Abstract
In order to sustain life, patients whose kidneys fail must receive dialysis or obtain a transplant. This study reports on the development and validation of measures of Stage of Change, Decisional Balance, and Self–efficacy based on the Transtheoretical Model (TTM) to assess patients' readiness to receive a deceased donor transplant. We surveyed 293 transplant-eligible kidney patients about their deceased donation readiness. Exploratory and Confirmatory analyses for all measures demonstrated factor structures similar to previous application of the TTM to other health behaviors, excellent model fit, and good internal and external validity. These brief, reliable instruments with good psychometric properties can guide the development of improved, individually-tailored transplant education for patients.
In the United States, there are over 500,000 patients with end-stage renal disease (ESRD), or kidney failure (United States Renal Data System, 2008). Once an individual's kidney fails, he or she must decide whether to start dialysis or obtain a transplant from either a deceased or living donor. The survival benefits of kidney transplant over dialysis are well established. In one analysis, the long-term mortality risk for transplanted recipients was 68% lower than dialysis patients waiting for kidneys, with a projected increase in life span of 3 to 17 years (Wolfe, et al., 1999). In addition, patients receiving transplants report better quality-of-life compared to dialysis patients (Neipp, et al., 2006), with patients receiving living donor transplants having lower rates of rejection than patients with deceased donor transplants (United Network for Organ Sharing, 2001). Unfortunately, few patients pursue transplantation; In 2006, only 16% of end-stage renal disease (ESRD) patients in the United States were on the transplant waiting list, with only 4% receiving transplants in that year (United States Renal Data System, 2008).
So, why isn't this optimal ESRD treatment chosen by more patients? Although extensive research has been done to understand whether individuals will donate their own organs to the waiting list after they die (Hall, et al., 2007; Robbins, et al., 2001), less is known about the transplant decision-making of those who need kidneys. The decision to pursue transplant is complex; interested patients must complete a medical evaluation, undergo and recover from surgery, and take immunosuppressant drugs for their entire lives. Research has shown that many patients believe that getting a transplant is too risky (Holley, McCauley, Doherty, Stackiewicz, & Johnson, 1996) due to their concerns about immunosuppressant side effects (Orsino, Cameron, Seidl, Mendelssohn, & Stewart, 2003) and undergoing surgery (Kurz, Scharff, Terry, Alexander, & Waterman, 2007; Waterman & Brennan, 2007). Finally, the wait for a deceased donor kidney, now averaging almost 4 years in the United States, can be prohibitive for many patients.
Quality transplant education is needed to ensure that all ESRD patients who want to learn about and pursue transplant can do so. When designing educational interventions, the use of established theoretical frameworks can increase their efficacy and utility. The Transtheoretical Model (TTM) is a model of behavior change shown to be robust in its ability to explain and facilitate change across many health behaviors. Thirty years of research on a variety of health behaviors and populations, including organ and blood donation (Burditt, et al., in press; Hall, et al., 2007; Robbins, et al., 2001), have identified key principles and processes involved with behavioral change. Research has also provided strong support for the reliability and validity of the model's core constructs, including Stage of Change (McConnaughy, Prochaska, & Velicer, 1983); Decisional Balance; (Velicer, DiClemente, Prochaska, & Brandenburg, 1985) and Self-Efficacy. (Velicer, DiClemente, Rossi, & Prochaska, 1990)
Constructs Comprising the Transtheoretical Model of Behavior Change
Stage of Change
Stage of Change is the central organizing construct of the TTM representing the temporal and motivational dimension of change. Unlike sociodemographic variables like race and education level, Stage of Change is modifiable. Longitudinal studies have found that people move through a series of five stages when modifying behavior on their own or with the help of formal intervention (Prochaska & DiClemente, 1983). In the Precontemplation stage, individuals may deny they need to change and be resistant to change; they may be unaware of the negative consequences of their behavior, or have given up the thought of changing because they are demoralized. They are not intending to change their behavior in the foreseeable future. Individuals in Contemplation are more likely to recognize the benefits of changing. However, they continue to overestimate the costs of changing and, therefore, are ambivalent. Individuals in Preparation have decided to change their behavior soon, and have already begun to take small steps toward that goal. People in Action are overtly engaged in modifying their behavior, while individuals in Maintenance have been able to sustain change for some time.
