Abstract
Objective
To characterize depression treatment-as-usual in a large primary care practice in the U.S. with co-located mental health care, and to examine predictors of receiving any treatment and receiving adequate treatment.
Methods
Primary care patients were systematically approached in waiting rooms. Those with a minimum level of depression symptoms (n = 91) were asked to participate in a study in which they completed assessments of mental health service use, depression symptoms, and related problems.
Results
In this setting with co-located mental health care, most patients with elevated depressive symptoms were receiving some type of mental health care, indicating they had been identified as depressed. However, only half were receiving “minimally adequate care.” Minority patients were less likely to receive any care. Patients who were more depressed, demonstrated poorer problem-solving ability, and had poorer physical health were more likely to receive any treatment and to receive minimally adequate treatment for depression.
Conclusion
Even in the context of co-located mental health care, there is still room for improving treatment of depressed patients. For some depressed patients, an important first step will be to ensure they are receiving minimally adequate care. However, others may need more intensive care, including combined treatments.
Keywords: depression, primary health care
BACKGROUND
Depression is one of the most common conditions in primary care settings. Estimates for the prevalence of major depressive disorder (MDD) in primary care range from 6–14% (Barrett, Barrett, Oxman, & Gerber, 1988; Coyne, Fechner-Bates, & Schwenk, 1994; Simon & VonKorff, 1995). Primary care physicians are the sole providers of care for many depressed patients: recent estimates suggest that 40% of U.S. residents receiving mental health treatment are treated in the general medical health sector alone (Uebelacker, Wang, Berglund, & Kessler, 2006).
Previous research suggests that not all depressed primary care patients are receiving adequate depression treatment. A large study found that, in 1997, between 48% and 60% of patients in managed primary care with current or recent major depression received mental health treatment at an index primary care visit (Wells, Schoenbaum, Unutzer, Lagomasino, & Rubenstein, 1999). Of those receiving treatment, there are varying estimates of rates of adequate treatment. Data from a large epidemiological study (National Comobidity Survey Replication, or NCS-R) suggest that only 15% of patients with major depression who were seen in the general medical sector received “minimally adequate” (i.e., guideline concordant) treatment, compared to 52% of those seen in the mental health specialty sector (Wang et al., 2005). These differences in minimally adequate treatment may be due in part to the frequency of follow-up visits rather than antidepressant dosages. Simon et al (Simon, Von Korff, Rutter, & Peterson, 2001) found psychiatrists are more likely than primary care physicians to provide adequate follow-up care after an antidepressant prescription; however, there were no differences in rates of minimally adequate dosages of antidepressants (rates were approximately 50% in both groups).
Recent trends in primary care research and practice have suggested that co-located OR integrated mental health may improve the care and treatment outcomes of patients with mental health problems (Blount, 2003; Unutzer et al., 2002). Primary care patients may be more likely to follow up on a mental health referral to a co-located provider than an off-site provider (Bartels et al., 2004). Several large healthcare organizations, such as the VA, now have programs to promote and maintain integrated primary care (Butler et al., 2008). Most naturalistic studies of depression treatment in primary care, as cited above, have not examined the patterns of care specifically in practices where co-located care is available. Mauksch and colleagues (Mauksch et al., 2007) did report that rates of mental health visits in general (not specific to depression) increased from before to after a quality improvement program (including integrated mental health care) was initiated at a low-income primary care clinic.
Given this background, in the current study, we examined mental health treatment-as-usual amongst depressed patients in a large primary care practice in the U.S. with co-located mental health specialists. Specifically, we examined: 1) type of treatment that patients received; 2) the characteristics of patients who did (vs. did not) receive mental health treatment; and 3) the characteristics of patients who did (vs. did not) receive minimally adequate mental health treatment. Given the fact of co-located care, we predicted that rates of depression treatment and rates of adequate depression treatment would be higher than those cited in some of the previous literature. However, we believed that predictors of treatment and treatment adequacy would be similar to that found in previous research. We hypothesized that minority status and lower income would be associated with decreased likelihood of receiving treatment and receiving adequate treatment, and having chronic depression, more severe depression, or poorer physical health would be associated with increased likelihood of receiving treatment and receiving adequate treatment. We also examined some predictors not typically examined in large surveys in the past, including problem-solving ability and family functioning. These latter predictors are important because they are potentially modifiable by psychosocial treatments.
