Abstract
OBJECTIVE: To determine the proportion of patients with noncardiac chest pain (NCCP) who see a gastroenterologist, the type and frequency of gastrointestinal (GI) and cardiac tests performed, and the frequency of cardiac death.
PATIENTS AND METHODS: A cohort of Olmsted County, Minnesota, residents presenting to the emergency department (ED) with chest pain between January 1, 1985, and December 31, 1992, was identified through the Rochester Epidemiology Project. We assessed the frequency of ED, cardiology, and gastroenterology visits and corresponding tests after a diagnosis of NCCP (n=320). We also assessed the frequency of cardiac events.
RESULTS: During follow-up, 49% of patients sought care in the ED, 42% had repeated cardiology evaluations, and 15% were seen by a gastroenterologist. Thirty-eight percent underwent esophagogastroduodenoscopy, but very few underwent manometry or a pH probe. Patients with NCCP of unknown origin had 3 times the rate of GI consultations as their counterparts with a GI disorder. Survival free of cardiac death in the subset with NCCP with a GI disorder was 90.2% at 10 years and 84.8% at 20 years, compared with 93.7% at 10 years and 88.1% at 20 years for the subset with NCCP of unknown origin.
CONCLUSION: The frequency of health care utilization in NCCP patients is high, but relatively few GI consultations and even fewer GI tests are performed. Patients dismissed from the hospital with NCCP continue to experience cardiac events, which may highlight a need for more aggressive cardiovascular risk factor management in this population.
The frequency of health care utilization in patients with noncardiac chest pain is high, but relatively few gastrointestinal consultations and even fewer gastrointestinal tests are performed; patients dismissed from the hospital with noncardiac chest pain continue to experience cardiac events.
CABG = coronary artery bypass graft; CI = confidence interval; ED = emergency department; EGD = esophagogastroduodenoscopy; GERD = gastroesophageal reflux disease; GI = gastrointestinal; MI = myocardial infarction; NCCP = noncardiac chest pain; NCCP-GI = NCCP secondary to GI diagnoses; NCCP-U = NCCP of unknown origin
In 2005, the American Heart Association estimated that 80 million Americans have cardiovascular disease.1 The magnitude of this number has impelled patients and physicians to consider acute chest pain as a harbinger for impending myocardial infarction (MI) and potential death. Along with heightened sensitivity to the evaluation of chest pain has come increasing evidence that a significant proportion of individuals with chest pain have noncardiac chest pain (NCCP).2 Noncardiac chest pain is defined by substernal chest pain in the absence of significant epicardial coronary artery stenoses. Previous population-based studies have reported the prevalence of this entity to be 23%.3
Noncardiac chest pain is attributed to a variety of disorders, including gastroesophageal reflux disease (GERD) and esophageal hypersensitivity,4 panic attack,5 musculoskeletal pain,6 and microvascular disease (cardiac syndrome X).7 GERD is the most prevalent cause of NCCP, accounting for up to 60% of cases.8-12 The prevalence of GERD in NCCP has been studied by pH monitoring and found to be 41% to 43%.13,14
The cost of evaluation of NCCP is estimated to be between $315 million and $1.8 billion per year.4,15 The economic impact is further illustrated by a hospital-based prospective study that reported more frequent health care visits by patients with NCCP than by those with ischemic heart disease.16 Therefore, determining whether subgroups of patients with NCCP use more health care resources than others is important.
For editorial comment, see page 309
Although it is thought that patients with NCCP have a good prognosis, there is a paucity of data to support this conclusion. A few studies report that patients with normal findings on coronary angiography have minimal cardiac morbidity and mortality.16,17 However, some studies point to increased cardiac mortality. A 16-year cohort study by Wilhelmsen et al18 found that men with nonspecific chest pain and normal findings on cardiac evaluation ultimately have high cardiovascular and noncardiovascular mortality rates. No large, long-term community studies have recorded the frequency of cardiac deaths that occur after a diagnosis of NCCP.
We identified patients with a diagnosis of NCCP to determine the frequency of gastrointestinal (GI) consultations and testing and to identify the frequency of cardiac death.
