Abstract
Background
Clinical and functional imaging evidence suggests that cerebellar dysfunction occurs in essential tremor (ET). In recent postmortem studies, we documented increased numbers of torpedoes (Purkinje cell axonal swellings) in ET patients without Lewy bodies. Purkinje cell loss, however, has never been rigorously assessed.
Objective
To quantitatively assess the number of Purkinje cells in brains of ET patients and similarly aged controls.
Methods
Postmortem cerebellar tissue was available in 14 ET cases (6 with Lewy bodies and 8 without Lewy bodies) and 11 controls. Calbindin immunohistochemistry was performed on paraffin sections of the cerebellum. Images were digitally recorded and blinded measurements of the number of Purkinje cells per millimeter of cell layer (linear density) were made.
Results
Purkinje cell linear density was inversely correlated with age (r=-0.53, P=.006) and number of torpedoes (r=-0.42, P=.04). Purkinje cell linear density differed by diagnosis (mean [SD], controls, 3.46 [1.27] cells/mm; ET cases with Lewy bodies, 3.33 [1.06] cells/mm; and ET cases without Lewy bodies, 2.14 [0.82] cells/mm; P=.04), with the most significant difference between ET cases without Lewy bodies and controls, where the reduction was 38.2% (P=.04). In an adjusted linear regression analysis that compared ET cases without Lewy bodies with controls, decreased linear density (outcome variable) was associated with ET (β=.56, P=.03).
Conclusions
We demonstrated a reduction in Purkinje cell number in the brains of patients with ET who do not have Lewy bodies. These data further support the view that the cerebellum is anatomically, as well as functionally, abnormal in these ET cases.
ESSENTIAL TREMOR (ET) IS A common and often progressive neurological disease, with a prevalence of approximately 4% among adults aged 40 years and older.1-3 There have been few postmortem ET studies.4-9 While these studies did not reveal consistent structural abnormalities, several noted mild to marked loss of Purkinje cells. However, as none of these were controlled studies (ie, there were no control brains for comparison), it was not clear whether this finding represented a normal age-related change.
Clinical and functional imaging evidence suggests that cerebellar dysfunction occurs in ET,10-13 and magnetic resonance spectroscopic imaging suggests that metabolic abnormalities occur; these abnormalities might represent neuronal loss.4 In several recent postmortem studies,14,15 we documented a marked increase in the number of Purkinje cell axonal swellings, torpedoes, in ET. In one ET case, the pathologic changes in the cerebellum were more manifest, with degenerative changes in the dentate nucleus.15 However, quantification of Purkinje cells was not rigorous in these earlier reports,14,15 thus it was not clear whether these torpedoes in the ET cerebellum were accompanied by Purkinje cell loss. To address this question, we quantitatively assessed cerebellar Purkinje cell numbers by measuring linear cell densities in ET patients' brains and controls' brains. This is the only study, to our knowledge, that has attempted to do so.
Announcement.
Trial Registration Required. In concert with the International Committee of Medical Journal Editors (ICMJE), Archives of Neurology will require, as a condition of consideration for publication, registration of all trials in a public trials registry (such as http://ClinicalTrials.gov). Trials must be registered at or before the onset of patient enrollment. This policy applies to any clinical trial starting enrollment after July 1, 2005. For trials that began enrollment before this date, registration will be required by September 13, 2005, before considering the trial for publication. The trial registration number should be supplied at the time of submission.
For details about this new policy, and for information on how the ICMJE defines a clinical trial, see the editorial by DeAngelis et al in the January issue of Archives of Dermatology (2005;141:76-77). Also see the Instructions to Authors on our Web site: www.archneurol.com.
METHODS
PARTICIPANTS
This study was conducted at the Essential Tremor Centralized Brain Repository (ETCBR) at Columbia University, New York, New York. Postmortem tissue from the cerebellum was available in 14 ET cases (5 were not included in earlier reports14,15) and 11 control brains (1 was not included in earlier reports14,15). The ET cases included 5 archival and 9 prospectively collected cases. All brains were well characterized by the New York Brain Bank, Columbia University Medical Center, and underwent complete neuropathologic assessment (among other things, this included alphasynuclein-stained sections of the dorsal vagal nucleus, locus ceruleus, and substantia nigra pars compacta; New York Brain Bank Web site, http://nybb.hs.columbia.edu) and determination of any pathologic findings. Each brain was rated by Braak and Braak staging16 for Alzheimer neurofibrillary changes and by Consortium to Establish a Registry for Alzheimer's Disease (CERAD) staging17 for plaque pathology.
The 5 archival ET cases comprised 2 from the New York Brain Bank, 2 from the Honolulu-Asia Aging Study, and 1 from the University of Kansas Brain Bank. In 3 of the 5 archival ET cases, the treating neurologists, all of whom were neurologists specializing in movement disorders, had assigned the ET diagnoses while the patients were alive. The ETCBR neurologists obtained clinical records (office records from treating internists and neurologists) to acquire data about tremor type, distribution, severity, and duration; coexistence of other medical and neurological disorders; and medications. Using these records, an ETCBR neurologist who specialized in movement disorders confirmed their diagnoses post mortem using ETCBR diagnostic criteria, which were modeled after the diagnostic criteria for ET proposed in the Consensus Statement of the Movement Disorder Society.18 The ETCBR criteria were as follows: (1) bilateral action tremor of the arms for 5 or more years with a diagnosis of ET during life, (2) head tremor or moderate or severe action tremor of at least one hand (ie, tremor resulted in difficulty with 2 or more activities of daily living or required medication), and (3) action tremor was not the result of other movement disorders, hyperthyroidism, other medical conditions, or medications.14 During serial assessments, the 2 archival ET patients from the Honolulu-Asia Aging Study had repeatedly demonstrated moderate to severe bilateral hand tremor in the absence of parkinsonism and other etiologies but had not received a diagnosis of ET during their lives.
