Abstract
With the aim of determining if specialty type or the amount of geriatric training during primary care residencies correlated with the rate of and comfort with dementia identification and management in patients 65 years and older, physician practice patterns were compared through a web-based survey. The survey was sent to family medicine, internal medicine, and geriatric physicians in Dallas County and the HealthTexas Provider Network as well as third-year family medicine and internal medicine residents in Texas. Chi-square analyses revealed no relationship between the quantity of geriatric training and either dementia screening rates or comfort with dementia diagnosis. However, there was a significant difference in these areas based on specialty: more geriatricians reported asking senior patients about memory problems and being very comfortable in making a diagnosis of dementia, while fewer family medicine and internal medicine physicians reported being very comfortable in making the dementia diagnosis. Most physicians surveyed supported instituting routine screening and evaluation of senior patients during residency training. Further research is needed to determine if brief screening modalities, enhanced training, and institution of national guidelines would result in earlier identification and management of dementia in primary care.
Dementia is a syndrome of acquired persistent dysfunction in several domains of intellectual functioning, including memory, language, visuospatial ability, and cognition. Approximately 10% of adults above age 65 and 50% of adults above age 90 have dementia (1). The annual health care–related costs and lost wages for US patients with dementia and their family caregivers is approximately $100 billion (2–5). While the majority of dementing illnesses are progressive, 11% of patients with cognitive decline have reversible causes, and the course of the disease may be modified by early diagnosis and therapeutic interventions (1). Given these factors as well as the social and psychosocial cost of dementing illnesses on patients and their families, early diagnosis and intervention are paramount.
The number of persons with dementia increases as the population ages. The number of persons aged 65 and older in 2030 is projected to be twice as large as in 2000, growing from 35 million to 72 million and representing nearly 20% of the total US population (6). Given that the number of geriatricians is not increasing at a similar rate, family medicine and internal medicine physicians will be uniquely poised to be the first to identify cognitive changes indicative of dementia. Unfortunately, studies indicate that primary care physicians (PCPs) may not be identifying dementia in the majority of symptomatic patients. In 1995 Callahan et al found that PCPs recorded a diagnosis of dementia in only 23.5% of patients with demonstrated moderate to severe cognitive impairment (7). Further, those PCPs who reported difficulty establishing a diagnosis of dementia had difficulty communicating the diagnosis to patients and family members (7, 8). These findings were echoed by Valcour et al, whose cross-sectional study of primary care (internal medicine) patients aged 65 and older found that 91% of cases of mild dementia were overlooked, and 65% of dementia cases were not documented in the outpatient medical record (9).
Most likely, many factors—related to both the physician and the patient—contribute to the underdiagnosis of dementia. One possible factor is the lack of clear national guidelines for dementia screening. The 2003 US Preventive Services Task Force report does not recommend for or against routine screening for dementia in older adults (2). The American Academy of Neurology and the Canadian Task Force of Preventive Healthcare concluded that there is insufficient evidence to recommend cognitive screening of asymptomatic individuals (10). Despite the lack of evidence for routine screening, the US Preventive Services Task Force states that early recognition of cognitive impairment, in addition to helping make diagnostic and treatment decisions, allows clinicians to anticipate problems patients may have in understanding and adhering to recommended therapy.
Physicians' lack of comfort with dementia screening and diagnosis, due to inadequate training in the care of the elderly, plays a significant role in the delayed recognition of this disease. In a survey of 403 physicians in general practice, family medicine, and internal medicine, physicians scored 74%, or a “C,” on a test of knowledge about Alzheimer's disease (11). Similarly, in a survey of PCPs, Cody and colleagues found that 54% had difficulty establishing a diagnosis of dementia, and 30% had difficulty communicating the dementia diagnosis to the patient and family (8). The authors concluded that educational initiatives and behavioral changes targeting physicians and dementia assessment protocols would be beneficial for improving dementia care. In 2003, only 27 of the 91 Residency Review Committee–accredited specialties had specific geriatrics training. The average duration of training in geriatrics varied from 2 weeks to 6 weeks, with 62% of the programs having a structured 4-week geriatrics experience (12–14).