PATIENTS AND METHODS
This study was approved by the Mayo Clinic Institutional Review Board. The population, previously defined by Prina et al,19 was identified through the Rochester Epidemiology Project, which provides access to almost all records of medical care provided to Olmsted County residents for the past 90 years. Patients were older than 18 years, resided in Olmsted County, and presented with acute chest pain to one of the county's 3 emergency departments (EDs) between January 1, 1985, and December 31, 1992. Those who had an admission diagnosis of unstable angina, subsequent inpatient cardiac evaluation, and a dismissal diagnosis of NCCP were included for retrospective review. The Diamond classification was used to diagnose unstable angina: new onset or worsening pattern of ischemic chest pain, occurring at rest or with minimal exertion and alleviated by sublingual nitroglycerin, rest, or both.20 For all study patients, the diagnosis of NCCP was specified by the attending cardiologist at hospital dismissal. Within 1 week of the initial ED evaluation or hospital admission date, 105 (33%) of the patients underwent one or more of the following tests: angiography (n=48; 15%), resting echocardiography (n=38; 12%), stress echocardiography (n=5; 2%), and nuclear cardiology scan (n=38; 12%). Patients dismissed from the hospital with a diagnosis of chest pain related to coronary artery disease or specific cardiac diseases were excluded.
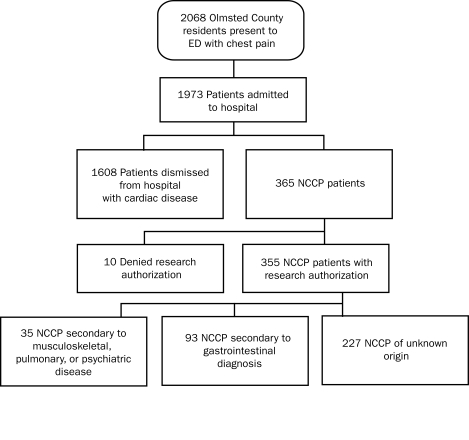
During the study period, 1973 patients were admitted from the ED with chest pain, and 365 patients (18%) were dismissed from the hospital with a diagnosis of NCCP. Of the 365 patients, 355 (97%) gave research authorization. These were further classified into a group of 227 patients (64%) with chest pain of unknown origin and a group of 128 patients (36%) with NCCP attributable to a specific diagnosis such as GERD, panic disorder, or pulmonary disease (Figure 1). This study focuses on patients with NCCP of unknown origin (NCCP-U; n=227) and NCCP secondary to GI diagnoses (NCCP-GI; n=93).
FIGURE 1.
Patient population. ED = emergency department; NCCP = noncardiac chest pain.
Data Collection
The complete medical records of 320 consenting patients (NCCP-U, n=227; NCCP-GI, n=93) were reviewed. For the initial 160 patients, complete paper and electronic records were used. Mayo Clinic's electronic record was introduced between 1993 and 1996, and a dual paper and electronic system was in existence through 2008. For the remaining 160 patients, only electronic documentation was used for abstraction. Records of all 320 patients were analyzed for mortality data and GI testing.
Baseline characteristics, including age, sex, Charlson comorbidity index, and prior cardiac and GI diagnoses, were recorded at ED presentation. The Charlson comorbidity index is a severity-weighted index of comorbid conditions.21 Follow-up visits to the ED, a cardiologist, or a gastroenterologist were noted between January 1993 and January 2003. Eighteen patients died before this period (5 of cardiac causes and 6 of noncardiac causes; the cause of death in the remaining 7 cases was unknown). Therefore, 302 patients are included in the analysis of the number of health care visits. Gastrointestinal tests were abstracted from the ED visit date through the last date of abstraction (varied from June 2005 to July 2006) and included esophagogastroduodenoscopy (EGD), 24-hour esophageal pH probe, and esophageal manometry. All death reports were abstracted through May 2006 with a focus on cardiac death as determined by the clinician's report. Autopsy reports were occasionally available to corroborate the clinician's report.
Statistical Analyses
Utilization summaries are provided as mean occurrences per 10 person-years of follow-up. The association of number of physician visits and diagnostic testing frequencies with dismissal diagnostic category (NCCP-U vs NCCP-GI group) was assessed using Poisson regression analyses. The natural logarithm of follow-up time was used as an offset in these models to account for differences in patient follow-up times. Rate ratios for physician visits and diagnostic tests in the NCCP-U group relative to the NCCP-GI group were calculated from model coefficients and adjusted for age and sex. For infrequently used diagnostic tests, Cox proportional hazards regression models were used to estimate hazard ratios for the initial occurrence of the diagnostic test in the NCCP-U group relative to the NCCP-GI group and adjusted for age and sex. The Cox models provide a better description of the relative risk for rare events.
