Abstract
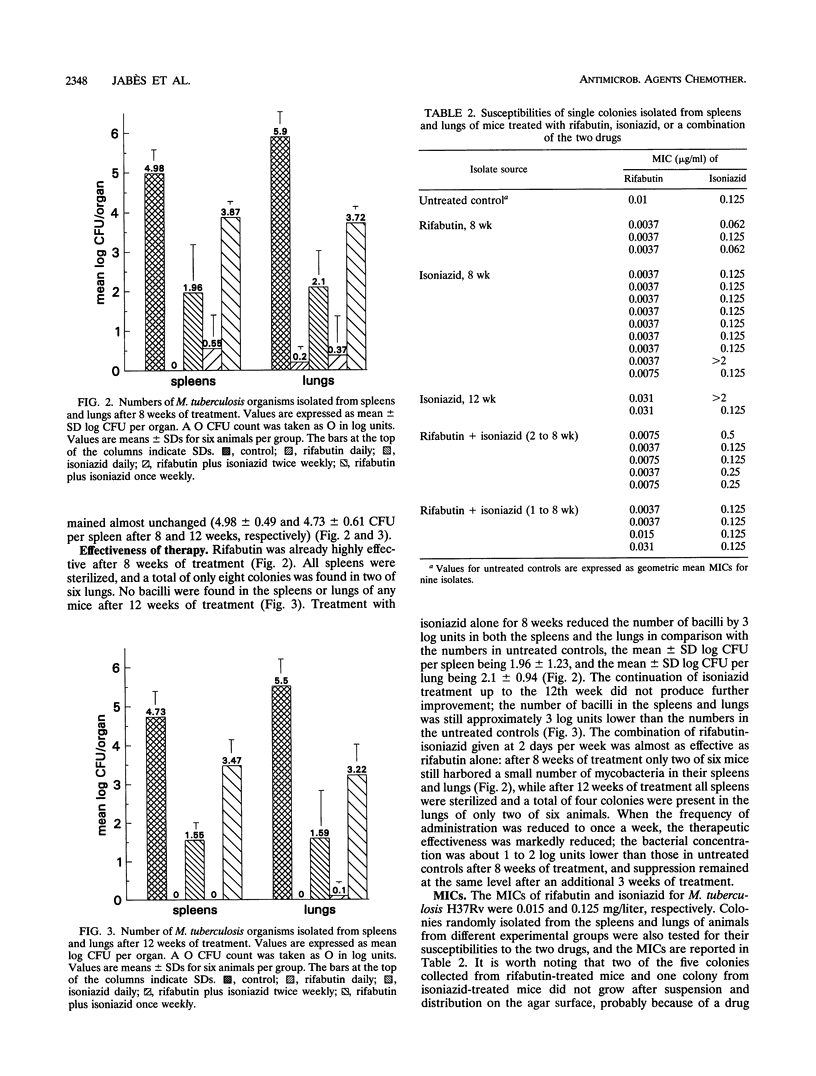
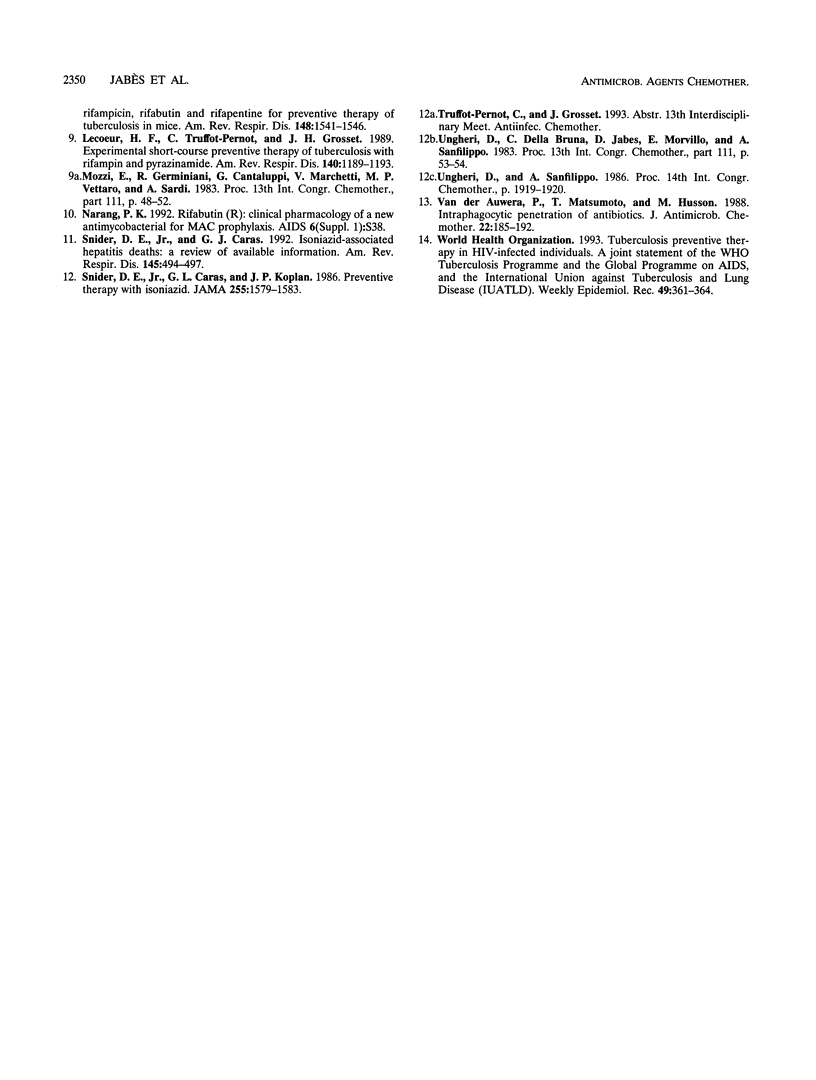
The ever-increasing incidence of tuberculosis calls for the implementation of control measures, including new efficient, short-term preventive therapies to replace 6 to 12 months of isoniazid therapy. The efficacies of 12-week regimens of rifabutin or isoniazid given daily and the combination of the two drugs administered intermittently were evaluated in mice infected with Mycobacterium tuberculosis after vaccination with the bacillus Calmette-Guérin (BCG) to imitate some features of the natural infection in humans with a low number of persisting bacteria. Rifabutin at 10 mg/kg of body weight per day was highly effective as early as the eighth week of treatment: all spleens were sterilized and the number of bacteria was drastically reduced in the lungs (mean +/- standard deviation log CFU, 0.2 +/- 0.3, compared with 5.9 +/- 0.6 for untreated controls). No bacilli were found in the spleens or lungs of any of the animals treated for 12 weeks. The combination of rifabutin at 10 mg/kg plus isoniazid at 25 mg/kg twice weekly was almost as effective as rifabutin daily: after 8 weeks of treatment only two of six mice harbored a small number of mycobacteria in their spleens and lungs; at week 12, all spleens were sterilized and a total of eight colonies were isolated from the lungs of two of six mice. Daily isoniazid and once-weekly rifabutin plus isoniazid therapies were less effective. Colonies randomly isolated from the spleens and lungs of mice from different experimental groups were also tested for their susceptibilities to the two drugs. The three surviving colonies from rifabutin-treated mice and all colonies from those administered rifabutin plus isoniazid remained fully susceptible to either drug. In contrast, 2 (18%) of the 11 colonies randomly selected from isoniazid-treated mice became resistant to isoniazid (MIC, > 2 micrograms/ml), although they were still susceptible to rifabutin. Three months of treatment with rifabutin, either daily alone or twice a week combined with isoniazid, proved to be a valid candidate for tuberculosis preventive therapy.