Decisional Balance
Decisional Balance represents an individual's relative weighing of the Pros and Cons of making a health behavior change (Velicer, et al., 1985). As individuals progress from Precontemplation to Action, assessment of the importance of the pros increases by one standard deviation (the strong principle of change) while the importance of the cons decreases by one half of a standard deviation (the weak principle of change). This construct serves as an intermediate indicator of when change will occur and is thought to be especially salient in the earlier Stages of Change (Velicer, et al., 2000).
Situational Self-Efficacy
Situational Self-Efficacy, or the degree to which an individual believes he or she can make or sustain a behavior change in difficult situations, also can influence motivation and persistence (Plotnikoff, Brez, & Hotz, 2000; Wells-Parker, Kenne, Spratke, & Williams, 2000). Although this construct is relevant across all Stage of Change transitions, it has been demonstrated to be particularly important in an individual's movement through the later Stages of Change (e.g., from Preparation to Action). Self-Efficacy is expected to increase as one progresses through the stages (Rossi & Redding, 2001).
Through this study, we examined the applicability of the TTM to a new behavior - Readiness to receive a deceased donor transplant. Specifically, we developed and validated new measures of Stage of Change, Decisional Balance, and Self-Efficacy for ESRD patients. We hypothesized that the patterns of relationships found between these three constructs would replicate what has been found for many other health behaviors (Hall & Rossi, 2008; Prochaska, 1994). Finally, since a deceased donation educational intervention could be created after development of these measures, we examined the relationship between transplant knowledge and these constructs.
Method
Formative Research and Measurement Development Overview
We conducted a series of focus group and quantitative studies to understand patients' transplant fears and what motivated them to begin evaluation (Waterman, Barrett, Stanley, Schenk, & Hong, 2004; Waterman, Covelli, et al., 2004; Waterman, et al., 2006). A panel of psychologists and health professionals with expertise in measure development, the TTM, kidney transplantation and organ donation reviewed the formative research and developed a set of preliminary measures of readiness to receive a deceased donor transplant. Cognitive interviews were completed with 25 kidney recipients and dialysis patients to ensure comprehension and clarity of measure items and survey instructions.
Measures
Stage of Change
We defined readiness to get a deceased donor transplant as a person being willing to accept a kidney from a deceased donor, evaluated, and eligible for transplant. We then asked patients, based on this definition, how ready they were to get a deceased donor transplant. Patients chose the statement most true for them of five options: I am not considering getting a deceased donor transplant in the next six months (Precontemplation), I am considering getting a deceased donor transplant in the next six months (Contemplation), I am preparing to get a deceased donor transplant in the next 30 days (Preparation), I am undergoing transplant evaluation to get a deceased donor transplant (Action), and I am listed and waiting to get a deceased donor transplant (Maintenance). This measure was based on previous staging algorithms developed for other organ donation and health behaviors (Hall, et al., 2007; Plummer, et al., 2001).
Decisional Balance
A 16-item Decisional Balance measure was created to assess the Pros and Cons of receiving a deceased donor transplant. This measure provides information about the relative importance an individual places on specific positive and negative outcomes of transplant (e.g., I would not have to be on dialysis; I could die during transplant surgery). Dialysis patients were asked to rate, “How important is this statement to your decision about transplant?” on a 5-point scale ranging from, “Not important” (1) to “Extremely important” (5).
Situational Self–Efficacy
A 15-item measure was created to assess an individual's degree of confidence in their ability to get a transplant in a variety of difficult situations (e.g., You didn't have transportation to the transplant center; your friends and family were unsupportive of you getting a transplant). Responses were made on a 5-point scale, ranging from “not at all confident”(1) to “completely confident”(5).
Transplant Knowledge
Finally, patients were asked 9 true/false and 9 multiple choice questions to determine patients' level of knowledge regarding basic facts, advantages, and outcomes of kidney transplantation. For example, patients were asked if they knew whether people who get transplants generally live longer than people who stay on dialysis and how many years a kidney transplant from a deceased donor is expected to last.
Recruitment and Participants
From April, 2007 – June, 2008, measure development data were collected from kidney patients undergoing dialysis within the context of a larger randomized-controlled education trial. While undergoing dialysis, 293 patients at 20 dialysis centers in St. Louis, Missouri completed a survey administered orally by a research assistant. Hemodialysis patients were eligible for the study if they were over age 18, had no medical contraindications to transplant (i.e., cancer, heart disease, etc.) as determined by their dialysis center Medical Director, could speak English, and were not blind. Patients received a $10 gift card for completing the survey. IRB approval for the study was obtained at Washington University School of Medicine and Saint Louis University in St. Louis, Missouri.