The 9 prospectively collected ET cases were all recruited through International Essential Tremor Foundation newsletters. International Essential Tremor Foundation members who were interested in brain donation responded to these quarterly brain bank advertisements.19 Each patient had ET diagnosed by his or her treating neurologist. To reconfirm these diagnoses, members interested in brain donation were mailed standardized clinical questionnaires (which included screening questions for Parkinson disease and spinocerebellar ataxia and family history information) and written instructions to assist them in the preparation of a videotaped neurological examination. Based on the instructions, they prepared a 30-minute videotaped neurological examination, following the sequential instructions. The videotape included (1) a full tremor demonstration (assessments of postural arm tremor, rest tremor [while seated and while walking], kinetic tremor [while pouring, using a spoon, drinking, drawing a spiral, and performing the finger-nose-finger maneuver with each hand], head tremor, chin tremor, and voice tremor), (2) elicitation of parkinsonism with items from the motor portion of the Unified Parkinson's Disease Rating Scale20 (facial expression and blink frequency while seated and facing the camera, speech, rest tremor in each limb evaluated while seated and while walking, rapid alternating movements [opening and closing each hand, pronating and supinating each hand, and foot taps], arising from a chair to a standing position, standing with arms at the sides, and walking for 60 seconds), and (3) an assessment of cerebellar signs with items taken from the International Cooperative Ataxia Rating Scale21 (as noted, speech, 3 types of rapid alternating movements, finger-nose-finger maneuver, drawing spirals with each hand, sitting, stance, and gait). Using these records, an ETCBR neurologist who specialized in movement disorders confirmed patients' diagnoses after death using ETCBR diagnostic criteria, which were modeled after the criteria proposed in the Consensus Statement of the Movement Disorder Society.18
Ten of 11 control brains were obtained through the New York Brain Bank. These were individuals who had been enrolled as healthy elderly controls in the Alzheimer's Disease Research Center or the Washington Heights Inwood Columbia Aging Project; they were followed up prospectively with serial neurological assessments, remaining free of a diagnosis of Alzheimer disease, ET, or Parkinson disease during life and not having significant neuropathologic changes on postmortem evaluation. These 10 controls were selected for this study based on their age (ie, they were frequency matched to ET participants based on age). One control brain was obtained from the Honolulu-Asia Aging Study as a match for the 2 cases from that study. This person had remained free of a neurological diagnosis during life.
Demographic and clinical information was collected on all cases and controls (from treating physicians and also directly from the patient in prospectively collected cases). Heavy ethanol use was defined as a man consuming a mean of 4 or more standard drinks (15 mL of absolute ethanol) per day or a woman consuming 3 or more standard drinks per day.22 Lifetime exposure to medications known to cause cerebellar damage (eg, lithium and diphenylhydantoin) was assessed.
PROCESSING TISSUE
Postmortem interval (PMI) was the number of hours between death and placement of the brain in a cold room or on ice. For the current analyses, the cerebellum was our primary region of interest because many studies have implicated its involvement in ET.10-15,23 A 3×20×25-mm parasagittal tissue block that came from the same region of the neocerebellum in cases and controls and included, in continuity, the cerebellar cortex, white matter, and dentate nucleus, was harvested from each brain and then immersion fixed in buffered formalin, 10%.14,15 Paraffin sections (7 μm) were stained with Luxol fast blue and hematoxylin and eosin for general tissue survey and quantification of torpedoes.
IMMUNOHISTOCHEMISTRY
Paraffin sections measuring 7 μm × 20 mm × 25 mm were placed on subbed glass slides. Calbindin immunoreactivity was evaluated using a primary mouse monoclonal antibody to calbindin D-28K (clone CG-955, Sigma-Aldrich Corp, St Louis, Missouri). Sections were deparaffinized, incubated in proteinase K, 0.1% (Sigma-Aldrich Corp), at room temperature for 10 minutes, washed, and then treated with hydrogen peroxide, 3%. All washes used phosphate-buffered saline. Secondary antibody treatment with antimouse IgG was visualized using avidin-biotin peroxidase complex (Vectastain Elite ABC; Vector Laboratories, Burlingame, California) with the chromogen 3,3-diaminobenzidine (DAB Substrate Kit, Vector Laboratories). For each brain, staining was also performed in the absence of primary antibody to be certain no nonspecific 3,3-diaminobenzidine reaction product was present.
