Abstract
Purpose
To review the recently issued guidelines for weight gain during pregnancy.
Recent findings
These guidelines were developed to minimize the negative health consequences for both mother and fetus of inadequate or excessive gain. They call for categorizing women’s prepregnancy body mass index using the WHO/NHLBI cutoff points and provide ranges of recommended weight gain for underweight (28–40 lb), normal-weight (25–35 lb), overweight (15–25 lb) and obese (11–20 lb) gravidas. Data were insufficient to construct specific guidelines for women with class II or class III obesity. Women should attempt to conceive at a normal weight for better obstetric outcomes. Improved comprehensive preconceptional care is necessary to help women reach this goal. Most American women currently gain below or above the new ranges, so changes are required in both women’s behavior and how their care is managed. Data from a variety of interventions related to improved diet and increased physical activity show that individualized care can assist women in gaining within these guidelines.
Summary
The guidelines offer many opportunities for obstetrician/gynecologists, together with ancillary health care providers, to assume a larger role as “women’s health care physicians” and to conduct research that could improve the health of mothers and children.
Keywords: pregnancy, weight gain, recommendations
Introduction
Since 1990, when the Institute of Medicine (IOM) last issued its guidelines for weight gain during pregnancy (Table 1) [1], much has changed about American women of childbearing age. They are heavier [2]; 8% are now in the body mass index (BMI) category of extreme obesity ≥40 kg/m2). They are also more racially and ethnically diverse. In addition, a higher proportion of women are older or have chronic medical conditions when they become pregnant and a higher proportion are carrying multiple fetuses. Half of the pregnancies among American women remain unwanted or mistimed [3]. In addition, much has been learned about the relationship between gestational weight gain (GWG) and the outcome of pregnancy since the guidelines were last issued, so the time was right for a reexamination of the 1990 IOM guidelines.
Table 1.
1990 IOM guidelines for weight gain and rate of weight gain during pregnancy for women with singleton fetusesa
| Prepregnancy weight-for-height category | Mothers of singletons |
|
|---|---|---|
| Total weight gain (lb) | Rate of weight gain in the second and third trimesters (lb/wk) | |
| Low (BMIa < 19.8 kg/m2) | 28–40 | ~ 1.0 (0.5 kg/wk) |
| Normal (19.8–26.0 kg/m2) | 25–35 | 1.0 (0.4 kg/wk) |
| High (>26.0–29.0 kg/m2) | 15–25 | 0.66 (0.3 kg/wk) |
| Obese (≥ 29.0 kg/m2) | ≥ 15 | Not specified |
Source: Reference [1]; women with twin fetuses were advised to gain 35–45 lb regardless of their prepregnancy BMI
Abbreviation used: BMI, body mass index
Use of the 1990 IOM guidelines for weight gain during pregnancy
In the period since both the 1990 IOM guidelines for weight gain during pregnancy [1] as well as a companion implementation guide [4] were issued, physicians have had experience with using them to help their patients moderate their weight gain. Although a majority of obstetrician/gynecologists report counseling their patients about weight control, diet and physical activity [5], this may not be what women are hearing. For example, both Cogswell et al. [6] and Stotland et al. [7] found that a high proportion of women reported that they were either not given advice on how much weight to gain during pregnancy or were advised to gain outside of the guidelines for their prepregnancy BMI category. Moreover, these guidelines, which call for women to gain at least 15 lb during pregnancy, may be in conflict with women’s own weight-control intentions. Fully one-third of pregnant women in a national sample reported that they were trying to maintain their prepregnancy weight or lose weight during pregnancy [8*]. These observations are in accord with women’s behavior as data from the 2002–03 Pregnancy Risk Assessment Monitoring System show that 50–73% of women gain either below or above the guidelines for their prepregnancy BMI category [9**].
The1990 IOM guidelines for weight gain during pregnancy [1] were developed before there were agreed-upon cutoff points for categorization of body mass index (BMI) among adults. However, since the release of the World Health Organization’s (WHO) criteria for BMI categories [10] in 1995 and their subsequent adoption by the National Heart, Lung and Blood Institute (NHLBI) [11], there has been a discrepancy between the cutoff points used for pregnant and non-pregnant women of childbearing age. More women are categorized as underweight and obese and fewer as normal-weight or overweight with the criteria used in the 1990 IOM guidelines than with the WHO/NHLBI criteria. In addition, the 1990 IOM guidelines [1] included only a minimal recommended weight gain (15 lb) for obese women, but no upper limit or range.