Kaplan-Meier methodology was used to summarize overall survival for the NCCP-U and NCCP-GI subsets separately. An extension of the Kaplan-Meier method accounting for the competing risk of death from specific known and, separately, unknown causes was used to summarize survival free of cardiac death.22 Observed patient survival was compared with the 1950-2000 Minnesota white population survival using the Hakulinen cohort method with a log-rank test.23
Possible factors related to overall survival were investigated using Cox proportional hazards models. Those factors significant at the α=.05 level in univariate models were considered further for a multivariate model. A backward selection procedure was used to select factors retained in the final model.
To estimate an association of demographics and previous diagnoses with a diagnosis of GI-related or unexplained chest pain, we used 2-sample t tests or Fisher exact tests, as appropriate.
RESULTS
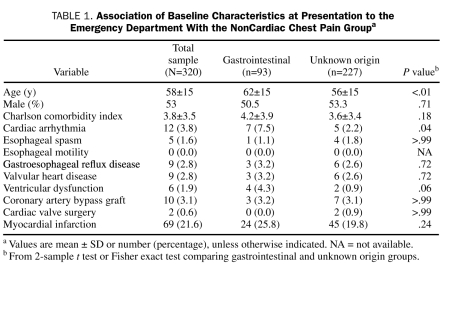
The sample was 53% male (n=168) and 96% white. Mean ± age was 58±15 years. Mean ± SD Charlson comorbidity index was 3.8±3.5 (Table 1). Specific preexisting medical diagnoses and demographics were analyzed to estimate associations with NCCP-GI vs NCCP-U. The NCCP-GI group was slightly older (P<.01) and had a higher proportion of cardiac arrhythmias (P=.04). These were the only statistically significant associations. Of note, 24 patients (26%) who had an NCCP-GI diagnosis had a history of MI compared with 45 patients (20%) in the NCCP-U cohort (P=.2). The NCCP-GI group had slightly increased rates of previous baseline cardiac events (including arrhythmia, valvular disease, ventricular dysfunction, and MI) and GERD, but these results were not statistically significant (Table 1).
TABLE 1.
Association of Baseline Characteristics at Presentation to the Emergency Department With the NonCardiac Chest Pain Groupa
Gastrointestinal diagnoses were made with a variety of tests, including EGD, ultrasonography, and computed tomography. In the NCCP-GI group, 35 patients (38%) were diagnosed as having GERD and 9 (10%) as having cholecystitis; the remaining 49 patients (53%) had miscellaneous diagnoses that included dyspepsia, peptic ulcer disease, biliary colic or cholelithiasis, choledocholithiasis, and a clinical diagnosis of esophageal spasm. Eighteen patients died before the health care visit utilization follow-up period began (January 1, 1993), and 72 additional patients died through May 2006. Health care utilization was tracked through January 1, 2003.
Physician Visits
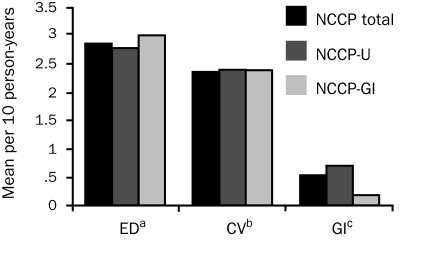
Summaries of visit and testing frequency are provided in Figures 2 and 3. Any individual patient could account for more than one physician visit or GI test. After hospital discharge, 49% of patients sought care in the ED (604 visits), 42% received cardiology consultations (562 visits), and 15% received gastroenterology consultations (164 visits). Utilization is reported in Figure 2 in mean visits per 10 person-years. Rate ratios, adjusted for age and sex, comparing the NCCP-U subset with the NCCP-GI subset for ED, cardiovascular, and GI visits were 0.9 (95% confidence interval [CI], 0.7-1.3; P=.8), 1.1 (95% CI, 0.7-1.7; P=.6), and 3.2 (95% CI, 1.4-7.2; P=.01), respectively.
FIGURE 2.
