Abstract
Background/objectives. To investigate the procedural and long-term outcome of primary percutaneous coronary intervention (PCI) in octogenarians with an acute myocardial infarction.
Methods. We performed a retrospective analysis of all consecutive octogenarian patients (n=98) with an acute myocardial infarction treated with primary PCI in the Catharina Hospital in the year 2006. We compared procedural results and outcome with a matched control group composed of non-octogenarians undergoing primary PCI. Follow-up period was one year.
Results. The initial success rate of PCI was similar in the two groups but short-term mortality was higher among the elderly patients: 30-day mortality 26.3 vs. 9.6%. Age-adjusted mortality between 30 days and one year was comparable in the two groups and similar to natural survival in the Netherlands. Octogenarians were less likely to have a normal left ventricular function during follow-up (48.3 vs. 66.7%). New York Heart Association (NYHA) class and recurrence rate of myocardial infarction was higher among octogenarians.
Conclusion. Technical success rate during primary PCI was as good for octogenarians as in younger patients, but 30-day mortality, though acceptable, was higher among the elderly. After 30 days, age-adjusted mortality was comparable in both groups. (Neth Heart J 2010;18:129–34.)
Keywords: Angioplasty, Transluminal, Percutaneous Coronary; Myocardial Infarction; Treatment Outcome
Ischaemic heart disease is a leading cause of death among patients all over the world.1 In general, age is a predictor of adverse events after acute coronary syndrome, including in-hospital and post-hospital mortality rates.2-4 Octogenarians constitute a fast growing group of cardiovascular patients, admitted for percutaneous coronary intervention (PCI).5-8 Elderly people frequently present with comorbid conditions and as a result have more adverse cardiac and noncardiac events, and increased early and late mortality compared with younger patients after PCI.5,9,10 Most studies have reported that older age is associated with decreased procedural success and/or increased in-hospital complications.8,10-18 In the elderly, coronary disease is diffuse and the vessels are more often severely calcified. Therefore, the procedure is often technically difficult.5,10,19,20 The presence of an acute or recent myocardial infarction substantially increases the risk of in-hospital death.10,21
Only limited data are available about the safety and efficacy of primary PCI in octogenarian patients with an acute myocardial infarction and most studies refer to selected patients, not to consecutive unselected patients. Largely for that reason, it is unclear whether the success rate of primary PCI is lower among the elderly.14,22 Some studies indicate a higher short- and long-term mortality and a higher complication rate,4,23-25 whereas others do not.22,26
The aim of this study is to analyse long-term outcome of primary PCI in octogenarians with an acute myocardial infarction more systematically. All octogenarians presenting in our hospital for myocardial infarction and undergoing primary PCI (the routine treatment in our hospital) were analysed and compared with a matched control population younger than 80 years.
Patients and methods
Primary PCI in the greater Eindhoven area and study population
The greater Eindhoven area has a population of 1.2 million people. In the area there is one interventional centre (the Catharina Hospital) and there are 11 referring centres. The care for patients with an acute myocardial infarction is performed in close cooperation with the ambulance services and the cardiologists in the referring hospitals. Patients suffering from myocardial infarction are either transported directly to the Catharina Hospital after the ambulance personal establish the diagnosis, or indirectly via one of the referring hospitals. Primary PCI is the routine treatment for these patients. A total of approximately 1300 primary PCIs are performed per year and from epidemiological data it is estimated that more than 90% of all patients in the area undergoing myocardial infarction are actually admitted and initially treated in the Catharina Hospital (the incidence of acute myocardial infarction in the Netherlands is 1:1000 per year). This means that almost all patients undergoing acute myocardial infarction are diagnosed and treated according to these standards and are analysable for outcome and follow-up. It also means that the octogenarians as a group in this study represent the average octogenarian with an acute myocardial infarction in the Netherlands and not just a selected subgroup.
In the year 2006, 1283 primary PCIs were performed in patients with an acute myocardial infarction. Among this group there were 98 octogenarians. This complete consecutive group was the primary study population. A matched control group was made of all patients below the age of 80 presenting with an acute myocardial infarction and undergoing primary PCI next to an octogenarian. In this way, we created a control group of similar size to the octogenarian group while the only differences were age and age-related conditions.
