SYNOPSIS
Objective
We assessed demographic and temporal trends of tuberculosis (TB)-related deaths in the United States and examined associated comorbidities listed on death certificates.
Methods
We analyzed TB-related mortality from 1990 through 2006 by examining multiple-cause-of-death data from the National Center for Health Statistics. We assessed age-adjusted mortality rates, secular trends, associations with demographic variables, and comorbid conditions.
Results
From 1990 through 2006, TB was reported as a cause of death among 53,505 people in the U.S. with a combined overall mean age-adjusted mortality rate of 1.16 per 100,000 person-years. The age-adjusted TB mortality rate declined from 2.22 per 100,000 person-years in 1990 to 0.47 per 100,000 person-years in 2006, demonstrating mean annual decline of about 10%. People aged 75 years and older; males; foreign-born people; and those of Hispanic, Asian, black, and Native American race/ethnicity had comparatively elevated TB-related mortality rates. The mortality rate in foreign-born people was more than two times higher than in U.S.-born people. About 89% of deaths among people of Asian race/ethnicity and nearly 50% among black people were foreign-born individuals. Human immunodeficiency virus and selected autoimmune diseases were more common in TB-related deaths.
Conclusions
TB mortality decreased substantially from 1990 through 2006, but remains an important cause of preventable mortality. The observed decrease was more pronounced among U.S.-born people than among foreign-born people. Disparities in TB-related mortality and the identification of important comorbid conditions can inform strategies targeting subpopulations at increased risk for fatal TB infection.
According to the World Health Organization, in 2007 an estimated two billion people—equal to one-third of the world's population—were infected with the bacterium that causes tuberculosis (TB) infection and disease.1 In spite of prevention and treatment programs in most nations, TB remains the second leading cause of death (COD) worldwide from infectious disease, exceeded only by human immunodeficiency virus (HIV)/acquired immunodeficiency syndrome (AIDS).2 Globally, approximately 9.2 million people become ill from active TB each year, and nearly 1.7 million people die from the disease.1
In the United States, TB is sometimes thought of as a disease of the past. In 2007, however, 13,293 people were diagnosed with active and potentially infectious TB disease.3 Severe cases of TB disease can require hospitalization and are extremely costly to treat, such that estimates of the total charges for the TB hospitalizations in the U.S. in 2000 exceeded $385 million.4 Although highly curative therapy is available in drug-sensitive cases, in-hospital mortality remains considerably high—ranging from 5% to 28%—and the persistence of multidrug-resistant TB (strains resistant to at least two primary anti-tubercular agents, Isoniazid and Rifampin) combined with the more recent emergence of extensively drug-resistant TB (resistant to almost all the anti-tubercular agents) present challenges to TB-control activities.3–5 In addition, persistent disparities between white people and racial/ethnic minority groups and between U.S.-born and foreign-born people continue to challenge progress toward TB elimination in the U.S.
Currently, an extensive body of peer-reviewed literature on TB incidence and prevalence is available, but the literature is scarce on the recent burden of TB-related mortality in the U.S.6,7 Understanding the mortality burden from TB disease can provide support to the funding of prevention, case-finding, and treatment strategies, including enhancing progress toward vaccine development. We analyzed the U.S. multiple-cause-of-death (MCOD) data from 1990 through 2006 to determine population-based estimates of demographic and temporal trends of TB-related deaths and associated comorbid conditions.
METHODS
All 50 states and the District of Columbia mandate mortality reporting using a standard death certificate set forth by the National Center for Health Statistics (NCHS). The death certificate provides information on characteristics of the decedent including age at death, gender, and race/ethnicity, as well as conditions that lead to death. The clinician completing the certificate records the CODs, which include immediate and underlying causes and other significant conditions contributing to death. The immediate COD is the final disease or condition leading directly to death, and the underlying COD is the condition that initiated the chain of events resulting in death. Diseases and related conditions reported on the death certificate are coded in accordance with the International Classification of Diseases, Ninth and 10th Revisions (ICD-9 and ICD-10) for 1990–1998 and 1999–2006 data, respectively.8,9
We analyzed the 1990 to 2006 U.S. MCOD data files, which were derived from death certificate information.10 TB-related death was defined as all observations that assigned any of the following ICD codes as either an underlying COD or a contributing COD: ICD-9 codes of 010-018 (TB), 137 (late effect of TB), and 647.3 (TB complicating pregnancy, childbirth, or the puerperium) or ICD-10 codes of A15-A19 (TB), B90 (sequelae of TB), J65 (pneumoconiosis associated with TB), and O98.0 (TB complicating pregnancy, childbirth, and the puerperium). Other mycobacteria-related deaths, such as those caused by non-tuberculous mycobacteria, were not included in the analyses.