Subspecialty consultations and emergency department (ED) visits in patients with noncardiac chest pain (NCCP) (mean visits per 10 person-years). Rate ratios are adjusted for age and sex. CV = cardiovascular; GI = gastrointestinal; U = unknown.
a Rate ratio comparing NCCP-U vs NCCP-GI for ED visits: 0.9 (P=.8).
b Rate ratio comparing NCCP-U vs NCCP-GI for CV visits: 1.1 (P=.6).
c Rate ratio comparing NCCP-U vs NCCP-GI for GI visits: 3.2 (P=.01).
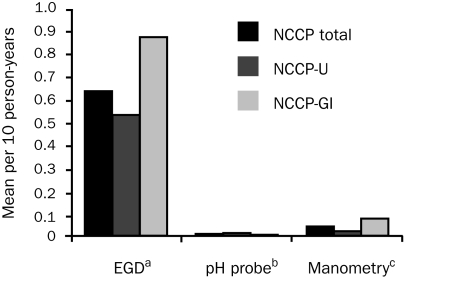
FIGURE 3.
Gastrointestinal (GI) testing in patients with noncardiac chest pain (NCCP) (mean tests per 10 person-years). Rate and hazard ratios are adjusted for age and sex. EGD = esophagogastroduodenoscopy; U = unknown.
a Rate ratio comparing NCCP-U vs NCCP-GI for EGD: 0.9 (P=.6).
b Hazard ratio comparing NCCP-U vs NCCP-GI for pH probes: 1.7 (P=.6).
c Hazard ratio comparing NCCP-U vs NCCP-GI for manometry: 1.2 (P=.8).
GI Testing
Mayo Clinic has an open-access endoscopy and esophageal laboratory. Of the total study sample, 38% underwent EGD (247 tests), 4% underwent manometry (13 tests), and 2% had pH probes (6 probes). Utilization is reported in Figure 3 in mean tests per 10 person-years. The rate ratio, adjusted for age and sex, comparing NCCP-U vs NCCP-GI for EGD was 0.9 (95% CI, 0.6-1.3; P=.6). The adjusted Cox model hazard ratios comparing NCCP-U vs NCCP-GI for manometry studies and pH probes were 1.2 (95% CI, 0.3-4.5; P=.8) and 1.7 (95% CI, 0.2-14.6; P=.6), respectively.
Death From Any Cause, Cardiac Death, and Noncardiac Death
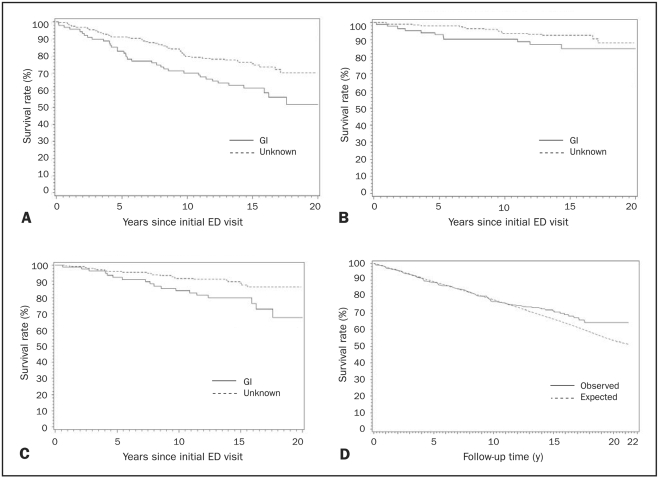
Death from any cause, cardiac death, and noncardiac death were recorded for both NCCP-GI and NCCP-U groups throughout the follow-up period. The follow-up period for death began at the initial ED visit. Ninety patients died during the follow-up period. Patient deaths were attributed to the following causes: 27 cardiac, 3 GI-related, 37 non-GI noncardiac, and 23 unknown. Kaplan-Meier survival plots are presented in Figure 4. Overall survival in NCCP-GI patients was 70.1% at 10 years and 51.8% at 20 years compared with 79.7% at 10 years and 70.2% at 20 years for NCCP-U patients. An expected survival curve was created for the Minnesota white population (1950-2000), which showed no statistically significant increase in all-cause mortality in the total NCCP cohort (P=.19) (Figure 4, D). Mortality in the NCCP-GI group was similar to the expected mortality (P=.57). However, the NCCP-U group had less mortality than expected (54 observed deaths vs 70.5 expected deaths; P=.05). The divergence occurred in the 11th year of follow-up.