METHODS
Participants
Table 1 describes the demographics of the research participants. This sample is consistent with the overall demographic characteristics of the practice. In this practice as a whole, the majority of patients are low income, with 51% of patients covered by Medicaid insurance, 10% by Medicare, 28% by private insurance, and 10% self-pay.
Table 1.
Participant Demographics
| % | N | Mean (SD) | |
|---|---|---|---|
| Gender (Women) | 78% | 68 | |
| Marital status (Married/living together) | 44% | 38 | |
| Race | |||
| American Indian | 5% | 4 | |
| Black | 10% | 9 | |
| White | 72% | 63 | |
| Biracial | 1% | 1 | |
| Don’t know/declines to answer | 12% | 10 | |
| Hispanic | 17% | 15 | |
| Education Levela | |||
| 8th grade or less | 23% | 17 | |
| 12th grade | 38% | 33 | |
| Some college or higher | 38% | 33 | |
| Family Incomea | |||
| $0–25,000 | 54% | 46 | |
| $25,000–$50,000 | 29% | 25 | |
| > $50,000 | 15% | 13 | |
| Don’t know/declines to answer | 2% | 2 | |
| Work Statusa | |||
| Full time or part time work | 34% | 29 | |
| Student | 2% | 2 | |
| Unemployed | 24% | 21 | |
| On Disability | 31% | 27 | |
| Homemaker | 8% | 7 | |
| Age | 34.7 (10.4) | ||
1 respondent with missing data
Procedures
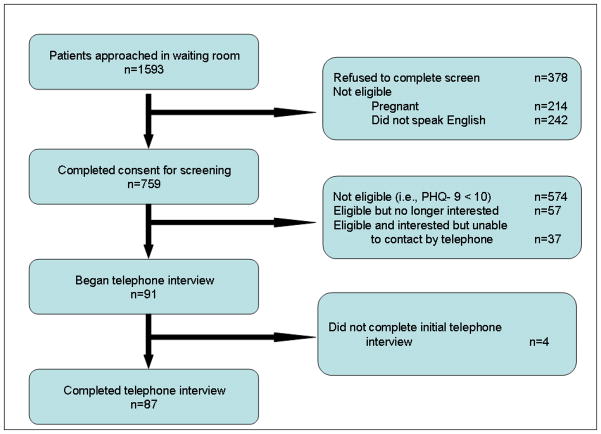
Data were collected from May 2004 – April 2007. Potential participants (n = 1592) were approached in the waiting area and asked if they were interested in a study on “depression, stress, or fatigue.” Research assistants attempted to approach all patients in the waiting area during a given clinic sessions. Please see Figure 1 for a graphic depiction of recruitment process. If a person was interested, he/she completed a brief consent for screening. Following the consent, they completed a PHQ-9. This process took approximately 5 minutes. 185 participants screened positive for depression (i.e., scored ≥ 10). If they scored ≥ 10, they were invited to participate in the next phase of the study, which involved a telephone assessment. Telephone assessments occurred within 4 weeks of the initial screening. During the telephone interview, participants gave their consent to participate in the study and orally completed all assessment measures (except the PHQ-9). This interview lasted approximately 1.5 hours. This study was approved by IRBs at the relevant institutions. Participants were paid $50 for this interview.
Figure 1.
Recruitment flow.
Setting
The setting for this research is a large family medicine training clinic in an urban setting in the U.S. with 39 residents and 14 faculty family physicians, serving 12,500 patients per year with approximately 30,000 visits annually. There is an interdisciplinary behavioral science faculty group consisting of psychiatry, psychology, and social work. These professionals function primarily in a consultation role, and assist physicians with developing treatment strategies. The practice also participates in a co-located mental health counseling program staffed by the local community mental health center. Patients may receive psychotherapy onsite with a mental health professional. Patients may also receive a 1-time consultation with a psychiatrist onsite.
Assessment Instruments
Demographics
Participants were asked to self-report on demographic items, including marital status, age, race, ethnicity (Hispanic or non-Hispanic), education, family income, and work status. For each of these items (except age), participants were asked to choose from a list of possible categories. (Please see Table 1 for a list of categories).