Patients were predominately male (56%), African-American (73%), and had incomes less than $20,000 a year (54%). Their educational level varied, from having some college or higher education (40%), a high school diploma (39%), or less than a high school education (21%). Patients were, on average, 54 years (SD=12 years), and had spent a median of 36 months on dialysis (IQR:13-72 months).
Analytic Procedure and Results
The overall sample of 293 participants was randomly split into two samples for measurement development purposes (N1=140 and N2=153). To validate these measures, the sequential method for scale development was used (Goldberg & Velicer, 2006; Redding, Maddock, & Rossi, 2006). Specifically, there were three phases of analysis for the Stage of Change, Decisional Balance, and Self-Efficacy measures: 1) exploratory analyses, 2) confirmatory analyses, and 3) external validation.
Analyses for Exploratory Phase
Exploratory Procedure Overview
Exploratory analyses were conducted on the N1 sample. Exploratory factor analysis was conducted using principle components analysis (PCA) with varimax rotation on the item intercorrelation matrices. The number of components retained was determined using the minimum average partial procedure (MAP) (Velicer, 1976) and parallel analysis (Zwick & Velicer, 1986).
The dimensional and psychometric properties of each measure were assessed. The aims of these exploratory analyses were to: (1) determine the number of components present and estimate the correlation between them; (2) provide estimates of the factor loadings, eliminate complex items (component loadings ≥ .40 on both components) and items with poor loadings (< .40 on both components); and (3) estimate internal consistency for each component using Cronbach's alpha. Furthermore, final item selection was determined on the basis of item clarity, simple expression of the idea, lack of redundancy with other selected items, and being representative of the conceptual definitions of the constructs.
Decisional Balance
Sixteen Decisional Balance items were included in the original exploratory factor analysis. PCA with varimax rotation on the 16 × 16 matrix of item intercorrelations was conducted to determine the Decisional Balance factor structure. The pool of 16 items was reduced to a total of 12 items, equally representing the Pros and Cons of having a kidney transplant.
MAP and parallel analysis indicated that a two–component solution best described the data, with one factor clearly reflecting the pros of receiving a deceased donor transplant, and the other, the cons. The two factors had average item loadings of 0.6 to 0.8, as well as satisfactory number of items (6) per factor (Velicer, 1976). Scale scores were derived from the sum of the individual item scores. These scales were shown to be internally consistent with coefficient alphas of (α =.75) for Pros and (α =.76) for Cons and to be independent from each other (r=.07). This final two–component solution showed good stability and accounted for 45.93% of the total item variance.
Situational Self–Efficacy
Fifteen self–efficacy items were included in the exploratory factor analysis. PCA with varimax rotation on the 15 × 15 matrix of item intercorrelations was conducted to determine the factor structure of the Self–Efficacy inventory and reduce the pool of 15 items to 8 items. MAP and parallel analysis indicated that a one–component solution best described the data. This final one–component solution showed good stability and internal consistency (α =.86) and accounted for 50.64% of the total item variance.
Analyses for Confirmatory Phase
Confirmatory Procedure Overview
Confirmatory factor analyses, using the N2 sample of 153 participants, were conducted on the Decisional Balance and Self–Efficacy measures using structural equation modeling in EQS (Bentler & Wu, 1993). Multiple models were tested and compared to determine the best fitting model using Maximum Likelihood (ML) as the estimator of fit. Four different fit indices were examined for each of the alternative models. These included: (1) the likelihood ratio chi–square test statistic; (2) the goodness of fit index (GFI); (3) the comparative fit index (CFI); and (4) the average absolute standardized residual statistic (AASR). Traditionally, values of GFI and CFI above .80 indicate good fit, while values above .90 indicate excellent fit (Tabachnick & Fidell, 2001). For AASR, values below .06 indicate excellent fit (Tabachnick & Fidell, 2001). All four fit indices were compared across models.
Decisional Balance
Alternative models were tested for Decisional Balance to determine which model provided the best fit for the data. Four models were tested: 1) null model (suggesting no latent factors and used as a comparative model), 2) one factor, 3) two uncorrelated Pros and Cons factors, and 4) two correlated Pros and Cons factors.
