Abstract
In a 2007 report, the US Surgeon General called for health care professionals to renew efforts to reduce underage drinking. Focusing on the adolescent patient, this review provides health care professionals with recommendations for alcohol-related screening, brief intervention, and referral to treatment. MEDLINE and published reviews were used to identify relevant literature. Several brief screening methods have been shown to effectively identify underage drinkers likely to have alcohol use disorders. After diagnostic assessment when germane, the initial intervention typically focuses on education, motivation for change, and consideration of treatment options. Internet-accessible resources providing effective brief interventions are available, along with supplemental suggestions for parents. Recent changes in federal and commercial insurance reimbursement policies provide some fiscal support for these services, although rate increases and expanded applicability may be required to prompt the participation of many practitioners. Nevertheless, advances in clinical methods and progress on reimbursement policies have made screening and brief intervention for underage drinking more feasible in general health care practice.
ADHD = attention-deficit/hyperactivity disorder; AUDIT = Alcohol Use Disorders Identification Test; AUDIT-C = Alcohol Use Disorders Identification Test–Consumption; AUD = alcohol use disorder; CAGE = Cut down, Annoyed, Guilty, Eye-opener; CRAFFT = Care, Relax, Alone, Family, Friends, Trouble; DSM-IV-TR = Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision); NIAAA = National Institute on Alcohol Abuse and Alcoholism; SAMHSA = Substance Abuse and Mental Health Services Administration; SBIRT = screening, brief intervention, and referral to treatment
Underage drinking is a statistically and culturally normative phenomenon in the United States. Alcohol use is typically initiated in middle adolescence, and binge drinking is common in high school students.1 Initiation of alcohol use in early adolescence increases the risk for alcohol use disorders (AUDs).2,3 Underage drinking peaks during the college-age years, and alcohol dependence is more common among older adolescents (ie, 18-20 years) than among any adult age group.4 More than one-third of college students have alcohol abuse or dependence, and among those with alcohol dependence, only approximately 1 in 20 have sought treatment.5 Given the relative infrequency of health care visits among this age group, any available opportunities for health care practitioners to identify and intervene with underage drinkers need to be used. Organizations representing health care professionals and federal health services agencies have agreed that identification of underage drinkers should be routine clinical practice. The US Surgeon General recently called for health care professionals to identify adolescents who use alcohol, provide expanded services for them, and develop treatment referral networks. Despite this consensus, few health care professionals adhere to these recommendations.6 Commonly cited barriers include time constraints, inadequate reimbursement, concerns about alienating the patient and family, inadequate training, and lack of intervention resources.7,8 Health care professional education has been shown to partially overcome these barriers.9 This review provides health care practitioners with contemporary information on alcohol-related screening, brief intervention, and referral to treatment (SBIRT) that will facilitate their participation in this national effort to reduce underage drinking.
Patients aged 12 through 20 years need to be screened for underage drinking. Adolescents in this age range may be seen by internists, pediatricians, family physicians, specialty physicians, and nonphysician practitioners. Any health care practitioners serving patients in this age group may be called on to identify and intervene with an underage drinker. The methods described in this article may also be implemented in a variety of health care settings, including but not limited to traditional outpatient clinics, emergency departments, and schools. Adolescents tend to have relatively little contact with health care practitioners, making screening and intervention for underage drinking important in virtually any health care setting. Therefore, we targeted this article to any health care professionals who serve individuals in this age range.
METHODS
To identify relevant articles, MEDLINE was searched using combinations of the terms alcohol, adolescents, screening, brief intervention, and primary care. The names of authors identified as having conducted research in this area were also used as search terms. Recent review articles on adolescent AUDs and screening for AUDs in primary care settings were used to identify relevant articles. Our goal was to provide a relatively succinct review article intended for a general medical audience. Therefore, we selected for discussion and citation the articles that were most pertinent to this goal.
SCREENING FOR UNDERAGE DRINKING AND AUDs
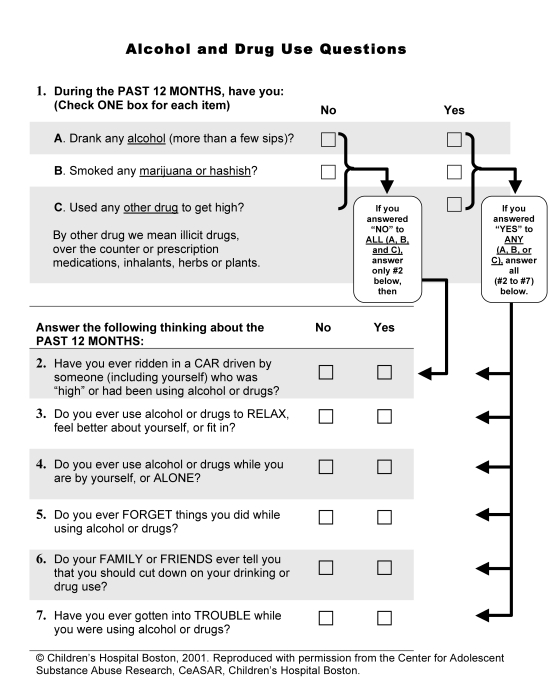
Compared with clinical impressions, systematic assessment methods substantially improve identification of adolescents likely to have AUDs.10 Screening for AUDs in adults traditionally relies on interview questions about alcohol-related problems organized to yield memorable mnemonics.1 Such tools may be readily incorporated into clinical practice. Two such tools have been examined in several studies: CAGE (Cut down, Annoyed, Guilty, Eye-opener) and CRAFFT (Care, Relax, Alone, Family, Friends, Trouble). CAGE, the most widely known of these screening methods, has been found to have relatively poor sensitivity and specificity in underage drinkers.1 CRAFFT11 begins with 3 questions about the presence or absence of alcohol, marijuana, or other drug use, then inquires about problems related to “alcohol or drugs” in 6 questions (Figure 1). At a threshold score of 2 of 6, some studies have found that CRAFFT has acceptable sensitivity and specificity for identifying adolescents likely to have AUDs or other substance use disorders (eg, sensitivity, 0.80; specificity, 0.86; positive predictive value, 0.53; and negative predictive value, 0.96).10 However, other studies have found that CRAFFT has poor specificity (0.33 in the study by Cook et al12 and 0.44 in the study by Kelly et al13). The advantages of CRAFFT include a broadened screening focus to the inclusion of “drugs,” the interview format, and simple response options (yes or no). Nonetheless, problem-focused screens do not eliminate the need for determining substance use patterns. Adolescents whose screening results are negative for problems may actually be engaging in high-risk drinking. A positive problem-focused screen needs to be followed by inquiries about substance consumption patterns and a diagnostic evaluation.
FIGURE 1.
Alcohol and drug use screening questions from CRAFFT (Care, Relax, Alone, Family, Friends, Trouble). From the Center for Adolescent Substance Abuse Research, Children's Hospital Boston, with permission.