ASSESSMENT OF PURKINJE CELL LINEAR DENSITY AND TORPEDOES
Sections were examined using a microscope with an ×4 objective. A color charged-coupling device video camera, a video capture card, and Videum 2.9.3a (Winnov, Santa Clara, California) Windows software were used to digitally record microscopic images. These were analyzed to quantify Purkinje cell linear density by a trained technician who was blinded to all clinical information and diagnoses. Slides were photographed with the dentate situated on the right and the folia branches extending leftward. For photographing, folia were labeled numerically and the 2 folia located most central in the slide were selected. Within each of these 2 folia, 4 smaller subregions consisting of the 2 most distal peaks (gyri) and the 2 most distal troughs (sulci) were chosen so that there were 8 subregions per participant. The photographs were arranged sequentially and the Purkinje cell layer was measured using Scion Image Software for Windows Beta 4.0.2 (Scion Corporation, Frederick, Maryland). Purkinje cells with visible nuclei were counted. Purkinje cell layer length and the number of nucleated Purkinje cells were summed from each of the 8 sub-regions and represented linear cell density (ie, Purkinje cells per millimeter of Purkinje cell layer). To assess the test-retest reliability of these estimates of Purkinje cell linear cell density, the trained tester repeated the analysis after several months on newly prepared and stained sections from 3 participants and obtained similar results (correlation between Purkinje cell linear densities measured at 2 different sessions, r=0.98). We also conducted a study in which we examined the consistency of our counts across different sections from the same tissue block. In 5 participants, the trained tester performed the same analysis on 2 different sections from the same block. Section-section agreement was high (r=0.99, with a mean 7.3% section-section difference in estimates of Purkinje cell linear density). Based on this high level of agreement, measurements were made on one cerebellar section per participant, though, as described, 8 regions were examined per section. To quantify torpedoes, the hematoxylin-eosin-stained 20×25-mm section was used and the number of torpedoes in the entire section was counted.
STATISTICAL ANALYSIS
In a previous study,14 ET cases demonstrated 2 patterns of pathologic changes: ET cases with Lewy bodies vs ET cases without Lewy bodies. As reported previously,14 these Lewy bodies were primarily found in the locus ceruleus. The number of cerebellar torpedoes was significantly increased in the ET cases without Lewy bodies.14 This pathologic subdivision of ET cases was also applied in the current analyses and all cases fell into 1 of these 2 categories.
Statistical analyses were performed using SPSS, version 13.0 (SPSS Inc, Chicago, Illinois). We used χ2 tests, t tests, and analysis of variance to compare ET cases with controls in terms of age, sex, and other characteristics. Pearson coefficients (r) were used to assess correlations between continuous, normally distributed variables. Purkinje cell linear densities were compared among diagnostic groups using t tests and analysis of variance. In an unadjusted linear regression analysis, in which the dependent variable was Purkinje cell linear density, we compared diagnostic groups. This model was then adjusted for age, sex, and PMI. We also tested for a trend in Purkinje cell linear density using a similar linear regression model that included all 3 diagnostic groups (controls [reference group], ET cases with Lewy bodies, and ET cases without Lewy bodies). In some analyses, ET cases were stratified into those with 10 or more torpedoes vs those with fewer than 10.
RESULTS
The 14 ET cases were similar to the 11 controls in terms of age, sex, race, PMI, and brain weight. None of the cases or controls had a history of heavy ethanol use or exposure to a medication known to cause cerebellar damage (Table). The mean number of torpedoes was 10 times higher in ET cases without Lewy bodies (mean [SD], 10.8 [6.3]) than in controls (1.2 [1.1]). One of the ET cases with Lewy bodies had Alzheimer disease (CERAD plaque score, C; Braak and Braak stage, V).
Table.
Demographic, Clinical, and Pathologic Features of Essential Tremor (ET) Cases and Controls
| Characteristic | All ET Cases | ET Cases With Lewy Bodies | ET Cases Without Lewy Bodies | Controls |
|---|---|---|---|---|
| No. of cases | 14 | 6 | 8 | 11 |
| Mean age (SD), y | 88.0 (7.7) | 89.0 (4.2) | 87.3 (9.8) | 84.6 (8.8) |
| Male sex, No. (%) | 7 (50) | 4 (66.7) | 3 (37.5) | 7 (63.6) |
| White race, No. (%) | 12 (85.7) | 4 (66.7) | 8 (100) | 10 (90.9) |
| Mean postmortem interval (SD), h | 6.7 (3.4) | 8.9 (3.1) | 5.7 (3.3) | 7.3 (9.3) |
| Mean brain weight (SD), g | 1169.7 (335.8) | 1241.9 (133.9) | 1115.5 (434.5) | 1238.1 (129.2) |
| History of heavy ethanol use, No. (%) | 0 | 0 | 0 | 0 |
| Treated with a medication for ET, No. (%) | 10 (74.1)a | 5 (83.3)a | 5 (62.5)b | 0 |
| Lifetime exposure to a medication known to cause cerebellar damage, No. (%) | 0 | 0 | 0 | 0 |
| Mean duration of tremor (SD, range), y | 27.9 (21.2, 5-65) | 26.0 (27.8, 5-65) | 29.1 (18.0, 9-57) | Not applicable |
| Family history of ET, first-degree relative, No. (%) | 6 (42.9)a | 2 (33.3)c | 4 (50.0)b | 0 |
| Family history of Parkinson disease, first-degree relativ, No. (%) | 0 | 0 | 0 | 0 |
| Mean No. of torpedoes (SD) | 8.2 (6.3)b | 4.8 (4.8) | 10.8 (6.3)a | 1.2 (1.1) |
| Mean Purkinje cell linear density (SD), cells/mm | 2.64 (1.09) | 3.33 (1.06) | 2.14 (0.82)c | 3.46 (1.27) |
P < .001 compared with controls
P < .01 compared with controls.