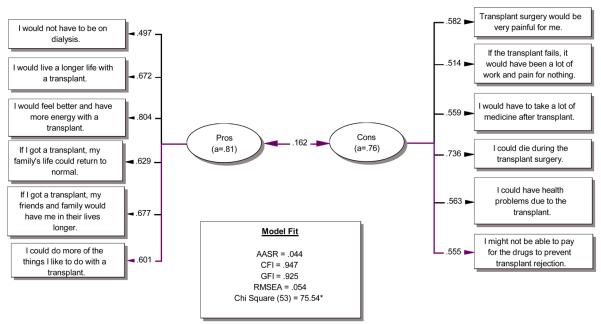
The two–factor correlated model demonstrated the best fit, χ2(76)=75.54, CFI=.95, GFI=.93 and AASR=.04. The reliability of the model was good, with coefficient alphas of .81 for Pros and .76 for Cons. The correlation between the Pros and Cons was .16. Figure 1 shows the set of final items and their factor loadings.
Figure 1.
Decisional Balance Model.
Situational Self–Efficacy
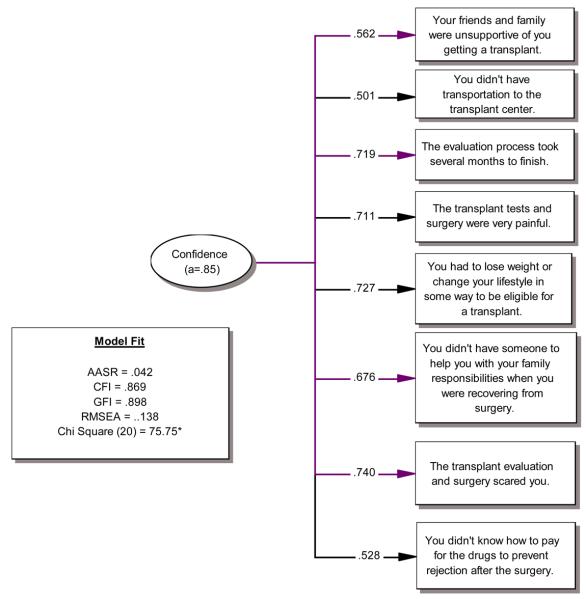
Due to the one–factor solution found for Self–Efficacy in the exploratory phase, only two models were tested: the null model (suggesting no latent factors and used as a comparative model) and a one–factor correlated model. The one-factor correlated model demonstrated the best fit. Results produced strong factor loadings and excellent model fit, χ2(20)=75.75, CFI=.87, GFI = .90 and AASR=.04). The internal consistency of the Self-Efficacy scale was .85. Each of the final items and their factor loadings are shown in Figure 2. In addition, the Self-Efficacy scale was correlated with Pros (r=.23, p < .01) and Cons (r=−.28, p < .01).
Figure 2.
Self-Efficacy Model.
Analyses for External Validation Phase
The external validity of the three measures was assessed by examining their relationships with each other. The magnitude and direction of these relationships were then compared to the relationships between these constructs found in other applications of the Transtheoretical Model (Hall & Rossi, 2008).
Stage of Change
The 293 transplant-eligible patients were classified by readiness to receive a deceased donor transplant. Sixty-six patients (22.5%) indicated that they were not going to call the transplant center to be placed on the waiting list in the next 6 months, classifying them into the Precontemplation Stage. Others indicated that they were planning to call the transplant center to be placed on the waiting list in the next 6 months (Contemplation Stage: 18.1%) or 30 days (Preparation Stage: 29.4%). Finally, the remaining patients were either being evaluated to be placed on the waiting list (Action Stage: 12.6%) or were on the waiting list already (Maintenance Stage: 17.4%).
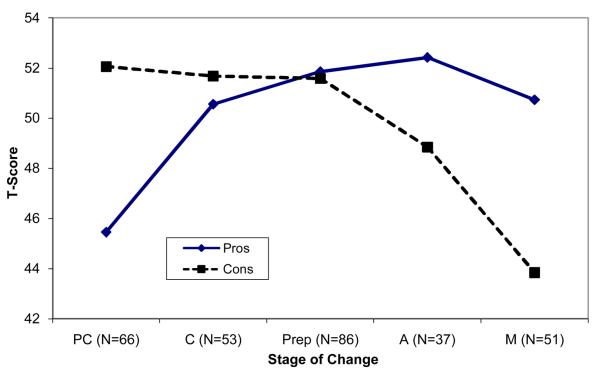
Decisional Balance by Stage
Multivariate Analysis of Variance (MANOVA) revealed that individuals in different stages of readiness to receive a deceased donor transplant differed significantly on their Decisional Balance Pros and Cons (F (8,556)=6.31, p<.001, η2 = .08). As would be predicted by the TTM, post–hoc analyses revealed that the Cons were lowest in Maintenance (p<.01) while the Pros were lowest in Precontemplation (p<.01). Mean T-score values for the Pros and Cons by Stage of Change are shown in Figure 3.