The 10-item Alcohol Use Disorders Identification Test (AUDIT)14 includes consumption (AUDIT-C; 3 items) and problem (7 items) subscales. AUDIT has consistently shown acceptable sensitivity and specificity in adults.15 AUDIT items may be presented by interview or questionnaire.16 The AUDIT takes approximately 2 minutes to administer and approximately 1 minute to score. This instrument is included in the National Institute on Alcohol Abuse and Alcoholism (NIAAA) clinician's guide.17 AUDIT has been tested in several adolescent samples. In a study of 415 adolescents aged 13 through 19 years who were seen in an emergency department,18 an AUDIT total score threshold of 3 yielded acceptable sensitivity (0.95) and specificity (0.75). Among 538 adolescents aged 14 through 18 years who were seen in a primary care clinic,19 an AUDIT total score threshold of 3 yielded acceptable sensitivity (0.88) and specificity (0.77). For adults, a score of 8 has typically been recommended, although some authors have suggested that a lower score should be adopted.15 Studies of older adolescents (ie, >18 years) have found that a threshold score of 8 has yielded acceptable results on both sensitivity and specificity.12,13 We recommend a threshold of 3 to maximize sensitivity of the scale for use in adolescents younger than 18 years. For those aged 18 through 20 years, a threshold of 8 is recommended.
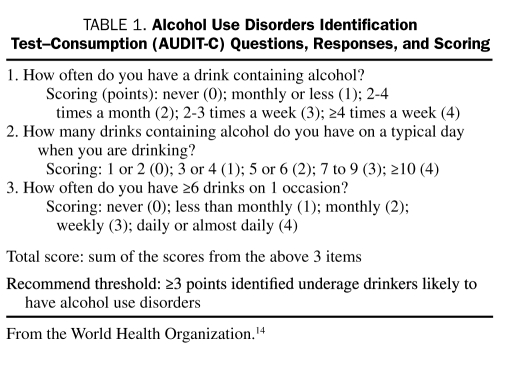
Abbreviated methods assessing alcohol consumption levels may be effective for identifying adolescents likely to have AUDs. These methods are based on a minimum quantity of one standard drink (ie, 12 oz of beer, 8 oz of malt liquor, 5 oz of wine, and 1.5 oz of spirits). The 3 AUDIT-C items (Table 1) and the 10-item AUDIT have shown similar sensitivities and specificities in adult samples.15 A single question asking the frequency of drinking episodes in the prior month with a threshold of 3 episodes was found to be 90% sensitive and 84% specific as a screen for adolescent AUDs.20 Among adults aged 18 through 20 years seen in an emergency department, AUDIT-C, CRAFFT, and the Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) (DSM-IV-TR) 2-item scale were effective screens.21 The 2-item screen required a positive response to one of 2 DSM-IV-TR symptoms, those involving hazardous use (A2) or drinking in larger amounts or for a longer period than intended (D3; Table 1). In this sample, the 2-item DSM-IV-TR screen showed 88% sensitivity and 90% specificity. The AUDIT-C, drinking frequency, and DSM-IV-TR 2-item screens need to be more thoroughly studied in adolescent samples. In the absence of a clearly superior approach among these methods, acceptable screening methods for possible underage drinkers include the 10-item AUDIT, AUDIT-C, drinking 3 or more times in the past month, endorsement of DSM-IV-TR items A2 or D3, and CRAFFT.
TABLE 1.
Alcohol Use Disorders Identification Test–Consumption (AUDIT-C) Questions, Responses, and Scoring
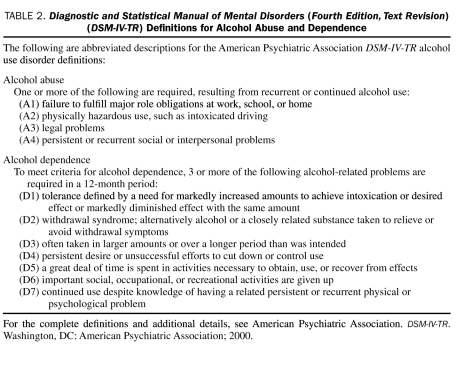
DIAGNOSIS OF AUDs
Only a few adolescents (ie, approximately 5% of 12- to 17-year-olds and 15% of 18- to 20-year-olds) meet DSM-IV-TR criteria for AUDs.1,4 The American Psychiatric Association DSM-IV-TR diagnostic criteria identify abuse and dependence as distinct disorders (Table 2). The 4 DSM-IV-TR abuse symptoms identify substance-related adverse health and social consequences. The 7 dependence symptoms comprise psychological and physiologic dimensions. Psychological dependence refers to compulsive use, whereas physiologic dependence refers to alcohol tolerance and withdrawal. To ensure that all AUD symptoms are evaluated, we recommend using structured or semistructured interviews, which are superior to unstructured clinical assessments.1 The NIAAA clinician's guide17 provides suggested wording for inquiring about these symptoms.
TABLE 2.
Diagnostic and Statistical Manual of Mental Disorders (Fourth Edition, Text Revision) (DSM-IV-TR) Definitions for Alcohol Abuse and Dependence
The DSM-IV-TR criteria in this arena were developed primarily for applications with adults. Several DSM-IV-TR items are problematic when applied to underage drinkers.22 The tolerance item does not clearly distinguish pathologic tolerance due to extreme drinking from the normal development of tolerance during the early stages of drinking. Intent to control use is assumed in 2 dependence items (D3 and D4; Table 2). Goals to limit alcohol use may be absent in some adolescents with problem drinking. Adolescent-parent conflicts about alcohol use may lead to an endorsement of the A4 abuse item. In some cases, a clinically meaningful alcohol problem may be present that warrants an AUD diagnosis. However, in other cases, such conflicts may signal family issues in which the adolescent does not exhibit excessive alcohol use. The intent of the diagnostic system is communicated in the introductory sentence to the definition of substance abuse and dependence in DSM-IV-TR as follows: “A maladaptive pattern of substance use leading to clinically significant impairment or distress.” Applying this description, the health care professional may elect not to diagnose alcohol abuse in adolescents in which impairment or distress is not evident. With these caveats in mind, the DSM-IV-TR criteria for AUDs may be validly applied to adolescents seen in primary care settings.
