To the Editor: Manivannan et al1 published a useful case of apical ballooning syndrome (ABS) after intravenous administration of epinephrine for anaphylaxis. The authors rightly underscored that high doses of intravenous epinephrine may induce ABS. However, specific concerns are warranted regarding some key points. Specifically, ABS occurring after anaphylaxis seems to be related to inappropriate use of epinephrine, including intravenous and intramuscular injections as well as high or low doses.
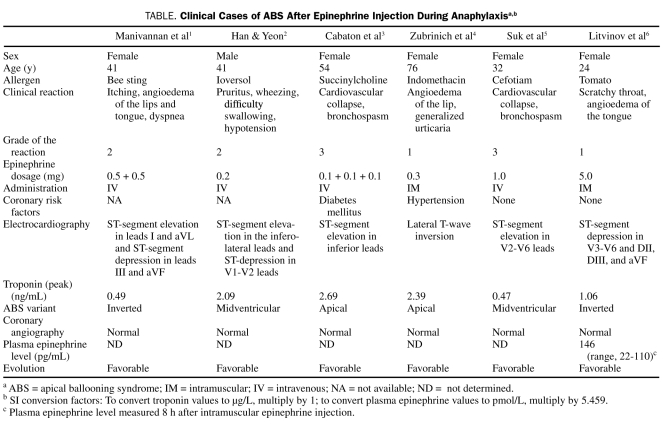
Five clinical cases have been reported for ABS after epinephrine administration for anaphylaxis (Table).2-6 Han and Yeon2 reported the first case, in which 0.2 mg of epinephrine was intravenously injected during moderate anaphylaxis. The authors considered that the midventricular hypokinesis was related to a cardiac manifestation of anaphylaxis. Cabaton et al3 and Suk et al5 reported ABS after perioperative anaphylaxis. Cabaton et al3 showed that epinephrine, even when injected at low intravenous doses, may have been involved in the occurrence of ABS. In this case, the 2 last boluses of epinephrine (0.1 mg × 2) were injected after generalized cutaneous signs appeared (indicating hemodynamic restoration) and were immediately followed by ventricular fibrillation. Suk et al5 reported ABS after a high dose (1 mg) of intravenous epinephrine associated with a norepinephrine infusion. The authors suggested that excessive catecholamine surges in response to anaphylaxis and/or to the administration of exogenous catecholamines may have played a role in the ABS occurrence. In the case published by Manivannan et al,1 2 intravenous doses of 0.5 mg of epinephrine were injected in the absence of cardiovascular disturbances. Hypotension occurring after the first bolus of epinephrine was related to an adverse cardiac response to epinephrine.
TABLE.
Clinical Cases of ABS After Epinephrine Injection During Anaphylaxisa,b
Zubrinich et al4 and Litvinov et al6 reported ABS after intramuscular injection of epinephrine. The former concluded that, given the mild clinical presentation, epinephrine (0.3 mg) should not have been used.4 The latter confirmed a direct causal role for suprapharmacologic doses of exogenous epinephrine (5 mg) in the pathophysiology of ABS.6
The dangers of epinephrine administration outside the context of severe anaphylaxis have been highlighted by the reports of serious outcomes. Recently, pharmacologic and suprapharmacologic doses of epinephrine have been reported to induce one of the 3 ABS variants.6 The catechol O-methyltransferase genotype and intense psychological stress may also influence predisposition to ABS.1,6 Finally, all the reported patients1-6 fulfilled Mayo Clinic criteria for ABS.1
Thus, as suggested during perioperative anaphylaxis, treatment may be initiated according to a 4-step clinical grading scale.7 Whereas grade 1 involves cutaneous-mucous signs in which epinephrine should never be injected, grade 2 corresponds to mild cutaneous-mucous features that may be associated with cardiovascular and/or respiratory signs for which titrated intravenous boluses (0.01-0.02 mg) of epinephrine may sometimes be necessary. The hallmark of grade 3 is cardiovascular collapse that may be associated with cutaneous-mucous signs and/or bronchospasm; titrated intravenous bolus administration of epinephrine (0.1-0.2 mg) is required and should be renewed if necessary. Finally, grade 4 is cardiac arrest that requires high doses of epinephrine, as warranted during cardiopulmonary resuscitation.
The important issue is not the route of epinephrine administration, but its appropriate use during anaphylaxis. Consequently, these cases emphasize the need for careful patient selection and titration of epinephrine when the clinical situation dictates its use.
References
- 1.Manivannan V, Li JTC, Prasad A, Campbell RL. Apical ballooning syndrome after administration of intravenous epinephrine during an anaphylactic reaction [letter]. Mayo Clin Proc. 2009;84(9):845-846 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Han Y, Yeon S. Midventricular hypokinesis as a cardiac manifestation of anaphylaxis: a case report. J Am Soc Echocardiogr. 2006;19(12):1529.e9-e11 [DOI] [PubMed] [Google Scholar]
- 3.Cabaton J, Rondelet B, Gergele L, Besnard C, Piriou V. Tako-tsubo syndrome after anaphylaxis caused by succinylcholine during general anaesthesia. Ann Fr Anesth Reanim. 2008;27(10):854-857 [DOI] [PubMed] [Google Scholar]
- 4.Zubrinich CM, Farouque HM, Rochford SE, Sutherland MF. Takotsubo-like cardiomyopathy after EpiPen administration. Intern Med J. 2008;38(11):862-865 [DOI] [PubMed] [Google Scholar]
- 5.Suk EH, Kim DH, Kweon TD, Na SW, Shin JA. Stress-induced cardiomyopathy following cephalosporin-induced anaphylactic shock during general anesthesia. Can J Anaesth. 2009;56(6):432-436 [DOI] [PubMed] [Google Scholar]
- 6.Litvinov IV, Kotowycz MA, Wassmann S. Iatrogenic epinephrine-induced reverse Takotsubo cardiomyopathy: direct evidence supporting the role of catecholamines in the pathophysiology of the “broken heart syndrome.” Clin Res Cardiol. 2009;98(7):457-462 [DOI] [PubMed] [Google Scholar]
- 7.Dewachter P, Mouton-Faivre C, Emala CW. Anaphylaxis and anesthesia: controversies and new insights. Anesthesiology 2009;111(5):1141-1150 [DOI] [PubMed] [Google Scholar]