FIGURE 4.
A, Overall survival. B, Survival free of cardiac death. C, Survival free of noncardiac death. D, Survival in noncardiac chest pain cohort vs expected survival; P=.19 (log-rank test). ED = emergency department; GI = gastrointestinal.
Survival free of cardiac death in the NCCP-GI group was 90.2% at 10 years and 84.8% at 20 years compared with 93.7% at 10 years and 88.1% at 20 years for the NCCP-U group. Patients in the NCCP-GI group experienced decreased survival due to cardiac death, as well as noncardiac death and death from any cause, at all time points.
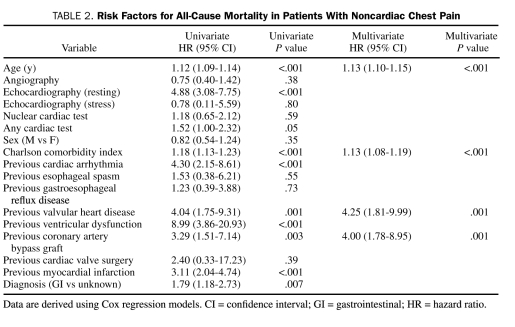
Analysis of risk factors for all-cause mortality using univariate models yielded statistically significant increased risk for age, Charlson comorbidity index, NCCP-GI diagnosis, resting echocardiography at time of NCCP diagnosis, and previous cardiac diagnoses, including arrhythmia, valvular disease, ventricular dysfunction, and MI and previous coronary artery bypass graft (CABG). Only age, Charlson comorbidity index, previous CABG, and previous valvular disease were significant after adjustment for other covariates (Table 2). No specific cardiac test or the absence of cardiac tests was associated with mortality. The diagnosis of NCCP-GI was not significant in the multivariate analysis for mortality. The NCCP-GI group was composed of patients with different diagnoses that required further evaluation. Patients with GERD, cholecystitis, or miscellaneous GI disorders (previously listed) were further evaluated. No survival difference occurred on the basis of the specific GI diagnosis (P=.51).
TABLE 2.
Risk Factors for All-Cause Mortality in Patients With Noncardiac Chest Pain
DISCUSSION
Noncardiac chest pain is common and costly. Patients with NCCP are seen in primary care, in the ED, and by subspecialists. With the exception of costs, little is known about health care utilization after a diagnosis of NCCP.
The first aim of this study was to determine the frequency of GI consultation and testing. In this sample, 49% of patients were reevaluated in the ED, and 42% underwent repeated cardiology evaluations; only 15% had GI consultations after the initial diagnosis of NCCP. Although repeated ED visits for chest pain are to be expected, the number of repeated cardiology evaluations and the paucity of GI consultations are surprising. Our result is in direct contradistinction to results from a survey by Wong et al24 of 205 primary care physicians in the United States. These investigators reported that, when referring patients for further management of NCCP, most primary care physicians preferred consultation by a gastroenterologist (75.6%) and less frequently asked for consultation by a cardiologist (7.8%). Despite these preferences, the primary care physicians in that study actually referred 29.8% of their NCCP patients to a gastroenterologist and 14% to a cardiologist. The latter figures more closely approximate those reported by Eslick et al25 in Australia, where 30% of NCCP patients sought the care of a gastroenterologist. Thus, patients in this study were seen less frequently by a gastroenterologist than in previous studies.
For patients with NCCP-U, the rate of being seen by a gastroenterologist was 3 times higher than for their NCCP-GI counterparts (P=.01). This may be explained by the fact that patients who are given a specific diagnosis for the cause of their chest pain exhibit decreased use of health care.26 An EGD was ordered for 38% of patients, and many had repeated studies (247 procedures). Few pH probes (2% of patients) and manometry studies (4% of patients) were performed. This result calls into question whether patients with NCCP are receiving appropriate testing after being diagnosed as having NCCP. These figures suggest that EGD is overused and that other testing modalities may be underused. In the absence of alarm symptoms, EGD is not a first-line diagnostic test in the evaluation of NCCP because esophagitis is rarely found during examination.27,28 The effect of proton pump inhibitors, which were introduced in 1990, on how diagnostic tests were ordered during the 1993-2003 follow-up period is unknown. Our results are somewhat similar to the results of a survey of 275 gastroenterologists by Ali and Lacy,29 which reported that 9.8% of survey responders would order an esophageal pH probe for the initial evaluation of NCCP and that 6.2% would order a manometry study.