Many health care practitioners are concerned that adolescents' self-report on alcohol use and related problems may not be candid. In situations in which social sanctions would result if an adolescent admits to drinking, this concern may be valid. However, options for supplementing self-report have major limitations. Parents tend to be uninformed about their teen's alcohol use and related problems.23 Blood and breath tests for alcohol yield positive results for only a few hours after consumption. Health care professionals can improve the validity of reports by assuring patients that their reports will be kept in confidence.24 Most states have regulations specifying that a minor may consent to assessment and treatment for substance use disorders.25
ASSESSMENT OF AUD COMPLICATIONS
In adult patients, health care practitioners are often called on to manage the medical consequences of alcohol dependence, including severe liver (eg, cirrhosis), cardiac (eg, cardiomyopathy), and neurologic impairments (eg, Wernicke-Korsakoff syndrome). These complications are uncommon among adolescents with AUDs.1 Rather, adolescents with AUDs often have other substance problems, mental disorders, and risky behaviors that lead to medical problems.1 Underage drinkers often smoke cigarettes and marijuana and use other illicit drugs. Common mental disorders among adolescents with AUDs include conduct disorder, attention-deficit/hyperactivity disorder (ADHD), and depression. Among those with depression, suicidal ideas and behavior need to be assessed. The possibility of a child maltreatment history should be considered.26 In adolescents, AUDs lead to problems in academic achievement and school adjustment.1 Somatic complaints in these adolescents, including reports of fatigue and abdominal distress, are typically associated with depression and anxiety disorders.27 Physical examination may find dental caries due to neglect of oral health maintenance.27 Although obvious neuropsychological impairment is typically not evident, late-developing cortical areas subserving cognitive, behavioral, and emotional regulation may be vulnerable to adverse alcohol effects.28,29 Risky sexual behaviors can lead to sexually transmitted diseases30 and pregnancy.31 These areas need to be explored in the clinical assessment of adolescents with AUDs. In underage drinkers, alcohol-related mortality is a tragic, although predictable, consequence most often a result of intoxicated driving.32 Fortunately rare, alcohol poisoning resulting in death occasionally occurs in this age group.33
INTERVENTIONS WITH ADOLESCENT UNDERAGE DRINKERS APPLICABLE IN THE HEALTH CARE SETTING
With underage drinkers, SBIRT requires both effective and feasible intervention. A consensus approach based on definitive studies indicating the best practices for adolescent SBIRT is not yet available. Nevertheless, prevention programs, brief interventions, and empirically supported treatments may be recommended. Approaches available to patients seen in primary care settings include office-based brief interventions, pharmacological treatments, Web-based programs, self-help organizations, and referral to specialized treatment.
Brief Interventions
Brief interventions (5-15 minutes) with follow-up provided to adult problem drinkers in primary care settings have been found to reduce alcohol consumption.34 Such interventions have been recommended as part of standard care for underage drinkers.35 Brief interventions examined in controlled intervention trials have varied considerably in length and content. At minimum, the practitioner administers the screening instrument, interprets the result for the patient, and provides simple advice on how to abstain from alcohol use. Interventions administered during multiple visits and requiring several hours to perform have also been termed brief. Primary care practitioners are unlikely to find such extended interventions feasible. The opportunity to address underage drinking typically occurs in the context of a health care visit initiated for other purposes. Interventions most likely to be used in this setting occur in 1 or 2 visits, with each visit requiring less than 15 minutes.
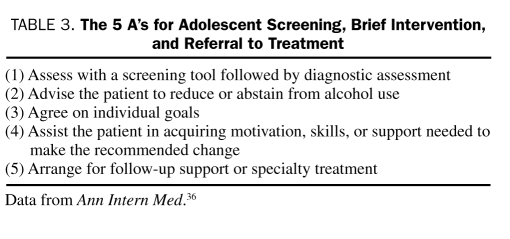
The US Preventive Services Task Force36,37 completed an effectiveness review on alcohol-related brief interventions applied in primary care settings; it concluded that there was “good evidence” that brief interventions with follow-up produce small to moderate reductions in alcohol consumption that are sustained for 6 to 12 months. The interventions found to be effective included feedback, advice and goal setting, advice for further assistance, and a follow-up contact. These interventions were performed in approximately 15 minutes during the initial contact, with a follow-up visit of similar intensity. The approach may be summarized by the 5 A's (Table 3). Resources that facilitate interventions included physician training, prompts, practice algorithms, and patient education materials. The recommendation to provide these services rated a grade B, signifying “at least fair evidence” that the service improves important health outcomes and that benefits outweigh harms. A similar conclusion was reached in a Cochrane review.34 Cost-benefit analyses have concluded that alcohol-related SBIRT is among the most cost-effective preventive services.36,38,39
TABLE 3.
The 5 A's for Adolescent Screening, Brief Intervention, and Referral to Treatment
For adolescents, the US Preventive Services Task Force36 concluded in 2004 that the evidence was insufficient to recommend for or against alcohol-related SBIRT in primary care settings. Few pertinent studies have been conducted in the past few years. An SBIRT approach with adolescents involving two 1-hour sessions was developed and pilot tested in a primary care clinic, with results showing reduced alcohol use.40 In the emergency department setting, a 45-minute, single-session intervention was shown to reduce alcohol use.41 Given that insufficient time is commonly cited as a barrier to providing SBIRT to adolescents,8 such interventions are problematic in primary care settings. A brief SBIRT for adolescents that focuses on alcohol and other drugs has been developed and found to be feasible in primary care settings.42 In a small randomized controlled trial (n=42),43 adolescents with a positive CRAFFT result underwent a 15-minute intervention conducted at a subsequently scheduled appointment. The intervention included an assessment of motivation to change, motivational enhancement, and goal setting. A 5- to 10-minute booster session was provided by telephone 1 month later. Outcome was determined 3 months after the intervention. A statistically significant reduction in the frequency of marijuana use was noted. However, frequency of alcohol use was not significantly reduced. The trend was in the expected direction with some reduction in alcohol use, and this negative finding may have been due to inadequate statistical power. Our recommendation to provide SBIRT to adolescent patients seen in primary care is thus based on generalization from adult research, studies conducted with adolescents in other settings, and promising results in primary care settings.
Alcohol-related SBIRT with adolescents may be enhanced by facilitating motivation to change and including norm-setting messages. Motivational interviewing is a style of counseling that facilitates identification of discrepancies between the effects of problem behaviors and future goals. Motivational interviewing was developed as an alternative to confrontational intervention styles. The motivational interviewing approach encourages the clinician to express empathy, avoid argument, and support self-efficacy.35 Although other approaches may be as effective, brief interventions using motivational interviewing have been shown to be superior to no treatment in reducing alcohol use in underage drinkers.41 Applied in the primary care setting, motivational interviewing has been found to reduce adolescent substance use.43 Norm setting attempts to correct adolescents' overestimates of peer alcohol use by providing normative information. For adolescents with problematic alcohol involvement, this information factually illustrates that normative peers typically have relatively little alcohol use. Norm setting has been found to mediate the effects of successful prevention programs on adolescent alcohol use.44 Among college students mandated to participate in an intervention as a result of alcohol policy violations, a Web-based normative feedback intervention was found to be more effective than Web-based education.45 Those in the normative feedback condition showed greater reductions in weekly drinking quantity and in the frequency of drinking to intoxication in a 30-day follow-up period. Health care practitioners who provide SBIRT for underage drinkers by incorporating the 5 A's can be reassured that they are providing an intervention likely to be helpful and arguably as effective as any other feasible approach.