Figure 3.
Pros and Cons by Stage of Change.
The prediction that a crossover between Pros and Cons would occur between Contemplation and Preparation was confirmed. In addition, the magnitude of change in the Pros and Cons by stage, a .72 standard deviation increase in the Pros and a .33 decrease in the Cons, was shown to be comparable to previous meta-analytic findings.
Self–Efficacy by Stage
Analysis of Variance (ANOVA) of the Self–Efficacy scale revealed a significant difference between Stage, F (4, 275) = 5.12, p<. 01, η2 = .07. Post–hoc Tukey tests showed that individuals in the Action and Maintenance Stages reported significantly higher confidence than those in Precontemplation (p <.01).
Transplant Knowledge's Relationship to all Constructs
On average, patients answered 8.04 questions (SD=2.7, 45%) correctly out of 18 questions possible. Analysis of Variance (ANOVA) tests revealed significant difference in transplant knowledge between Stages, F (4, 288)=6.82, p < .001, η2=.09. Post–hoc Tukey tests showed that individuals in Precontemplation, Contemplation and Preparation had significantly less transplant knowledge than patients in Maintenance (p<.01). Transplant knowledge was not significantly correlated with Pros (r = .10) or Self-Efficacy (r=.095), but was negatively correlated with Cons (r = −.285, p < .001).
Discussion
By 2015, US estimates suggest that there will be over 100,000 new ESRD patients yearly (Gilbertson, et al., 2005). Healthcare professionals educating these patients must assess how ready each patient is to pursue deceased donor transplant and then provide education tailored to meet the patient's needs. While, the TTM has previously been applied as a theoretical framework to other organ donation behaviors (Hall, et al., 2007; Robbins, et al., 2001), this is the first study to confirm that the Stage of Change, Decisional Balance, and Self–Efficacy constructs of the TTM are an excellent fit for assessing the decision-making of kidney patients considering whether to obtain deceased donor transplants. In addition, the relationships found between these constructs are consistent with previous TTM research findings across more than 40 health behaviors (Hall & Rossi, 2008).
In this study, over 40% of dialysis patients were not considering or not yet ready to pursue deceased donor transplant. To meet the largest number of patients where they are in their decision-making process, the TTM recommends tailoring education by Stage. Stage-tailored strategies emphasize the benefits of transplant, increase self-efficacy to manage the challenges of the transplant evaluation process, and reduce the importance of the cons of transplant. The newly developed Stage of Change measure provides simple action criteria guiding how education should be delivered for individuals in different Stages. For example, tailored discussion with a patient in Contemplation should emphasize transplant's advantages, such as freedom from the dietary restrictions of dialysis or ability to return to work, while patients in Preparation might discuss what transplant surgery would entail and at which transplant center to begin evaluation.
The Decisional Balance construct, where patients assess the importance of transplant Pros like living longer and Cons like the risk of death undergoing surgery applies well to this health behavior. With this study also revealing a significant negative association between transplant knowledge and level of cons, it may be that providing patients with factual knowledge about the actual risk of surgical complications or costs of immunosuppressive medications may help alleviate fears. As predicted, as readiness to pursue transplant increases, the importance of transplant's Pros increases and Cons decreases.
Getting a transplant is not easy. Patients are asked to lose weight, complete a series of tests over many months, cope with an anxiety-provoking surgery, and be limited in their ability to work or manage their family responsibilities for up to a month as they recover. Some patients, particularly those of low socioeconomic status, face transplant challenges such as inadequate transportation, support from their family and friends, or ability to pay for medical expenses. The Self-Efficacy measure reveals that confidence to manage these issues increases quickly as patients move into Contemplation for deceased donor transplant. However, since undergoing transplant evaluation is so complex, increases in Self-Efficacy after the Contemplation stage were then delayed until after patients moved into Maintenance and were actually listed on the waiting list.