Structured Clinical Interview for DSM-IV-R Axis I Disorders, Clinician Version, (SCID-IV)
Trained raters administered the mood disorder module and the psychotic screen of the SCID-IV (First, Spitzer, Gibbon, & Williams, 2001) in order to assess current and past mood disorder diagnosis.
Patient Health Questionnaire (PHQ-9)
The PHQ-9(Kroenke, Spitzer, & Williams, 2001) was used to screen patients to determine whether they had elevated depressive symptoms and were eligible for the study.
Center for Epidemiologic Studies Depression Scale (CES-D)
The CES-D (Radloff, 1977) is a commonly used scale that assesses level of current depression symptom severity. The CES-D has demonstrated acceptable reliability and validity (Radloff, 1977).
Antidepressant Treatment
Participants were asked a series of questions in order to assess current mental health treatment. Participants were given a comprehensive list of antidepressants and other psychiatric medications, and then asked if they were currently taking any of those medications. If they responded affirmatively, we collected information about the dosing and period of treatment, as well as the type of physician prescribing the medication. Participants were encouraged to look at their pill bottle if needed. For all participants except those who met lifetime criteria for bipolar disorder, antidepressant treatment was considered “minimally adequate” if the current dosage exceeded guidelines for a minimal usual daily dosage(Work Group on Major Depressive Disorder, 2000). For those participants with a lifetime history of bipolar disorder, following American Psychiatric Association guidelines(Work Group on Bipolar Disorder, 2002), treatment was considered minimally adequate only if the participant was taking a mood stabilizer at a dosage that exceeded guidelines for a minimal daily dosage.
Psychotherapeutic Treatment
Participants were given a list of types of professionals (including physicians, psychiatrists, psychologists, social workers, and counselors) and asked if they had ever seen those professionals for “problems with emotions, nerves, or use of alcohol or drugs.” If they said yes, they were asked how many times they had seen that professional for that purpose in the past 3 months. “Minimally adequate” psychotherapeutic treatment was considered to be seeing a mental health professional at least 6 times in the previous 3 months. This decision was based on data from recent trials of psychotherapy for depression within primary care in which effectiveness has been demonstrated with as few as 4–6 therapy sessions (e.g., P. Arean, Hegel, Vannoy, Fan, & Unuzter, 2008).
Alcohol Use Disorders Identification Test (AUDIT)
The AUDIT (Saunders, Aasland, Babor, de la Fuente, & Grant, 1993) was used to identify individuals with harmful drinking behavior. A cut-off of 8 or greater was used to indicate hazardous alcohol use (Babor, Higgins-Biddle, Saunders, & Monteiro, 2001).
Family Assessment Device (FAD)
The FAD (Epstein, Baldwin, & Bishop, 1983) is a 60-item self-report measure of family functioning. For this study, we used only the 12-item general functioning scale (FAD-gf), completed by the patient. Scores are continuous and range from 1–4; higher scores indicate poorer functioning.
MOS 20-item Short-Form Health Survey (SF-20)
The SF-20 (Hays, Sherbourne, & Mazel, 1995) includes items adapted from longer health-related surveys. For the purposes of this research, we used the general health perceptions scale. Scores range from 0 to 100; higher scores indicate better perceived health.
Social Problem-Solving Inventory-Revised (SPSI)
The SPSI (D’ Zurilla, Nezu, & Maydeu-Olivares, in press) is a 52-item self-report questionnaire that assesses several dimensions of problem-solving abilities and yields a total score. Higher scores indicate better problem-solving abilities.
Analyses
In order to characterize demographics, clinical aspects of the sample, and type of treatment received, we calculated simple percentages. In order to examine predictors of receiving treatment and of receiving minimum adequate treatment, we calculated bivariate logistic regression equations, with each equation containing only one predictor – either a categorical predictor (i.e., gender, minority status, income status, presence of chronic depression, and presence of hazardous alcohol use as assessed by the AUDIT) or a continuous predictor (i.e., depression severity as assessed by the CES-D, family functioning as assessed by the FAD-gf, general health perceptions as assessed by the SF-20, and problem solving ability as assessed by the SPSI). This allowed us to calculate odds ratios and their confidence intervals. Finally, in order to determine which predictors accounted for unique variance in the outcome variable, we entered all significant predictors into one of two logistic regression equations predicting either whether treatment was received, or whether minimum adequate treatment was received. We used SPSS 17.0 (“SPSS Statistics Rel. 17.0.0,” 2008) to conduct all analyses.