Psychopharmacological Interventions
In many patients with AUDs, brief interventions may be insufficient. In patients for whom specialty referral is problematic, the health care practitioner may be inclined to consider pharmacological interventions as a supplement or alternative to specialty referral. However, we are reluctant to recommend any of the pharmacological approaches described in this section. These medications have not been proven safe and effective for adolescents with AUDs. Pharmacological interventions for AUDs and related comorbidities have received little study in adolescent samples. With this caveat, we review the available pharmacological options.
Pharmacological interventions for adolescents with AUDs may target withdrawal symptoms, produce aversion, diminish craving, diminish reinforcing effects, or target comorbid mental disorders.1 Benzodiazepines are used for acute alcohol withdrawal. The use of benzodiazepines is appropriate but rarely necessary in this age group.46 Benzodiazepines have substantial abuse potential, and their use for adolescents with AUDs should be limited to settings with rigorous supervision. Disulfiram (Antabuse) produces aversion to alcohol. Disulfiram blocks aldehyde dehydrogenase, resulting in increased acetaldehyde levels after alcohol consumption. Alcohol use while taking disulfiram causes nausea, hypotension, and flushing. Disulfiram is appropriate only for highly motivated patients unlikely to use alcohol, may produce other problematic adverse effects, and has not been systematically studied in adolescents.1 Acamprosate (Campral) is used to reduce alcohol craving. Acamprosate is a synthetic γ-aminobutyric acid analogue. The drug shares some of the cellular actions of taurine affecting γ-aminobutyric acid and glutaminergic receptors in the nucleus accumbens, a brain region that may be responsible for the reinforcing effects of alcohol. Acamprosate has been shown to also suppress calcium flux that results from long-term alcohol exposure, thereby altering the conformation and activity of the N-methyl-d-aspartate receptors. Although approved by the US Food and Drug Administration for the treatment of alcoholism, some recent studies have failed to find a significant effect of acamprosate on alcohol use.47,48 Little systematic information is available on the use of acamprosate in adolescents.1 Naltrexone (Revia and Vivitrol) produces a reduction in the rewarding effects of alcohol. Naltrexone is an opioid antagonist that interacts with endogenous opioid receptors. Although the effects on alcohol use were not substantial, naltrexone has performed somewhat better than acamprosate in some recent studies.47,48 Naltrexone has not been systematically studied in adolescents. Thus, disulfiram, acamprosate, and naltrexone remain experimental for use in adolescents with AUDs, and their use in general health care settings is not recommended at this time.
Medications may also target comorbid mental disorders, such as major depressive disorder or ADHD. Prescribing antidepressant medications for adolescents with AUDs and comorbid depression is an increasingly common practice.46 However, there is little empirical support for this practice. In a recently completed double-blind, placebo-controlled study,49 50 underage drinkers 15 through 20 years old with both AUDs and major depressive disorder were randomly assigned to fluoxetine or placebo. All patients received cognitive behavior therapy and motivation enhancement therapy. Fluoxetine produced no significant improvements on alcohol-related or depression-related outcome variables. In a trial that combined fluoxetine or placebo with cognitive behavior therapy for adolescents with substance use disorders, major depressive disorder, and conduct disorder, fluoxetine was superior to placebo on 1 of 2 depression measures, but a significant effect was not evident on substance use or conduct problems.50 Although ADHD may be effectively treated with stimulant medication, concerns about abuse and diversion present potential problems. For adolescents with comorbid ADHD and AUDs, opting for the methylphenidate transdermal patch or the nonstimulant drug atomoxetine reduces abuse potential.51 Ideally, an abstinent period of several weeks and reevaluation precede the initiation of pharmacological treatment. Symptoms of mental disorders often improve with alcohol abstinence. Furthermore, ongoing alcohol and other drug use combined with prescription medications may result in unanticipated hazardous interactions. For pharmacological interventions that target comorbid psychopathologic disorders, definitive controlled trials in adolescent samples are lacking. The clinician must rely largely on judgment without supporting data to justify pharmacotherapy in adolescents with AUDs.
Internet-Accessible Resources
The brief intervention achievable during a primary care visit may be supplemented after the visit by adolescents and parents participating in Internet-accessible programs. Educational materials and prevention activities for underage drinkers are available without cost through the NIAAA (www.niaaa.nih.gov), the Substance Abuse and Mental Health Services Administration (SAMHSA) (www.samhsa.gov), and the National Institute on Drug Abuse (www.nida.nih.gov). The NIAAA has developed an educational program for younger adolescents (ie, aged 11-13 years) that includes activities for teens and information for parents and teachers. The Cool Spot program (www.thecoolspot.gov) emphasizes techniques found to be effective in established prevention programs, including norm setting. Additionally, the NIAAA publishes a guide for parents of younger adolescents. SAMHSA provides health care practitioners with SBIRT resources (http://sbirt.samhsa.gov). The SAMHSA site includes links to handbooks on alcohol screening and intervention, a guide to motivational interviewing, continuing medical education curricula, information on relevant self-help organizations, and referral resources. Additionally, this SBIRT site provides reimbursement codes for commercial insurance carriers, Medicare, and Medicaid. Moreover, the SAMHSA site provides links to the US Surgeon General's report on underage drinking and a summary of the report written for families (ie, A Guide to Action for Families). The National Institute on Drug Abuse site provides similar resources primarily focusing on other substances.
Several Internet-accessible interventions have been developed for underage drinking or alcohol problems and have demonstrated effects on alcohol consumption.52 With versions designed for high school students and college students, Check-up to Go (http://www.echeckuptogo.com/usa/) uses a brief assessment to tailor individualized norm setting and motivational feedback interventions. Designed for college students, MyStudentBody.com includes a module for alcohol prevention and 5 other health area modules. These programs have been designed for large educational institutions and typically charge access fees. Although not conventionally used in health care settings, contracts with fee-based, Web-accessed interventions may be cost-effective for group practices and health care networks.
Alcohol Treatment Referral
In general medical or primary care settings, organizations typically do not have the required facilities, skills, and staff to provide specialized and comprehensive treatment for adolescents with AUDs.53 Although occasionally there are obstacles to obtaining treatment,54 referral for further assessment and specialized care constitutes the current standard of care. For adolescents, optimal treatment programs encourage abstinence, promote participation in self-help programs, target associated psychosocial problems, involve parents, and facilitate the formation of new social networks.55 Adults with AUDs seen in primary care settings are typically neither identified nor referred.56 Those referred to specialized addictions treatment usually do not adhere to treatment recommendations.57 For underage drinkers, the extent to which referral to specialty care results in successful treatment engagement has yet to be established.
The primary care practitioner may improve referral success by discussing the consequences of continued drinking, the positive effects of abstinence, the benefits of treatment, any anticipated barriers to obtaining treatment, and steps that may be taken to overcome identified barriers.58 Greater parental involvement may also enhance treatment outcomes.59 After treatment referral, the primary care practitioner may continue to contribute by advising abstinence and facilitating treatment adherence.