Experience has consistently shown that women who gained within the IOM’s 1990 guidelines for weight gain during pregnancy [1] have better outcomes of pregnancy [12–13,14*,15**]. However, this experience is based entirely on observational studies, so it remains unknown whether these improved outcomes result from the characteristics of women whose behavior permits them to gain within the guidelines or from true benefits of gaining within the ranges developed in the 1990 IOM report. However, women who gain outside of the guidelines do not necessarily have worse outcomes of pregnancy [16] because many factors other than GWG are related to the short- and long-term outcomes of pregnancy.
Consequences of gestational weight gain for mother and infant
Since 1990, knowledge has improved about the consequences of GWG for both the mother and the infant. These are reviewed in detail in a systematic evidence-based review [17**] as well as in the new report from the IOM and the National Research Council (NRC), Weight Gain During Pregnancy: Reexamining the Guidelines [9**]. Of all of the maternal antepartum, intrapartum and postpartum outcomes considered in the systematic, evidence-based review [17** the evidence that GWG was related to these outcomes was rated as “weak,” except for cesarean delivery and intermediate-term (3–36 mo) postpartum weight retention, where it was rated as “moderate.” Of all of the birth and postnatal outcomes considered, the evidence that GWG was related to these outcomes was also rated as “weak,” except for expressions of birthweight (birthweight, low birthweight, macrosomia and small-and large-for-gestational age) and preterm birth, where it was rated as “strong.”
Numerous investigators have sought an association of GWG with gestational diabetes mellitus (GDM) or hypertensive disorders during pregnancy. However, reviews of these studies [9**,17**] found that most investigators did not measure weight gain before the diagnosis of GDM or account for the possibility of a shortened duration of gestation associated with hypertensive disorders of pregnancy, such as preeclampsia. The time order of measurement relative to diagnosis is important for GDM because treatment with diet and/or insulin plus increased physical activity may affect subsequent weight gain.
The evidence for an association between GWG and cesarean delivery was inconsistent, in part because of failure to adjust for route of prior delivery among multiparous women. When weight gain categorized as being above the IOM’s 1990 guidelines, however, it was consistently associated with an increased risk of cesarean delivery [9**].
Higher GWG (whether within or above the 1990 IOM guidelines) was associated with greater postpartum weight retention, but this body of evidence was plagued by lack of consistent adjustment for important factors such as dietary intake, physical activity and breastfeeding behavior [9**]. Higher GWG may lead to excessive postpartum weight retention and, thus, increase the risk of moving into a higher BMI category [9**]. This retained weight increases the risks to the woman and her fetus during a subsequent pregnancy and to the woman’s own longer-term health.
The 1990 IOM guidelines for weight gain during pregnancy were based on the strong association between GWG and infant size at birth. Evidence for this association is also present in the data obtained subsequently [9**;17**]. Although the association between GWG and preterm birth is strong, it is also complex and biological plausibility for a causal relationship is questionable [9**]. In contrast, moderately strong evidence links GWG to infant mortality [9**]. Of great interest, given the high proportion of women whose weight gains exceeded the 1990 IOM guidelines and the high proportion of obesity among children [18*], is the possibility of an association between GWG and childhood obesity. Evidence for this is, to date, limited and inconsistent but more research on this subject is warranted.
The 2009 IOM/NRC guidelines for weight gain during pregnancy
On this background, the Committee to Reexamine IOM Pregnancy Weight Guidelines prepared and the IOM and NRC has recently issued new guidelines for weight gain during pregnancy [9**]. These guidelines were developed very differently from those published in 1990 [1]. Instead of developing weight gain ranges in which just the risk of low birthweight or preterm birth was minimized, this committee examined the trade-offs between mother and infant in both short- and longer-term outcomes and sought the ranges in which this trade-off was most favorable. This was assessed primarily by considering the outcomes most consistently and plausibly associated with GWG: infants born small- or large-for-gestational age, the mother’s risk for an unplanned cesarean delivery and excessive (≥5 kg) postpartum weight retention. In developing the ranges for each category of prepregnancy BMI, the committee considered the incidence or prevalence of each condition, whether the short- or long-term outcomes of the conditions were permanent and the quality of the available data.
