Abstract
Various rural prevention research challenges have been articulated through a series of sessions convened since the mid 1990s by the National Institutes of Health, particularly the National Institute on Drug Abuse. Salient in this articulation was the need for effective collaboration among rural practitioners and scientists, with special consideration of accommodating the diversity of rural areas and surmounting barriers to implementation of evidence-based interventions. This paper summarizes the range of challenges in rural prevention research and describes an evolving community-university partnership model addressing them. The model entails involvement of public school staff and other rural community stakeholders, linked with scientists by Land Grant University-based Extension system staff. Examples of findings from over 16 years of partnership-based intervention research projects include those on engagement of rural residents, quality implementation of evidence-based interventions, and long-term community-level outcomes, as well as factors in effectiveness of the partnerships. Findings suggest a future focus on building capacity for practitioner-scientist collaboration and developing a network for more widespread implementation of the partnership model in a manner informed by lessons learned from partnership-based research to date.
In the mid 1990s, the National Institute on Drug Abuse (NIDA) and other National Institutes of Health (NIH) entities (eg, the National Institute of Mental Health) convened panels, supported workshops, and issued publications to foster development of the subfield of rural-based preventive research.1,2 In part, the intent of these efforts was to assess research needs—to articulate a research agenda for this subfield and to identify related issues and challenges.
A wide range of rural prevention research needs were identified through this process,3-7 including: (1) investigation of intervention implementation barriers in rural areas, including the recruitment, engagement, and retention of rural residents for preventive interventions6,8,9; (2) conduct of rigorous research on community outcomes of promising preventive interventions with rural populations10; and (3) examination of factors in and benefits of effective community-based collaborative research with rural residents, guided by models such as the Preventive Intervention Research Cycle and others addressing participatory research.11 As an indication of the need for additional research, a late 1990s literature review revealed only 2 randomized controlled studies with general populations of rural families.9,12
In addition to highlighting challenges in meeting the above specified research needs, this paper also will present: (1) a community-university partnership model that addresses those challenges; (2) illustrative findings from implementation of this partnership model; and (3) future directions suggested by those findings. The focus will be on elaborating what was initially presented at a NIDA workshop session titled “Prevention Research Partnerships and Rural Community Service Infrastructure: Challenges and Opportunities,” included as part of the set of workshop sessions upon which this special issue is based. Primarily, the focus will be on one of the key recommendations for addressing the research needs emerging from the rural-based prevention panels noted above; specifically, the development of effective models for collaboration between intervention researchers and rural community practitioners, together with other community stakeholders. Elaboration of these recommendations has included evaluation of the prospects for research based in existing rural intervention delivery systems such as the Cooperative Extension System9,11 and other types of innovative partnerships,4 with an eye toward translation of research into ongoing rural community practice.
Challenges to Rural Prevention Research
In order to set the stage for presenting the development of the community-university partnership model and findings from resultant research that follow, this section will identify and discuss selected challenges in meeting rural prevention research needs.
General Challenge of Collaboration and Capacity Building
As part of the NIH efforts noted above, one of the tasks was to delineate challenges and future directions for moving this subfield of rural prevention research forward, as described in a 1997 NIDA Monograph and in a 1997 special issue of the American Journal of Community Psychology. Judged to be central to positive future developments was effective collaboration between researchers and community-based practitioners that is ecologically valid and sensitive to local needs,13 a judgment underscored in the recent NIDA-sponsored workshop on Drug Abuse Research in Rural Communities.14-16
The natural tensions in scientist-practitioner partnerships are sufficiently challenging that the American Journal of Community Psychology recently has devoted a special issue to the topic (Volume 35, 2005). Salient among the tensions discussed are basic ones such as fundamental differences between practitioners’ and researchers’ goals and methods. Generally, scientists have more emphasis on basic science and the incremental advancement of knowledge—as opposed to practitioners’ focus on addressing community needs and improving local quality of life. Typically, scientists use cautious, methodical approaches, whereas practitioners’ goals often are pursued through timely, real-world community action. Another factor renders it quite difficult to overcome these natural tensions. That is, frequently neither universities nor local service delivery agencies provide adequate support or rewards for the substantial efforts required to collaborate. For example, university-based scientists’ career advancement is frequently based primarily on traditional disciplinary activities, such as publishing in scientific journals.17 In cases where the university does provide support for researcher involvement, community practitioners may be involved on a volunteer basis, thereby leading the practitioners to conclude that their time and efforts are less valued.