Self-help groups may provide effective help in many cases. For teens, Alateen offers self-help meetings in the context of the Al-Anon organization (www.al-anon.alateen.org). Al-Anon offers support and information for the family and friends of problem drinkers. Participation in Alcoholics Anonymous meetings may be appropriate and helpful for older teens (www.aa.org).
REIMBURSEMENT
One of the obstacles to effective SBIRT has been a lack of reimbursement for these services. This issue is being partially addressed by federal and commercial health care insurance carriers. Effective January 2007, the US Centers for Medicare and Medicaid Services allowed reimbursement for providing alcohol- and drug-related SBIRT. In March 2008, the Federal Employee Health Benefits Program (carrier letter 2008-06) encouraged health plans that provide coverage for federal employees to adopt reimbursement for screening and brief intervention through new billing codes for commercial insurance and the Health Care Services Procedures Coding System (ie, Current Procedural Terminology codes 99408 and 99409 and Health Care Services Procedures Coding System codes G0396 and G0397). The fee schedule ranged from $29.42 (Medicare: 15-30 minutes) to $65.51 (commercial insurance: >30 minutes).
For health care practitioners and organizations promoting SBIRT for underage drinkers, implementation of these specific reimbursement codes for SBIRT is encouraging. However, whether this rate of reimbursement is sufficient to prompt and adequately cover these services remains to be determined. The opportunity to screen and intervene for underage drinking typically arises in the context of a visit for other purposes. Under such circumstances, separate billing for added SBIRT services may not be permitted. Thus, the creation of these billing codes is a welcome step toward integrating SBIRT services into routine health care, but additional refinements will likely be needed for these services to be fully funded.
SUGGESTED APPROACH TO ALCOHOL-RELATED SBIRT FOR ADOLESCENTS
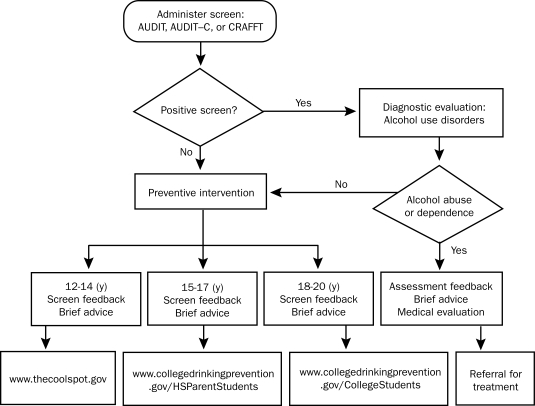
We recognize that definitive empirical support for a specific approach to intervening with underage drinkers in the primary care setting is lacking. However, to say that the literature reviewed herein provides no guidance would be an overstatement. On the basis of this literature, our experience, ongoing research, and an adaptation of the recommendations for adults described in Helping Patients Who Drink Too Much: A Clinician's Guide,17 we suggest the following approach. The suggested SBIRT steps are summarized in a flowchart presented in Figure 2.
FIGURE 2.
Suggested steps for screening, brief intervention, and referral to treatment. AUDIT = Alcohol Use Disorders Identification Test; AUDIT–C = Alcohol Use Disorders Identification Test–Consumption; CRAFFT = Care, Relax, Alone, Family, Friends, Trouble.
The practitioner may be assisted by organizing these elements into the 5 A's (Table 3). The 5 A's consist of the following elements: (1) Assess with a screening tool followed by diagnostic assessment; (2) Advise the patient to reduce or abstain from alcohol use; (3) Agree on individual goals; (4) Assist the patient in acquiring motivation, skills, or support needed to make the recommended change; and (5) Arrange for follow-up support or specialty treatment.36
Assess With a Screening Tool Followed by Diagnostic Assessment
Brief interventions designed to be conducted by health care practitioners typically begin with screening and are followed by a diagnostic assessment when indicated. For screening, we recommend the 10-item AUDIT administered by questionnaire or interview. The questionnaire version may be administered and scored by ancillary office staff, minimizing the required physician time. Using the total score, a threshold of 3 is recommended for adolescents younger than 18 years, and a threshold of 8 is recommended for those aged 18 through 20 years. Acceptable alternative screening methods are the AUDIT-C, alcohol use frequency, or CRAFFT.
For adolescents with a screen result negative for AUDs, age-appropriate assessment feedback may preface subsequent intervention elements. Keep in mind that, among those with a negative screen result, some adolescents will have substantial alcohol use and others may even have an AUD (ie, a false-negative screen result). Discussion of the results may assist in determining the validity of the responses and identifying appropriate individual goals.
For adolescents with a screen result positive for AUDs, further assessment is recommended. Patients with a positive screen result need to undergo a diagnostic assessment for AUDs, an evaluation for other high-risk behaviors, and a focused medical examination. The physician may ask face-valid questions regarding whether the patient has experienced the 11 symptoms that comprise the AUD diagnostic criteria in DSM-IV-TR. For adolescents with AUDs, a thorough evaluation includes an examination for alcohol-related comorbidities and consequences. These comorbidities include cigarette smoking, other drug use, mental disorders such as ADHD, and risky sexual behavior. Some adolescents may have alcohol-related liver injury. Feedback then focuses on the positive and negative results and may segue into advice and intervention.
Advise the Patient to Reduce or Abstain From Alcohol Use
All adolescents should be advised to abstain from using alcohol. We recognize that most adolescents have had drinking experiences and that alcohol use among college-age individuals is often tolerated although not sanctioned. Nevertheless, the hazards of underage drinking are well documented, and advising abstinence may have a modest beneficial influence. The health care practitioner may be a particularly credible source of information regarding the adverse health effects of alcohol consumption. Some adolescents refuse to consider alcohol abstinence or avoid engaging in this discussion. In these cases, the discussion of alcohol abstinence may lead to consideration of individual goals.
Agree on Individual Goals
To the extent that adolescents agree that alcohol abstinence is a worthwhile goal, an agreement between the patient and health care practitioner may be straightforward. However, for adolescents with problematic alcohol use, the advice to discontinue alcohol use may not be welcomed. In establishing individual goals in more problematic patients, the nonconfrontational style suggested by the motivational interviewing approach has been found to be helpful. Although abstinence is ideal, interim goals may include reducing alcohol use and obtaining further assistance.