The evidence remains strong that prepregnancy BMI is an important determinant of many outcomes of pregnancy [9**], so the new guidelines for weight gain during pregnancy (Table 2) continue to be presented according to prepregnancy BMI category. Adequate evidence was available to extend the guidelines to the category of obese (≥ 30 kg/m2) women. To provide consistency in women’s care, these new guidelines are based on the BMI cutoffs developed by the WHO [10] and adopted by the NHLBI [11] that are widely used in the United States and elsewhere. Separate guidelines are provided for mothers of singletons and, provisionally, for mothers of twins. Evidence was insufficient to develop even provisional guidelines for underweight women carrying twins or for women carrying higher-order multiple fetuses.
Table 2.
2009 IOM/NRC guidelines for weight gain and rate of weight gain during pregnancy for women with singleton fetuses and for weight gain for women with twin fetuses
| Prepregnancy body mass index category | Mothers of singletons | Mothers of twins (provisional) | |
|---|---|---|---|
| Total weight gain (lb) | Rate of weight gain in the second and third trimesters (lb/wk) | Total weight gain at term (lb) | |
| Underweight (< 18.5 kg/m2) | 28–40 | 1.0 (1.0–1.3) | No guideline available |
| Normal-weight (18.5–24.9 kg/m2) | 25–35 | 1.0 (0.8–1.0) | 37–54 |
| Overweight (25.0–29.9 kg/m2) | 15–25 | 0.6 (0.5–0.7) | 31–50 |
| Obese (≥ 30.0 kg/m2) | 11–20 | 0.5 (0.4–0.6) | 25–42 |
Notable for their absence in these new guidelines is any special recommendation for women of short (< 157 cm) stature, adolescents or members of racial/ethnic minority groups [9**]. Evidence available to the committee for all three of these groups was quite limited. The evidence showed that the association between GWG and unplanned cesarean delivery was not modified by short stature. Neither adolescence nor being a member of a racial/ethnic subgroup of the population modified the association between GWG and the various outcomes of pregnancy considered by the committee. However, the available evidence was insufficient to reject this possibility, so the committee concluded that further study of it was warranted.
Although the proportion of women of childbearing age in the American population who are overweight (BMI ≥25 kg/m2) or obese (BMI ≥30 kg/m2) appears to have stabilized, the proportion who are severely obese (BMI ≥40 kg/m2) is increasing [2]. Evidence was insufficient to construct guidelines for weight gain among the women with class II (BMI 35–39.9 kg/m2) or class III (BMI ≥40 kg/m2) obesity using the committee’s approach. The committee acknowledged that gains lower than those recommended for obese women in general might be appropriate for women with class II or class III obesity. This is because some women in these prepregnancy BMI categories gain minimally during pregnancy or even lose weight while managing their pattern of dietary intake to avoid ketonemia. However, the committee was concerned about the potential of low or no gain during pregnancy, particularly among women with glucose intolerance, to be harmful if it was associated with fetal growth restriction or ketonemia [9**].
In addition to recommendations for total GWG, the new guidelines include recommendations for rate of GWG (Table 2). These were constructed as a linear interpolation between the ~1–2 kg that women typically gain during the first trimester and the target total GWG for each prepregnancy BMI category divided by the number of weeks in the remaining 2 trimesters of pregnancy.
Use of the 2009 IOM/NRC guidelines for weight gain during pregnancy
The 2009 IOM guidelines are intended to be used “in concert with good clinical judgment as well as a discussion between the woman and her prenatal care provider about diet and exercise” [9**]. Consideration of relevant clinical evidence, such as the adequacy and consistency of fetal growth, as well as the woman’s personal circumstances will be necessary to inform this good clinical judgment. The committee recommended that weight loss issues be addressed preconceptionally or between pregnancies, not during pregnancy, because the safety of intentional weight loss during pregnancy has not been determined [9**]. Recommendation on how to monitor weight gain during pregnancy remain the same as in the 1990 IOM report [1] and the companion implementation guide [4]. Draft charts for use with patients are provided in the report [9].