A number of practitioners and scientists have discussed these scientist-practitioner tensions and have suggested various types of collaborations and partnerships to address them.18,19 These tensions are contemplated and addressed by the guiding principles of community participatory research.14,20,21 In addition to the treatment of community as a unit, these principles emphasize: (1) building on community strengths and resources; (2) closely integrating scientific knowledge-building and community actions, incorporating the values and perspectives of both science and practice; (3) collaborating across multiple phases of research; and especially, (4) enhancing skills, competencies, and social capital among community residents. These principles are incorporated by the partnership model described subsequently.
A frequently cited challenge in the relevant literature from the mid 1990s was the need for the development of community capacity and infrastructure that addressed both barriers to intervention implementation and to the conduct of rigorous intervention research. Capacity building was indicated as especially necessary to overcome barriers concerning limited availability and accessibility of evidence-based services and to further develop the limited research conducted in rural communities. Research in rural communities faces a problem similar to that encountered with prevention research in urban settings; that is, developing local capacity to sustain interventions and intervention evaluation after the initial research is completed and there is no more funding.
Rural Research Challenges of Definitions and Diversity
A clear case was made in the NIDA monograph and the American Journal of Community Psychology special issue that collaboration and intervention research were rendered more challenging by (1) inconsistencies in the use of the term “rural,”22 (2) the diversity of rural America,23 and (3) the diverse mechanisms by which services in a rural area can affect the epidemiology of a public health problem.24-27 Recurrent questions raised in related discussions include “What is meant by ‘rural’?” and “What about ‘rural’ really matters in the etiology of problems addressed by preventive interventions?” For example, the ultimate goal of researchers to disseminate generalizable research findings is made more difficult by inconsistencies in the literature regarding rural setting and population classification schemes. Also, culturally competent interventions tailored to particular populations or types of rural area are very limited.15,28,29 These challenges present difficulties when researchers’ intend to generalize findings or to standardize interventions across similar types of settings and populations.
Related Challenges With Evidence-Based Intervention
Evidence-based interventions present special challenges to both practitioners and scientists working in rural areas,30 including the insufficient number of evidence-based interventions to adequately address all populations and settings, as well as the resource requirements for evidence-based intervention implementation. As defined here, evidence-based interventions are interventions founded upon a strong theory base that target clearly specified populations and outcomes, employ psychometrically sound measurement of outcomes, and focus on rigorous evaluation of outcomes, preferably using randomized, controlled studies. A major challenge is the dissemination of available evidence-based interventions, particularly in rural areas, as has been discussed in recent reports. For example, only 8% of 54 evaluated interventions in the statewide Youth Strategies Initiative in Maryland had an evidence base and high fidelity in the first year of operation.31 Ennett and colleagues surveyed 1,795 middle schools and found that only 14% of school-based interventions had both effective content and delivery.32 Further, 12 community coalitions implementing 18 substance abuse prevention strategies rarely chose evidence-based interventions in Hallfors’ and colleagues’ study of the Fighting Back Coalitions.33
Despite the availability of an increasing number of evidence-based interventions, there is little evidence of successful dissemination (Peter Nathan, University of Iowa, personal communication, July 2003). There also is limited knowledge about economic and social factors influencing program and service utilization in rural areas34,35; especially little is known about evidence-based intervention delivery in diverse rural settings.36 One striking fact about the state of the art is that evidence-based intervention implementation rates are low even with a considerable level of encouragement, guidance, and technical assistance to the community coalitions involved. Importantly, as indicated by the studies cited above, where evidence-based interventions are implemented, there is limited sustainability of implementation over time.