Assist the Patient in Acquiring Motivation, Skills, or Support Needed to Make the Recommended Change
Patients may be directed to prevention or intervention programs according to their developmental stage and alcohol involvement characteristics. Although some health care practitioners may be prepared to deliver interventions that go beyond the first 3 interventions, most brief office visits will need to be supplemented by postvisit resources. To supplement the assessment and advice provided in the brief office-based intervention, we suggest that the health care practitioner provide the patient with Web addresses where the patient may obtain additional information or a preventive intervention. For young adolescents (ie, 12-14 years old), www.thecoolspot.gov provides age-appropriate norm setting and other information. For mid-year adolescents (ie, 15-17 years old) and older adolescents (ie, 18-20 years old), www.collegedrinkingprevention.gov provides similar age-appropriate information. Although much of the site is designed for college students, a section of the site has been specifically designated for high school students. These programs and related written materials are available without charge. Alternatively, large practices or medical centers may consider contracting commercial services, such as Electronic Check-up to Go (http://www.echeckuptogo.com/usa/) or My Student Body (www.mystudentbody.com).
Parents of adolescents may benefit from obtaining additional information on intervention options. For parents of young adolescents, the parent-oriented section of www.thecoolspot.com may be helpful. In addition, written guides are available from the NIAAA for parents of young adolescents (ie, Make A Difference: Talk to Your Child About Alcohol, National Institutes of Health publication 06-4314; available at www.niaaa.nih.gov/Publications/). For parents of mid-year and older adolescents, www.collegedrinkingprevention.gov has age-appropriate parent sections. The US Surgeon General has developed a guide for parents of mid-year adolescents (ie, A Guide to Action for Families; available at www.surgeongeneral.gov/topics/underagedrinking/). These information sources are a valuable supplement to direct intervention with adolescents. Furthermore, such resources may be pertinent to adult patients with adolescents. The parent resources are described herein in the context of screening and intervening with the adolescent. We should also indicate that these information sources may be of interest to parents and practitioners interested in obtaining further information about discussing alcohol use with their own adolescents.
Arrange for Follow-up Support or Specialty Treatment
Assessment feedback and norm-setting information provided in a nonconfrontational style provide part of the rationale for treatment referral. Visits to Web sites that provide alcohol-related information may also reinforce the referral recommendation. Ideally, adolescents with AUDs should be referred to addiction specialists with adolescent-focused services. For young and mid-year adolescents, referral to a child psychiatrist or psychologist may be a viable alternative because AUDs are typically accompanied by comorbid mental disorders. Parental involvement will be needed, and confidentiality issues will need to be addressed with the adolescent and parents. Family-oriented services or self-help groups (eg, Al-Anon) will typically be needed. For older adolescents, adult addiction specialty programs and self-help groups (eg, Alcoholics Anonymous) may be more appropriate.
Although referral to practitioners specializing in adolescent substance use disorders represents the ideal response, referral attempts may be met with several obstacles. Specialty services may not be available in some areas. Alternatives may include referral to psychiatrists, psychologists, or social workers with relevant experience. In areas where specialized adolescent addiction services are geographically available, some adolescents may have inadequate health insurance coverage for such services to be available to the individual patient. In situations in which the patient or family has the resources to take advantage of available services, cooperation on the part of the adolescent and parent may be necessary for successful treatment engagement.
Successful alcohol-related SBIRT in adults typically includes a follow-up visit or telephone-administered supplementary intervention.58 We believe that a follow-up visit by the adolescent to the primary care physician will enhance referral success. The follow-up visit can be brief, including an assessment of interim alcohol use, reinforcement of advice, and inquiry about adherence to recommendations. Alternatively, a follow-up contact by telephone can be used to encourage adherence to recommendations. The telephone call can be made by the primary care physician or an office staff member.
CONCLUSION
The tools now available to health care practitioners have substantially enhanced SBIRT for underage drinkers. Screening methods to identify underage drinkers likely to have AUDs have been developed, validated, and refined. The assessment of AUDs relies on valid self-report, and assurance of confidentiality has been shown to improve the veracity of reports by underage drinkers. Therefore, we encourage health care practitioners to determine permissible approaches in their state, to establish confidentiality policies, and to routinely communicate these policies to adolescents and their parents. When tempered by sound clinical judgment, systematic interviewing methods may be used to validly apply DSM-IV-TR AUD criteria to adolescents. Prevention programs that provide adolescents with alcohol-related education are available from federal sources with no charge. Brief interventions, including those applicable in the office setting and others available through the Internet, incorporate education, advice, norm setting, and motivational interviewing targeted to reducing alcohol use. Although additional research is needed in the primary care setting, these approaches have been shown to delay or reduce alcohol involvement. Recent changes in federal guidelines and commercial insurance policies support reimbursement for SBIRT activities. Encouraging health care practitioners to engage in screening and intervention with underage drinkers is a useful step. However, to be truly effective, such encouragement must be accompanied by widely available specialty resources and adequate reimbursement for screening and intervention services. For many or even most of our patients, these resources are lacking. Although viable SBIRT approaches are currently accessible, a more comprehensive commitment to making the component resources available is needed for the promise of SBIRT for underage drinking to be fully realized.