The second aim of our study was to report on overall mortality and, specifically, cardiac death in patients with NCCP. Although prognosis for patients with NCCP is thought to be favorable, data to support this view are limited. Additionally, certain subgroups of NCCP patients may be at increased risk of cardiac death; to our knowledge, the current study is the first study of its size to report on this end point in NCCP-GI and NCCP-U groups.
In this study, NCCP-GI patients displayed less survival free of cardiac death during all points of the follow-up period compared with their NCCP-U counterparts (Figure 4, B). After 10 and 20 years of follow-up, the NCCP-GI group had rates of survival free of cardiac death of 90.2% and 84.8%, respectively. Although the total sample did not display a significantly increased frequency of death compared with what would be expected in this community, a substantial number of cardiac deaths occurred in an NCCP population. This result may be partially explained by overlapping risk factors for GERD (most common cause of NCCP) and coronary artery disease, including obesity, obstructive sleep apnea, diabetes mellitus, and smoking.30-36
The NCCP-GI group displayed less overall survival at all time points, specifically 70.1% at 10 years and 51.8% at 20 years, compared with their NCCP-U counterparts. The univariate analysis revealed an association between the NCCP-GI group and increased mortality (hazard ratio, 1.79; P=.007). However, the multivariate analysis did not support an association between the NCCP-GI subset and increased all-cause mortality; this was likely due to older age (62 vs 56 years) and increased frequency of previous cardiac arrhythmia at baseline in the NCCP-GI group. As expected, age, Charlson comorbidity index, previous valvular surgery, and previous CABG were statistically significant predictors of all-cause mortality in the multivariate analysis.
The results of the current study should be interpreted with limitations in mind. Although initial NCCP episodes may have occurred at any site throughout Olmsted County, all follow-up information was collected solely from Mayo Clinic. Thus, physician visits potentially could have been underestimated. However, the closest medical centers are 71 miles away (La Crosse, WI) and 84 miles away (St. Paul and Minneapolis, MN). According to survey data, 90% of respondents would receive their care from one of 3 providers in the county, and 96% would see an Olmsted County provider for a major medical problem.37 Given this information, it is likely that ED visits alone could have been underrepresented; that is, no gastroenterologists or cardiologists practice at sites in Olmsted County other than Mayo Clinic. Another possible limitation resulted from data collection using only electronic medical records for half of this sample. This could result in a small underestimation of visits and testing because the follow-up period began in 1993 and electronic medical records were firmly in place in 1995.
CONCLUSION
The frequency of health care utilization in community residents with NCCP is high. Patients in this study received few GI consultations and underwent even fewer GI tests. Patients with NCCP seen in esophageal laboratories represent a very small fraction of people with NCCP in the community. Further study is needed to determine whether patients with NCCP would benefit from more frequent GI consultations and more diverse use of GI testing modalities.
Patients dismissed from the hospital with NCCP continue to experience subsequent cardiac death. All-cause mortality in patients with NCCP is not significantly different than that in the community. However, we do not know whether patients with NCCP die more frequently of cardiac death than would be expected.
We speculate that cardiac death in patients with NCCP may relate to overlapping risk factors for GERD and coronary artery disease, including obesity, obstructive sleep apnea, diabetes mellitus, and smoking. Until cardiac death in this population is better understood, it is prudent to screen for cardiac risk factors such as hypertension, hypercholesterolemia, and diabetes mellitus and aggressively manage these comorbid conditions when present.
Footnotes
Support was provided by TAP Pharmaceutical Products (now part of Takeda Pharmaceuticals North America).
This study was presented in part at the American College of Gastroenterology Annual Scientific Meeting; October 24, 2006; Las Vegas, NV; and Digestive Disease Week; May 21, 2007; Washington, DC.