The results of this study are limited by the cross-sectional nature of the sample representing the different Stages of Change. Although previous longitudinal studies of Decisional Balance and the Stage of Change for smoking cessation have supported cross-sectional results (Prochaska, et al., 1994), longitudinal research is still required to more completely address this issue. It also should be noted that the application of the measures may be somewhat limited by geographic, age, and educational characteristics of the sample. Particularly, additional research on deceased donor decision-making with samples of ESRD patients who are Asian, Hispanic, and of higher socioeconomic status should still be conducted.
In addition, due to the scarcity of deceased donor organs, ESRD patients also must decide whether to accept expanded criteria donors who are older or less healthy, or seek living donor kidneys from family members, friends or altruistic donors. Since these kidneys vary in their quality (Schnitzler, et al., 2003; United Network for Organ Sharing, 2001), patients could have different levels of readiness to pursue these deceased and living donor transplant options. With the complexity of family relationships, the varied availability of eligible living donors, and high levels of patient discomfort asking others to be living donors (Waterman, Deych, Hyland, Paiva, & Robbins, 2009), additional research is still needed to evaluate the utility of the TTM for living donation decision-making.
Some educational programs have been shown to increase the rates of transplantation. (Bass, Galley-Reilley, Twiss, & Whitaker, 1999; Rodrigue, Cornell, Lin, Kaplan, & Howard, 2007; Schweitzer, et al., 1997). However, available transplant education are generally brief and not individually tailored to patients' readiness to pursue deceased donor transplant. Efforts to improve these educational shortcomings are needed, with the measures developed here being an important first step. With inconsistent transplant education occurring nationally, a computerized expert system for tailoring transplant education based on an assessment of patients' Stage of Change, Decisional Balance profile and level of Self-Efficacy (Velicer, et al., 1993; Velicer, Prochaska, Fava, Laforge, & Rossi, 1999) could now be created. Thus, if educated early in their disease progression, kidney patients would have time to ask questions, learn about all their options, develop positive transplant attitudes, and if ready, pursue deceased donation.
ACKNOWLEDGEMENTS
This research was supported by the National Institute of Diabetes, Digestive Disorders, and Kidney Disease (K01DK066239) and the Health Resources and Services Administration, Division of Organ Transplantation (R390T05429).
References
- Bass M, Galley-Reilley J, Twiss DE, Whitaker D. A diversified patient education program for transplant recipients. ANNA Journal. 1999;26(3):287–292. 343. [PubMed] [Google Scholar]
- Bentler PM, Wu EJC. EQS/Windows user's guide. 4. ed. BMDP Statistical Software; Los Angeles: 1993. [Google Scholar]
- Burditt C, Robbins M, Paiva A, Velicer W, Koblin B, Kessler D. Motivation for blood donation among African-Americans: Developing measures for stage of change, decisional and efficacy constructs. Journal of Behavioral Medicine. doi: 10.1007/s10865-009-9214-7. in press. [DOI] [PubMed] [Google Scholar]
- Gilbertson DT, Liu J, Xue JL, Louis TA, Solid CA, Ebben JP, et al. Projecting the number of patients with end-stage renal disease in the United States to the year 2015. Journal of the American Society of Nephrology. 2005;16(12):3736–3741. doi: 10.1681/ASN.2005010112. [DOI] [PubMed] [Google Scholar]
- Goldberg L, Velicer W. Principles of exploratory factor analysis. 2nd ed. Springer Pub; New York: 2006. [Google Scholar]
- Hall KL, Robbins ML, Paiva A, Knott JE, Harris L, Mattice B. Donation intentions among African American college students: decisional balance and self-efficacy measures. Journal of Behavioral Medicine. 2007;30(6):483–495. doi: 10.1007/s10865-007-9121-8. [DOI] [PubMed] [Google Scholar]
- Hall KL, Rossi JS. Meta-analytic examination of the strong and weak principles across 48 health behaviors. Preventative Medicine. 2008;46(3):266–274. doi: 10.1016/j.ypmed.2007.11.006. [DOI] [PubMed] [Google Scholar]