RESULTS
First, we examined the clinical characteristics of the sample. Of these participants with elevated depressive symptoms, 43 (50% of the total sample) met formal criteria for a current major depressive episode (MDE). Of those who did not meet criteria for a current MDE, most (76%) had a history of major depressive disorder. Twelve patients (14% of the total sample) had a history of bipolar disorder or schizoaffective disorder.
We examined patterns of treatment in this sample. Table 2 presents these data, broken into two groups of participants: 1) entire sample (all with depressive symptoms); and 2) those with a current MDE or with dysthymia. Rates of treatment are similar across both groups. We found that, whereas 83% of those patients with who met full criteria for depression reported receiving some sort of treatment, only 53% reported receiving “minimally adequate” treatment.
Table 2.
Frequencies of Primary Care Participants Receiving Treatment for Depression
| All Participantsa (n = 84) | Participants with a Current MDE or Dysthymia (n = 47) | |||
|---|---|---|---|---|
| % | N | % | N | |
| Any type of treatment for MDD | 80% | 67 | 83% | 39 |
| Counseling with a mental health professional in the past 3 months | 49% | 41 | 55% | 26 |
| Minimum adequate counseling with a mental health professional in past 3 months | 21% | 18 | 23% | 11 |
| Current antidepressant or mood stabilizer treatment | 62% | 52 | 64% | 30 |
| Minimum adequate dose | 44% | 37 | 49% | 23 |
| Minimum adequate treatment (medication or counseling) | 50% | 42 | 53% | 25 |
| Combined treatment (medication and counseling) | 38% | 32 | 43% | 20 |
| Combined minimally adequate treatment | 14% | 12 | 19% | 9 |
Does not include 2 participants with schizoaffective disorder or one with unknown lifetime disorder.
Next, we examined what type of professional prescribed medications in these primary care patients. Of those who were prescribed an antidepressant or mood stabilizer (n = 52), 38 (73%) received the prescription from their primary care physician, 12 (23%) from a psychiatrist, and 2 from another physician. Psychiatrists were more likely than primary care physicians to prescribe a minimum adequate dose (χ2= 5.52, df = 1, p ≤ .025). Sixty-one percent (n= 23) of PCP prescriptions represented a minimum adequate dose, compared to 100% (n = 12) of psychiatrist prescriptions.
Table 3 presents predictors of receiving any mental health treatment. We conducted a series of logistic regression analyses, in which each of the potential predictors were entered into separate bivariate regression equations predicting whether participants received any treatment. As can be seen in table 3, white, non-Latino patients and those with higher levels of depression, poorer general health, and poorer problem solving skills were more likely to receive any treatment. Next, we entered the four significant bivariate predictors into a multivariate logistic regression equation predicting any treatment. Although the overall equation predicted a significant percentage of the variance, (χ2 = 14.64, df = 4, p < .01, R2 = 0.17), none of the four variables predicted significant unique variance in probability of receiving any treatment.
Table 3.
Bivariate Logistic Regression Analyses Predicting Likelihood of Receiving Any Depression Treatment (n = 84).
| B | Wald test (df = 1) | Odds ratio | 95% Confidence interval | ||
|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||
| Gender | 0.77 | 0.91 | 2.16 | 0.44 | 10.54 |
| Minority | 1.31 | 5.15* | 3.71 | 1.20 | 11.49 |
| Low Income | −0.07 | 0.01 | 0.94 | 0.32 | 2.73 |
| Chronic Depression | −0.20 | 0.11 | 1.22 | 0.37 | 4.01 |
| Depression Severity | 0.05 | 5.53* | 1.06 | 1.01 | 1.10 |
| Family Functioning | 0.70 | 2.09 | 2.01 | 0.78 | 5.18 |
| General Health Perceptions | −0.02 | 4.18* | 0.98 | 0.96 | 0.99 |
| Problem Solving Ability | −0.06 | 7.11* | 0.94 | 0.90 | 0.98 |
| Hazardous Alcohol Use | −0.81 | 1.00 | 0.45 | 0.09 | 2.18 |
Note. These analyses represent 9 separate bivariate logistic regression analyses.
p < .05.
