W, Tang F, Fontanet A, Zhan L, Wang TB, Zhang PH, Luan YH, Cao CY, Zhao QM, Wu XM. Molecular epidemiology of SARS-associated coronavirus, Beijing. Emerg Infect Dis. 2005;11:1420–1424. doi: 10.3201/eid1109.040773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Case Definitions for Surveillance of Severe Acute Respiratory Syndrome (SARS) http://www.who.int/csr/sars/casedefinition/en/
- Leung GM, Hedley AJ, Ho LM, Chau P, Wong IO, Thach TQ, Ghani AC, Donnelly CA, Fraser C, Riley S. The epidemiology of severe acute respiratory syndrome in the 2003 Hong Kong epidemic: an analysis of all 1755 patients. Ann Intern Med. 2004;141:662–673. doi: 10.7326/0003-4819-141-9-200411020-00006. [DOI] [PubMed] [Google Scholar]
- Liang W, Zhu Z, Guo J, Liu Z, Zhou W, Chin DP, Schuchat A, Beijing Joint SEG. Severe acute respiratory syndrome, Beijing, 2003. Emerg Infect Dis. 2004;10:25–31. doi: 10.3201/eid1001.030553. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahmad OB, Boschi-Pinto C, Lopez AD, Murray CJ, Lozano R, Inoue M. Age Standardization of Rates: A New WHO Standard. Geneva: World Health Organization; 2000. [Google Scholar]
- Lee SH. The SARS epidemic in Hong Kong. J Epidemiol Community Health. 2003;57:652–654. doi: 10.1136/jech.57.9.652. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling BJ, Muller MP, Wong IO, Ho LM, Louie M, McGeer A, Leung GM. Alternative methods of estimating an incubation distribution: examples from severe acute respiratory syndrome. Epidemiology. 2007;18:253–259. doi: 10.1097/01.ede.0000254660.07942.fb. [DOI] [PubMed] [Google Scholar]
- R Development Core Team. R: A Language and Environment for Statistical Computing. Vienna: R Foundation for Statistical Computing; 2008. [Google Scholar]
- Editorial. Public health versus political frontiers. Lancet. 2007;369:616. doi: 10.1016/S0140-6736(07)60286-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chan KS, Zheng JP, Mok YW, Li YM, Liu YN, Chu CM, Ip MS. SARS: prognosis, outcome and sequelae. Respirology. 2003;8(Suppl):S36–40. doi: 10.1046/j.1440-1843.2003.00522.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galvani AP, Lei X, Jewell NP. Severe acute respiratory syndrome: temporal stability and geographic variation in case-fatality rates and doubling times. Emerg Infect Dis. 2003;9:991–994. doi: 10.3201/eid0908.030334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang JT, Sheng WH, Fang CT, Chen YC, Wang JL, Yu CJ, Chang SC, Yang PC. Clinical manifestations, laboratory findings, and treatment outcomes of SARS patients. Emerg Infect Dis. 2004;10:818–824. doi: 10.3201/eid1005.030640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stockman LJ, Bellamy R, Garner P. SARS: systematic review of treatment effects. PLoS Med. 2006;3:e343. doi: 10.1371/journal.pmed.0030343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ghani AC, Donnelly CA, Cox DR, Griffin JT, Fraser C, Lam TH, Ho LM, Chan WS, Anderson RM, Hedley AJ, Leung GM. Methods for estimating the case fatality ratio for a novel, emerging infectious disease. Am J Epidemiol. 2005;162:479–486. doi: 10.1093/aje/kwi230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peiris JS, Chu CM, Cheng VC, Chan KS, Hung IF, Poon LL, Law KI, Tang BS, Hon TY, Chan CS. Clinical progression and viral load in a community outbreak of coronavirus-associated SARS pneumonia: a prospective study. Lancet. 2003;361:1767–1772. doi: 10.1016/S0140-6736(03)13412-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen KT, Twu SJ, Chang HL, Wu YC, Chen CT, Lin TH, Olsen SJ, Dowell SF, Su IJ, Taiwan SRT. SARS in Taiwan: an overview and lessons learned. Int J Infect Dis. 2005;9:77–85. doi: 10.1016/j.ijid.2004.04.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Donnelly CA, Ghani AC, Leung GM, Hedley AJ, Fraser C, Riley S, Abu-Raddad LJ, Ho L-M, Thach T-Q, Chau P. Epidemiological determinants of spread of causal agent of severe acute respiratory syndrome in Hong Kong. Lancet. 2003;361:1761–1766. doi: 10.1016/S0140-6736(03)13410-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cowling BJ, Muller MP, Wong IOL, Ho L-M, Lo S-V, Tsang T, Lam TH, Louie M, Leung GM. Clinical prognostic rules for severe acute respiratory syndrome in low- and high-resource settings. Arch Intern Med. 2006;166:1505–1511. doi: 10.1001/archinte.166.14.1505. [DOI] [PubMed] [Google Scholar]