Further, physicians' concerns about the futility of making a diagnosis of dementia due to a perceived lack of treatment options and the time required to effectively diagnose the disease and educate patients and their families play a significant role in underdiagnosis (10, 15).
Patient factors contributing to the underrecognition of dementia include the patient's and family members' lack of awareness of the disease process and cultural factors (16, 17). In many cultures, memory problems are assumed to be part of the aging process rather than a consequence of disease.
The purpose of this study was to survey PCPs in an effort to better understand the possible reasons for underdiagnosis of dementia. No studies to date have investigated the relationship between quantity of training in geriatrics and rates of screening and diagnosis among PCPs. Therefore, this study aimed to assess geriatric, family medicine, and internal medicine physicians' and residents' practice patterns in dementia evaluation and management in patients aged 65 and older to determine if such a relationship exists. A secondary purpose was to obtain physicians' opinions about establishing guidelines for dementia screening.
METHODS
For this institutional review board–approved study, the authors identified family medicine and internal medicine residency programs in Texas and sent an e-mail to program directors requesting the participation of third-year residents. The total number of possible recipients was 258 third-year family medicine residents and 282 internal medicine residents. Similarly, the authors identified family medicine, internal medicine, and geriatric medicine physicians practicing in Dallas County (N = 250) and within HealthTexas Provider Network (family medicine, N = 109; internal medicine, N = 127; geriatrics, N = 8) and requested their participation by an e-mail directed to the office managers with a request to forward it to the appropriate individuals.
The e-mail included an informational letter introducing the study and a request that participants use a hyperlink to access the anonymous, web-based survey. This survey had 28 questions assessing participants' demographic information, specialty, extent of geriatric training, and practice preferences about dementia. Physicians were also asked their opinions regarding establishing national guidelines for dementia screening and diagnosis and the measures they would support for increasing physician knowledge of dementia diagnosis and management. Items selected for survey inclusion were modeled after those reported in similar studies (8, 11). The survey took approximately 3 minutes to complete.
A reminder was sent 2 weeks after the initial mailing requesting those who had not completed the survey to do so. Due to poor resident response, a third reminder was sent to the family and internal medicine residency program directors in Texas, requesting that they again share the informational letter with their third-year residents.
RESULTS
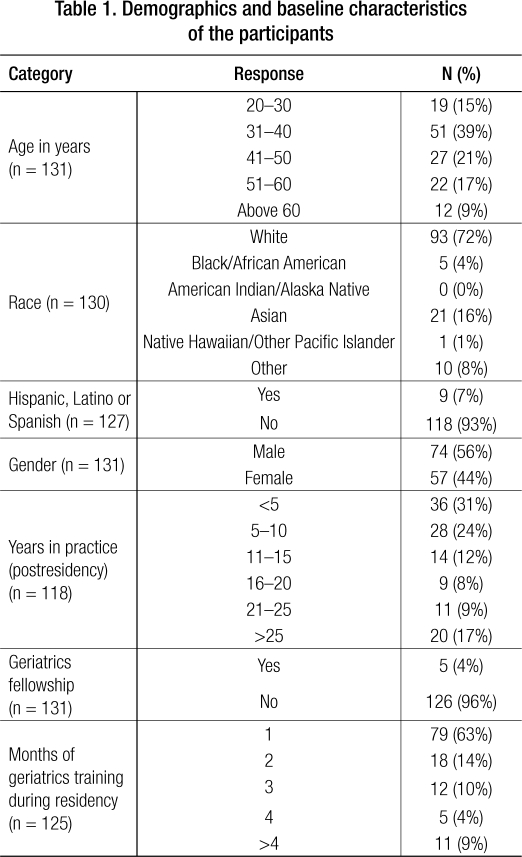
There were 134 respondents: 55% in family medicine, 41% in internal medicine, and 4% in geriatric medicine. Most respondents (79%) were practicing physicians; 20% were residents and 1% were fellows. Demographic information is summarized in Table 1. It was not possible to calculate a true response rate, since it was unclear if all of the intended recipients received the survey from either the program coordinators or office managers.