REFERENCES
- 1.American Heart Association Heart Disease and Stroke Statistics—2005 Update Dallas, TX: American Heart Association; 2005. [Google Scholar]
- 2.Nevens F, Janssens J, Piessens J, Ghillebert G, De Geest H, Vantrappen G. Prospective study on prevalence of esophageal chest pain in patients referred on an elective basis to a cardiac unit for suspected myocardial ischemia. Dig Dis Sci. 1991;36:229-235 [DOI] [PubMed] [Google Scholar]
- 3.Locke GR, III, Talley NJ, Fett SL, Zinsmeister AR, Melton LJ., III Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted County, Minnesota. Gastroenterology 1997;112:1448-1456 [DOI] [PubMed] [Google Scholar]
- 4.Richter JE, Bradley LA, Castell DO. Esophageal chest pain: current controversies in pathogenesis, diagnosis, and therapy. Ann Intern Med. 1989;110:66-78 [DOI] [PubMed] [Google Scholar]
- 5.Olden KW. The psychological aspects of noncardiac chest pain. Gastroenterol Clin North Am. 2004;33:61-67 [DOI] [PubMed] [Google Scholar]
- 6.Wise JL, Locke GR, Zinsmeister AR, Talley NJ. Risk factors for non-cardiac chest pain in the community. Aliment Pharmacol Ther. 2005;22:1023-1031 [DOI] [PubMed] [Google Scholar]
- 7.Cannon RO, III, Epstein SE. “Microvascular angina” as a cause of chest pain with angiographically normal coronary arteries. Am J Cardiol. 1988;61:1338-1343 [DOI] [PubMed] [Google Scholar]
- 8.DeMeester TR, O'Sullivan GC, Bermudez G, Midell AI, Cimochowski GE, O'Drobinak J. Esophageal function in patients with angina-type chest pain and normal coronary angiograms. Ann Surg. 1982;196:488-498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.de Caestecker JS, Blackwell JN, Brown J, Heading RC. The oesophagus as a cause of recurrent chest pain: which patients should be investigated and which tests should be used? Lancet 1985;2:1143-1146 [DOI] [PubMed] [Google Scholar]
- 10.Peters L, Maas L, Petty D, et al. Spontaneous noncardiac chest pain: evaluation by 24-hour ambulatory esophageal motility and pH monitoring. Gastroenterology 1988;94:878-886 [PubMed] [Google Scholar]
- 11.Soffer EE, Scalabrini P, Wingate DL. Spontaneous noncardiac chest pain: value of ambulatory esophageal pH and motility monitoring. Dig Dis Sci. 1989;34:1651-1655 [DOI] [PubMed] [Google Scholar]
- 12.Janssens J, Vantrappen G, Ghillebert G. 24-Hour recording of esophageal pressure and pH in patients with noncardiac chest pain. Gastroenterology 1986;90:1978-1984 [DOI] [PubMed] [Google Scholar]
- 13.Ahmed T, Vaezi MF. The role of pH monitoring in extraesophageal gastroesophageal reflux disease. Gastrointest Endosc Clin N Am. 2005;15:319-331 [DOI] [PubMed] [Google Scholar]
- 14.Lacima G, Grande L, Pera M, Francino A, Ros E. Utility of ambulatory 24-hour esophageal pH and motility monitoring in noncardiac chest pain: report of 90 patients and review of the literature. Dig Dis Sci. 2003;48:952-961 [DOI] [PubMed] [Google Scholar]
- 15.Achem SR, DeVault KR. Recent developments in chest pain of undetermined origin. Curr Gastroenterol Rep. 2000;2:201-209 [DOI] [PubMed] [Google Scholar]
- 16.Tew R, Guthrie EA, Creed FH, Cotter L, Kisely S, Tomenson B. A long-term follow-up study of patients with ischaemic heart disease versus patients with nonspecific chest pain. J Psychosom Res. 1995;39:977-985 [DOI] [PubMed] [Google Scholar]
- 17.Potts SG, Bass CM. Psychosocial outcome and use of medical resources in patients with chest pain and normal or near-normal coronary arteries: a long-term follow-up study. Q J Med. 1993;86:583-593 [PubMed] [Google Scholar]
- 18.Wilhelmsen L, Rosengren A, Hagman M, Lappas G. “Nonspecific” chest pain associated with high long-term mortality: results from the primary prevention study in Goteborg, Sweden. Clin Cardiol. 1998;21:477-482 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Prina LD, Decker WW, Weaver AL, et al. Outcome of patients with a final diagnosis of chest pain of undetermined origin admitted under the suspicion of acute coronary syndrome: a report from the Rochester Epidemiology Project. Ann Emerg Med. 2004;43:59-67 [DOI] [PubMed] [Google Scholar]