Community-University Partnership Model
Because of keen interest in addressing rural practitioner-research collaboration, capacity-building, and related challenges, a number of prevention scientists have been especially intent on grounding research in existing rural intervention delivery systems and in clarifying what types of system- and organizational-level change will be necessary to support and sustain community-university partnerships.11,13,37,38 In the case of our program of research, we have been particularly interested in strengthening the linkages among the rural-serving, Land Grant University-based Cooperative Extension System, the public school system, and other service delivery or resource systems. For example, we are assessing how University Extension agents can link with organization change agents within school systems who are responsible for prevention programming, in order to collaboratively incorporate such programs into comprehensive school plans that are tied to school system accountability mechanisms. From this perspective, we are clarifying ways to integrate our prevention partnership work with ongoing school reform efforts.
Molgaard and colleagues11,39 summarize potential benefits that could accrue to rural communities through Extension-assisted preventive intervention research and research supported by community-university partnerships.39 There is tremendous opportunity in linking the Extension and public school systems with social service delivery systems, in large measure because of their existing capacity for intervention delivery and partnering in intervention research. Specifically, the Cooperative Extension System has been characterized as the largest informal education system in the world.11,40 It has over 3,150 agents in nearly every county in the United States and agents are typically highly educated. Importantly, the Extension System was founded on principles encouraging a science-with-practice orientation.41 Complementing these features, the public school system is a universal program delivery system reaching nearly all children. Furthermore, each state has networks for public education programming support and as a whole there has been increasing emphasis on accountability and an empirical orientation.38 Nonetheless, the scientist-practitioner tensions summarized in the introduction also are in evidence in the Cooperative Extension and public school systems; the projects subsequently described illustrate some progress in addressing these tensions.
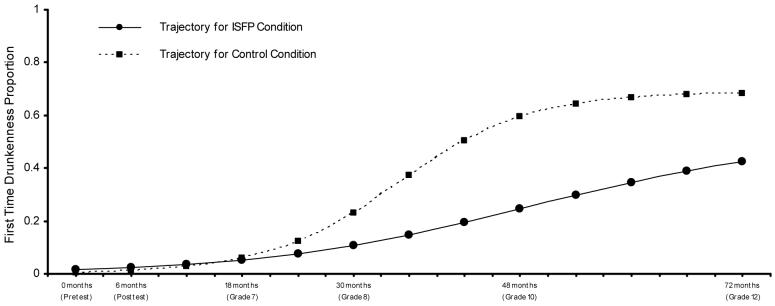
The purpose of the Extension-assisted program of research subsequently described is to expand the knowledge base on the effectiveness of preventions positive youth development and health promotion interventions for youth, adults, families, and communities, with emphasis on community-university partnership approaches to the dissemination of evidence-based interventions. This program of research is being pursued by the Partnerships in Prevention Science Institute (www.ppsi.iastate.edu) at Iowa Sate University. Projects at the Institute have been funded primarily by 3 institutes at the National Institutes of Health (National Institute on Drug Abuse, National Institute on Alcoholism and Alcohol Abuse, and National Institute of Mental Health), and they have been conducted in collaboration with other state universities. All together there have been 17 studies funded by series of grants. Illustrative findings from the primary, ongoing randomized prevention studies are presented below. A timeline for these studies is provided in Figure 1. In chronological order, they are called Project Family (including both a pilot study and a trial), CaFaY (Capable Families and Youth), and PROSPER (PROmoting School-community-university Partnerships to Enhance Resilience). Figure 1 outlines starting points for each major project, along with the timing of interventions and the initiation of longitudinal assessments for each of the projects.