Table 1.
Demographics and baseline characteristics of the participants
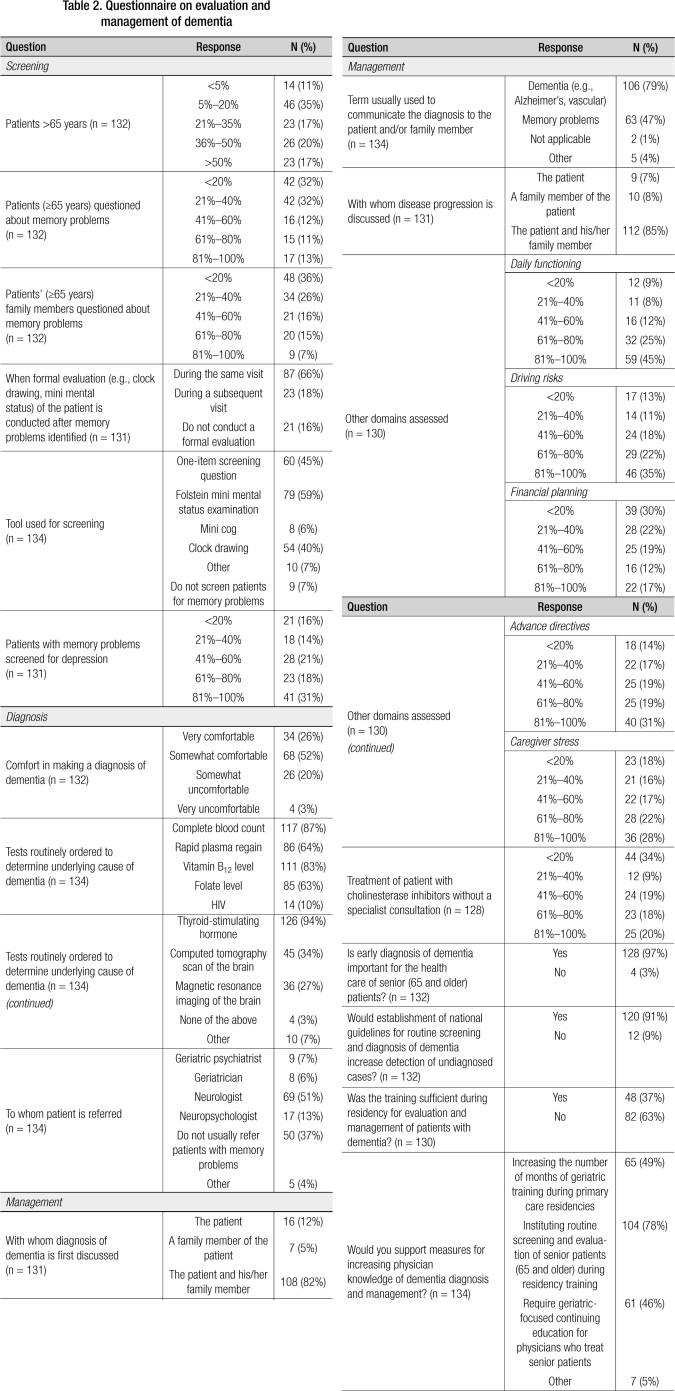
Even though the majority of the respondents (97%) believed that an early diagnosis of dementia is important for the care of seniors, most of them did not routinely screen their patients for memory problems. The Folstein mini mental status examination was the most commonly used tool for screening (59%), and physicians often conducted a formal evaluation at the same visit (66%). Laboratory tests ordered included thyroid-stimulating hormone (94%), complete blood count (87%), vitamin B12 (83%), folate (63%), and rapid plasma reagin (64%). Most physicians ordered radiological evaluation for patients with memory problems (computed tomography of the brain [34%] or magnetic resonance imaging [27%]). More than 50% of the PCPs referred their patients to a neurologist, with far fewer referring them to a neuropsychologist (13%), geriatrician (6%), or geriatric psychiatrist (7%). Further, few physicians initiated treatment with cholinesterase inhibitors without consultation with a specialist. Financial planning, advance directives, and caregiver stress were least addressed by the PCPs. Responses for the survey questions are summarized in Table 2.