We calculated mortality rates using bridged-race population estimates—an estimate by the NCHS to allow varying multiple-race categories from different data collection systems to be more comparable—from the U.S. Census Bureau for years 1990 through 2006.11,12 Variables included in the analysis were age, gender, race/ethnicity, year of death, and place of birth. Race/ethnicity was categorized as non-Hispanic white (white), Hispanic, Asian/Pacific Islander (Asian), non-Hispanic black (black), and American Indian/Alaska Native (Native American). Age at death was grouped into people aged <1, 1–4, 5–14, 15–24, 25–34, 35–44, 45–54, 55–64, 65–74, 75–84, and ≥85 years. Anyone born in the U.S. or its associated jurisdictions was classified as U.S.-born. People not meeting this definition were considered foreign-born. Information on place of birth was not available for the years 2005 and 2006.
We calculated age-specific TB-related mortality rates and 95% confidence intervals (CIs) for each age group. Age-adjusted rates and rate ratios (RRs) were standardized to the year 2000 U.S. population by gender and race/ethnicity. Temporal trends were modeled by Poisson regression analysis. Premature mortality was measured for all deaths as years of potential life lost (YPLL) before 75 years of age. To assess comorbid conditions, we matched TB-related deaths with randomly selected non-TB deaths on age, gender, and race/ethnicity from 1990 through 2006 and computed matched odds ratio (MOR) comparisons of selected comorbidities. Denominators for computing rates for foreign-born people were obtained from the U.S. Census population estimates.13–16 We assessed age-specific temporal changes by comparing TB-related deaths for the years 1990, 1995, 2000, and 2005. We used SAS® version 9.2 for all calculations.17
RESULTS
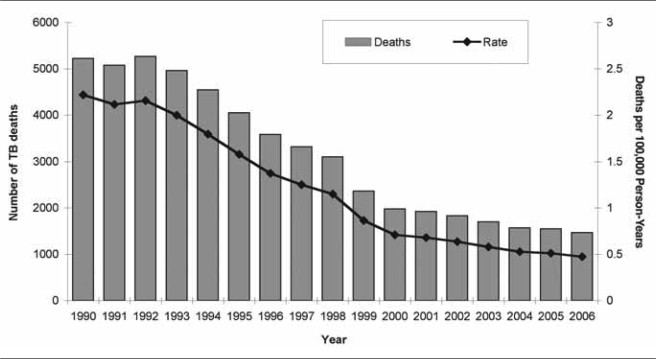
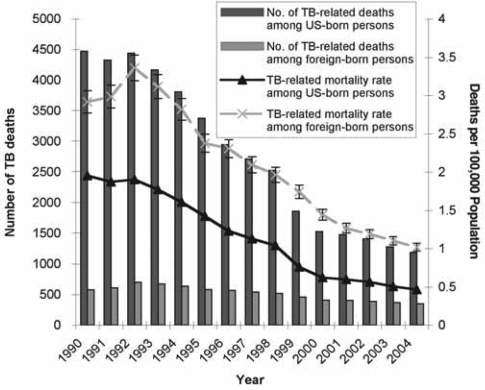
From 1990 through 2006, a total of 53,505 TB-related deaths were identified, comprising 0.13% of the 39,694,210 total deaths in the U.S. TB was reported as the underlying COD in 21,285 (39.8%) of these deaths and as one of the contributing causes in 32,220 deaths (60.2%). The age-adjusted mortality rate for TB declined from 2.22 per 100,000 person-years in 1990 (95% CI 2.16, 2.28; n=5,224) to 0.47 per 100,000 person-years in 2006 (95% CI 0.45, 0.50; n=1,468) with a combined overall mean annual mortality rate of 1.16 per 100,000 person-years (95% CI 1.15, 1.17; n=53,505). Poisson regression analysis demonstrated an annually declining temporal trend of 10.44% (95% CI 10.27, 10.60) in TB mortality, but the slope of the decline appeared to be leveling somewhat from the year 2000 forward (Figure 1).