Helping women to gain within the new guidelines will be a challenge because both women and physicians will have to change their behaviors. Many women will have to gain less than they are currently gaining because half or more of American women are gaining too little or too much relative to the range specified in the new guidelines (Figure 1). Physicians will have to provide a more comprehensive set of services to women in more BMI categories and more women in each category than is presently the case. This includes women who are planning a pregnancy, who are pregnant and who have recently been pregnant. These services will have to be individualized to a woman’s circumstances and involve other health care personnel who can help women–at a minimum–with advice on diet and physical activity. Beyond showing that all of the interventions that have been successful in getting women to gain within the 1990 IOM guidelines or just to moderate their weight gain have involved individualized care, too little is known about what else would be helpful. Individualized care appears to be necessary, but may not be sufficient as not all interventions with this approach have been successful (Table 3).
Figure 1.
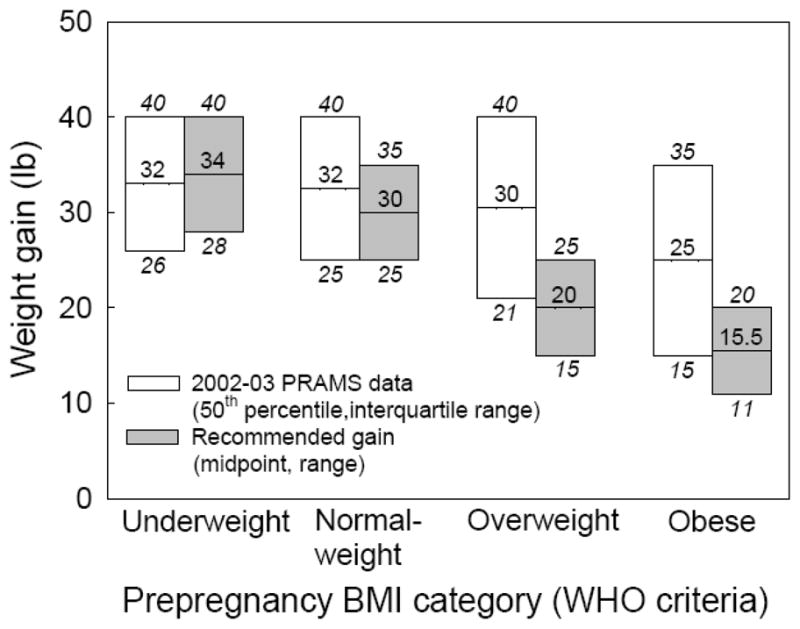
Comparison of current gestational weight gain of American women (Pregnancy Risk Assessment Monitoring System, 2002–03) with the 2009 IOM/NRC guidelines [9]. For the former, the interquartile range and mean is graphed. For the latter, the range and mid-point of the range is graphed. Adapted with permission from reference [9].
Table 3.
Strategies used to assist women to gain within the 1990 IOM guidelines or to moderate their weight gain: interventions studies published since 2000
| Author, year | Study site (n) | Intervention | Results |
|---|---|---|---|
| Gray-Donald et al., 2000 [19] | James Bay, Quebec, Canada (107 control, 112 intervention) | “Regular, individual diet counselling, physical activity sessions and other activities related to nutrition” | No differences in diet, weight gain, plasma glucose at 24–30 wk, birthweight or maternal weight at 6 wk postpartum |
| Polley et al., 2002 [20] | Pittsburgh, PA, USA (59 control, 61 intervention) | Stepped-care behavioral intervention with advice on appropriate weight gain, exercise and healthful eating during pregnancy; underweight women excluded | Reduced proportion who exceeded the 1990 IOM guidelines for GWG only among the normal-weight–and not the overweight–women |
| Olson et al., 2004 [21] | Cooperstown, NY, USA (381 historical controls, 179 intervention) | Monitoring of GWG using new tools in the obstetric chart, mailed information about GWG (“health checkbook”); normal-weight and overweight women only | Reduced the proportion who exceeded the 1990 IOM guidelines for GWG only among the lower-income–but not the higher-income–women |
| Kinnunen et al., 2007 [22] | Tampere and Hämeenlinna, Finland (63 control in 3 clinics, 69 intervention in 3 clinics) | Individual counseling on diet and physical activity during 5 routine visits with a public health nurse compared to usual care; primiparous women only | No difference in the proportion who exceeded the 1990 IOM guidelines for GWG; reduction in high birthweight (≥ 4000 g) in the intervention group |
| Kinnunen et al., 2007 [23] | Tampere and Hämeenlinna, Finland (39 control in 3 clinics, 53 intervention in 3 clinics) | Individual counseling on diet and physical activity during 5 routine visits with a public health nurse compared to usual care; primiparous women only | Increase in the proportion (adjusted analyses) of primiparous women who returned to their prepregnancy weight by 10 mo postpartum |