Table 2.
Questionnaire on evaluation and management of dementia
Chi-square analyses of variance were used to assess the relationship between both specialty and months of geriatrics training and each of the survey domain items (i.e., dementia screening, dementia diagnosis and management, improving dementia recognition and management). No relationship was identified between months of geriatric training and screening rates (chi square = 14.664, P = 0.549). However, a significant relationship between specialty and screening rates was identified (chi square = 23.559, P = 0.003), with the few geriatrician respondents reporting more frequent dementia screening of senior patients than the other specialties. Chi-square analyses also indicated a significant difference in comfort making a diagnosis of dementia by specialty (chi square = 22.820, P = 0.001). Specifically, few family medicine physicians reported being “very comfortable” in making a diagnosis of dementia, and more geriatricians reported being “very comfortable” in making a diagnosis of dementia. No other analyses reached statistical significance.
DISCUSSION
Previous research has indicated that PCPs underdiagnose dementia (7–9). The goal of this study was to determine if the duration of geriatric training in primary care residencies and the specialty area (i.e., geriatrics vs internal medicine vs family practice) were factors related to screening rates and comfort in diagnosing dementia. Interestingly, there was no relationship between the amount of PCPs' geriatric training and their comfort with dementia screening and how often they questioned the patient about memory problems. However, there was a significant difference in these areas based on specialty. More geriatricians reported asking senior patients about memory problems and being very comfortable in making a diagnosis of dementia, while fewer family medicine and internal medicine physicians reported being very comfortable in making the dementia diagnosis. This difference could be due to the fact that geriatricians are involved only in the care of the elderly and therefore are more vigilant for this disease, whereas PCPs are involved in the care of patients with broader age groups. Further, geriatricians are less likely to have negative attitudes toward management of patients with dementia-related illnesses. Our study results are comparable to the findings by Chodosh et al, that physicians with geriatric credentials (defined as geriatric fellowship experience and/or the certificate of added qualifications) recognized cognitive impairment more often than those without (18).
Several limitations to this study must be addressed. First, the sample in this study was largely a convenience sample, chosen in part based on the availability of e-mail addresses. However, the sample size was comparable to that of earlier studies assessing physicians' knowledge (8, 19). It is also possible that submitting the questionnaire in checklist format introduced response bias, with physicians reporting behaviors considered appropriate rather than their actual behaviors. Lastly, not all specialty groups were equally represented, and the response rate from the residents was poor in spite of the third mailing. Physicians with a geriatric fellowship accounted for only 4% of our sample.
According to a 1994 survey, most general practitioners were aware of the clinical features of dementia, although many felt their knowledge and expertise were inadequate and strongly supported instituting a dementia protocol (19–21). However, the ACCESS (Alzheimer's Disease Coordinated Care for San Diego Seniors) study, a comprehensive dementia care management model, demonstrated no significant differences in providers' knowledge or attitudes that proved favorable to dementia care. Further, the physicians in the intervention group viewed dementia patients as difficult to manage in primary care.