Footnotes
This work was supported by National Institutes of Health grants U01AA016482, K02AA00291, and P50DA05605 to Dr Clark.
REFERENCES
- 1.Thatcher DL, Clark DB. Adolescent alcohol abuse and dependence: development, diagnosis, treatment, and outcomes. Curr Psychiatry Rev. 2006;2(1):159-177 [Google Scholar]
- 2.Clark DB. The natural history of adolescent alcohol use disorders. Addiction 2004;99(suppl 1):5-22 [DOI] [PubMed] [Google Scholar]
- 3.Hingson RW, Heeren T, Winter MR. Age at drinking onset and alcohol dependence: age at onset, duration, and severity. Arch Pediatr Adolesc Med. 2006;160(7):739-746 [DOI] [PubMed] [Google Scholar]
- 4.Grant BF, Dawson DA, Stinson FS, Chou SP, Dufour MC, Pickering RP. The 12-month prevalence and trends in DSM-IV alcohol abuse and dependence: United States, 1991-1992 and 2001-2002. Drug Alcohol Depend 2004;74(3):223-234 [DOI] [PubMed] [Google Scholar]
- 5.Knight JR, Wechsler H, Kuo M, Seibring M, Weitzman ER, Schuckit MA. Alcohol abuse and dependence among U.S. college students. J Stud Alcohol. 2002;63(3):263-270 [DOI] [PubMed] [Google Scholar]
- 6.Millstein SG, Marcell AV. Screening and counseling for adolescent alcohol use among primary care physicians in the United States. Pediatrics 2003;111(1):114-122 [DOI] [PubMed] [Google Scholar]
- 7.American Academy of Pediatrics Practices and Attitudes Toward Adolescent Drug Screening Elk Grove Village, Ill: American Academy of Pediatrics, Division of Child Health Research; 1997. Periodic Survey of Fellows No. 31 [Google Scholar]
- 8.Van Hook S, Harris SK, Brooks T, et al. New England Partnership for Substance Abuse Research The “Six T's”: Barriers to screening teens for substance abuse in primary care. J Adolesc Health 2007May;40(5):456-461 Epub 2007 Feb 15 [DOI] [PubMed] [Google Scholar]
- 9.Ozer EM, Adams SH, Lustig JL, et al. Increasing the screening and counseling of adolescents for risky health behaviors: a primary care intervention. Pediatrics 2005;115(4):960-968 [DOI] [PubMed] [Google Scholar]
- 10.Wilson CR, Sherritt L, Gates E, Knight JR. Are clinical impressions of adolescent substance use accurate? Pediatrics 2004;114(5):e536-e540 [DOI] [PubMed] [Google Scholar]
- 11.Knight JR, Sherritt L, Shrier LA, Harris SK, Chang G. Validity of the CRAFFT substance abuse screening test among general adolescent clinic patients. Arch Pediatr Adolesc Med. 2002;156(6):607-614 [DOI] [PubMed] [Google Scholar]
- 12.Cook RL, Chung T, Kelly TM, Clark DB. Alcohol screening in young persons attending a sexually transmitted disease clinic: comparisons of AUDIT, CRAFFT, and CAGE instruments. J Gen Intern Med. 2005;20(1):1-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kelly TM, Donovan JE, Chung T, Cook RL, Delbridge TR. Alcohol use disorders among emergency-department treated older adolescents: a new brief screen (RUFT-Cut) using the AUDIT, CAGE, CRAFFT, and RAPS-QF. Alcohol Clin Exp Res. 2004;28(5):746-753 [DOI] [PubMed] [Google Scholar]
- 14.Babor TF, Higgins-Biddle JC, Saunders JB, Montiero MG. AUDIT The Alcohol Use Disorders Identification Test: Guidelines for Use in Primary Care 2nd ed.WHO Publication No. 01.6a Geneva, Switzerland: World Health Organization; 2001. http://whqlibdoc.who.int/hq/2001/WHO_MSD_MSB_01.6a.pdf Accessed May 4, 2009 [Google Scholar]
- 15.Reinert DF, Allen JP. The Alcohol Use Disorder Identification Test: an update of research findings. Alcohol Clin Exp Res. 2007;31(2):185-199 [DOI] [PubMed] [Google Scholar]
- 16.Graham A, Goss C, Xu S, Magid DJ, Diguiseppi C. Effect of using different modes to administer the AUDIT-C on identification of hazardous drinking and acquiescence to trial participation among injured patients. Alcohol Alcohol 2007Sep–Oct;42(5):423-429 Epub 2007 Mar 6 [DOI] [PubMed] [Google Scholar]
- 17.US Department of Health and Human Services, National Institutes of Health, National Institute on Alcohol Abuse and Alcoholism Helping Patients Who Drink Too Much: A Clinician's Guide: Updated 2005 Edition Rockville, MD: NIAAA Publications; 2005. http://pubs.niaaa.nih.gov/publications/Practitioner/CliniciansGuide2005/guide.pdf Accessed June 4, 2009 [Google Scholar]
- 18.Chung T, Colby SM, Barnett NP, Rohsenow DJ, Spirito A, Monti PM. Screening adolescents for problem drinking: performance of brief screens against DSM-IV alcohol diagnoses. J Stud Alcohol 2000;61(4):579-587 [DOI] [PubMed] [Google Scholar]
- 19.Knight JR, Sherritt L, Harris SK, Gates EC, Chang G. Validity of brief alcohol screening tests among adolescents: a comparison of the AUDIT, POSIT, CAGE and CRAFFT. Alcohol Clin Exp Res. 2003;27(1):67-73 [DOI] [PubMed] [Google Scholar]
- 20.Clark DB, Chung T, Martin CS. Alcohol use frequency as a screen for alcohol use disorders in adolescents. Int J Adolesc Med Health 2006;18(1):181-187 [DOI] [PubMed] [Google Scholar]
- 21.Kelly TM, Donovan JE, Chung T, Bukstein OG, Cornelius JR. Brief screens for detecting alcohol use disorder among 18-20 year old young adults in emergency departments: comparing AUDIT-C, CRAFFT, RAPS4-QF, FAST, RUFT-Cut, and DSM-IV 2-Item Scale. Addict Behav. 2009August;34(8):668-674 Epub 2009 Apr 2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Martin CS, Chung T, Langenbucher JW. How should we revise diagnostic criteria for substance use disorders in the DSM-V? J Abnorm Psychol. 2008;117(3):561-575 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fisher SL, Bucholz KK, Reich W, et al. Teenagers are right--parents do not know much: an analysis of adolescent-parent agreement on reports of adolescent substance use, abuse, and dependence. Alcohol Clin Exp Res. 2006;30(10):1699-1710 [DOI] [PubMed] [Google Scholar]
- 24.Ford CA, Millstein SG, Alpern-Felsher BL, Irvin CE., Jr Influence of physician confidentiality assurances on adolescents' willingness to disclose information and seek future health care. JAMA 1997;278(12):1029-1034 [PubMed] [Google Scholar]
- 25.Weddle M, Kokotailo P. Adolescent substance abuse: confidentiality and consent. Pediatr Clin North Am. 2002;49(2):301-315 [DOI] [PubMed] [Google Scholar]
- 26.Clark DB, De Bellis MD, Lynch KG, Cornelius JR, Martin CS. Physical and sexual abuse, depression and alcohol use disorders in adolescents: onsets and outcomes. Drug Alcohol Depend 2003;69(1):51-60 [DOI] [PubMed] [Google Scholar]
- 27.Clark DB, Lynch KG, Donovan JD, Block GD. Health problems in adolescents with alcohol use disorders: self-report, liver injury and physical examination findings and correlates. Alcohol Clin Exp Res. 2001;25(9):1350-1359 [PubMed] [Google Scholar]
- 28.Clark DB, Thatcher DL, Tapert SF. Alcohol, psychological dysregulation and adolescent brain development. Alcohol Clin Exp Res. 2008March;32(3):375-385 Epub 2008 Jan 30 [DOI] [PubMed] [Google Scholar]