- Fowler RA, Lapinsky SE, Hallett D, Detsky AS, Sibbald WJ, Slutsky AS, Stewart TE. Critically ill patients with severe acute respiratory syndrome. JAMA. 2003;290:367–373. doi: 10.1001/jama.290.3.367. [DOI] [PubMed] [Google Scholar]
- Karlberg J, Chong DS, Lai WY. Do men have a higher case fatality rate of severe acute respiratory syndrome than women do? Am J Epidemiol. 2004;159:229–231. doi: 10.1093/aje/kwh056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang IS, Hsiung CA, Wen CC, Wu YJ, Yang CC. Non-parametric maximum-likelihood estimation in a semiparametric mixture model for competing-risks data. Scand J Statist. 2007;34:870–895. [Google Scholar]
- Severe acute respiratory syndrome--Singapore, 2003. MMWR Morb Mortal Wkly Rep. 2003;52:405–411. [PubMed] [Google Scholar]
- Liang WN, Liu M, Chen Q, Liu ZJ, He X, Pan Y, Xie XQ. Assessment of impacts of public health interventions on the SARS epidemic in Beijing in terms of the intervals between its symptom onset, hospital admission, and notification. Biomed Environ Sci. 2005;18:153–158. [PubMed] [Google Scholar]
- Cowling BJ, Ho LM, Leung GM. Effectiveness of control measures during the SARS epidemic in Beijing: a comparison of the Rt curve and the epidemic curve. Epidemiol Infect. 2008;136:562–566. doi: 10.1017/S0950268807008722. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brauer M, Hoek G, Van Vliet P, Meliefste K, Fischer PH, Wijga A, Koopman LP, Neijens HJ, Gerritsen J, Kerkhof M. Air pollution from traffic and the development of respiratory infections and asthmatic and allergic symptoms in children. Am J Respir Crit Care Med. 2002;166:1092–1098. doi: 10.1164/rccm.200108-007OC. [DOI] [PubMed] [Google Scholar]
- Ponce de Leon A, Anderson HR, Bland JM, Strachan DP, Bower J. Effects of air pollution on daily hospital admissions for respiratory disease in London between 1987-88 and 1991-92. J Epidemiol Community Health. 1996;50(Suppl 1):s63–70. doi: 10.1136/jech.50.Suppl_1.s63. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Battling the spread of SARS, Asian nations escalate travel restrictions. http://www.iht.com/articles/2003/04/12/a7_20.php
- Leung GM, Rainer TH, Lau FL, Wong IO, Tong A, Wong TW, Kong JH, Hedley AJ, Lam TH. A clinical prediction rule for diagnosing severe acute respiratory syndrome in the emergency department. Ann Intern Med. 2004;141:333–342. doi: 10.7326/0003-4819-141-5-200409070-00106. [DOI] [PubMed] [Google Scholar]
- Ma MH, Chen SY, Chiang WC, Su CP, Chen WJ. A clinical prediction rule for the severe acute respiratory syndrome. Ann Intern Med. 2005;142:225. doi: 10.7326/0003-4819-142-3-200502010-00019. [DOI] [PubMed] [Google Scholar]
- Chow KY, Lee CE, Ling ML, Heng DM, Yap SG. Outbreak of severe acute respiratory syndrome in a tertiary hospital in Singapore, linked to an index patient with atypical presentation: epidemiological study. BMJ. 2004;328:195. doi: 10.1136/bmj.37939.465729.44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Booth CM, Matukas LM, Tomlinson GA, Rachlis AR, Rose DB, Dwosh HA, Walmsley SL, Mazzulli T, Avendano M, Derkach P. Clinical features and short-term outcomes of 144 patients with SARS in the greater Toronto area. JAMA. 2003;289:2801–2809. doi: 10.1001/jama.289.21.JOC30885. [DOI] [PubMed] [Google Scholar]