P < .05 compared with controls.
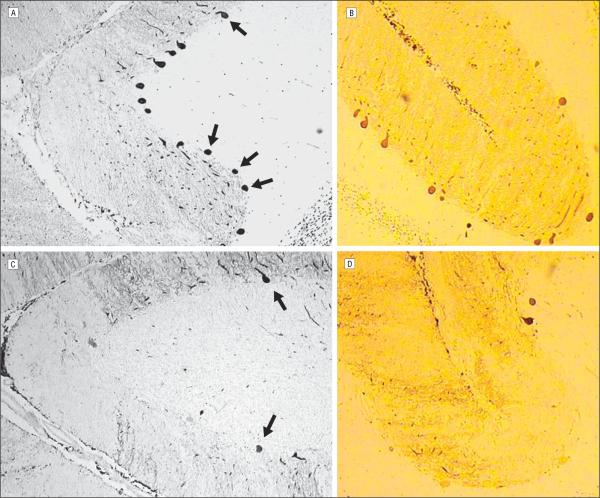
Purkinje cell linear density differed by diagnosis (mean [SD], controls, 3.46 [1.27] cells/mm [n=11]; ET cases with Lewy bodies, 3.33 [1.06] cells/mm [n=8]; and ET cases without Lewy bodies, 2.14 [0.82] cells/mm [n=6]; F=3.71; P=.04). In this analysis, there was a significant 38.2% difference (P=.04) between ET cases without Lewy bodies and controls (Figure 1 and Figure 2). Combining all 14 ET cases into one group, mean Purkinje cell linear density was 2.64 (SD, 1.09) cells/mm (ie, 23.5% lower than that of controls), with a P value for the casecontrol comparison that was of marginal significance (t=1.72, P=.1).
Figure 1.
Purkinje cell linear density differed by diagnosis (mean [SD], controls, 3.46 [1.27] cells/mm; essential tremor [ET] cases with Lewy bodies,3.33 [1.06] cells/mm; and ET cases without Lewy bodies, 2.14 [0.82] cells/mm; F=3.71; P=.04), with a 38.2% difference between ET cases without Lewy bodies and controls (P=.04). Bars show SE.
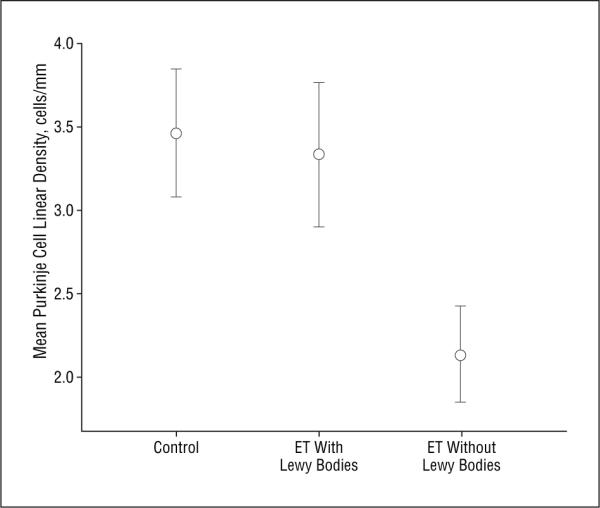
Figure 2.
Representative photographs (original magnification ×40) of calbindin immunohistochemistry on similar cerebellar folia sections from 2 individuals: an 84-year-old healthy control (A and B) and a 90-year-old patient with essential tremor (C and D). It is evident that whereas 12 Purkinje cells are seen in the Purkinje layer of the control (A, 4 denoted by arrows), only 2 are seen in the patient with essential tremor (C, arrows). Numerous Purkinje cell bodies are densely stained in the control (B), whereas there are only 2 evident in the patient with essential tremor (D). The Purkinje cell linear density was 4.29 cells/mm in the control and 1.27 cells/mm in the patient with essential tremor.
In our sample of 14 ET cases and 11 controls, Purkinje cell linear density was inversely correlated with age (r=-0.53, P=.006); with every 1-year increase in age, Purkinje cell linear density declined by 0.08 cells/mm. Purkinje cell linear density was also inversely correlated with the number of torpedoes (r=0.42, P=.04); with each 1-torpedo increase, Purkinje cell linear density declined by 0.08 cells/mm. Purkinje cell linear density did not correlate with PMI (r=0.24, P=.33), CERAD plaque score (r=0.60, P=.78), Braak and Braak stage (r=-0.32, P=.14), or brain weight (r=0.34, P=.11), nor did it differ between men and women (neither in the total sample nor when stratified by diagnosis).
In an unadjusted linear regression analysis that compared ET cases without Lewy bodies (n=8) with controls (n=11), Purkinje cell linear density (outcome variable) was lower in ET cases without Lewy bodies than in controls (β=.66, P=.02). Adjusting in this model for age, sex, and PMI, the association remained significant (β=.56, P=.03). Adjusting for brain weight in the same model did not change the results either (β=.56, P=.03).