Intervention
Standard techniques for primary PCI and stent implantation were used, either the femoral or the radial approach. Also standard medical treatment was used according to present guidelines.27 Generally, choice of stents and adjunctive treatment by glycoprotein IIb/IIIa antagonists was left to the opinion of the attending cardiologist. Intra-aortic balloon counterpulsation was used when clinically indicated. Treatment after PCI was according to standard routine and consisted at least of aspirin and clopidogrel as well β-blockade and ACE inhibition in the majority of patients.
In general, after admission to our hospital the ambulance waits until the primary PCI is performed, after which the patient is immediately transported to the referring hospital nearest to where the patient is living. As a consequence, further medical treatment was performed in the referring hospital in the place of residence of the patient.
Follow-up
Follow-up was performed by contacting the treating cardiologist from the referring centres where the patients received their medical follow-up controls and by telephoning the patients when required. The primary outcome measures were technical success rate of PCI, and 30-day and one-year survival. Secondary endpoints were left ventricular function, New York Heart Association (NYHA) class, recurrent myocardial infarction or PCI and coronary artery bypass grafting (CABG) after 30 days and one year.
Statistical analysis
The data are presented as mean ± standard deviation for continuous data or as counts. Continuous data were compared using the Student’s t-test, whereas categorical data were compared using the Χ2 test or Fisher’s exact test.
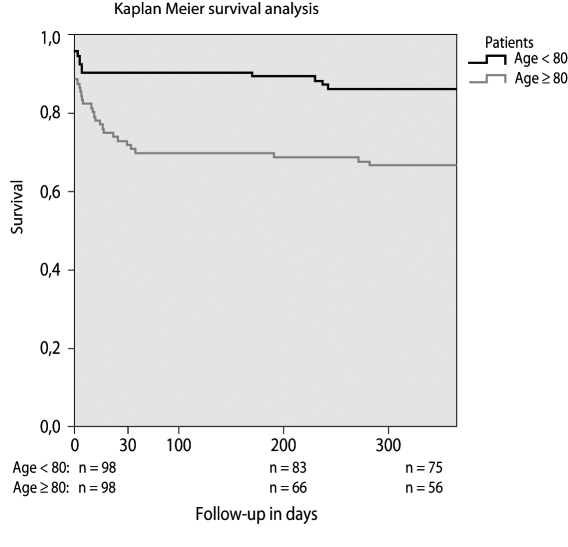
Thirty-day and one-year survival is presented in Kaplan-Meier curves. To investigate the influence of confounding variables a Cox proportional hazard model was used to test association between mortality and these variables. A p value of <0.05 was considered to be statistically significant. Data analysis was performed on an intention-to-treat basis, and was analysed in SPSS software (Version 15.0, SPSS inc., Chicago, Illinois).
Results
Baseline characteristics and procedural results
The total number of patients undergoing acute PCI in the Catharina Hospital in the year 2006 was 1283. There were 98 patients aged ≥80 years and we made a matched control group of 98 patients aged <80 years as defined in the methods. The mean age in the octogenarian group was 83.5 (±3.4) years with a range of 80 to 97 years, and 57.2 (±11.7) years in the control group, with a range of 29 to 78 years. Baseline characteristics are listed in table 1. Elderly patients were more likely to be women (53.1 vs. 23.5%; p<0.001) and to have had a prior cerebrovascular accident (14.7 vs. 5.3%; p=0.03). Also diabetes was more common among the elderly (26.3 vs. 10.6%; p=0.01).
Table 1.
Baseline characteristics.
| Variable | Age group | P value | |
|---|---|---|---|
| ≥80 (n=98) | <80 (n=98) | ||
| Median age | 83.5±3.4 | 57.2±11.7 | |
| Women | 52 (53.1) | 23 (23.5) | <0.001 |
| Diabetes mellitus | 25 (26.3) | 10 (10.6) | 0.01 |
| Previous CVA | 14 (14.7) | 5 (5.3) | 0.03 |
| Hypertension | 40 (42.1) | 33 (35.1) | 0.32 |
| Peripheral vascular disease | 6 (6.3) | 6 (6.3) | 0.99 |
| COPD | 8 (8.4) | 8 (8.5) | 0.98 |
| Current or prior malignancy | 10 (10.5) | 6 (6.4) | 0.31 |
| Renal impairment | 2 (2.1) | 3 (3.2) | 0.68 |
| Previous MI | 24 (25) | 13 (13.8) | 0.05 |
| Previous PCI | 10 (10.4) | 12 (12.8) | 0.61 |
| Previous CABG | 4 (4.2) | 3 (3.2) | 1.00 |
Values are presented as numbers (%) or mean ± SD. CVA=cerebrovascular accident, COPD=chronic obstructive pulmonary disease, MI=myocardial infarction, PCI=percutaneous coronary intervention, CABG=coronary artery bypass grafting. Renal impairment=creatinine ≥150 μmol/l.