- Holley JL, McCauley C, Doherty B, Stackiewicz L, Johnson JP. Patients' views in the choice of renal transplant. Kidney International. 1996;49(2):494–498. doi: 10.1038/ki.1996.70. [DOI] [PubMed] [Google Scholar]
- Kurz RS, Scharff DP, Terry T, Alexander S, Waterman A. Factors influencing organ donation decisions by african americans: a review of the literature. Medical Care Research and Review. 2007;64(5):475–517. doi: 10.1177/1077558707304644. [DOI] [PubMed] [Google Scholar]
- McConnaughy EA, Prochaska JO, Velicer WF. Stages of Change in Psychotherapy - Measurement and Sample Profiles. Psychotherapy-Theory Research and Practice. 1983;20(3):368–375. [Google Scholar]
- Neipp M, Karavul B, Jackobs S, Meyer zu Vilsendorf A, Richter N, Becker T, et al. Quality of life in adult transplant recipients more than 15 years after kidney transplantation. Transplantation. 2006;81(12):1640–1644. doi: 10.1097/01.tp.0000226070.74443.fb. [DOI] [PubMed] [Google Scholar]
- Orsino A, Cameron JI, Seidl M, Mendelssohn D, Stewart DE. Medical decision-making and information needs in end-stage renal disease patients. General Hospital Psychiatry. 2003;25(5):324–331. doi: 10.1016/s0163-8343(03)00069-0. [DOI] [PubMed] [Google Scholar]
- Plotnikoff RC, Brez S, Hotz SB. Exercise behavior in a community sample with diabetes: understanding the determinants of exercise behavioral change. Diabetes Education. 2000;26(3):450–459. doi: 10.1177/014572170002600312. [DOI] [PubMed] [Google Scholar]
- Plummer BA, Velicer WF, Redding CA, Prochaska JO, Rossi JS, Pallonen UE, et al. Stage of change, decisional balance, and temptations for smoking: measurement and validation in a large, school-based population of adolescents. Addictive Behaviors. 2001;26(4):551–571. doi: 10.1016/s0306-4603(00)00144-1. [DOI] [PubMed] [Google Scholar]
- Prochaska JO. Strong and weak principles for progressing from precontemplation to action on the basis of twelve problem behaviors. Health Psychology. 1994;13(1):47–51. doi: 10.1037//0278-6133.13.1.47. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, DiClemente CC. Stages and processes of self-change of smoking: toward an integrative model of change. Journal of Consulting and Clinical Psychology. 1983;51(3):390–395. doi: 10.1037//0022-006x.51.3.390. [DOI] [PubMed] [Google Scholar]
- Prochaska JO, Velicer WF, Rossi JS, Goldstein MG, Marcus BH, Rakowski W, et al. Stages of change and decisional balance for 12 problem behaviors. Health Psychology. 1994;13(1):39–46. doi: 10.1037//0278-6133.13.1.39. [DOI] [PubMed] [Google Scholar]
- Redding CA, Maddock JE, Rossi JS. The sequential approach to measurement of health behavior constructs: issues in selecting and developing measures. Californian Journal of Health Promotion. 2006;4(1):83–101. [Google Scholar]
- Robbins ML, Levesque DA, Redding CA, Johnson JL, Prochaska JO, Rohr MS, et al. Assessing family members' motivational readiness and decision making for consenting to cadaveric organ donation. Journal of Health Psychology. 2001;6(5):523–535. doi: 10.1177/135910530100600506. [DOI] [PubMed] [Google Scholar]
- Rodrigue JR, Cornell DL, Lin JK, Kaplan B, Howard RJ. Increasing live donor kidney transplantation: a randomized controlled trial of a home-based educational intervention. American Journal of Transplant. 2007;7(2):394–401. doi: 10.1111/j.1600-6143.2006.01623.x. [DOI] [PubMed] [Google Scholar]
- Rossi JS, Redding CA. Structure and function of self-efficacy across the stages of change for 10 health behaviors. Annals of Behavioral Medicine. 2001;23S:94. [Google Scholar]
- Schnitzler MA, Whiting JF, Brennan DC, Lin G, Chapman W, Lowell J, et al. The expanded criteria donor dilemma in cadaveric renal transplantation. Transplantation. 2003;75(12):1940–1945. doi: 10.1097/01.TP.0000076381.16276.1B. [DOI] [PubMed] [Google Scholar]
- Schweitzer EJ, Yoon S, Hart J, Anderson L, Barnes R, Evans D, et al. Increased living donor volunteer rates with a formal recipient family education program. Am J Kidney Disease. 1997;29(5):739–745. doi: 10.1016/s0272-6386(97)90128-1. [DOI] [PubMed] [Google Scholar]
- Tabachnick BG, Fidell LS. Using multivariate statistics. 4th ed. Allyn and Bacon; Boston, MA: 2001. [Google Scholar]
- United Network for Organ Sharing Living donation: an overview. 2001 from www.unos.org.
