Abstract
Objective:
To report 4 cases of hyperfamiliarity for faces (HFF) and review 5 previously reported cases.
Methods:
We identified cases of HFF from PubMed search and references in prior reports.
Results:
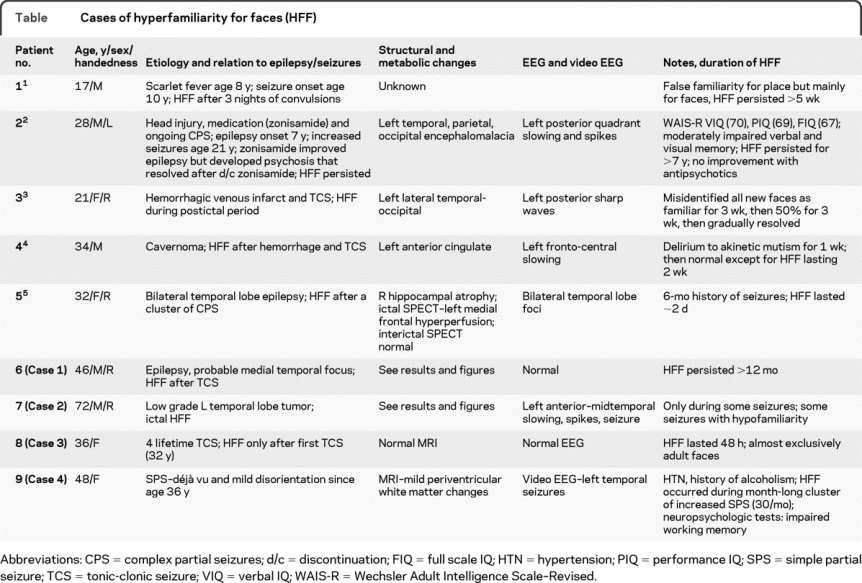
Three of our 4 cases had pathologic findings that were most extensive in the left temporal lobe. HFF occurred after a tonic-clonic seizure (cases 1 and 3), during simple partial seizures (case 2), and in the setting of an increase in simple partial seizure frequency but not during seizures (case 4). All 9 cases were adults with 1 or more seizures; symptoms first occurred after seizures in 5 cases and during seizures in 1 case. Ictal symptoms lasted from seconds to minutes and from 2 days to more than 7 years in the other 6 cases. The duration of HFF was not associated with the presence or extent of a structural lesion. While in several cases HFF appears to result from a postictal Todd paralysis, the mechanism underlying persistent cases is uncertain.
Conclusions:
This modality (visual)–specific and stimulus (face)–specific syndrome is associated with diverse structural, functional imaging, and neurophysiologic findings. Lesions are more often left-sided and involve the temporal lobe. Epilepsy and seizures were present in all 9 cases, suggesting a pathophysiologic relationship, which likely varies among cases. Although only reported in 9 patients, HFF is probably much more common than it is diagnosed.
GLOSSARY
- HFF
= hyperfamiliarity for faces.
Faces are unique visual stimuli for primates, encoding data about an individual's sex, group affiliation, identity, age, mood, direction of gaze, and behavioral intention. Visual recognition and mnemonic systems distinguish novel from previously encountered faces. The ability to translate the facial recognition by the fusiform face area into the emotionally relevant labels of familiar or novel, and grade the intensity of the familiarity, likely confers survival value. Facial familiarity can be dissociated from semantic or autobiographic elements of episodic memory since we may feel that we saw a face before, but cannot recall the name or place where it was seen. The hyperfamiliarity for faces (HFF) syndrome is a disorder in which unfamiliar people or faces appear familiar. Typically occurring without concurrent psychiatric, emotional, or memory disorders, the association of a familiar feeling with novel faces is a relatively isolated symptom. Kraeplin's1 1886–1887 classification of paramnesias included one HFF case, categorized as a complete associative falsification of recall. We report 4 additional cases and review 5 previously reported cases.
METHODS
Case 1.
A 46-year-old right-handed policeman had a tonic-clonic seizure, preceded that day by a complex partial seizure with an aura of anxiety, déjà vu, and a sulfuric smell. Six months earlier he had developed intermittent anxiety spells lasting 15 seconds. He had no risk factors for epilepsy. MRI and sleep-deprived EEG were normal. His neurologic examination was normal; he was treated with lamotrigine. A month later, he reported 1) that everyone appeared familiar, 2) memory problems, 3) increased emotionality for sadness, and 4) trouble with multitasking and distractibility. HFF began after his convulsion. A week later, he attended a community fundraiser, and every face looked familiar. He kept asking strangers, “Where do I know you from?”