Table 4 presents predictors of receiving minimally adequate treatment. Again, we conducted a series of bivariate logistic regression analyses. Patients with more severe depression, poorer general health, and poorer problem solving skills were more likely to receive minimally adequate treatment. Next, we entered the three significant bivariate predictors (CES-D, general health perceptions, and SPSI) into a multivariate logistic regression equation predicting minimally adequate treatment. Although the overall equation predicted a significant percentage of the variance, (χ2 = 8.41 df = 3, p < .05, R2 = 0.10), none of the three variables predicted significant unique variance in probability of receiving minimally adequate treatment.
Table 4.
Bivariate Logistic Regression Analyses Predicting Likelihood of Receiving Adequate Depression Treatment (n = 84).
| B | Wald test (df = 1) | Odds ratio | 95% Confidence interval | ||
|---|---|---|---|---|---|
| Lower bound | Upper bound | ||||
| Gender | 0.45 | 0.66 | 1.56 | 0.53 | 4.59 |
| Minority | 0.69 | 2.00 | 1.98 | 0.77 | 5.13 |
| Low Income | −0.15 | 0.12 | 0.86 | 0.36 | 2.04 |
| Chronic Depression | 0.32 | 0.39 | 1.38 | 0.51 | 3.76 |
| Depression Severity | 0.04 | 4.17* | 1.04 | 1.00 | 1.08 |
| Family Functioning | 0.65 | 3.00 | 1.19 | 0.92 | 4.00 |
| General Health Perceptions | −0.02 | 3.94* | 0.98 | 0.96 | 1.00 |
| Problem Solving Ability | −0.04 | 5.14* | 0.96 | 0.93 | 1.00 |
| Hazardous Alcohol Use | 0.29 | 0.28 | 1.33 | 0.47 | 3.81 |
Note. These analyses represent 9 separate bivariate logistic regression analyses.
p < .05.
DISCUSSION
Previous literature has documented that many depressed primary care patients go unrecognized (Simon & VonKorff, 1995), yet we found fairly high rates of treatment in this sample. This is not an artifact of our recruitment strategy, as all patients were recruited in the waiting room while waiting for an appointment with their physician for any reason. The high rate of treatment indicates that many depressed patients were being recognized as depressed at this clinic. Although we can only speculate, reasons for this may include the availability of co-located specialty mental health care, which may improve access to treatment and raise provider awareness. Other alternatives include the possibility that in general, recognition of depression in primary care is increasing over time, or that recognition of depression is higher in academic medical settings.
Although rates of case finding were better than expected, adequacy of treatment was less optimal. Although most depressed patients were receiving treatment, only 50% were judged to have minimally adequate treatment. This is substantially higher than some previous estimates of adequacy of primary care treatment for depression (Katon, Von Korff, Lin, Bush, & Ormel, 1992; Wang et al., 2005), and similar to another estimate (Mauksch et al., 2007). We note that this latter (higher) estimate was from a clinic which had initiated quality improvement that included integrated mental health care. Our data and this previous data suggest that even in settings with co-located care, a substantial percentage of depressed patients are not receiving minimum adequate treatment; for them a first step is to bring care up to guideline concordant levels.
A group that may be equally as large in size are those patients who are receiving minimally adequate treatment yet still have significant depressive symptoms (in our sample, this was 42 people, or 5.5% of all patients who completed the waiting room screening process (n = 758)). We note that, despite the availability of on-site mental health professionals, very few patients (14%) were receiving combined minimally adequate treatment (i.e, both medication and psychotherapy at minimally adequate levels). Research suggests that combination treatment may improve outcomes, particularly for individuals with chronic depression (Keller et al., 2000). Therefore, there may be a need for more assertive tailoring of individual treatment strategies, even in settings which have co-located care. In particular, medication and problem-solving therapy (P. A. Arean, Hegel, & Reynolds, 2001) may be warranted for those with poor problem-solving skills. Structured behavioral therapies, combined with medication, may be generally appropriate for those who need to cope with physical health problems.