Figure 1. Timeline for Primary Partnership-Based, Randomized Studies and Their Key Intervention and Data Collection Activities.
Note: Only starting points for interventions are depicted; CaFaY and PROSPER elective booster sessions were offered after the initial “core” programs were implemented in the specified school grades. Each project had pretest assessments during the fall semester, followed by the specified interventiions, with posttest assessments approximately six months following the pretest (in the spring semester). Assessments continue on a yearly basis following the pottest assessments. Project Family conducted in-home questionnaires and video-taped interviews only. CaFaY conducted in-school, classroom-based questionnaire assessments, with a selected subsample participating in in-home assessments. PROSPER conducted community team process interviews and school resource assessments, along with school-based and in-home assessments.
Three Generations of Partnerships
Land Grant Extension-assisted partnerships have evolved across 3 generations. Our evaluation of community-based interventions began with a first-generation structure for collaborative research and program implementation in Project Family. That is, we worked with local Extension agents early in the process to hire and coordinate other local school staff and program facilitators, who would, in turn, closely coordinate with those of us at the university to implement and evaluate the evidence-based interventions we selected for study. Through experience, we have learned how helpful it is to involve Extension agents who could act as intermediaries at the state’s regional level and assist us in coordinating our intensive program implementation and evaluation work across communities. This led to a second-generation, 3-tier partnership structure for the CaFaY project. This second-generation partnership, however, entailed only a loosely knit group of local residents who helped with organization and implementation of the intervention but did not function as a local team in the traditional sense (eg, with regularly scheduled meetings).
Inspired by successes of the projects based in the first 2 generations of partnerships, we co-hosted a conference42 that lead to the design for the third generation of partnerships incorporating community teams. This third-generation partnership model is being evaluated through a collaborative project conducted with the Pennsylvania State University called PROSPER. A somewhat unique feature of the PROSPER community teams is that they are relatively small in size, especially compared with the so-called “big tent” community coalitions. These teams are designed to be very strategic with very focused intervention goals. One of their major tasks is to select for implementation in their community both a family-focused and school-based intervention chosen from a menu of evidence-based interventions.
To briefly summarize a theoretical framework underpinning the partnership model, Diffusion of Innovation Theory43 describes a change agent linking function that entails connecting “resource systems” with clients or consumers of those resource systems. We emphasize the related, systems-level function of building and sustaining capacity through coordinated efforts of agents serving different but interrelated roles in public education systems. Our partnership model promotes the linking of agents devoted to intervention-related capacity-building within a public school to external agents who share the same intervention goals, while building the overall capacity of the partnerships to meet the shared intervention goals.
Within this framework, an internal capacity-building agent in a public school system generates, coordinates, and sustains resources within that organization for the “clients” of evidence-based interventions—in this case, students in public schools and their family members—with the idea of building capacity for intervention on an ongoing basis. External resource systems agents are those from agencies outside of public schools, both within the state public education system—the state university, state department of education, and area education agencies—and in the local community (eg, human service providers). These agents from resource systems external to the public schools generate, coordinate, and provide intervention training, technical assistance, and evaluation. The linking agents in our framework are from the Land Grant University Extension system. This system provides agents who are accessible to communities throughout the state who, as part of their routine work, can link schools’ internal capacity-builders and sustainers with their external resource providers. Thus, these linking agents provide both local and horizontal linkages (eg, internal or school-based agents with external representatives of community agencies), and vertical linkages (eg, school agents with regional or state-level technical assistants).
The organizational structure for the third-generation partnership model is outlined in Figure 2. Local teams (including the public school, Extension, and local resource people described above) receive support from an intermediate-level coordinator team—one that includes Prevention Coordinators based in our university outreach or Extension system. They provide continuous, proactive technical assistance, as well as documentation of ongoing partnership processes. Both local and coordinating teams receive resources and support from a state-level team—including prevention scientists. The primary functions of this state-level team are to provide administrative oversight, offer input on data collection and analyses, and draft project reports.