| Claesson et al., 2007 [24] | Linköping (155 intervention) and 2 nearby cities (193 control), Sweden | Weekly motivational talks and aqua aerobics classes; obese women only | Decrease in GWG and in BMI at the postpartum check-up |
| Wolff et al., 2008 [25**] | Copenhagen, Denmark (27 control, 23 intervention) | Restriction of GWG to 6–7 kg with 10 1-h dietary consultations; obese women only | Decrease in GWG, decrease in serum insulin and leptin concentrations at 27 wk gestation, and decrease in serum insulin and fasting blood glucose concentrations at 36 wk gestation |
| Asbee et al., 2009 [26*] | Charlotte, NC (43 control, 57 intervention) | Organized, consistent program of intensive dietary and lifestyle counseling | Decrease in GWG |
| Thornton et al., 2009 [27*] | New York City, NY area (133 control, 124 intervention) | Prescription for a balanced nutritional regimen with recording of all foods eaten each day; obese women only | Decrease in last weight before delivery and weight at 6 wk postpartum; decrease in gestational hypertension |
All of the interventions published since 2000 have focused on reducing GWG in the treated group and have used a variety of approaches to achieve this goal (Table 3). These approaches have included counseling on diet or exercise or both, monitoring of weight gain, provision of unique physical activity classes, dietary prescription and even daily recording of dietary intake. Most of these interventions have been delivered by ancillary health personnel (such as public health nurses, nurse midwives, dietitians and exercise consultants or trainers), not physicians. These interventions have had adequate statistical power to detect differences in weight gain or postpartum weight. In contrast, they have not had adequate statistical power to detect differences in obstetric outcomes, such as the incidence of unplanned cesarean deliveries, and birth outcomes, such as birth weight or gestational age at birth. Finding out what really works and why are research opportunities for obstetricians. Demonstrating with an experimental study that women who gain within the guidelines have better obstetric outcomes than those who do not would be a major contribution to the literature on this subject.
Implications of the 2009 IOM/NRC guidelines for weight gain during pregnancy
If all of the action recommendations in Nutrition During Pregnancy: Reexamining the Guidelines [9**] were to implemented, this would represent a “radical” change in the care of women of childbearing age in the United States. It would also represent a major opportunity for obstetrician/gynecologists to assume a larger role in the care of these women, including providing comprehensive preconceptional and postpartum care. This would help to fulfill the role of obstetrican/gynecologists as “women’s health care physicians” [http://www.acog.org/, accessed June 29, 2009]. The committee that wrote the new guidelines envisioned a model of care that considered all women of childbearing age to have the potential to become pregnant and, thus, to be eligible for services that have until now been limited to women who announced that they were planning a pregnancy. As a result of such a change in the model of what care should be delivered to women and when, improvements in the health of both women and their children may be achieved.
Acknowledgments
PMC was supported by NIH grant HD292965.