In our survey, 63% of the physicians believed they did not receive sufficient training in dementia evaluation and management during residency. Despite this, only 49% supported increasing the duration of geriatric training during residency; in contrast, 78% supported instituting routine screening and evaluation of senior patients during residency training. Our study does not allow comment on who is responsible for this screening. This could reflect the fact that the content of the training, rather than the duration, may be an important factor in increasing comfort in diagnosing and managing dementia. In 2004, it was estimated that there was a significant increase in the number of programs with a required geriatrics curriculum (96%) compared with 2001. Further, resident attitudes as a barrier to implementing the curriculum dropped from 32% in 2001 to 4% in 2004 (12). It is possible that increasing physician exposure to dementia screening, diagnostic disclosure (22), and management during training and instituting national guidelines would be helpful in providing patients and family with improved quality of care. Therefore, more research is needed to determine if these measures would result in earlier identification and management of dementia.
Acknowledgments
The authors wish to acknowledge Ms. Debra Faber, MLS, for her assistance and preparation of the manuscript. This paper was presented at the North American Primary Care Research Group (NAPCRG) as poster for research in progress in October 2006.
References
- 1.Adelman AM, Daly MP. Initial evaluation of the patient with suspected dementia. Am Fam Physician. 2005;71(9):1745–1750. [PubMed] [Google Scholar]
- 2.Boustani M, Peterson B, Hanson L, Harris R, Lohr KN, U.S. Preventive Services Task Force Screening for dementia in primary care: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2003;138(11):927–937. doi: 10.7326/0003-4819-138-11-200306030-00015. [DOI] [PubMed] [Google Scholar]
- 3.Evans DA, Smith LA, Scherr PA, Albert MS, Funkenstein HH, Hebert LE. Risk of death from Alzheimer's disease in a community population of older persons. Am J Epidemiol. 1991;134(4):403–412. doi: 10.1093/oxfordjournals.aje.a116102. [DOI] [PubMed] [Google Scholar]
- 4.Ernst RL, Hay JW. The US economic and social costs of Alzheimer's disease revisited. Am J Public Health. 1994;84(8):1261–1264. doi: 10.2105/ajph.84.8.1261. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Arno PS, Levine C, Memmott MM. The economic value of informal caregiving. Health Aff (Millwood) 1999;18(2):182–188. doi: 10.1377/hlthaff.18.2.182. [DOI] [PubMed] [Google Scholar]
- 6.He W, Sengupta M, Velkoff VA, DeBarros KA. 65⊞ in the United States: 2005 [Current Population Reports]. Washington, DC: US Department of Health and Human Services and US Department of Commerce. Retrieved from http://www.census.gov/prod/2006pubs/p23-209.pdf
- 7.Callahan CM, Hendrie HC, Tierney WM. Documentation and evaluation of cognitive impairment in elderly primary care patients. Ann Intern Med. 1995;122(6):422–429. doi: 10.7326/0003-4819-122-6-199503150-00004. [DOI] [PubMed] [Google Scholar]
- 8.Cody M, Beck C, Shue VM, Pope S. Reported practices of primary care physicians in the diagnosis and management of dementia. Aging Ment Health. 2002;6(1):72–76. doi: 10.1080/13607860120101158. [DOI] [PubMed] [Google Scholar]
- 9.Valcour VG, Masaki KH, Curb JD, Blanchette PL. The detection of dementia in the primary care setting. Arch Intern Med. 2000;160(19):2964–2968. doi: 10.1001/archinte.160.19.2964. [DOI] [PubMed] [Google Scholar]