Walking on the street, every person I see looks familiar to me. I say hello to everyone. There was a baseball game between a predominantly black town, and mine, which is mainly Irish Catholic. The other coach is black and I felt like I definitely knew him. I walked over and asked “Don't I know you?” They guy looked at me and said “I don't think so.” When I walked back everyone asked me what the hell I was doing.
Hyperfamiliarity occurred to a lesser degree with faces in photographs or on television, but not voices. His memory problems mainly affect autobiographical events. He had no recall of the 45-minute office visit a month earlier. Uncharacteristically, emotional scenes evoke tears. Simultaneously talking to someone and listening to the police radio in his and neighboring towns had been second nature for him, but he could no longer attend to multiple streams of conversation.
Neuropsychological testing revealed impairment of sustained attention and vigilance, and immediate encoding and short delay cued recall, and delayed recall of the Rey Osterrieth Complex Figure. Facial recognition was low average.
Case 2.
A 62-year-old right-handed attorney had developed partial epilepsy at age 31. Initial seizures involved severe anxiety and “doom,” palpitations, déjà vu, and a bad nightmare. A convulsion led to medical attention. Brain CT was normal. Phenytoin controlled tonic-clonic but not partial seizures. At age 43, partial seizures increased. MRI revealed a nonenhancing mass in the left mid-parahippocampal gyrus with slight involvement of the hippocampus that has been stable over 18 years (figure 1). Video-EEG revealed a left anterior to midtemporal seizure focus.
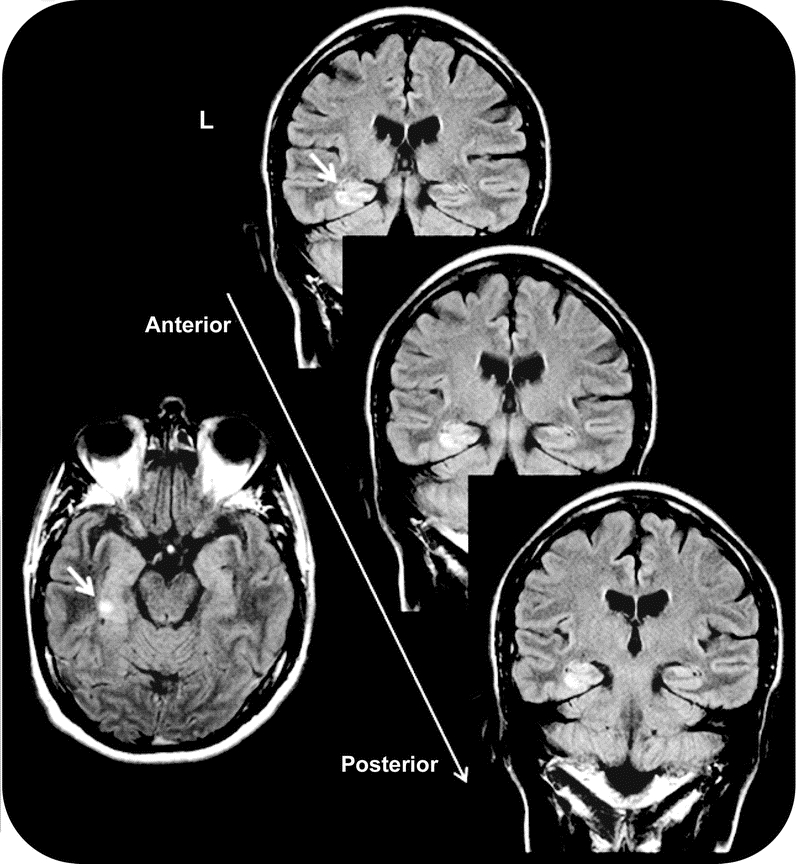
Figure 1 MRI–fluid-attenuated inversion recovery images nonenhancing left mid-parahippocampal lesion (see arrow) in case 2 (L = left hemisphere)
Current seizures involve fear with loss of memory and identity. He reported, “I sometimes don't know who I am or where I am.” During some seizures, he noted, “I get the feeling that a complete stranger is someone I have known for the past 20 years. Their face looks familiar.” More often, someone he knows well is difficult to identify. Interictally, he is irritable and depressed.
Neuroimaging results.