Procedural characteristics are listed in table 2. The mean onset of pain to arrival time was similar in both groups (194 vs. 196 minutes). The arrival to reperfusion time (‘door to balloon’) was slightly longer in octogenarians (20 vs. 16 minutes), however it did not reach the level of significance (p=0.10). Procedural success rate was equal between the two groups (89 vs. 89%). Postprocedural TIMI flow was not different between the two groups either. Younger patients more often received a drug-eluting stent (17.3 vs. 38.1%; p<0.001). Patients aged over 80 years were more likely to receive a bare metal stent (67.3 vs. 51.0%; p=0.02). Younger patients were more likely to receive glycoprotein IIb/IIIa inhibitors compared with octogenarians (19.4 vs. 33.7%; p=0.02). In six patients in the octogenarian group and four patients in the non-octogenarian group, no intervention was performed, because the patient had died before the actual intervention could be performed, the operator was unable to reach the stenosis, or the smallest balloon could not pass the stenosis. According to the intention-to-treat principle, these patients are included in the analysis. Periprocedural mortality (table 3) was not significantly different between the groups (4.1 vs. 2.0%; p=0.68).
Table 2 .
Procedural characteristics.
| Variable | Age group | P value | |
|---|---|---|---|
| ≥80 (n=98) | <80 (n=98) | ||
| Onset-arrival time (min) | 194*±108 | 196†±148 | 0.94 |
| Arrival-reperfusion time (min) | 20‡±10.5 | 16§±8.3 | 0.10 |
| Cardiogenic shock | 18 (18.4) | 11 (11.2) | 0.16 |
| Respiratory support | 11 (11.2) | 10 (10.2) | 0.82 |
| Anterior wall infarction | 52 (53.1) | 44 (44.9) | 0.25 |
| Coronary artery | |||
| - Left main | 1 (1.0) | 2 (2.0) | 1.00 |
| - LAD | 50 (51.0) | 43 (43.9) | 0.32 |
| - LCX | 11 (11.2) | 8 (8.2) | 0.47 |
| - RCA | 33 (33.7) | 45 (45.9) | 0.08 |
| Vein graft | 1 (1.0) | 0 (0) | 1.00 |
| Balloon dilatation only | 9 (9.2) | 5 (5.1) | 0.27 |
| No intervention | 6 (6.1) | 4 (4.1) | 0.52 |
| Number of stents used | 1.4±0.7 | 1.4±0.8 | 0.93 |
| - 1 | 59 (60.2) | 66 (67.3) | 0.30 |
| - 2 | 16 (16.3) | 15 (15.3) | 0.85 |
| - 3 | 4 (4.1) | 4 (4.1) | |
| - ≥ 4 | 3 (3.1) | 2 (2.0) | 1.00 |
| DES | 17 (17.3) | 37(38.1) | <0.001 |
| BMS | 66 (67.3) | 50(51.0) | 0.02 |
| DES + BMS | 0 (0) | 2 (2.0) | 0.50 |
| Successful PCI | 89 | 89 | |
| Postprocedural TIMI flow | 2.5±0.9 | 2.7±0.8 | 0.22 |
| - 0 | 8 (8.2) | 7 (7.1) | 0.79 |
| - 1 | 4 (4.1) | 2 (2.0) | 0.68 |
| - 2 | 14 (14.3) | 6 (6.1) | 0.06 |
| - 3 | 72 (73.5) | 83 (84.7) | 0.05 |
| IABP | 3 (3.1) | 7 (7.1) | 0.33 |
| Glycoprotein IIb/IIIa antagonists | 19 (19.4) | 33 (33.7) | 0.02 |
Values are presented as numbers (%) or mean ± SD. * Data available for 45 patients, † Data available for 59 patients, ‡ Data available for 22 patients, § Data available for 36 patients, LAD=left anterior descending artery, LCX=left circumflex artery, RCA=right coronary artery, DES=drug-eluting stent, BMS=bare metal stent, PCI=percutaneous coronary intervention, TIMI= Thrombolysis in Myocardial Infarction, IABP=intra-aortic balloon pump.