Full text
PDF


Images in this article
Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Dickinson J. M., Mitchison D. A. In vitro observations on the suitability of new rifamycins for the intermittent chemotherapy of tuberculosis. Tubercle. 1987 Sep;68(3):183–193. doi: 10.1016/0041-3879(87)90054-7. [DOI] [PubMed] [Google Scholar]
- Heifets L. B., Lindholm-Levy P. J., Iseman M. D. Rifabutine: minimal inhibitory and bactericidal concentrations for Mycobacterium tuberculosis. Am Rev Respir Dis. 1988 Mar;137(3):719–721. doi: 10.1164/ajrccm/137.3.719. [DOI] [PubMed] [Google Scholar]
- Iseman M. D. Less is more: short-course preventive therapy of tuberculosis. Am Rev Respir Dis. 1989 Nov;140(5):1187–1187. doi: 10.1164/ajrccm/140.5.1187. [DOI] [PubMed] [Google Scholar]
- Lecoeur H. F., Truffot-Pernot C., Grosset J. H. Experimental short-course preventive therapy of tuberculosis with rifampin and pyrazinamide. Am Rev Respir Dis. 1989 Nov;140(5):1189–1193. doi: 10.1164/ajrccm/140.5.1189. [DOI] [PubMed] [Google Scholar]
- Snider D. E., Jr, Caras G. J. Isoniazid-associated hepatitis deaths: a review of available information. Am Rev Respir Dis. 1992 Feb;145(2 Pt 1):494–497. doi: 10.1164/ajrccm/145.2_Pt_1.494. [DOI] [PubMed] [Google Scholar]
- Snider D. E., Jr, Caras G. J., Koplan J. P. Preventive therapy with isoniazid. Cost-effectiveness of different durations of therapy. JAMA. 1986 Mar 28;255(12):1579–1583. [PubMed] [Google Scholar]
- Van der Auwera P., Matsumoto T., Husson M. Intraphagocytic penetration of antibiotics. J Antimicrob Chemother. 1988 Aug;22(2):185–192. doi: 10.1093/jac/22.2.185. [DOI] [PubMed] [Google Scholar]