Neuroimaging results and description of cases 3 and 4 are presented in the table.
Table Cases of hyperfamiliarity for faces (HFF)
MRI morphometry methods (cases 1 and 2).
Methods are described in appendix e-1 on the Neurology® Web site at www.neurology.org; both patients signed institutional review board–approved study consent.
Subcortical volumes.
For data on subcortical volumes, see appendix e-1.
Cortical thickness.
Patient 1.
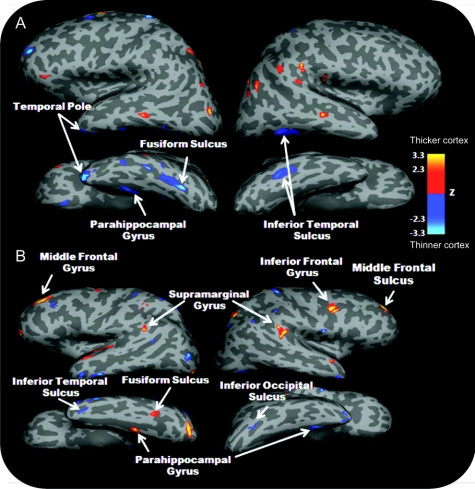
Several areas of decreased thickness were found (figure 2 and figure e-1), most notably the left posterior fusiform gyrus and middle parahippocampal gyrus and the right posterior inferior temporal gyrus. Increased thickness was observed mainly in the middle temporal gyri.
Figure 2 Z test comparison of cortical thickness across the whole brain between patient 1 (A), patient 2 (B), and their respective normative group
Blue indicates thinner cortex and red thicker cortex in the patient compared to age-matched and gender-matched normal control subjects (thresholded at z = ±2.3, cluster threshold p = 0.05).
Patient 2.
See figure 2 for areas of cortical thinning and thickening compared to controls and figure e-2 for position of changes in the parahippocampal regions.
DISCUSSION
HFF is an uncommon modality-specific and stimulus-specific syndrome identified in 9 patients with epilepsy or a tonic-clonic seizure. The diagnosis rests on a selective false familiarity for multiple faces; delusions are not present and neither voices nor nonface visual objects falsely elicit hyperfamiliarity in these patients. Lesions or seizure foci usually involved the left hemisphere (left 5, bilateral 2, unknown 2) and temporal lobe (6/7 with known localization) (table).2–5 The MRIs are normal or show nonspecific changes in 2/8 cases with imaging; lesions include remote trauma (1), stroke (2), and low-grade tumor (1).
The duration of HFF ranged from seconds to minutes in the ictal case and from 2 days to more than 7 years in the other cases. Duration did not correlate with the presence or extent of a lesion. Symptoms lasting hours to days may have resulted from a Todd paralysis5 (cases 4, 8, and 9). Paradoxically, persistent HFF occurred in 2 cases (2, 6) after seizures; these patients had no abnormal MRI results or remote head injuries and the mechanisms are unknown.
The physiology of recollection and familiarity are relevant to HFF. Recollection is the retrieval of specific contextual or related details associated with a prior episode. Familiarity is a feeling of recognition for a particular item without accompanying associated episodic details or any specific context. Selective lesions, electrical stimulation, and functional MRI studies reveal that the hippocampus is important for recollection while the perirhinal cortex is implicated in the feeling of familiarity.6–8 Déjà vu (already seen) and déjà vécu (already lived through) are hyperfamiliarity for a present experience with an undefined and often nonexistent past (familiarity without retrieval). They occur during seizures and stimulation of the amygdala, hippocampus, and perirhinal cortex, more common with right temporal hyperexcitability,9 supporting right dominance in familiarity.9 The neural response to a familiar stimulus is suppression as compared to the activation with a novel stimulus.8 Familiarity strength is signaled through graded repetition suppression.8 Epileptic discharges during déjà vu and vécu may suppress function and thereby mimic the experience of familiarity.
Déjà vu/vécu9 and HFF may result from increased activity in right relative to left medial temporal areas. HFF may be produced by impaired left hemisphere identification of unique facial features and excessive right hemisphere processes that link individual faces with emotional and personal meaning, leading to spurious familiarity feelings.10 Left temporal lobe dysfunction may impair novelty signaling and detection of specific facial features while disinhibiting right temporal regions that falsely signal familiarity.