Table 3 .
Cumulative and additive mortality data of octogenarians and non-octogenarians.
| Variable | Age group | P value | |
|---|---|---|---|
| ≥80 (n=98) | <80 (n=98) | ||
| Death during procedure | 4 (4.1) | 2 (2.0) | 0.68 |
| Death during hospital stay | 12 (12.2) | 5 (5.1) | 0.07 |
| Cumulative mortality rate <30 days | 25 (26.3) | 9 (9.6) | 0.003 |
| Cumulative mortality rate <1 year | 34 (35.8) | 13 (13.8) | <0.001 |
| Additive mortality between 30 days and 1 year | 9 (9.5) | 4 (4.3) | 0.16 |
| Cardiac cause of death | 29 of 34 | 10 of 13 | 0.67 |
Values are presented as numbers (%).
Follow-up
Mortality data are listed in table 3. In-hospital mortality was not significantly higher among the elderly (12.2 vs. 5.1%; p=0.07). In contrast, overall 30-day mortality was higher among the elderly (26.3 vs. 9.6%; p=0.003). Cumulative mortality over one year is also significantly higher among octogenarians (35.8 vs. 13.8%; p<0.001). However, when looking at the additional age-adjusted mortality between 30 days and one year, this is not significantly higher among octogenarian patients (9.5 vs. 4.3%; p=0.16). So the higher one-year mortality is fully accounted for by the higher 30-day mortality. The proportion of patients who died of a cardiac cause was similar in both groups (29 out of 34 vs. 10 out of 13; p=0.67). Kaplan-Meier survival curves are shown in figure 1.
Figure 1 .
Kaplan-Meier survival analysis.
The Cox proportional hazards model was used to identify independent predictors of 30-day and one-year mortality. Results are shown in table 4. The most explicit predictor of 30-day as well as one-year mortality is cardiogenic shock at initial admission (present in 18 octogenarians vs. 11 non-octogenarians). Moreover, age and post-procedural TIMI flow <3 were independent predictors of mortality at 30 days and one year. The hazard ratio for octogenarians for 30-day and one-year mortality after primary PCI compared with non-octogenarians was 2.74 and 2.64.
Table 4.
Independent predictors of 30-day and one-year mortality at multivariate analysis.
| Variable |
Hazard ratio (95% CI) |
P value |
|---|---|---|
| 30 days | ||
| Shock | 9.83 (4.91-19.66) | <0.001 |
| Postprocedural TIMI flow <3 | 4.67 (2.36-9.26) | <0.001 |
| Age ≥80 years | 2.74 (1.27-5.90) | 0.01 |
| One year | ||
| Shock | 4.84 (2.77-8.44) | <0.001 |
| Prior or current malignancy | 3.74 (1.96-7.13) | <0.001 |
| Postprocedural TIMI flow <3 | 3.06 (1.79-5.22) | <0.001 |
| Age ≥80 years | 2.64 (1.50-4.76) | 0.001 |
CI=confidence interval. TIMI=Thrombolysis in Myocardial Infarction.
At one-year follow-up normal left ventricular function was less frequent in octogenarians compared with non-octogenarians (48.3 vs. 66.7%; p=0.03). Mean NYHA class is significantly higher among the elderly (1.9 vs. 1.3; p<0.001). Moreover, a higher proportion of the octogenarians experienced a recurrent myocardial infarction (20.5 vs. 9.4%; p=0.046). The other variables determined at follow-up (re-PCI and CABG) were not significantly different between the two groups.
Discussion
This study performed in an unselected, consecutive and complete cohort of octogenarians and a matched control group revealed similar procedural success rates of primary PCI between octogenarians and younger patients. However, the octogenarians had a significantly higher 30-day mortality. Once the first 30 days are over, the additional age-adjusted mortality is not higher than in the younger patients.
Older patients present with more comorbidity and more generalised atherosclerotic disease, which is age-related. PCI is therefore more challenging from the technical point of view. Nevertheless, success rates of PCI with TIMI 3 flow and arrival to reperfusion time are not different from the younger population, which is consistent with findings in other studies.14,26,28 Therefore, this study supports the standpoint that primary PCI should not be withheld based on age alone.