In an unadjusted linear regression analysis that included all participants (ie, a test for trend), Purkinje cell linear density (outcome variable) was associated with diagnosis (controls [reference group], ET cases with Lewy bodies, and ET cases without Lewy bodies; test for trend, β=.64, P=.02) After adjusting for age, sex, and PMI, this association remained significant (test for trend β=.56, P=.03). Starting with the same adjusted model and further adjusting for brain weight or for Braak and Braak stage and CERAD plaque score did not change the results. Removing the one ET case with Alzheimer disease did not change these results either.
We further stratified ET cases without Lewy bodies into those with 10 or more torpedoes (n=3) vs those with fewer than 10 torpedoes (n=5). Mean Purkinje cell linear density was 1.42 (SD, 0.41) cells/mm in ET cases with 10 or more torpedoes, which was 59.0% lower than that of controls (3.46 [SD, 1.27] cells/mm, P=.04). Mean Purkinje cell linear density was 2.57 (SD, 0.69) cells/mm in ET cases with fewer than 10 torpedoes. This was 25.7% lower (P=.43) than that of controls (Figure 3).
Figure 3.
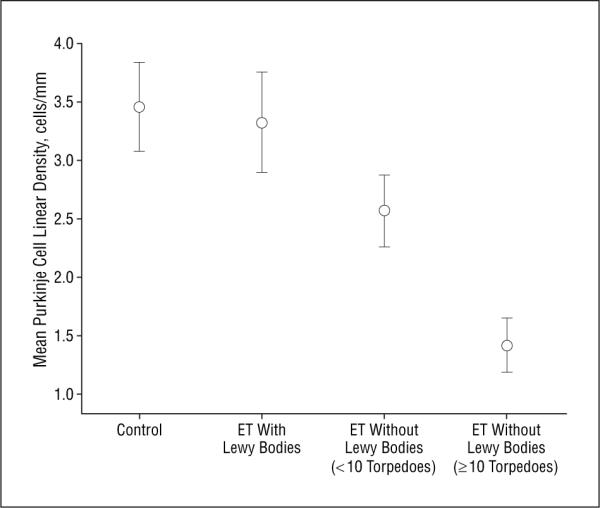
We stratified essential tremor (ET) cases without Lewy bodies into those with 10 or more torpedoes (n=3) and those with fewer than 10 torpedoes (n=5). Purkinje cell linear density was lower in those with 10 or more torpedoes (mean [SD], 1.42 [0.41] cells/mm or 59.0% lower than that of controls) than in those with fewer than 10 torpedoes (2.57 [0.69] cells/mm or 25.7% lower than that of controls). For comparison of those with 10 or more vs fewer than 10 torpedoes, t=2.59, P=.04. Bars show SE.
COMMENT
This study has sought to further elucidate the pathogenesis of ET. Converging clinical and neuroimaging data suggest the presence of cerebellar dysfunction in ET,10-15,23 and recent postmortem studies have shown the existence of microscopic changes (Purkinje cell swellings) in the cerebellum of most ET cases.14,15 The loss of Purkinje cells in the ET cerebellum rarely has been commented on. However, a quantitative comparison of the number of Purkinje cells in ET vs control brains has never been undertaken. Thus, the actual loss of Purkinje cells in a subset of ET brains has not been formally assessed. In this study, we demonstrated that ET patients without Lewy bodies had a significant reduction in the number of Purkinje cells compared with a similarly aged control group.
In the older literature, authors occasionally commented briefly on the presence of Purkinje cell loss in some of their ET cases. In one case, this loss was mild,7 whereas in 3 others it was more marked.4-6 In a more recent study, Rajput et al9 commented on the presence of mild Purkinje cell loss in 2 of their 20 ET cases.9 However, as mentioned, none of these studies performed a formal quantification of Purkinje cell number and none compared these ET case brains with control brains. Although we demonstrated a reduction in Purkinje cells in ET patients without Lewy bodies, the reduction was modest (approximately 40%), which is less than that which has been reported in patients with multiple system atrophy (60%-75% in postmortem studies).24,25
We found that Purkinje cell linear density was inversely associated with age. With healthy aging, the loss of Purkinje cells has been estimated to be 2.5% to 5.0% per decade.26-28 This underscores the importance of the use of a healthy age-matched comparison group. It also lends validity to our method of assessing Purkinje cell linear density (ie, failure to demonstrate this association between age and Purkinje cell linear density would have raised concerns about the validity of our linear density data).
We also found an inverse correlation between linear density of Purkinje cells and the number of torpedoes. This further corroborates the validity of our measure of linear density of Purkinje cells and suggests that torpedoes and Purkinje cell loss may be concomitant features of cerebellar degeneration.
As in our previous study,14 ET cases could be divided into groups based on the presence or absence of Lewy bodies. Essential tremor patients with Lewy bodies have them (Lewy bodies) in the locus ceruleus and have a relatively low number of torpedoes, whereas ET patients without Lewy bodies have increased numbers of torpedoes and, as we have now demonstrated, a reduction in Purkinje cell number. Essential tremor patients with Lewy bodies had a similar Purkinje cell linear density as controls, further supporting the notion that there are pathologic subtypes of ET.14 This pathologic subdivision of ET cases seems to indicate, as has been suggested recently,29,30 that ET may be a family of diseases unified by the presence of action tremor that is further characterized by etiological, clinical, and pathologic heterogeneity. The clinical features that distinguish ET cases with Lewy bodies vs without are not established and are currently under investigation. That some cases of ET have Lewy bodies as their primary pathologic manifestation converges with a wealth of clinical data that center on the apparent links between ET and Parkinson disease.31-38 The development of Parkinson disease has often been described in ET patients,31,32,38 and ET-like action tremor is more common in Parkinson disease families than in control families,34 again, further demonstrating the links between ET and Lewy body disease. Whether ET patients with Lewy bodies are more prone to develop Parkinson disease than their counterparts without Lewy bodies is currently unknown.