- 29.Gogtay N, Giedd JN, Lusk L, et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc Natl Acad Sci U S A 2004May;101(21):8174-8179 Epub 2004 May 17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Cook RL, Clark DB. Is there an association between alcohol consumption and sexually transmitted diseases? A systematic review. Sex Transm Dis. 2005;32(3):156-164 [DOI] [PubMed] [Google Scholar]
- 31.Clark DB, Lesnick L, Hegedus AM. Traumas and other adverse life events in adolescent alcohol abuse and dependence. J Am Acad Child Adolesc Psychiatry 1997;36(12):1744-1751 [DOI] [PubMed] [Google Scholar]
- 32.Clark DB, Martin CS, Cornelius JR. Adolescent-onset substance use disorders predict young adult mortality. J Adolesc Health 2008June;42(6):637-639 Epub 2008 Mar 6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Yoon YH, Stinson FS, Yi HY, Dufour MD. Accidental alcohol poisoning mortality in the United States, 1996-1998. Alcohol Res Health 2003;27(1):110-118 [PMC free article] [PubMed] [Google Scholar]
- 34.Kaner EF, Beyer F, Dickinson HO, et al. Effectiveness of brief alcohol interventions in primary care populations. Cochrane Database Sys Rev. 2007(2):CD004148 [DOI] [PubMed] [Google Scholar]
- 35.Levy S, Vaughan BL, Knight JR. Office-based intervention for adolescent substance abuse. Pediatr Clin North Am. 2002;49(2):329-343 [DOI] [PubMed] [Google Scholar]
- 36.US Preventive Services Task Force Screening and behavioral counseling interventions in primary care to reduce alcohol misuse: recommendation statement. Ann Intern Med. 2004;140(7):554-556 [DOI] [PubMed] [Google Scholar]
- 37.Whitlock EP, Polen MR, Green CA, Orleans T, Klein J. Behavioral counseling interventions in primary care to reduce risky/harmful alcohol use by adults: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med. 2004;140(7):557-568 [DOI] [PubMed] [Google Scholar]
- 38.Kraemer KL. The cost-effectiveness and cost-benefit of screening and brief intervention for unhealthy alcohol use in medical settings. Subst Abus 2007;28(3):67-77 [DOI] [PubMed] [Google Scholar]
- 39.Solberg LI, Maciosek MV, Edwards NM. Primary care intervention to reduce alcohol misuse: ranking its health impact and cost effectiveness. Am J Prev Med. 2008;34(2):143-152 [DOI] [PubMed] [Google Scholar]
- 40.Knight JR, Sherrit L, Van Hook S, Gates EC, Levy S, Chang G. Motivational interviewing for adolescent substance use: a pilot study. J Adolesc Health 2005;37(2):167-169 [DOI] [PubMed] [Google Scholar]
- 41.Monti PM, Colby SM, Barnett NP, et al. Brief intervention for harm reduction with alcohol-positive older adolescents in a hospital emergency department. J Consult Clin Psychol. 1999;67(6):989-994 [DOI] [PubMed] [Google Scholar]
- 42.Stern SA, Meredith LS, Gholson J, Gore P, D'Amico EJ. Project CHAT: a brief motivational substance abuse intervention for teens in primary care. J Subst Abuse Treat 2007March;32(2):153-165 Epub 2006 Nov 22 [DOI] [PubMed] [Google Scholar]
- 43.D'Amico EJ, Miles JN, Stern SA, Meredith LS. Brief motivational interviewing for teens at risk of substance use consequences: a randomized pilot study in a primary care clinic. J Subst Abuse Treat 2008July;35(1):53-61 Epub 2007 Nov 26 [DOI] [PubMed] [Google Scholar]
- 44.Wynn SR, Schulenberg J, Maggs JL, Zucker RA. Preventing alcohol misuse: the impact of refusal skills and norms. Psychol Addict Behav. 2000;14(1):36-47 [DOI] [PubMed] [Google Scholar]
- 45.Doumas DM, McKinley LL, Book P. Evaluation of two Web-based alcohol interventions for mandated college students. J Subst Abuse Treat 2009January;36(1):65-74 Epub 2008 Jul 26 [DOI] [PubMed] [Google Scholar]
- 46.Clark DB, Wood DS, Cornelius JR, Bukstein OG, Martin CS. Clinical practices in the pharmacological treatment of comorbid psychopathology in adolescents with alcohol use disorders. J Subst Abuse Treat 2003;25(4):293-295 [DOI] [PubMed] [Google Scholar]
- 47.Anton RF, O'Malley SS, Ciraulo DA, et al. COMBINE Study Research Group Combined pharmacotherapies and behavioral interventions for alcohol dependence: the COMBINE study: a randomized controlled trial. JAMA 2006;295(17):2003-2017 [DOI] [PubMed] [Google Scholar]
- 48.Richardson K, Baillie A, Reid S, et al. Do acamprosate or naltrexone have an effect on daily drinking by reducing craving for alcohol? Addiction 2008;103(6):953-959 [DOI] [PubMed] [Google Scholar]
- 49.Cornelius JR, Bukstein OG, Wood DS, Kirisci L, Douaihy A, Clark DB. Double-blind placebo-controlled trial of fluoxetine in adolescents with comorbid major depression and an alcohol use disorder. Addict Behav. doi: 10.1016/j.addbeh.2009.03.008. [published online ahead of print March 12, 2009] [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Riggs PD, Mikulich-Gilbertson SK, Davies RD, Lohman M, Klein C, Stover SK. A randomized controlled trial of fluoxetine and cognitive behavioral therapy in adolescents with major depression, behavior problems, and substance use disorders. Arch Pediatr Adolesc Med. 2007;161(11):1026-1034 [DOI] [PubMed] [Google Scholar]
- 51.Bukstein O. Substance abuse in patients with attention-deficit/hyperactivity disorder. Medscape J Med. 2008;10(1):24 [PMC free article] [PubMed] [Google Scholar]
- 52.Walters ST, Hester RK, Chiauzzi E, Miller E. Demon rum: high-tech solutions to an age-old problem. Alcohol Clin Exp Res. 2005;29(2):270-277 [DOI] [PubMed] [Google Scholar]
- 53.Spandorfer JM, Israel Y, Turner BJ. Primary care physicians' views on screening and management of alcohol abuse: inconsistencies with national guidelines. J Fam Pract. 1999;48(11):899-902 [PubMed] [Google Scholar]
- 54.McLellan AT, Meyers K. Contemporary addiction treatment: a review of systems problems for adults and adolescents. Biol Psychiatry 2004;56(10):764-770 [DOI] [PubMed] [Google Scholar]
- 55.Bukstein OG, Working Group on Quality Issues Summary of the practice parameters for the assessment and treatment of children and adolescents with substance use disorders. J Am Acad Child Adolesc Psychiatry 1998;37(1):122-126 [DOI] [PubMed] [Google Scholar]
- 56.D'Amico EJ, Paddock SM, Burnam AU, Kung FY. Identification of and guidance for problem drinking by general medical providers: results from a national survey. Med Care 2005;43(3):229-236 [DOI] [PubMed] [Google Scholar]
- 57.Rochat S, Wietlisbach V, Burnand B, Landry U, Yersin B. Success of referral for alcohol dependent patients from a general hospital: predictive value of patient and process characteristics. Subst Abus 2004;25(1):9-15 [DOI] [PubMed] [Google Scholar]
- 58.Zanjani F, Miller B, Turiano N, Ross J, Oslin D. Effectiveness of telephone-based referral care management, a brief intervention to improve psychiatric treatment engagement. Psychiatr Serv. 2008;59(7):776-781 [DOI] [PubMed] [Google Scholar]
- 59.Clark DB, Thatcher DL, Maisto SA. Supervisory neglect and adolescent alcohol use disorders: effects on AUD onset and treatment outcome. Addict Behav 2005October;30(9):1737-1750 Epub 2005 Sep 2 [DOI] [PubMed] [Google Scholar]