- United States Renal Data System USRDS 2008 annual report: atlas of chronic kidney disease and end-stage renal disease in the United States. 2008 from http://www.usrds.org/2008/pdf/V1_Introduction_2008.pdf.
- Velicer WF. Determining the number of components from the matrix of partial correlations. Psychometrika. 1976;41:321–327. [Google Scholar]
- Velicer WF, DiClemente CC, Prochaska JO, Brandenburg N. Decisional balance measure for assessing and predicting smoking status. Journal of Personality and Social Psychology. 1985;48(5):1279–1289. doi: 10.1037//0022-3514.48.5.1279. [DOI] [PubMed] [Google Scholar]
- Velicer WF, DiClemente CC, Rossi JS, Prochaska JO. Relapse Situations and Self-Efficacy - an Integrative Model. Addictive Behaviors. 1990;15(3):271–283. doi: 10.1016/0306-4603(90)90070-e. [DOI] [PubMed] [Google Scholar]
- Velicer WF, Prochaska JO, Bellis JM, DiClemente CC, Rossi JS, Fava JL, et al. An expert system intervention for smoking cessation. Addictive Behaviors. 1993;18(3):269–290. doi: 10.1016/0306-4603(93)90029-9. [DOI] [PubMed] [Google Scholar]
- Velicer WF, Prochaska JO, Fava JL, Laforge RG, Rossi JS. Interactive versus noninteractive interventions and dose-response relationships for stage-matched smoking cessation programs in a managed care setting. Health Psychology. 1999;18(1):21–28. doi: 10.1037//0278-6133.18.1.21. [DOI] [PubMed] [Google Scholar]
- Velicer WF, Prochaska JO, Fava JL, Rossi JS, Redding CA, Laforge RG, et al. Using the Transtheoretical Model for population-based approaches to health promotion and disease prevention. Homeostasis in Health and Disease. 2000;40:174–195. [Google Scholar]
- Waterman AD, Barrett AC, Stanley SL, Schenk EA, Hong BA. Kidney recipients' use of health education about transplantation; Paper presented at the American Tranpslant Congress.2004. [Google Scholar]
- Waterman AD, Brennan DC. Improving patient education delivery to increase living donation rates. American Journal of Transplant. 2007;7(2):269–270. doi: 10.1111/j.1600-6143.2006.01652.x. [DOI] [PubMed] [Google Scholar]
- Waterman AD, Covelli T, Caisley L, Zerega W, Schnitzler M, Adams D, et al. Potential living kidney donors' health education use and comfort with donation. Progress in Transplant. 2004;14(3):233–240. doi: 10.1177/152692480401400309. [DOI] [PubMed] [Google Scholar]
- Waterman AD, Deych E, Hyland S, Paiva A, Robbins M. Living donation willingness explained: find a volunteer, don't ask; Paper presented at the American Transplant Congress; Boston, MA. May 30-June 3.2009. [Google Scholar]
- Waterman AD, Stanley SL, Covelli T, Hazel E, Hong BA, Brennan DC. Living donation decision making: recipients' concerns and educational needs. Progress in Transplant. 2006;16(1):17–23. doi: 10.1177/152692480601600105. [DOI] [PubMed] [Google Scholar]
- Wells-Parker E, Kenne DR, Spratke KL, Williams MT. Self-efficacy and motivation for controlling drinking and drinking/driving: an investigation of changes across a driving under the influence (DUI) intervention program and of recidivism prediction. Addictive Behaviors. 2000;25(2):229–238. doi: 10.1016/s0306-4603(99)00042-8. [DOI] [PubMed] [Google Scholar]
- Wolfe RA, Ashby VB, Milford EL, Ojo AO, Ettenger RE, Agodoa LY, et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. New England Journal of Medicine. 1999;341(23):1725–1730. doi: 10.1056/NEJM199912023412303. [DOI] [PubMed] [Google Scholar]
- Zwick WR, Velicer WF. Comparison of 5 Rules for Determining the Number of Components to Retain. Psychological Bulletin. 1986;99(3):432–442. [Google Scholar]