Figure 1.
Number of TB-related deaths and age-adjusted mortality rates per 100,000 person-years by year, United States, 1990–2006
TB = tuberculosis
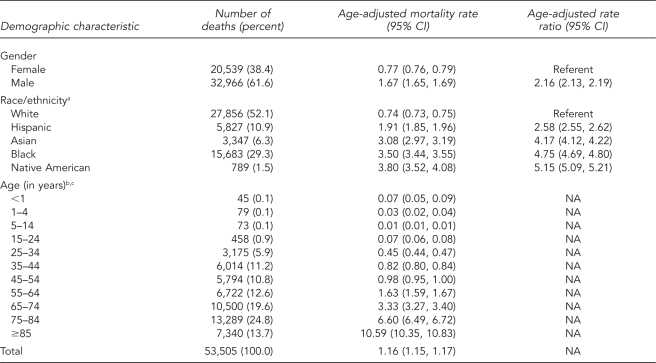
Men were more likely to experience TB-related deaths than women and were predominant among decedents (RR=2.16, 95% CI 2.13, 2.19) (Table 1). The declining trends over time in TB mortality rates for both genders were similar to that of the overall trend.
Table 1.
Age-adjusted TB-related mortality rates per 100,000 person-years and mortality rate ratios by gender, race/ethnicity, and age group, United States, 1990–2006
aRace/ethnicity was missing for three TB-related deaths.
bAge was missing for 16 TB-related deaths.
cMortality rates are age-specific rates, not age-adjusted rates.
TB = tuberculosis
CI = confidence interval
NA = not applicable
TB-related deaths among racial/ethnic groups demonstrated substantial disparities. Although the largest proportion of deaths was observed among white people (n=27,856, 52.1%), they had the lowest age-adjusted mortality rate (Table 1). Compared with white people, Native American (RR=5.15, 95% CI 5.09, 5.21), black (RR=4.75, 95% CI 4.69, 4.80), Asian (RR=4.17, 95% CI 4.12, 4.22), and Hispanic (RR=2.58, 95% CI 2.55, 2.62) people were more likely to experience TB-related death. When the study years were divided into early (1990–2000) and later (2001–2006) periods for comparison, TB-related mortality among Asian people (from RR=4.23, 95% CI 4.17, 4.28 in the early years to RR=5.88, 95% CI 5.71, 6.05 in the later years) and Native Americans (from RR=5.09, 95% CI 5.02, 5.16 in the early years to RR=6.87, 95% CI 6.68, 7.07 in the later years) increased relative to TB-related mortality among white people.
The mean age for TB decedents was 65 years (median = 69 years). TB was responsible for a total of 696,782 YPLL. The number of TB-related deaths increased with age and peaked at people aged 75–84 years (n=13,289, 24.8%); the highest age-specific mortality rate was observed among people aged 85 years and older at 10.59 per 100,000 person-years (95% CI 10.35, 10.83; n=7,340) (Table 1).
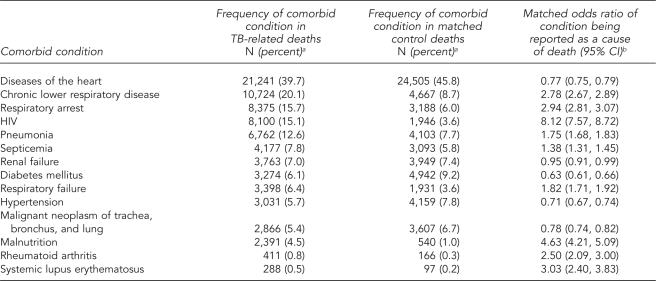
Several diseases/conditions were found to be associated with TB on the death certificate. After adjusting for age, gender, and race/ethnicity, HIV (MOR=8.12, 95% CI 7.57, 8.72) and malnutrition (MOR=4.63, 95% CI 4.21, 5.09) were more likely to be reported on a death certificate that included TB as a cause of death compared with a death certificate of a matched control subject (Table 2). Systemic lupus erythematosus (MOR=3.03, 95% CI 2.40, 3.83) and rheumatoid arthritis (MOR=2.50, 95% CI 2.09, 3.00) also demonstrated a positive association.