Patients with HFF quickly accept that their recognition is false, likely reflecting preserved right hemispheric and frontal areas. In contrast, fixed delusions of misidentification or reduplication disorders usually result from lesions in bifrontal and/or right hemispheric areas.10 Lesions that destroy or isolate stimuli from right perirhinal cortex may impair familiarity (e.g., Capgras syndrome) while hyperfamiliarity (e.g., Fregoli syndrome) may result from overactivity in right perirhinal cortex,10 consistent with the effects of left temporal lesions in HFF.
Finally, HFF is probably much more common than clinically identified. The 4 cases described here were seen by a single author (O.D.) over a 2-year period without any systematic survey of patients. Thus, it is likely that the vast majority of cases go unrecognized and include cases with and without epilepsy.
DISCLOSURE
Dr. Devinsky serves on a speaker's bureau for UCB; has served as a consultant for Medivation, Inc.; serves as an Associate Editor of Epilepsy and Behavior and Co-Editor of Reviews in Neurological Diseases; receives royalties from the publication of Cognitive and Behavioral Neurology (Oxford University Press, 2002); and receives research support from the NIH/NINDS (R01 NS053998 [Phenome Core Leader]). Dr. Davachi has received travel expenses and/or honoraria for lectures or educational activities not funded by industry; has filed a US patent (17VV-148865, filed 2009) regarding: Methods and systems for evaluating cognitive augmenting agents and augmented cognitive training protocols; serves as a consultant for Dart Neuroscience; and receives research support from Dart Neuroscience and the NIH/NIMH (RO1MH074692 [PI]). Dr. Santschi, Mr. Quinn, and Dr. Staresina report no disclosures. Dr. Thesen receives research support from the NIH (RO1 NS018741 [PI on subcontract] and RO1-PA07-070 [PI on subcontract]), Finding a Cure for Epilepsy and Seizures (FACES), and from the Tuberous Sclerosis Alliance.
Supplementary Material
Address correspondence and reprint requests to Dr. Orrin Devinsky, NYU Epilepsy Center, 223 E 34 St., New York, NY 10016 od4@nyu.edu
Supplemental data at www.neurology.org
Disclosure: Author disclosures are provided at the end of the article.
Received May 4, 2009. Accepted in final form January 12, 2010.
REFERENCES
- 1.Kraeplin E. Ueber Erinnerungsfalschungen. Arch Psychiatr Nervenkr 1886;830–843, 1887;18:199–239, 395–436.
- 2.Murai T, Kubota Y, Sengoku A. Unknown people believed to be known: the ‘assoziierende Erinnerungs-fälschungen’ by Kraepelin. Psychopathology 2000;33:52–54. [DOI] [PubMed] [Google Scholar]
- 3.Vuilleumier P, Mohr C, Valenza N, Wetzel C, Landis T. Hyperfamiliarity for unknown faces after left lateral temporo-occipital venous infarction: a double dissociation with prosopagnosia. Brain 2003;126:889–907. [DOI] [PubMed] [Google Scholar]
- 4.Nente F, Carrillo-Mezo R, Mendez MF, Ramirez-Bermudez J. Pathological hyperfamiliarity for others From a left anterior cingulate lesion. J Neuropsychiatry Clin Neurosci 2007;19:345–346. [DOI] [PubMed] [Google Scholar]
- 5.Bujarski K, Sperling MR. Post-ictal hyperfamiliarity syndrome in focal epilepsy. Epilepsy Behav 2008;13:567–569. [DOI] [PubMed] [Google Scholar]
- 6.Davachi L, Mitchell JP, Wagner AD. Multiple routes to memory: distinct medial temporal lobe processes build item and source memories. Proc Natl Acad Sci 2003;100:2157–2162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bowles B, Crupi C, Mirsattari SM, et al. Impaired familiarity with preserved recollection after anterior temporal-lobe resection that spares the hippocampus. Proc Natl Acad Sci USA 2007;104:16382–16387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gonsalves BD, Kahn I, Curran T, Norman KA, Wagner AD. Memory strength and repetition suppression: multimodal imaging of medial temporal cortical contributions to recognition. Neuron 2005;47:751–761. [DOI] [PubMed] [Google Scholar]
- 9.Gianotti G. Face familiarity feelings, the right temporal lobe and the possible underlying neural mechanisms. Brain Res Rev 2007;56:214–235. [DOI] [PubMed] [Google Scholar]
- 10.Devinsky O. Delusional misidentifications and duplications: right brain lesions, left brain delusions. Neurology 2009;72:80–87. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.