When we examined patient predictors of any treatment and of minimally adequate treatment, we found that that, consistent with previous research (Harman, Edlund, Fortney, & Kallas, 2005; Wang, Berglund, & Kessler, 2000), those less depressed and with better perceived physical health were less likely to receive any treatment or adequate treatment. Our data did not, however, support the hypothesis that those with chronic depression (i.e., of at least 2 years duration) would be more likely to be receiving any treatment or adequate treatment for depression.
Contrary to what we might have expected, patients with poorer problem-solving ability were more likely to receive any treatment or adequate treatment. We believe this reflects the fact that they had higher levels of depression symptoms. Thus, more severely ill patients were receiving more appropriate care. In addition, consistent with documented disparities (Chun-Chung, Jaffe, & Snowden, 2003), minority patients were less likely to receive any mental health care. Reasons for these disparities may range from provider biases or discrimination in term of diagnosis or treatment to differences in patient’s beliefs about treatment to differences in access to care based on health insurance or other factors (McQuire & Miranda, 2008).
Although we measured some patient factors not examined in other studies, there are other patient factors which may influence treatment adequacy, such as patient mental health literacy (defined as ““the knowledge and beliefs about mental disorders which aid their recognition, management or prevention” (Jorm et al., 1997)), or instrumental barriers such as transportation or cost of care. It is important to point out that, although patient factors influence treatment, provider factors and health care organizational factors may also have an impact on treatment. In our study, the specialty of the physician prescribing medication had an impact on quality of care. We found that primary care physicians were less likely to prescribe an adequate dose of medication than psychiatrists; however, this could be due to the fact that the psychiatrists were likely managing the more severely ill patients. In this study, we attempted to control one major organizational factor that influences treatment, i.e., the availability of co-located mental health care. However, there are other organizational factors that must be considered and that do have a positive impact on quality of care, i.e., the use of a patient registry and a specified system for tracking and following up with depressed patients (Unutzer et al., 2002).
There are several limitations to this study that we would like to point out. First, this study does not include patients who were successfully treated for their depression in the past. If their treatment was completely successful, they would not have elevated depressive symptoms at the time of study recruitment and therefore would not be included in the sample. However, the patients identified in this study, as patients with current depressive symptoms, remain a concern for clinicians and researchers alike. Second, the relatively small sample size and the use of one large clinic necessarily place a limit on the generalizability of these results; in addition, power to detect predictors of treatment may have been limited due to the sample size. Third, the measures of treatment adequacy are inexact and do not reflect specific clinical decisions made in each case. Finally, we want to point out that, although we examined statistical predictors of treatment status, this is a cross-sectional and observational study, and therefore we cannot make conclusions about causality.
Despite the limitations of our sample, we believe these data have implications for many primary care practices. First, although co-located care may improve case-finding (and may, indeed, improve adequacy of treatment), there are still many people who continue to have elevated depressive symptoms (fully 11% of those who completed our waiting room screening process). Second, there are two related issues that need to be addressed: ensuring that all depressed patients receive minimally adequate treatment as a first step, and then ensuring that they receive more assertive treatment (e.g., combined psychotherapy and medication) as needed. Third, there continues to be a need to reduce racial and ethnic disparities in likelihood of being treated for depression. Integrative care management programs that include the use of a depression care managers, screening, tracking, and facilitated access to therapy (in addition to co-located mental health professionals) (e.g., Unutzer et al., 2002), may be useful in solving some of these problems.
Footnotes
Publisher's Disclaimer: The following manuscript is the final accepted manuscript. It has not been subjected to the final copyediting, fact-checking, and proofreading required for formal publication. It is not the definitive, publisher-authenticated version. The American Psychological Association and its Council of Editors disclaim any responsibility or liabilities for errors or omissions of this manuscript version, any version derived from this manuscript by NIH, or other third parties. The published version is available at www.apa.org/pubs/journals/fsh.
Contributor Information
Lisa A. Uebelacker, Warren Alpert Medical School of Brown University and Butler Hospital
Marcia Smith, Warren Alpert Medical School of Brown University and Memorial Hospital of Rhode Island.