Table 2.
Frequency of selected comorbid causes of death and matched odds ratios comparing TB-related deaths with deaths from other conditions, United States, 1990–2006
aTotal n=53,486. Three TB-related deaths in people of undetermined race/ethnicity and 16 TB-related deaths in people of undetermined age were excluded from matched analyses.
bAdjusted for age, gender, and race/ethnicity
TB = tuberculosis
CI = confidence interval
HIV = human immunodeficiency virus
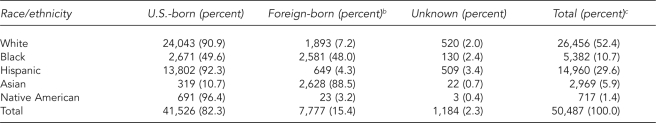
We identified 50,487 TB-related deaths from 1990 to 2004 (Table 3; as noted previously, 2005 and 2006 MCOD data did not contain place-of-birth information and so were excluded from the analysis). Of these, 7,777 (15.4%) deaths were among foreign-born people. The percentage of deaths accounted for by foreign-born people increased from 11.1% in 1990 to 22.3% in 2004 (Figure 2). When comparing mortality by place of birth, the majority of the deaths among white (n=24,043, 90.9%), Hispanic (n=13,802, 92.3%), and Native American (n=691, 96.4%) racial/ethnic groups were U.S.-born people. In contrast, the majority of the TB-related deaths among Asian people (n=2,628, 88.5%) and nearly half among black people (n=2,581, 48.0%) were foreign-born individuals. From 1990 through 2004, the number of TB-related deaths among U.S.-born people decreased by 73.5% (from 4,474 to 1,187) compared with a decrease of 39.7% (from 579 to 349) among foreign-born people (Figure 2). The TB-related mortality rate declined from 1.95 deaths per 100,000 population in 1990 (95% CI 1.90, 2.01; n=4,474) to 0.47 deaths per 100,000 population in 2004 (95% CI 0.44, 0.49; n=1,187) among U.S.-born people, and from 2.92 deaths per 100,000 population in 1990 (95% CI 2.68, 3.16; n=579) to 1.02 deaths per 100,000 population in 2004 (95% CI 0.91, 1.13; n=349) among foreign-born people.
Table 3.
Frequency of TB-related deaths by race/ethnicity and place of birth, United States, 1990–2004a
a2005 and 2006 multiple-cause-of-death data do not contain place-of-birth information and were excluded from the analysis.
bRace/ethnicity was missing for three foreign-born TB-related deaths.
cRow percentage
TB = tuberculosis
Figure 2.
Number of TB-related deaths in U.S.-born and foreign-born people by year, United States, 1990–2004a
a2005 and 2006 multiple-cause-of-death data do not contain place-of-birth information and were excluded from the analysis.
TB = tuberculosis
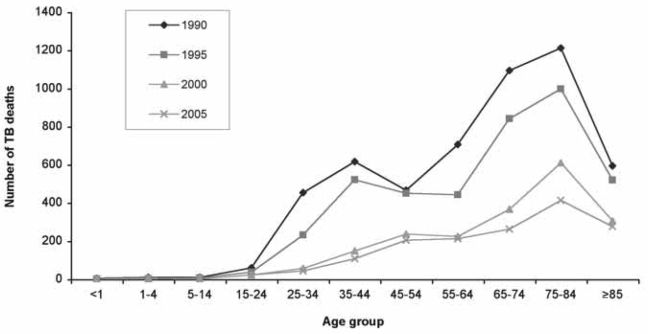
Figure 3 shows the frequency distribution of TB-related mortality by age group during four separate years: 1990, 1995, 2000, and 2005. The years 1990 and 1995 mark the AIDS epidemic era, and a bimodal age distribution curve, peaking at 35–44 and 75–84 years of age, is observed. By 2000, total TB-related deaths decreased by more than 50% from 1995 (from 4,050 to 1,978), and the peak previously observed at 35–44 years of age had diminished significantly. In 2005, the major change from 2000 was a decrease in the number of deaths in people aged 65–84 years (from 977 to 675); the curve is unimodal with a peak observed at 75–84 years of age (n=413). The total count of TB-related deaths in 2005 represented a 70% decrease from 1990 (from 5,223 to 1,550) and a 21% decrease from 2000 (from 4,050 to 1,550).