- 10.Petersen RC, Stevens JC, Ganguli M, Tangalos EG, Cummings JL, DeKosky ST. Practice parameter: early detection of dementia: mild cognitive impairment (an evidence-based review). Report of the Quality Standards Subcommittee of the American Academy of Neurology. Neurology. 2001;56(9):1133–1142. doi: 10.1212/wnl.56.9.1133. [DOI] [PubMed] [Google Scholar]
- 11.Brown CJ, Mutran EJ, Sloane PD, Long KM. Primary care physicians' knowledge and behavior related to Alzheimer's disease. J Appl Gerontol. 1998;17(4):462–479. [Google Scholar]
- 12.Bragg EJ, Warshaw GA, Arenson C, Ho ML, Brewer DE. A national survey of family medicine residency education in geriatric medicine: comparing findings in 2004 to 2001. Fam Med. 2006;38(4):258–264. [PubMed] [Google Scholar]
- 13.Bragg EJ, Warshaw GA. ACGME requirements for geriatrics medicine curricula in medical specialties: progress made and progress needed. Acad Med. 2005;80(3):279–285. doi: 10.1097/00001888-200503000-00014. [DOI] [PubMed] [Google Scholar]
- 14.Warshaw GA, Bragg EJ, Thomas DC, Ho ML, Brewer DE, Association of Directors of Geriatric Academic Programs Are internal medicine residency programs adequately preparing physicians to care for the baby boomers? A national survey from the Association of Directors of Geriatric Academic Programs Status of Geriatrics Workforce Study. J Am Geriatr Soc. 2006;54(10):1603–1609. doi: 10.1111/j.1532-5415.2006.00895.x. [DOI] [PubMed] [Google Scholar]
- 15.Boise L, Camicioli R, Morgan DL, Rose JH, Congleton L. Diagnosing dementia: perspectives of primary care physicians. Gerontologist. 1999;39(4):457–464. doi: 10.1093/geront/39.4.457. [DOI] [PubMed] [Google Scholar]
- 16.Ross GW, Abbott RD, Petrovitch H, Masaki KH, Murdaugh C, Trockman C, Curb JD, White LR. Frequency and characteristics of silent dementia among elderly Japanese-American men. The Honolulu-Asia Aging Study. JAMA. 1997;277(10):800–805. [PubMed] [Google Scholar]
- 17.Braun KL, Browne CV. Perceptions of dementia, caregiving, and help seeking among Asian and Pacific Islander Americans. Health Soc Work. 1998;23(4):262–274. doi: 10.1093/hsw/23.4.262. [DOI] [PubMed] [Google Scholar]
- 18.Chodosh J, Petitti DB, Elliott M, Hays RD, Crooks VC, Reuben DB, Galen Buckwalter J, Wenger N. Physician recognition of cognitive impairment: evaluating the need for improvement. J Am Geriatr Soc. 2004;52(7):1051–1059. doi: 10.1111/j.1532-5415.2004.52301.x. [DOI] [PubMed] [Google Scholar]
- 19.Turner S, Iliffe S, Downs M, Wilcock J, Bryans M, Levin E, Keady J, O'Carroll R. General practitioners' knowledge, confidence and attitudes in the diagnosis and management of dementia. Age Ageing. 2004;33(5):461–467. doi: 10.1093/ageing/afh140. [DOI] [PubMed] [Google Scholar]
- 20.Chodosh J, Berry E, Lee M, Connor K, DeMonte R, Ganiats T, Heikoff L, Rubenstein L, Mittman B, Vickrey B. Effect of a dementia care management intervention on primary care provider knowledge, attitudes, and perceptions of quality of care. J Am Geriatr Soc. 2006;54(2):311–317. doi: 10.1111/j.1532-5415.2005.00564.x. [DOI] [PubMed] [Google Scholar]
- 21.Brodaty H, Howarth GC, Mant A, Kurrle SE. General practice and dementia. A national survey of Australian GPs. Med J Aust. 1994;160(1):10–14. [PubMed] [Google Scholar]
- 22.Connell CM, Boise L, Stuckey JC, Holmes SB, Hudson ML. Attitudes toward the diagnosis and disclosure of dementia among family caregivers and primary care physicians. Gerontologist. 2004;44(4):500–507. doi: 10.1093/geront/44.4.500. [DOI] [PubMed] [Google Scholar]