Angelique W. Lewis, Warren Alpert Medical School of Brown University and Butler Hospital
Ryan Sasaki, Butler Hospital.
Ivan W. Miller, Warren Alpert Medical School of Brown University and Butler Hospital
References
- Arean P, Hegel M, Vannoy S, Fan MY, Unuzter J. Effectiveness of problem-solving therapy for older, primary care patients with depression: results from the IMPACT project. Gerontologist. 2008;48(3):311–323. doi: 10.1093/geront/48.3.311. [DOI] [PubMed] [Google Scholar]
- Arean PA, Hegel MT, Reynolds CF. Treating depression in older medical patients with psychotherapy. J Clin Geropsych. 2001;7:93–104. [Google Scholar]
- Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test. Guidelines for use in primary care. 2. World Health Organization; 2001. [Google Scholar]
- Barrett JE, Barrett JA, Oxman TE, Gerber PD. The prevalence of psychiatric disorders in a primary care practice. Arch Gen Psychiatry. 1988;45:583–587. doi: 10.1001/archpsyc.1988.01800360048007. [DOI] [PubMed] [Google Scholar]
- Bartels SJ, Coakley EH, Zubritsky C, Ware JH, Miles KM, Arean PA, et al. Improving access to geriatric mental health services: a randomized trial comparing treatment engagement with integrated versus enhanced referral care for depression, anxiety, and at-risk alcohol use. Am J Psychiatry. 2004;161(8):1455–1462. doi: 10.1176/appi.ajp.161.8.1455. [DOI] [PubMed] [Google Scholar]
- Blount A. Integrated primary care: organizing the evidence. Family Systems and Health. 2003;21:121–133. [Google Scholar]
- Butler M, Kane RL, McAlpine D, Kathol RG, Fu SS, Hagedorn H, et al. Integration of Mental Health/Substance Abuse and Primary Care No. 173 (Prepared by the Minnesota Evidence-based Practice Center under Contract No. 290–02–0009. AHRQ Publication No. 09-E003. Rockville, MD: Agency for Healthcare REsearch and Quality; 2008. [Google Scholar]
- Chun-Chung J, Jaffe K, Snowden L. Racial/ethnic disparities in the use of mental health services in poverty areas. Am J Public Health. 2003;93:792–797. doi: 10.2105/ajph.93.5.792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Coyne JC, Fechner-Bates S, Schwenk TL. Prevalence, nature, and comorbidity of depressive disorders in primary care. Gen Hosp Psychiatry. 1994;16:267–276. doi: 10.1016/0163-8343(94)90006-x. [DOI] [PubMed] [Google Scholar]
- D’ Zurilla TJ, Nezu AM, Maydeu-Olivares S. Manual for the Social Problem-Solving Inventory-Revised. North Tonawanda, NY: Multi-Health Systems; in press. [Google Scholar]
- Epstein NB, Baldwin LM, Bishop DS. The McMaster Family Assessment Device. J Marital Fam Ther. 1983;9:171–180. [Google Scholar]
- First MB, Spitzer RL, Gibbon M, Williams JBW. Structured clinical interview for DSM-IV-TR Axis I disorders, Research version, Patient edition with Psychotic Screen (SCID-I/P W/PSY SCREEN) New York: Biometrics Research, New York State Psychiatric Institute; 2001. [Google Scholar]
- Harman JS, Edlund MJ, Fortney JC, Kallas H. The influence of comorbid chronic medical conditions on the adequacy of depression care for older Americans. J Am Geriatr Soc. 2005;53:2178–2183. doi: 10.1111/j.1532-5415.2005.00511.x. [DOI] [PubMed] [Google Scholar]
- Hays RD, Sherbourne CD, Mazel RM. User’s manual for Medical Outcomes Study (MOS) core measures of health-related quality of life. RAND Corporation, MR-162-RC; 1995. [Google Scholar]
- Jorm AF, Korten AE, Jacomb PA, Christensen A, Rodgers B, Pollitt P. “Mental health literacy”: a survey of the public’s ability to recognise mental disorders and their beliefs about the effectiveness of treatment. Medical Journal of Australia. 1997;166:182–186. doi: 10.5694/j.1326-5377.1997.tb140071.x. [DOI] [PubMed] [Google Scholar]
- Katon W, Von Korff M, Lin E, Bush T, Ormel J. Adequacy and duration of antidepressant treatment in primary care. Med Care. 1992;30:67. doi: 10.1097/00005650-199201000-00007. [DOI] [PubMed] [Google Scholar]