What is remarkable is the onset of pain to arrival time which is equal in both groups. The expectation was that elderly patients would have a longer delay, as found by Guagliumi et al. The opposite finding in this study can possibly be explained by the fact that elderly patients frequently have a history of cardiac disease and are used to medical care, and therefore are taken more seriously when having symptoms and calling for medical attention. Secondly they often live in nursing homes with fast access to healthcare. Also, the unique system in the Eindhoven area with triage by the ambulance and fast transport of patients to the heart centre without routine intervention of a local hospital can explain these findings.
Mortality among octogenarians is higher in the first 30 days of follow-up. This is only partially explained by the fact that more of the elderly patients are in shock when they arrive at the hospital (slightly, but not significantly more common in the octogenarians). Multivariate analysis showed shock to be an independent risk factor with a hazard ratio of 9.83. However, age in itself is also a significant predictor of 30-day mortality, as also found in previous studies.14,26 Between discharge from hospital and 30 days, the mortality among the elderly is high, which might be reduced by prolonging the hospital stay. Looking at the additional mortality between 30 days and one year this is not significantly higher among octogenarians and is similar to age-adjusted mortality of patients aged 83.5 years in the Netherlands: 8.9% in one year (according to the Dutch Central Bureau of Statistics, Voorburg/Heerlen).
Our study is unique among studies investigating the outcome of primary PCI in octogenarians because it can be assumed on demographic grounds that (almost) all patients with an acute myocardial infarction were actually referred to our hospital and all of them were treated (or attempted to be treated) by primary PCI. Therefore our study reflects the outcome of primary PCI in average octogenarians, not in a selected group of patients. As far as we know, this degree of representativeness has not been achieved in any previous studies.
Study limitations
Our study has several limitations. In the first place, our study only analyses outcome of primary PCI as treatment for acute myocardial infarction in the octogenarians, and thus did not compare primary PCI with other treatment modalities. This is due to the policy in the greater Eindhoven area to perform primary PCI as first-line treatment for acute myocardial infarction, also for octogenarians. This policy is based upon previous studies comparing primary PCI with medical therapy in this group of patients showing the advantage of primary PCI. Secondly, the design of the study in itself was prohibitive of a true control group. Therefore, a matched control group was chosen. Because age was the only criterion decisive for the assignment of a patient to the study group or the control group, it can be assumed that all other baseline differences and differences in outcome were merely a result of the older age and are not related to any other bias. Therefore, we believe that this study design was valid to analyse the outcome of primary PCI in octogenarians compared with non-octogenarians. In the third place, follow-up in our study was only one year. But given the fact that after 30 days there was no longer any excess mortality for up to one year, it is justified to conclude that primary PCI in octogenarians is associated with a higher mortality in the short term, but once the 30-days period is over, age-adjusted mortality is not higher than in younger patients. Finally, this study is a retrospective analysis, and therefore subject to the limitations of any such analysis, but it is complete and included almost all octogenarians with an acute myocardial infarction during the year 2006.
Conclusion
Our study demonstrates that primary PCI in octogenarians has a high technical and procedural success rate, but is associated with a significantly higher 30-day mortality compared with younger patients. Independent risk factors for 30-day mortality are shock, postprocedural TIMI flow less than 3 and age ≥80 years. Age-adjusted mortality after the first 30 days is not higher than in younger patients.
Acknowledgements
We wish to thank all the referring hospitals for their contribution in collecting follow-up data: Maxima Medical Centre Eindhoven, Maxima Medical Centre Veldhoven, Tweesteden Hospital Tilburg, St Elisabeth Hospital Tilburg, VieCurie Hospital Venlo, Laurentius Hospital Roermond, Jeroen Bosch Hospital Den Bosch, St Maartens Gasthuis Weert, Bernhoven Hospital Oss, St Anna Hospital Geldrop, Elkerliek Hospital Helmond.