Figure 3.
Frequency distribution for TB-related deaths by age, United States, 1990, 1995, 2000, and 2005
TB = tuberculosis
DISCUSSION
The study findings indicate that TB-related mortality rates in the U.S. declined substantially from 1990 to 2006. Nevertheless, TB remains an important cause of preventable death in the U.S., resulting in more than 53,000 deaths throughout the study period. TB mortality rates were comparatively higher in males, ethnic minority groups, foreign-born people, and older people. Positive associations with HIV, malnutrition, and autoimmune conditions were observed.
Consistent with earlier findings, our data indicated significantly higher TB-related deaths among men than women throughout the 17-year study period, and these findings parallel previously reported gender disparities in TB incidence.4,5,18–21 Higher mortality among men may be, in part, explained by differences in initial exposure to TB infection, as men are at higher risk for TB infection and disease activation because of increased HIV prevalence—the strongest predisposing factor for TB.22,23 Other studies suggest that differences in notification rates, societal roles that may influence access to care, and/or lifestyle choices such as poor nutrition, smoking, and alcohol consumption between men and women may play a role in the observed epidemiologic differences.24
Racial/ethnic minority groups sustained a disproportionate burden of TB deaths during the study period. Although the greatest disparity was observed among Native Americans, black people experienced the greatest burden of deaths. Black people not only had the second highest mortality rate and RR, but also comprised nearly 30% of the total TB-related deaths for the study period, during which they represented approximately 12% of the total population. As racial disparities persistently appear in national TB incidence rates, elevated TB-related mortality rates most likely reflect increased incidence of TB disease among these groups.3 Socioeconomic status, specifically poverty and disparities in access to health care, may also explain the differences, especially concerning the need for urgent clinical management of fulminant TB disease.19
Differences in TB mortality were found in relation to place of birth as well. First, the TB-related mortality rate among U.S.-born and foreign-born people declined significantly from 1990 to 2004, but was persistently higher among foreign-born individuals. The percentage of TB-related mortalities accounted for by foreign-born people also doubled from 1990 to 2004, reflecting a similar trend in TB incidence.13 Second, the magnitude of association between a person's place of birth and TB-related deaths varied among racial/ethnic groups. For instance, foreign-born Asian people, whose number of TB-related deaths was nearly nine times that of U.S.-born Asian people, had the greatest disparity, also reflecting elevated TB incidence among these people. On the contrary, foreign-born Hispanic people only accounted for 4.3% of the total Hispanic TB-related deaths, while the proportion of their incident TB cases have been steadily rising from 55.4% in 1993 to 77.2% in 2007.3,13 Such findings suggest that, over time, if the foreign-born proportion of reported Hispanic incident TB cases continues to increase, then it is likely that the proportion of foreign-born Hispanic TB-related deaths will increase as well.
Increased susceptibility to infectious diseases as well as increased risk of activating latent TB infection in people with HIV/AIDS is widely recognized.25–27 Our data confirm such associations and also support previous studies that reported HIV/AIDS to be an important risk factor for both TB infection and disease.18,27,28 Similarly, decedents with autoimmune diseases, specifically rheumatologic diseases such as systemic lupus erythematosus and rheumatoid arthritis, had elevated MORs when compared with control subjects. This could be a result of the intrinsic immunosuppressive nature of the autoimmune diseases or the effect of therapeutic drug-induced immunosuppression on TB infection and disease activation.29 Although a positive disease association with malnutrition was expected, as numerous studies have shown malnutrition and poverty to be associated with TB susceptibility and death, one must be careful in assessing causality from these data because of inherit temporal ambiguity.19–21 While people with malnutrition may have a reduced immunological response, making them more susceptible to TB, it is also possible that TB disease itself leads to malnutrition. Our finding, which must be interpreted with caution, may indicate that although diabetes is a recognized risk factor for TB infection, it may not be a risk factor for severe infection and death. Alternatively, our results may be a spurious finding resulting from errors in coding.