- Keller MB, McCullough JP, Klein DN, Arnow B, Dunner DL, Gelenberg AJ, et al. A comparison of nefazodone, the cognitive behavioral-analysis system of psychotherapy, and their combination for the treatment of chronic depression. N Engl J Med. 2000;342(20):1462–1470. doi: 10.1056/NEJM200005183422001. [DOI] [PubMed] [Google Scholar]
- Kroenke K, Spitzer RL, Williams JBW. The PHQ-9: Validity of a brief depression severity measure. J Gen Intern Med. 2001;16:606–613. doi: 10.1046/j.1525-1497.2001.016009606.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mauksch LB, Reitz R, Tucker S, Hurd S, Russo J, Katon WJ. Improving quality of care for mental illness in an uninusred, low-income primary care population. General Hospital Psychiatry. 2007;29:302–309. doi: 10.1016/j.genhosppsych.2007.04.002. [DOI] [PubMed] [Google Scholar]
- McQuire TG, Miranda J. New evidence regarding racial and ethnic disparities in mental health: Policy implications. Health Affairs. 2008;27:393–403. doi: 10.1377/hlthaff.27.2.393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Radloff LS. The CES-D scale: a self-report depression scale for research in the general population. Applied Psychological Measurement. 1977;1:385–401. [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the Alcohol use Disorders Identification Test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption II. Addiction. 1993;88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Simon GE, Von Korff M, Rutter CM, Peterson DA. Treatment process and outcomes for managed care patients receiving new antidepressant prescriptions from psychiatrists and primary care physicians. Arch Gen Psychiatry. 2001;58(4):395–401. doi: 10.1001/archpsyc.58.4.395. [DOI] [PubMed] [Google Scholar]
- Simon GE, VonKorff M. Recognition, management, and outcomes of depression in primary care. Arch Fam Med. 1995;4(2):99–105. doi: 10.1001/archfami.4.2.99. [DOI] [PubMed] [Google Scholar]
- SPSS Statistics Rel. 17.0.0. Chicago: SPSS Inc; 2008. [Google Scholar]
- Uebelacker LA, Wang PS, Berglund P, Kessler RC. Clinical differences among patients treated for mental health problems in general medical and specialty mental health settings in the National Comorbidity Survey Replication. Gen Hosp Psychiatry. 2006;28(5):387–395. doi: 10.1016/j.genhosppsych.2006.05.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Unutzer J, Katon W, Callahan CM, Williams JW, Hunkeler EM, Harpole L, et al. Collaborative care management of late-life depression in the primary care setting: a randomized controlled trial. JAMA. 2002;288:2836–2845. doi: 10.1001/jama.288.22.2836. [DOI] [PubMed] [Google Scholar]
- Wang PS, Berglund P, Kessler RC. Recent care of common mental disorders in the United States. J Gen Intern Med. 2000;15:284–292. doi: 10.1046/j.1525-1497.2000.9908044.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang PS, Lang M, Olfson M, Pincus HA, Wells KB, Kessler RC. Twelve-month use of mental health services in the U.S.: Results from the National Comorbidity Survey Replication (NCS-R) Arch Gen Psychiatry. 2005;62:629–640. doi: 10.1001/archpsyc.62.6.629. [DOI] [PubMed] [Google Scholar]
- Wells KB, Schoenbaum M, Unutzer J, Lagomasino IT, Rubenstein LV. Quality of care for primary care patients with depression in managed care. Arch Fam Med. 1999;8:529–536. doi: 10.1001/archfami.8.6.529. [DOI] [PubMed] [Google Scholar]
- Work Group on Bipolar Disorder. Practice guideline for the treatment of patients with bipolar disorder. 2. American Psychiatric Association; 2002. [Google Scholar]
- Work Group on Major Depressive Disorder. Practice Guideline for the Treatment of Patients with Major Depression. 2. American Psychiatric Association; 2000. [Google Scholar]