- Chan KH, Poon LL, Cheng VC, Guan Y, Hung IF, Kong J, Yam LY, Seto WH, Yuen KY, Peiris JS. Detection of SARS coronavirus in patients with suspected SARS. Emerg Infect Dis. 2004;10:294–299. doi: 10.3201/eid1002.030610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Poon LL, Chan KH, Wong OK, Yam WC, Yuen KY, Guan Y, Lo YM, Peiris JS. Early diagnosis of SARS coronavirus infection by real time RT-PCR. J Clin Virol. 2003;28:233–238. doi: 10.1016/j.jcv.2003.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang W, McLaws ML, Liu M, Mi J, Chan DK. Hindsight: a re-analysis of the severe acute respiratory syndrome outbreak in Beijing. Public Health. 2007;121:725–733. doi: 10.1016/j.puhe.2007.02.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leung GM, Lim WW, Ho LM, Lam TH, Ghani AC, Donnelly CA, Anderson RM. Seroprevalence of IgG antibodies to SARS-coronavirus in asymptomatic or subclinical population groups. Epidemiol Infect. 2003;134:211–221. doi: 10.1017/S0950268805004826. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Characteristics of SARS patients in Hong Kong, Beijing and Taiwan. The associated case-fatality ratios and adjusted odds ratios (95% confidence intervals) are also reported. CFR, case fatality ratio; AOR, adjusted odds ratio; CI, confidence interval. * Patients with unknown age, pre-existing comorbid conditions or admission date were excluded. † Adjusted for sex, age, health care worker status, preexisting comorbid conditions and nosocomial infection. ‡ Data on final outcome were not available for 12 patients in Taiwan and were excluded for analysis. § The estimates were not shown as there was not more than 2 deaths in these age groups out of a relatively large number of patients. || Based on the WHO World Standard Population distribution [16].
Characteristics of SARS patients in Hong Kong, Beijing and Taiwan (pooled data). The associated case-fatality ratios and adjusted odds ratios (95% confidence intervals) are also reported. CFR, case fatality ratio; AOR, adjusted odds ratio; CI, confidence interval. * Data on final outcome were not available for 12 patients in Taiwan and were excluded for analysis. Patients with unknown age, pre-existing comorbid conditions or admission date were excluded from multivariable logistic regression models. † Adjusted for sex, age, health care worker status, preexisting comorbid conditions, nosocomial infection and region. ‡ Based on the WHO World Standard Population distribution [16].
Case fatality ratio by different onset-to-admission periods, Hong Kong, Beijing and Taiwan. CFR, case fatality ratio; CI, confidence interval. * Excluding 16 patients with unknown admission dates or discharge outcome.
Case fatality ratio by different onset-to-admission periods in Beijing, XTS Hospital, Hospital 302 and Hospital 309. CFR, case fatality ratio; CI, confidence interval.
Factors affecting the onset-to-death and onset-to-discharge period of SARS patients in Hong Kong, Beijing and Taiwan. CI, confidence interval. * The acceleration factor is computed as exp(β). It indicates the relative increase (>1) or decrease (<1) in the median time from onset of symptoms to death or discharge. † also adjusted for interaction between location with admission before symptom onset. ‡ also adjusted for interaction between location with health care worker and pre-existing comorbid conditions.
Factors affecting the onset-to-death and onset-to-discharge period of SARS patients in Hong Kong, Beijing (restricted to Hospitals 302 and 309 only and Taiwan. CI, confidence interval. * The acceleration factor is computed as exp(β). It indicates the relative increase (>1) or decrease (<1) in the median time from onset of symptoms to death or discharge. † also adjusted for interaction between location with admission before symptom onset. ‡ also adjusted for interaction between location with health care worker and pre-existing comorbid conditions.