References and recommended reading
Papers of particular interest, published within the annual period of review, have been highlighted as:
* of special interest
** of outstanding interest
- 1.Institute of Medicine (Subcommittees on Nutritional Status and Weight Gain During Pregnancy and Dietary Intake and Nutrient Supplements During Pregnancy, Committee on Nutritional Status During Pregnancy and Lactation, Food and Nutrition Board) Nutrition During Pregnancy: Part I, Weight Gain; Part II, Nutrient Supplements. Washington, DC: National Academy Press; 1990. [Google Scholar]
- 2.Ogden CL, Carroll MD, Curtin LR, et al. Prevalence of overweight and obesity in the United States, 1999–2004. JAMA. 2006;295:1549–1555. doi: 10.1001/jama.295.13.1549. [DOI] [PubMed] [Google Scholar]
- 3.Institute of Medicine (Committee on Unintended Pregnancy, Division of Health Promotion and Disease Prevention) The Best Intentions: Unintended Pregnancy an the Well-Being of Children and Families. Washington, D.C: National Academy Press; 1995. [Google Scholar]
- 4.Institute of Medicine (Committee on Nutritional Status During Pregnancy and Lactation, Subcommittee for a Clinical Application Guide) Nutrition During Pregnancy and Lactation: An Implementation Guide. Washington, D.C: National Academy Press; 1992. [Google Scholar]
- 5.Power ML, Cogswell ME, Schulkin J. Obesity prevention and treatment practices of U.S. obstetrician-gynecologists. Obstet Gynecol. 2006;108:961–968. doi: 10.1097/01.AOG.0000233171.20484.db. [DOI] [PubMed] [Google Scholar]
- 6.Cogswell ME, Scanlon KS, Fein SB, Schieve LA. Medically advised, mother’s personal target, and actual weight gain during pregnancy. Obstet Gynecol. 1999;94:616–622. doi: 10.1016/s0029-7844(99)00375-0. [DOI] [PubMed] [Google Scholar]
- 7.Stotland NE, Haas JS, Brawarsky P, et al. Body mass index, provider advice, and target gestational weight gain. Am J Obstet Gynecol. 2005;105:633–638. doi: 10.1097/01.AOG.0000152349.84025.35. [DOI] [PubMed] [Google Scholar]
- 8*.Bish CL, Chu SY, Shapiro-Mendoza CK, et al. Trying to lose or maintain weight during pregnancy--United States, 2003. Matern Child Health J. 2009;13:286–292. doi: 10.1007/s10995-008-0349-x. Provides a unique insight about why women may not choose to follow the recommendations of their physicians for weight gain during pregnancy. [DOI] [PubMed] [Google Scholar]
- 9**.Rasmussen KM, Yaktine AL, editors. Institute of Medicine (Committee to Reexamine IOM Pregnancy Weight Guidelines, Food and Nutrition Board and Board on Children, Youth, and Families) Weight Gain During Pregnancy: Reexamining the Guidelines. Washington, DC: National Academy Press; 2009. Provides new guidelines for weight gain during pregnancy that are based on minimizing the risks of inadequate or excessive gains to mothers as well as their infants. [Google Scholar]
- 10.WHO Expert Committee on Physical Status. Physical Status: The Use and Interpretation of Anthropometry. WHO Technical Report Series No. 854. Geneva: World Health Organization; 1995. [PubMed] [Google Scholar]
- 11.NHLBI Obesity Education Initiative Expert Panel on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults. Clinical Guidelines on the Identification, Evaluation, and Treatment of Overweight and Obesity in Adults: the Evidence Report (NIH Publication No. 98-4083) Bethesda, MD: National Institutes of Health; 1998. [Google Scholar]
- 12.Carmichael S, Abrams B, Selvin S. The association of pattern of maternal weight gain with length of gestation and risk of spontaneous preterm delivery. Paediatr Perinat Epidemiol. 1997;11:392–406. doi: 10.1046/j.1365-3016.1997.d01-28.x. [DOI] [PubMed] [Google Scholar]
- 13.Abrams B, Altman SL, Pickett KE. Pregnancy weight gain: still controversial. Am J Clin Nutr. 2000;71:1233S–1241S. doi: 10.1093/ajcn/71.5.1233s. [DOI] [PubMed] [Google Scholar]
- 14*.Langford A, Joshu C, Chang JJ, et al. Does gestational weight gain affect the risk of adverse maternal and infant outcomes in overweight women? Matern Child Health J. 2008 doi: 10.1007/s10995-008-0318-4. Provides evidence that overweight women who gained within the 1990 IOM guidelines for weight gain during pregnancy had better outcomes of pregnancy than those who did not. [DOI] [PubMed] [Google Scholar]
