Abstract
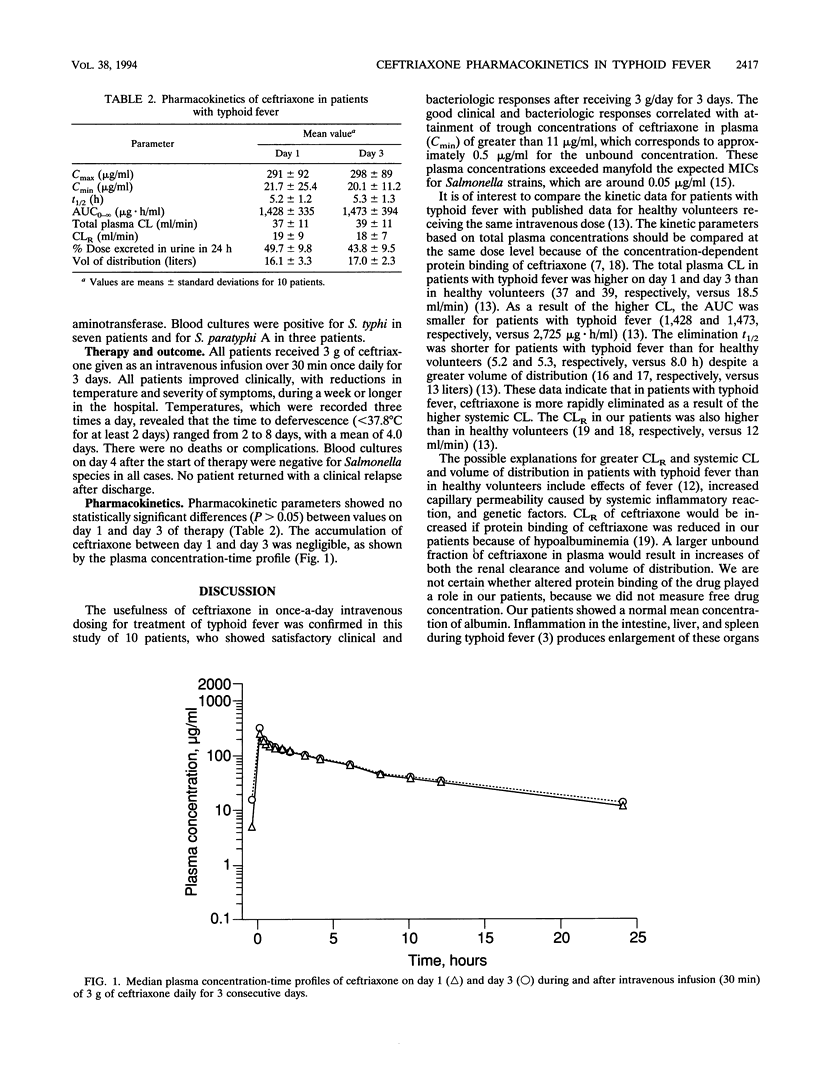
Ceftriaxone in short courses has emerged as an effective alternative to chloramphenicol for the treatment of typhoid fever. To study the pharmacokinetics of ceftriaxone in acute typhoid fever, 10 febrile Nepalese adolescents and young adults with blood culture-positive illness were treated with 3 g of ceftriaxone (intravenous infusion for 30 min) daily for 3 days. On the 1st and 3rd day of treatment, blood and urine samples were collected at defined intervals for measurements of drug concentrations. Kinetic parameters including concentrations at the end of infusion (Cmax) and 24 h after the end of infusion (Cmin), elimination half-life (t1/2), area under the plasma concentration-time curve (AUC), total plasma clearance, renal clearance, percentage excreted in urine, and volume of distribution were estimated. On day 1, mean values were as follows: Cmax, 291 micrograms/ml; Cmin, 21.7 micrograms/ml; plasma t1/2, 5.2 h; AUC, 1,428 micrograms.h/ml; total plasma clearance, 37 ml/min; renal clearance, 19 ml/min; percentage excreted in urine, 49.7%; and volume of distribution, 16.1 liters. Mean values on day 3 were not significantly different from those on day 1. Compared with published values for healthy volunteers who received the same dose, our mean t1/2s and AUCs were lower and our mean total plasma clearances, renal clearances, and volumes of distribution were higher. The good clinical responses of these patients to therapy and the adequate Cmins support the use of ceftriaxone once daily for the treatment of typhoid fever.
Full text
PDF

Selected References
These references are in PubMed. This may not be the complete list of references from this article.