References
- 1.Murray CJ, Lopez AD. Mortality by cause for eight regions of the world: Global Burden of Disease Study. Lancet. 1997;349:1269-76. [DOI] [PubMed] [Google Scholar]
- 2.Boersma E, Pieper KS, Steyerberg EW, Wilcox RG, Chang WC, Lee KL, et al. Predictors of outcome in patients with acute coronary syndromes without persistent ST-segment elevation. Results from an international trial of 9461 patients. The PURSUIT Investigators. Circulation. 2000;101:2557-67. [DOI] [PubMed] [Google Scholar]
- 3.Eagle KA, Lim MJ, Dabbous OH, Pieper KS, Goldberg RJ, Van de Werf, et al. A validated prediction model for all forms of acute coronary syndrome: estimating the risk of 6-month postdischarge death in an international registry. JAMA. 2004;291:2727-33. [DOI] [PubMed] [Google Scholar]
- 4.Granger CB, Goldberg RJ, Dabbous O, Pieper KS, Eagle KA, Cannon CP, et al. Predictors of hospital mortality in the global registry of acute coronary events. Arch Intern Med. 2003;163:2345-53. [DOI] [PubMed] [Google Scholar]
- 5.Graham MM, Ghali WA, Faris PD, Galbraith PD, Norris CM, Knudtson ML. Survival after coronary revascularization in the elderly. Circulation. 2002;105:2378-84. [DOI] [PubMed] [Google Scholar]
- 6.Hassani SE, Wolfram RM, Kuchulakanti PK, Xue Z, Gevorkian N, Suddath WO, et al. Percutaneous coronary intervention with drug-eluting stents in octogenarians: characteristics, clinical presentation, and outcomes. Catheter Cardiovasc Interv. 2006;68:36-43. [DOI] [PubMed] [Google Scholar]
- 7.Peterson ED, Alexander KP, Malenka DJ, Hannan EL, O'Conner GT, McCallister BD, et al. Multicenter experience in revascularization of very elderly patients. Am Heart J. 2004;148:486-92. [DOI] [PubMed] [Google Scholar]
- 8.Thompson RC, Holmes DR, Jr., Grill DE, Mock MB, Bailey KR. Changing outcome of angioplasty in the elderly. J Am Coll Cardiol. 1996;27:8-14. [DOI] [PubMed] [Google Scholar]
- 9.Barakat K, Wilkinson P, Deaner A, Fluck D, Ranjadayalan K, Timmis A. How should age affect management of acute myocardial infarction? A prospective cohort study. Lancet. 1999;353:955-9. [DOI] [PubMed] [Google Scholar]
- 10.Batchelor WB, Anstrom KJ, Muhlbaier LH, Grosswald R, Weintraub WS, O'Neill WW, et al. Contemporary outcome trends in the elderly undergoing percutaneous coronary interventions: results in 7,472 octogenarians. National Cardiovascular Network Collaboration. J Am Coll Cardiol. 2000;36:723-30. [DOI] [PubMed] [Google Scholar]
- 11.Abizaid AS, Mintz GS, Abizaid A, Saucedo JF, Mehran R, Pichard AD, et al. Influence of patient age on acute and late clinical outcomes following Palmaz-Schatz coronary stent implantation. Am J Cardiol. 2000;85:338-43. [DOI] [PubMed] [Google Scholar]
- 12.Alfonso F, Azcona L, Perez-Vizcayno MJ, Hernandez R, Goicolea J, Fernandez-Ortiz A, et al. Initial results and long-term clinical and angiographic implications of coronary stenting in elderly patients. Am J Cardiol. 1999;83:1483-7, A7. [DOI] [PubMed] [Google Scholar]
- 13.De Gregorio J, Kobayashi Y, Albiero R, Reimers B, Di Mario C, Finci L, et al. Coronary artery stenting in the elderly: short-term outcome and long-term angiographic and clinical follow-up. J Am Coll Cardiol. 1998;32:577-83. [DOI] [PubMed] [Google Scholar]
- 14.Guagliumi G, Stone GW, Cox DA, Stuckey T, Tcheng JE, Turco M, et al. Outcome in elderly patients undergoing primary coronary intervention for acute myocardial infarction: results from the Controlled Abciximab and Device Investigation to Lower Late Angioplasty Complications (CADILLAC) trial. Circulation. 2004;110:1598-604. [DOI] [PubMed] [Google Scholar]
- 15.Matetzky S, Sharir T, Noc M, Domingo M, Chyu K, Kar S, et al. Primary angioplasty for acute myocardial infarction in octogenarians. Am J Cardiol. 2001;88:680-3. [DOI] [PubMed] [Google Scholar]