- 15**.Olson CM. Achieving a healthy weight gain during pregnancy. Annu Rev Nutr. 2008;28:411–423. doi: 10.1146/annurev.nutr.28.061807.155322. Reviews the literature on experimental studies that are designed to help women gain within the guidelines during pregnancy. [DOI] [PubMed] [Google Scholar]
- 16.Parker JD, Abrams B. Prenatal weight gain advice: an examination of the recent prenatal weight gain recommendations of the Institute of Medicine. Obstet Gynecol. 1992;79:664–669. [PubMed] [Google Scholar]
- 17**.Viswanathan M, Siega-Riz AM, Moos M-K, et al. Evidence Report/Technology Assessment, Number 168 (AHRQ Publication No. 08-E09) Research Triangle Park, NC: RTI International--University of North Carolina Evidence-based Practice Center; 2008. Outcomes of Maternal Weight Gain. Provides a systematic, evidence-based review of the consequences of gestational weight gain (both absolute gain and gain relative to the 1990 IOM guidelines for weight gain during pregnancy) for mother and infant. [Google Scholar]
- 18*.Ogden CL, Carroll MD, Flegal KM. High body mass index for age among US children and adolescents, 2003–2006. JAMA. 2008;299:2401–2405. doi: 10.1001/jama.299.20.2401. Provides the latest nationally representative data for measures of obesity among American children and adolescents. [DOI] [PubMed] [Google Scholar]
- 19.Gray-Donald K, Robinson E, Collier A, et al. Intervening to reduce weight gain in pregnancy and gestational diabetes mellitus in Cree communities: an evaluation. CMAJ. 2000;163:1247–1251. [PMC free article] [PubMed] [Google Scholar]
- 20.Polley BA, Wing RR, Sims CJ. Randomized controlled trial to prevent excessive weight gain in pregnant women. Int J Obes. 2002;26:1494–1502. doi: 10.1038/sj.ijo.0802130. [DOI] [PubMed] [Google Scholar]
- 21.Olson CM, Strawderman MS, Reed RG. Efficacy of an intervention to prevent excessive gestational weight gain. Am J Obstet Gynecol. 2004;191:530–536. doi: 10.1016/j.ajog.2004.01.027. [DOI] [PubMed] [Google Scholar]
- 22.Kinnunen TI, Pasanen M, Aittasalo M, et al. Preventing excessive weight gain during pregnancy--a controlled trial in primary health care. Eur J Clin Nutr. 2007;61:884–891. doi: 10.1038/sj.ejcn.1602602. [DOI] [PubMed] [Google Scholar]
- 23.Kinnunen TI, Pasanen M, Aittasalo M, et al. Reducing postpartum weight retention--a pilot trial in primary health care. Nutr J. 2007;6:21. doi: 10.1.1186/1475-2891-6-21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Claesson I-M, Sydsjö G, Brynhildsen J, et al. Weight gain restriction for obese pregnant women: a case-control intervention study. BJOG. 2007;115:44–50. doi: 10.1111/j.1471-0528.2007.01531.x. [DOI] [PubMed] [Google Scholar]
- 25**.Wolff S, Legarth J, Vangsgaard K, et al. A randomized trial of the effects of dietary counseling on gestational weight gain and glucose metabolism in obese pregnant women. Int J Obes. 2008;32:495–501. doi: 10.1038/sj.ijo.0803710. Provides the evidence from a randomized trial among obese women that reducing weight gain during pregnancy results in a more favorable metabolic profile. [DOI] [PubMed] [Google Scholar]
- 26*.Asbee SM, Jenkins TR, Butler JR, et al. Preventing excessive weight gain during pregnancy through dietary and lifestyle counseling: a randomized controlled trial. Obstet Gynecol. 2009;113:305–312. doi: 10.1097/AOG.0b013e318195baef. Provides evidence that from a randomized trial an organized, consistent program of lifestyle counseling prevents excessive weight gain during pregnancy. [DOI] [PubMed] [Google Scholar]
- 27*.Thornton YS, Smarkola C, Kopacz SM, Ishoof SB. Perinatal outcomes in nutritionally monitored obese pregnant women: a randomized clinical trial. J Natl Med Assoc. 2009;101:569–577. doi: 10.1016/s0027-9684(15)30942-1. Provides evidence from a randomized trial among obese women that an intervention consisting of a prescribed, balanced nutritional regiment and recording of daily food intake resulted in a lower weight at delivery and lower postpartum weight retention. [DOI] [PubMed] [Google Scholar]