When examining temporal changes specific for age groups, a bimodal peak that included younger age groups disappears after 1995. This observation may have been the result of more intense TB and HIV control efforts, including the introduction of highly active antiretroviral therapy in late 1995, as such therapy and subsequent immune reconstitution reduce the likelihood of TB infection, activation, and death.30 The findings also serve as a follow-up to a previous study by Braun et al. that showed the emergence of bimodal age distribution from 1980 to 1990.7 In addition, the fact that more than half of the deaths were observed in people aged 65 years or older compared with approximately 21% of reported TB incident cases in the respective age groups raises public health concerns for elderly populations, given the aging of the American population.13,31 As higher mortality among older people may be attributed to a greater prior exposure and age-related decreases in immune response, which may trigger subsequent development of active disease from latent TB infection, public health interventions aimed at older people, who disproportionately suffer from greater numbers of comorbid illnesses, will be necessary.32
Limitations
The primary strength of this study was the population-based nature of the data. However, several limitations exist in studies based on death certificate data; therefore, findings must be interpreted with caution. Misclassification of variables, including CODs, may occur. A previous study in New York City in 1992 found that 66% (n=206) of 310 people who died with active TB had no mention of TB on the death certificate.33 Such an error would tend to underestimate the true magnitude of the TB mortality burden, and our findings should be viewed as minimum estimates. Furthermore, death certificate data cannot distinguish between people who die with and people who die from TB because a clinician who knows that a decedent had TB may be likely to consider it an immediate or underlying COD, even if it is not.
Changes in coding to ICD-10 in 1999 from ICD-9 also suggest that our findings, particularly trends, must be viewed with caution. Demographic information on death certificates and in the census data are subject to bias and error resulting from problems of reporting, classification, and coverage. This issue is especially true for the minority population groups such as Native American, Hispanic, and Asian, as well as foreign-born individuals. Generally, misclassification of deaths (numerator data) results in an underestimation in the death rates, while the undercount of population (denominator data) tends to overestimate the rates. Reporting of country of origin may also be inaccurate and bias the mortality comparisons made between U.S.-born and foreign-born people.
CONCLUSIONS
The results of our study provide information on the burden of TB-related mortality that can assist in shaping more effective TB control and prevention programs. As certain groups including foreign-born Asian, Hispanic, black, and Native American people, as well as people with HIV and autoimmune diseases, exhibit disproportionately higher TB-related mortality, enhanced prevention efforts, active case-finding, early and adequate treatment targeting these groups, and further investigations to determine whether the observed differences can be attributed solely to the documented higher incidence rate of active disease in these groups are warranted. The continued burden of TB-related mortality underscores the importance of current efforts to develop effective TB vaccines as well as improved treatment.34
Acknowledgments
The authors thank Matthew D. Redelings, Loren Lieb, and Alex Ho for their contributions to the analysis and interpretation of data for this study. The authors also thank Ike Song and William Kang for their editorial review. This work was supported by the Los Angeles County Department of Public Health and the Department of Preventive Medicine of the University of Southern California's Keck School of Medicine in Los Angeles, California.