- 16.Singh M, Mathew V, Garratt KN, Berger PB, Grill DE, Bell MR, et al. Effect of age on the outcome of angioplasty for acute myocardial infarction among patients treated at the Mayo Clinic. Am J Med. 2000;108:187-92. [DOI] [PubMed] [Google Scholar]
- 17.Taddei CF, Weintraub WS, Douglas JS, Jr., Ghazzal Z, Mahoney E, Thompson T, et al. Influence of age on outcome after percutaneous transluminal coronary angioplasty. Am J Cardiol. 1999;84:245-51. [DOI] [PubMed] [Google Scholar]
- 18.Wennberg DE, Makenka DJ, Sengupta A, Lucas FL, Vaitkus PT, Quinton H, et al. Percutaneous transluminal coronary angioplasty in the elderly: epidemiology, clinical risk factors, and in-hospital outcomes. The Northern New England Cardiovascular Disease Study Group. Am Heart J. 1999;137:639-45. [DOI] [PubMed] [Google Scholar]
- 19.Weintraub WS, Veledar E, Thompson T, Burnette J, Jurkovitz C, Mahoney E. Percutaneous coronary intervention outcomes in octogenarians during the stent era (National Cardiovascular Network). Am J Cardiol. 2001;88:1407-10, A6. [DOI] [PubMed] [Google Scholar]
- 20.Cohen HA, Williams DO, Holmes DR, Jr., Selzer F, Kip KE, Johnston JM, et al. Impact of age on procedural and 1-year outcome in percutaneous transluminal coronary angioplasty: a report from the NHLBI Dynamic Registry. Am Heart J. 2003;146:513-9. [DOI] [PubMed] [Google Scholar]
- 21.Klein LW, Block P, Brindis RG, McKay CR, McCallister BD, Wolk M, et al. Percutaneous coronary interventions in octogenarians in the American College of Cardiology-National Cardiovascular Data Registry: development of a nomogram predictive of in-hospital mortality. J Am Coll Cardiol. 2002;40:394-402. [DOI] [PubMed] [Google Scholar]
- 22.Wenaweser P, Ramser M, Windecker S, Lutolf I, Meier B, Seiler C, et al. Outcome of elderly patients undergoing primary percutaneous coronary intervention for acute ST-elevation myocardial infarction. Catheter Cardiovasc Interv. 2007;70:485-90. [DOI] [PubMed] [Google Scholar]
- 23.DeGeare VS, Stone GW, Grines L, Brodie BR, Cox DA, Garcia E, et al. Angiographic and clinical characteristics associated with increased in-hospital mortality in elderly patients with acute myocardial infarction undergoing percutaneous intervention (a pooled analysis of the primary angioplasty in myocardial infarction trials). Am J Cardiol. 2000;86:30-4. [DOI] [PubMed] [Google Scholar]
- 24.Feldman DN, Gade CL, Slotwiner AJ, Parikh M, Bergman G, Wong SC, et al. Comparison of outcomes of percutaneous coronary interventions in patients of three age groups (<60, 60 to 80, and >80 years) (from the New York State Angioplasty Registry). Am J Cardiol. 2006;98:1334-9. [DOI] [PubMed] [Google Scholar]
- 25.Teplitsky I, Assali A, Golovchiner G, Shor N, Weiss A, Battler A, et al. Acute and intermediate-term results of percutaneous coronary stenting in octogenarian patients. Int J Cardiovasc Intervent. 2003;5:195-9. [DOI] [PubMed] [Google Scholar]
- 26.Sakai K, Nakagawa Y, Soga Y, Ando K, Yokoi H, Iwabuchi M, et al. Comparison of 30-day outcomes in patients <75 years of age versus >or=75 years of age with acute myocardial infarction treated by primary coronary angioplasty. Am J Cardiol. 2006;98:1018-21. [DOI] [PubMed] [Google Scholar]
- 27.Silber S, Albertsson P, Aviles FF, Camici PG, Colombo A, Hamm C, et al. Guidelines for percutaneous coronary interventions. The Task Force for Percutaneous Coronary Interventions of the European Society of Cardiology. Eur Heart J. 2005;26:804-47. [DOI] [PubMed] [Google Scholar]
- 28.Migliorini A, Moschi G, Valenti R, Parodi G, Dovellini EV, Carrabba N, et al. Routine percutaneous coronary intervention in elderly patients with cardiogenic shock complicating acute myocardial infarction. Am Heart J. 2006;152:903-8. [DOI] [PubMed] [Google Scholar]