- Anton P. A., Kemp J. A., Butler T., Jacobs M. R. Comparative efficacies of ceftriaxone, moxalactam, and ampicillin in experimental Salmonella typhimurium infection. Antimicrob Agents Chemother. 1982 Aug;22(2):312–315. doi: 10.1128/aac.22.2.312. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arvidsson A., Alván G., Angelin B., Borgå O., Nord C. E. Ceftriaxone: renal and biliary excretion and effect on the colon microflora. J Antimicrob Chemother. 1982 Sep;10(3):207–215. doi: 10.1093/jac/10.3.207. [DOI] [PubMed] [Google Scholar]
- Coovadia Y. M., Gathiram V., Bhamjee A., Garratt R. M., Mlisana K., Pillay N., Madlalose T., Short M. An outbreak of multiresistant Salmonella typhi in South Africa. Q J Med. 1992 Feb;82(298):91–100. [PubMed] [Google Scholar]
- Edelman R., Levine M. M. Summary of an international workshop on typhoid fever. Rev Infect Dis. 1986 May-Jun;8(3):329–349. doi: 10.1093/clinids/8.3.329. [DOI] [PubMed] [Google Scholar]
- Findlay C. D., Brown R. M., Allcock J. E., Lowe P. A., Wise R. A study of the relationship between dose and pharmacokinetics of ceftriaxone. J Antimicrob Chemother. 1982 Jan;9(1):57–62. doi: 10.1093/jac/9.1.57. [DOI] [PubMed] [Google Scholar]
- Islam A., Butler T., Nath S. K., Alam N. H., Stoeckel K., Houser H. B., Smith A. L. Randomized treatment of patients with typhoid fever by using ceftriaxone or chloramphenicol. J Infect Dis. 1988 Oct;158(4):742–747. doi: 10.1093/infdis/158.4.742. [DOI] [PubMed] [Google Scholar]
- Kalager T., Digranes A., Bergan T., Solberg C. O. The pharmacokinetics of ceftriaxone in serum, skin blister and thread fluid. J Antimicrob Chemother. 1984 May;13(5):479–485. doi: 10.1093/jac/13.5.479. [DOI] [PubMed] [Google Scholar]
- Kumana C. R., Lauder I. J., Chan M., Ko W., Lin H. J. Differences in diazepam pharmacokinetics in Chinese and white Caucasians--relation to body lipid stores. Eur J Clin Pharmacol. 1987;32(2):211–215. doi: 10.1007/BF00542199. [DOI] [PubMed] [Google Scholar]
- Lan C. K., Cheng D. L., Lasserre R. Two to three days treatment of typhoid fever with ceftriaxone. Southeast Asian J Trop Med Public Health. 1986 Mar;17(1):119–124. [PubMed] [Google Scholar]
- Lasserre R., Sangalang R. P., Santiago L. Three-day treatment of typhoid fever with two different doses of ceftriaxone, compared to 14-day therapy with chloramphenicol: a randomized trial. J Antimicrob Chemother. 1991 Nov;28(5):765–772. doi: 10.1093/jac/28.5.765. [DOI] [PubMed] [Google Scholar]
- Mackowiak P. A. Influence of fever on pharmacokinetics. Rev Infect Dis. 1989 Sep-Oct;11(5):804–807. [PubMed] [Google Scholar]
- McNamara P. J., Stoeckel K., Ziegler W. H. Pharmacokinetics of ceftriaxone following intravenous administration of a 3 g dose. Eur J Clin Pharmacol. 1982;22(1):71–75. doi: 10.1007/BF00606428. [DOI] [PubMed] [Google Scholar]
- Naqvi S. H., Bhutta Z. A., Farooqui B. J. Therapy of multidrug resistant typhoid in 58 children. Scand J Infect Dis. 1992;24(2):175–179. doi: 10.3109/00365549209052609. [DOI] [PubMed] [Google Scholar]
- Neu H. C., Meropol N. J., Fu K. P. Antibacterial activity of ceftriaxone (Ro 13-9904), a beta-lactamase-stable cephalosporin. Antimicrob Agents Chemother. 1981 Mar;19(3):414–423. doi: 10.1128/aac.19.3.414. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oie S. Drug distribution and binding. J Clin Pharmacol. 1986 Nov-Dec;26(8):583–586. doi: 10.1002/j.1552-4604.1986.tb02953.x. [DOI] [PubMed] [Google Scholar]
- Stoeckel K., McNamara P. J., Brandt R., Plozza-Nottebrock H., Ziegler W. H. Effects of concentration-dependent plasma protein binding on ceftriaxone kinetics. Clin Pharmacol Ther. 1981 May;29(5):650–657. doi: 10.1038/clpt.1981.90. [DOI] [PubMed] [Google Scholar]
- Stoeckel K. Pharmacokinetics of Rocephin, a highly active new cephalosporin with an exceptionally long biological half-life. Chemotherapy. 1981;27 (Suppl 1):42–46. doi: 10.1159/000238028. [DOI] [PubMed] [Google Scholar]
- Ti T. Y., Monteiro E. H., Lam S., Lee H. S. Ceftriaxone therapy in bacteremic typhoid fever. Antimicrob Agents Chemother. 1985 Oct;28(4):540–543. doi: 10.1128/aac.28.4.540. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vesell E. S. Sounding board. Why are toxic reactions to drugs so often undetected initially? N Engl J Med. 1980 May 1;302(18):1027–1029. doi: 10.1056/NEJM198005013021811. [DOI] [PubMed] [Google Scholar]