REFERENCES
- 1.World Health Organization. 2008 global tuberculosis facts. Geneva: WHO; 2008. [Google Scholar]
- 2.Frieden TR, Sterling TR, Munsiff SS, Watt CJ, Dye C. Tuberculosis. Lancet. 2003;362:887–99. doi: 10.1016/S0140-6736(03)14333-4. [DOI] [PubMed] [Google Scholar]
- 3.Trends in tuberculosis—United States, 2007. MMWR Morb Mortal Wkly Rep. 2008;57(11):281–5. [PubMed] [Google Scholar]
- 4.Hansel NN, Merriman B, Haponik EF, Diette GB. Hospitalizations for tuberculosis in the United States in 2000: predictors of in-hospital mortality. Chest. 2004;126:1079–86. doi: 10.1378/chest.126.4.1079. [DOI] [PubMed] [Google Scholar]
- 5.Rao VK, Iademarco EP, Fraser VJ, Kollef MH. The impact of comorbidity on mortality following in-hospital diagnosis of tuberculosis. Chest. 1998;114:1244–52. doi: 10.1378/chest.114.5.1244. [DOI] [PubMed] [Google Scholar]
- 6.White MC, Portillo CJ. Tuberculosis mortality associated with AIDS and drug or alcohol abuse: analysis of multiple cause-of-death data. Public Health. 1996;110:185–9. doi: 10.1016/s0033-3506(96)80074-6. [DOI] [PubMed] [Google Scholar]
- 7.Braun MM, Cote TR, Rabkin CS. Trends in death with tuberculosis during the AIDS era. JAMA. 1993;269:2865–8. [PubMed] [Google Scholar]
- 8.World Health Organization. International classification of diseases, ninth revision. Geneva: WHO; 1980. [Google Scholar]
- 9.World Health Organization. International classification of diseases, 10th revision. Geneva: WHO; 1992. [Google Scholar]
- 10.National Center for Health Statistics (US) Data file documentations, multiple cause-of-death, 1990–2006 [machine readable data file and documentation, CD-ROM Series 20] Hyattsville (MD): NCHS; 2008. [Google Scholar]
- 11.National Center for Health Statistics (US); Census Bureau with support from the National Cancer Institute. Bridged-race intercensal estimates of the July 1, 1990–July 1, 1999, United States resident population by county, single-year of age, sex, race, and Hispanic origin, prepared by the U.S. [cited 2008 Jan 5]. Available from: URL: http://www.cdc.gov/nchs/about/major/dvs/popbridge/popbridge.htm.
- 12.National Center for Health Statistics (US) Estimates of the July 1, 2000–July 1, 2006, United States resident population from the vintage 2006 postcensal series by year, county, age, sex, race, and Hispanic origin, prepared under a collaborative arrangement with the U.S. Census Bureau. [cited 2008 Jan 5]. Available from: URL: http://www.cdc.gov/nchs/about/major/dvs/popbridge/popbridge.htm.
- 13.Centers for Disease Control and Prevention (US) Reported tuberculosis in the United States, 2007. Atlanta: CDC; 2008. Sep, [Google Scholar]
- 14.Census Bureau (US) Quarterly estimates of the United States foreign-born and native resident population: April 1, 1990, to July 1, 1999. Washington: Census Bureau; 2000. [cited 2009 Jul 21]. available from: URL: http://www.census.gov/popest/archives/1990s/nat-nativity-sum.txt. [Google Scholar]
- 15.Census Bureau (US) Annual estimates of the United States foreign-born and native resident populations. Washington: Census Bureau; 2008. [cited 2009 Jul 21]. Current population survey. Also available from: URL: http://www.census.gov/population/www/socdemo/foreign/datatbls.html. [Google Scholar]
- 16.Census Bureau (US) Annual estimates of the United States foreign-born and native resident populations. Washington: Census Bureau; 2008. [cited 2009 Jul 21]. Current population survey table creator. Also available from: URL: http://www.census.gov/hhes/www/cpstc/cps_table_creator.html. [Google Scholar]
- 17.SAS Institute, Inc. SAS®: Version 9.2. Cary (NC): SAS Institute, Inc.; 2008. [Google Scholar]
- 18.Rieder HL, Cauthen GM, Kelly GD, Bloch AB, Snider DE., Jr. Tuberculosis in the United States. JAMA. 1989;262:385–9. [PubMed] [Google Scholar]