The mean Purkinje cell linear density that we report for our controls was 3.46 (SD, 1.27) cells/mm. A range of mean linear Purkinje cell densities has been reported among healthy controls, with some studies reporting results as low as 1.6 cells/mm39 and others in the range of 2 to 3 cells/mm (2.36 cells/mm25 and 2.5-3 cells/mm40), 4 to 5 cells/mm (4.49 cells/mm,41 4.6 cells/mm,42 and 4.6 cells/mm43), 6 to 7 cells/mm (6.9 cells/mm44 and 7.1 cells/mm45), and 10 to 11 cells/mm.46 This variability is likely caused by a variety of issues, including technical factors, such as fixation shrinkage, staining techniques, and section thickness, but also by demographic differences including age. Our numbers are within the reported range.
This study had limitations. First, we sampled only one region of the cerebellar hemisphere. This does not diminish the validity of our findings. However, it remains to be demonstrated that these findings can be generalized to other regions of the ET cerebellum (eg, vermis). Second, a stereological assessment of Purkinje cell number would have allowed for greater precision as well as a randomized assessment. Such a study is currently under way. Third, while the number of participants seems relatively small, this actually represents the second largest series of reported ET cases, with all except one previous study9 reporting the results of only 1 or 2 cases. With our sample size, statistically significant findings were demonstrable. The strengths of this study include its use of a standardized, blinded, quantitative assessment of Purkinje cells and control brains for comparison. In addition, we could adjust for a number of important potential confounders (eg, age and PMI). Finally, we were able to examine the associations between linear density of Purkinje cells and other pathologic changes in the cerebellum (ie, torpedoes).
In summary, we demonstrated a reduction in Purkinje cell number in ET patients without Lewy bodies. These data further support the view that the cerebellum is functionally and structurally abnormal in these ET cases.
Acknowledgments
Funding/Support: This study was supported by grants R01 NS42859, 5R01 AG017155, P50 AG08702, and P01 AG07232 from the National Institutes of Health, Bethesda, Maryland; by the International Essential Tremor Foundation, Lenexa, Kansas; and by the Parkinson's Disease Foundation, New York, New York.
Footnotes
Financial Disclosure: None reported.
REFERENCES
- 1.Louis ED, Marder K, Cote L, et al. Differences in the prevalence of essential tremor among elderly African Americans, whites, and Hispanics in northern Manhattan, NY. Arch Neurol. 1995;52(12):1201–1205. doi: 10.1001/archneur.1995.00540360079019. [DOI] [PubMed] [Google Scholar]
- 2.Dogu O, Sevim S, Camdeviren H, et al. Prevalence of essential tremor: door-to-door neurological exams in Mersin Province, Turkey. Neurology. 2003;61(12):1804–1807. doi: 10.1212/01.wnl.0000099075.19951.8c. [DOI] [PubMed] [Google Scholar]
- 3.Benito-León J, Bermejo-Pareja F, Morales JM, Vega S, Molina JA. Prevalence of essential tremor in three elderly populations of central Spain. Mov Disord. 2003;18(4):389–394. doi: 10.1002/mds.10376. [DOI] [PubMed] [Google Scholar]
- 4.Hassler R. Zur pathologischen Anatomie des senilen und des parkinsonistischen Tremor. J Psychol Neurol. 1939;49:193–230. [Google Scholar]
- 5.Mylle G, Van Bogaert L. Etudes anatomo-cliniques de syndromes hypercinetiques complexes, I: sur le tremblement familial. Monatsschr Psychiatr Neurol. 1940;103:28–43. [Google Scholar]
- 6.Mylle G, van Bogaert L. Du tremblement essentiel non-familial. Monatsschr Psychiatr Neurol. 1948;115:80–90. [Google Scholar]
- 7.Herskovits E, Blackwood W. Essential (familial, hereditary) tremor: a case report. J Neurol Neurosurg Psychiatry. 1969;32(6):509–511. doi: 10.1136/jnnp.32.6.509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rajput AH, Rozdilsky B, Ang L, Rajput A. Clinicopathological observations in essential tremor: report of six cases. Neurology. 1991;41(9):1422–1424. doi: 10.1212/wnl.41.9.1422. [DOI] [PubMed] [Google Scholar]
- 9.Rajput A, Robinson CA, Rajput AH. Essential tremor course and disability: a clinicopathologic study of 20 cases. Neurology. 2004;62(6):932–936. doi: 10.1212/01.wnl.0000115145.18830.1a. [DOI] [PubMed] [Google Scholar]