- 20.Diamond GA. A clinically relevant classification of chest discomfort. J Am Coll Cardiol. 1983;1:574-575 [DOI] [PubMed] [Google Scholar]
- 21.Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis. 1987;40:373-383 [DOI] [PubMed] [Google Scholar]
- 22.Gooley TA, Leisenring W, Crowley J, Storer BE. Estimation of failure probabilities in the presence of competing risks: new representations of old estimators. Stat Med. 1999;18:695-706 [DOI] [PubMed] [Google Scholar]
- 23.Therneau T, Offord J. Expected survival based on hazard rates. Technical Report No. 63 Rochester, MN: Department of Health Sciences Research, Mayo Clinic; http://mayoresearch.mayo.edu/mayo/research/biostat/upload/63.pdf Published February18, 1999. Accessed January 19, 2010 [Google Scholar]
- 24.Wong WM, Beeler J, Risner-Adler S, Habib S, Bautista JM, Fass R. Attitudes and referral patterns of primary care physicians when evaluating subjects with noncardiac chest pain—a national survey. Dig Dis Sci. 2005;50(4):656-661 [DOI] [PubMed] [Google Scholar]
- 25.Eslick GD, Jones MP, Talley NJ. Non-cardiac chest pain: prevalence, risk factors, impact and consulting—a population-based study. Aliment Pharmacol Ther. 2003;17:1115-1124 [DOI] [PubMed] [Google Scholar]
- 26.Rose S, Achkar E, Easley KA. Follow-up of patients with non-cardiac chest pain; value of esophageal testing. Dig Dis Sci. 1994;39:2063-2068 [DOI] [PubMed] [Google Scholar]
- 27.Frobert O, Funch-Jensen P, Jacobsen NO, Kruse A, Bagger JP. Upper endoscopy in patients with angina and normal coronary angiograms. Endoscopy 1995;27:365-370 [DOI] [PubMed] [Google Scholar]
- 28.Hsia PC, Maher KA, Lewis JH, Cattau EL, Jr, Fleischer DE, Benjamin SB. Utility of upper endoscopy in the evaluation of noncardiac chest pain. Gastrointest Endosc. 1991;37:22-26 [DOI] [PubMed] [Google Scholar]
- 29.Ali MA, Lacy BE. Esophageal manometry and pH monitoring: gastroenterologists' adherence to published guidelines. J Clin Gastroenterol. 2005;39:584-590 [DOI] [PubMed] [Google Scholar]
- 30.El-Serag H. Role of obesity in GORD-related disorders. Gut 2008;57:281-284 [DOI] [PubMed] [Google Scholar]
- 31.Fass R. The pathophysiological mechanisms of GERD in the obese patient. Dig Dis Sci. 2008;53(9):2300-2306 [DOI] [PubMed] [Google Scholar]
- 32.Green BT, Broughton WA, O'Connor JB. Marked improvement in nocturnal gastroesophageal reflux in a large cohort of patients with obstructive sleep apnea treated with continuous positive airway pressure. Arch Intern Med. 2003;163:41-45 [DOI] [PubMed] [Google Scholar]
- 33.Nishida T, Tsuji S, Tsujii M, et al. Gastroesophageal reflux disease related to diabetes: analysis of 241 cases with type 2 diabetes mellitus. J Gastroenterol Hepatol. 2004;19:258-265 [DOI] [PubMed] [Google Scholar]
- 34.Wang X, Pitchumoni CS, Chandrarana K, Shah N. Increased prevalence of symptoms of gastroesophageal reflux diseases in type 2 diabetics with neuropathy. World J Gastroenterol. 2008;14:709-712 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Watanabe Y, Fujiwara Y, Shiba M, et al. Cigarette smoking and alcohol consumption associated with gastro-oesophageal reflux disease in Japanese men. Scand J Gastroenterol. 2003;38:807-811 [DOI] [PubMed] [Google Scholar]
- 36.Nilsson M, Johnsen R, Ye W, Hveem K, Lagergren J. Lifestyle related risk factors in the aetiology of gastro-oesophageal reflux. Gut 2004;53:1730-1735 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Melton LJ., III History of the Rochester Epidemiology Project. Mayo Clin Proc. 1996;71:266-274 [DOI] [PubMed] [Google Scholar]