- 19.McKenna MT, McCray E, Jones JL, Onorato IM, Castro KG. The fall after the rise: tuberculosis in the United States, 1991 through 1994. Am J Public Health. 1998;88:1059–63. doi: 10.2105/ajph.88.7.1059. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Cantwell MF, Snider DE, Jr, Cauthen GM, Onorato IM. Epidemiology of tuberculosis in the United States, 1985 through 1992. JAMA. 1994;272:535–9. [PubMed] [Google Scholar]
- 21.Bennett DE, Courval JM, Onorato I, Agerton T, Gibson JD, Lambert L, et al. Prevalence of tuberculosis infection in the United States population: the National Health and Nutrition Examination Survey, 1999–2000. Am J Resp Crit Care Med. 2008;177:348–55. doi: 10.1164/rccm.200701-057OC. [DOI] [PubMed] [Google Scholar]
- 22.Selwyn PA, Sckell BM, Alcabes P, Friedland GH, Klein RS, Schoenbaum EE. High risk of active tuberculosis in HIV-infected drug users with cutaneous anergy. JAMA. 1992;268:504–9. [PubMed] [Google Scholar]
- 23.Friedman LN, Williams MT, Singh TP, Frieden TR. Tuberculosis, AIDS, and death among substance abusers on welfare in New York City. N Engl J Med. 1996;334:828–33. doi: 10.1056/NEJM199603283341304. [DOI] [PubMed] [Google Scholar]
- 24.World Health Organization. Gender and tuberculosis. Geneva: WHO; 2002. [cited 2009 Jun 15]. Also available from: URL: http://www.who.int/gender/other_health/en/genderTB.pdf. [Google Scholar]
- 25.Burwen DR, Bloch AB, Griffin LD, Ciesielski CA, Stern HA, Onorato IM. National trends in the concurrence of tuberculosis and acquired immunodeficiency syndrome. Arch Intern Med. 1995;155:1281–6. [PubMed] [Google Scholar]
- 26.Markowitz N, Hansen NI, Hopewell PC, Glassroth J, Kvale PA, Mangura BT, et al. The Pulmonary Complications of HIV Infection Study Group. Incidence of tuberculosis in the United States among HIV-infected persons. Ann Intern Med. 1997;126:123–32. doi: 10.7326/0003-4819-126-2-199701150-00005. [DOI] [PubMed] [Google Scholar]
- 27.Barnes PF, Bloch AB, Davidson PT, Snider DE., Jr. Tuberculosis in patients with human immunodeficiency virus infection. N Engl J Med. 1991;324:1644–50. doi: 10.1056/NEJM199106063242307. [DOI] [PubMed] [Google Scholar]
- 28.Harries AD. Tuberculosis and human immunodeficiency virus infection in developing countries. Lancet. 1990;335:387–90. doi: 10.1016/0140-6736(90)90216-r. [DOI] [PubMed] [Google Scholar]
- 29.Franco-Paredes C, Diaz-Borjon A, Senger MA, Barragan L, Leonard M. The ever-expanding association between rheumatologic diseases and tuberculosis. Am J Med. 2006;119:470–7. doi: 10.1016/j.amjmed.2005.10.063. [DOI] [PubMed] [Google Scholar]
- 30.Albalak R, O'Brien RJ, Kammerer JS, O'Brien SM, Marks SM, Castro KG, et al. Trends in tuberculosis/human immunodeficiency virus comorbidity, United States, 1993–2004. Arch Intern Med. 2007;167:2443–52. doi: 10.1001/archinte.167.22.2443. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Trends in aging—United States and worldwide. MMWR Morb Mortal Wkly Rep. 2003;52(6):101–4. 106. [PubMed] [Google Scholar]
- 32.Frost WH. The age selection of mortality from tuberculosis in successive decades. Am J Hyg. 1939;30:91–6. doi: 10.1093/oxfordjournals.aje.a117343. [DOI] [PubMed] [Google Scholar]
- 33.Washko RM, Frieden TR. Tuberculosis surveillance using death certificate data, New York City, 1992. Public Health Rep. 1996;111:251–5. [PMC free article] [PubMed] [Google Scholar]
- 34.Hoft DF, Blazevic A, Abate G, Hanekom WA, Kaplan G, Soler JH, et al. A new recombinant bacille Calmette-Guerin vaccine safely induces significantly enhanced tuberculosis-specific immunity in human volunteers. J Infect Dis. 2008;198:1491–501. doi: 10.1086/592450. [DOI] [PMC free article] [PubMed] [Google Scholar]