- 10.Deuschl G, Wenzelburger R, Loffler K, Raethjen J, Stolze H. Essential tremor and cerebellar dysfunction: clinical and kinematic analysis of intention tremor. Brain. 2000;123:1568–1580. doi: 10.1093/brain/123.8.1568. [DOI] [PubMed] [Google Scholar]
- 11.Helmchen C, Hagenow A, Miesner J, et al. Eye movement abnormalities in essential tremor may indicate cerebellar dysfunction. Brain. 2003;126(pt 6):1319–1332. doi: 10.1093/brain/awg132. [DOI] [PubMed] [Google Scholar]
- 12.Jenkins IH, Bain PG, Colebatch JG, et al. A positron emission tomography study of essential tremor: evidence for overactivity of cerebellar connections. Ann Neurol. 1993;34(1):82–90. doi: 10.1002/ana.410340115. [DOI] [PubMed] [Google Scholar]
- 13.Bucher SF, Seelos KC, Dodel RC, Reiser M, Oertel WH. Activation mapping in essential tremor with functional magnetic resonance imaging. Ann Neurol. 1997;41(1):32–40. doi: 10.1002/ana.410410108. [DOI] [PubMed] [Google Scholar]
- 14.Louis ED, Vonsattel JPG, Honig LS, Ross GW, Lyons KE, Pahwa R. Neuropathologic findings in essential tremor. Neurology. 2006;66(11):1756–1759. doi: 10.1212/01.wnl.0000218162.80315.b9. [DOI] [PubMed] [Google Scholar]
- 15.Louis ED, Vonsattel JPG, Honig LS, et al. Essential tremor associated with pathological changes in the cerebellum. Arch Neurol. 2006;63(8):1189–1193. doi: 10.1001/archneur.63.8.1189. [DOI] [PubMed] [Google Scholar]
- 16.Braak H, Braak E. Diagnostic criteria for neuropathologic assessment of Alzheimer's disease. Neurobiol Aging. 1997;18(4suppl):S85–S88. doi: 10.1016/s0197-4580(97)00062-6. [DOI] [PubMed] [Google Scholar]
- 17.Mirra SS. The CERAD neuropathology protocol and consensus recommendations for the postmortem diagnosis of Alzheimer's disease: a commentary. Neurobiol Aging. 1997;18(4suppl):S91–S94. doi: 10.1016/s0197-4580(97)00058-4. [DOI] [PubMed] [Google Scholar]
- 18.Deuschl G, Bain P, Brin M. Consensus statement of the Movement Disorder Society on Tremor: Ad Hoc Scientific Committee. Mov Disord. 1998;13(suppl 3):2–23. doi: 10.1002/mds.870131303. [DOI] [PubMed] [Google Scholar]
- 19.Louis ED, Borden S, Moskowitz CB. Essential tremor centralized brain repository: diagnostic validity and clinical characteristics of a highly selected group of essential tremor cases. Mov Disord. 2005;20(10):1361–1365. doi: 10.1002/mds.20583. [DOI] [PubMed] [Google Scholar]
- 20.Fahn S, Elton RL, UPDRS Development Committee . Unified Parkinson's Disease Rating Scale. In: Fahn S, Marsden CD, Goldstein M, Calne CD, editors. Recent Developments in Parkinson's Disease. Vol 2. Macmillan; Florham Park, NJ: 1987. pp. 153–163. [Google Scholar]
- 21.Trouillas P, Takayanagi T, Hallett M, et al. International Cooperative Ataxia Rating Scale for pharmacological assessment of the cerebellar syndrome: The Ataxia Neuropharmacology Committee of the World Federation of Neurology. J Neurol Sci. 1997;145(2):205–211. doi: 10.1016/s0022-510x(96)00231-6. [DOI] [PubMed] [Google Scholar]
- 22.Harasymiw JW, Bean P. Identification of heavy drinkers by using the early detection of alcohol consumption score. Alcohol Clin Exp Res. 2001;25(2):228–235. [PubMed] [Google Scholar]
- 23.Louis ED, Shungu D, Chan S, Mao X, Jurewicz EC, Watner D. Metabolic abnormality in patients with essential tremor: a proton magnetic resonance spectroscopic imagining study. Neurosci Lett. 2002;333(1):17–20. doi: 10.1016/s0304-3940(02)00966-7. [DOI] [PubMed] [Google Scholar]
- 24.Bebin EM, Bebin J, Currier RD, Smith EE, Perry TL. Morphometric studies in dominant olivopontocerebellar atrophy: comparison of cell losses with amino acid decreases. Arch Neurol. 1990;47(2):188–192. doi: 10.1001/archneur.1990.00530020094021. [DOI] [PubMed] [Google Scholar]
- 25.Kume A, Takahashi A, Hashizume Y, Asai J. A histometrical and comparative study on Purkinje cell loss and olivary nucleus cell loss in multiple system atrophy. J Neurol Sci. 1991;101(2):178–186. doi: 10.1016/0022-510x(91)90043-7. [DOI] [PubMed] [Google Scholar]
- 26.Ellis RS. A preliminary quantitative study of Purkinje cells in normal, subnormal and senscent human cerebella with some notes on functional organization. J Comp Neurol. 1919;30:229–252. [Google Scholar]
- 27.Ellis RS. Norms for some structural changes in the human cerebellum from birth to old age. J Comp Neurol. 1920;32:1–33. [Google Scholar]
- 28.Hall TC, Miller AKH, Corsellis JAN. Variations in the human Purkinje cell population according to age and sex. Neuropathol Appl Neurobiol. 1975;1:267–292. [Google Scholar]
- 29.Louis ED. Essential tremor. Lancet Neurol. 2005;4(2):100–110. doi: 10.1016/S1474-4422(05)00991-9. [DOI] [PubMed] [Google Scholar]
- 30.Benito-León J, Louis ED. Essential tremor: emerging views of a common disorder. Nat Clin Pract Neurol. 2006;2(12):666–678. doi: 10.1038/ncpneuro0347. [DOI] [PubMed] [Google Scholar]
- 31.Louis ED, Frucht SJ. Prevalence of essential tremor in patients with Parkinson's disease vs. Parkinson-Plus syndromes. Mov Disord. 2007;22(10):1402–1407. doi: 10.1002/mds.21383. [DOI] [PubMed] [Google Scholar]
- 32.Yahr MD, Orosz D, Purohit DP. Co-occurrence of essential tremor and Parkinson's disease: a clinical study of a large kindred with autopsy findings. Parkinsonism Relat Disord. 2003;9(4):225–231. doi: 10.1016/s1353-8020(02)00057-3. [DOI] [PubMed] [Google Scholar]
- 33.Shahed J, Jankovic J. Exploring the relationship between essential tremor and Parkinson's disease. Parkinsonism Relat Disord. 2007;13(2):67–76. doi: 10.1016/j.parkreldis.2006.05.033. [DOI] [PubMed] [Google Scholar]
- 34.Louis ED, Levy G, Mejia-Santana H, et al. Risk of action tremor in relatives of tremor dominant PD and postural instability gait disorder PD. Neurology. 2003;61(7):931–936. doi: 10.1212/wnl.61.7.931. [DOI] [PubMed] [Google Scholar]
- 35.Ondo WG, Lai D. Olfaction testing in patients with tremor-dominant Parkinson's disease: is this a distinct condition? Mov Disord. 2005;20(4):471–475. doi: 10.1002/mds.20365. [DOI] [PubMed] [Google Scholar]
- 36.Pahwa R, Koller WC. Is there a relationship between Parkinson's disease and essential tremor? Clin Neuropharmacol. 1993;16(1):30–35. doi: 10.1097/00002826-199302000-00003. [DOI] [PubMed] [Google Scholar]
- 37.Geraghty JJ, Jankovic J, Zetusky WJ. Association between essential tremor and Parkinson's disease. Ann Neurol. 1985;17(4):329–333. doi: 10.1002/ana.410170404. [DOI] [PubMed] [Google Scholar]
- 38.Chaudhuri KR, Buxton-Thomas M, Dhawan V, Peng R, Meilak C, Brooks DJ. Long duration asymmetrical postural tremor is likely to predict development of Parkinson's disease and not essential tremor: clinical follow up study of 13 cases. J Neurol Neurosurg Psychiatry. 2005;76(1):115–117. doi: 10.1136/jnnp.2004.046292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Matsumoto R, Nakano I, Arai N, Oda M, Yagashita S, Hashizume Y. Loss of den-tate nucleus neurons is associated with torpedo formation: a morphometric study in progressive supranuclear palsy and dentatorubro-pallidoluysian atrophy. Acta Neuropathol (Berl) 1998;95(2):149–153. doi: 10.1007/s004010050779. [DOI] [PubMed] [Google Scholar]
- 40.Torvik A, Torp S, Lindboe CF. Atrophy of the cerebellar vermis in ageing: a morphometric and histologic study. J Neurol Sci. 1986;76(23):283–296. doi: 10.1016/0022-510x(86)90176-0. [DOI] [PubMed] [Google Scholar]
- 41.Wegiel J, Wisniewski HM, Dziewiatkowski J, et al. Cerebellar atrophy in Alzheimer's disease: clinicopathological correlations. Brain Res. 1999;818(1):41–50. doi: 10.1016/s0006-8993(98)01279-7. [DOI] [PubMed] [Google Scholar]
- 42.Fukutani Y, Cairns NJ, Rosser MN, Lantos PL. Purkinje cell loss and astrocytosis in the cerebellum in familial and sporadic Alzheimer's disease. Neurosci Lett. 1996;214(1):33–36. doi: 10.1016/0304-3940(96)12875-5. [DOI] [PubMed] [Google Scholar]
- 43.Karhunen PJ, Erkinjuntti T, Laippala P. Moderate alcohol consumption and loss of cerebellar Purkinje cells. BMJ. 1994;308(6945):1663–1667. doi: 10.1136/bmj.308.6945.1663. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sjöbeck M, Englund E. Alzheimer's disease and the cerebellum: a morphologic study on neuronal and glial changes. Dement Geriatr Cogn Disord. 2001;12(3):211–218. doi: 10.1159/000051260. [DOI] [PubMed] [Google Scholar]
- 45.Phillips SC, Harper CG, Kril J. A quantitative histological study of the cerebellar vermis in alcoholic patients. Brain. 1987;110:301–314. doi: 10.1093/brain/110.2.301. [DOI] [PubMed] [Google Scholar]
- 46.Lohr JB, Jeste DV. Cerebellar pathology in schizophrenia? a neuronometric study. Biol Psychiatry. 1986;21(10):865–875. doi: 10.1016/0006-3223(86)90259-3. [DOI] [PubMed] [Google Scholar]