Figure 2. Third Generation Organizational Structure for State Public Education Partnerships.
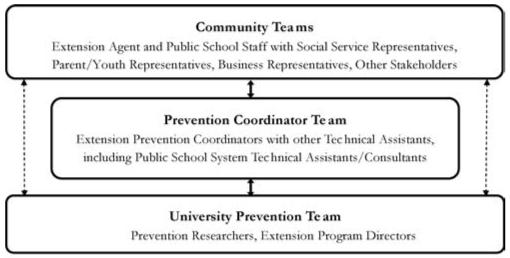
*Note: Dased lines represent intermittent direct contact; solid lines represent regular direct contact. These partnerships are presently called PROSPER Partnerships (PROmoting School/community-university Partnerships to Enhance Resilience).
Reprinted with the kind permission of Springer Publishing. Spoth R, Greenberg M, Bierman K, Redmond C. PROSPER Community-university partnership model for public education systems: capacity-building for evidence-based, competence-building prevention. Prevention Science. 2004, fig 2;5:31-39.
Illustrative Findings
To date, our community-university partnerships in rural areas have produced findings that underscore the opportunities represented by the public education collaborative framework. These findings will be mapped onto the 3 research needs cited in the opening paragraphs of this article: (1) investigation of implementation barriers in the delivery of community-level evidence-based interventions; (2) research on community-level outcomes through partnership-delivered evidence-based interventions; and (3) evaluation of factors in effective community-university partnerships, especially concerning implementation quality, partnership-based intervention outcomes, and intervention sustainability.
Findings From Research on Intervention Implementation
As extensive literature has clarified, program implementation quality is a major issue in community-based programming.44-46 A key indicator of quality implementation is adherence to intervention protocols. We typically address adherence through observer fidelity ratings. Essential content of the interventions is delineated on observer rating sheets and observers record whether or not that content was delivered. The proportion of sessions observed typically ranges from about 20% to 60%, depending on the total number of sessions and whether the focus is on a school or family program. Our findings indicate that high levels of adherence are achievable for family- and school-based universal interventions. In the community-university partnership projects, the adherence rates have been consistently high, recently averaging over 90% adherence for both family programs and school-based programs.47 The community-university partnerships increase implementation quality by helping with selection of effective implementers, increasing the quality of training, increasing culturally competent intervention, and increasing user friendliness of material.
A number of implementation and participation barriers typically encountered, such as travel distance, travel-related time demands, and scheduling conflicts, become especially relevant in conducting family-focused interventions in rural settings. For these reasons, we have developed a program of research incorporating consumer-research methods that seek to clarify factors that influence participation in preventive interventions. The resultant knowledge serves to inform the development of participation strategies that increase the reach of prevention efforts. Two earlier articles provide an overview of those findings.48,49 One of the key conclusions from this research is that implementers should be guided by input from prospective intervention consumers in choosing how to devote the necessary resources to recruitment and retention, regardless of whether the objective is to involve representative samples or to maximize local population participation.50 It follows that local implementers need to develop effective strategies for garnering the substantial resources necessary to promote participation. A related conclusion is that local implementers need to provide participation incentives51 and accommodate busy schedules to minimize time demands on participants, possibly entailing multiple schedule options.48 Importantly, empirical study has confirmed that local teams functioning as part of a community-university partnership with proactive technical assistance and employing such strategies are successful in sustaining evidence-based intervention recruitment.52
We have been keenly interested in retaining both lower- and higher-risk families in our research projects and interventions. We examined our project retention by constructing a composite risk index consisting of socioeconomic status, parent internalizing and externalizing problems, child internalizing and externalizing problems, and parent-child interaction distress based on observer ratings. A number of studies demonstrate our ability to retain higher- and lower-risk families equally well.53,54
As Biglan and others have noted, intervention dissemination research also requires careful attention to recruitment, engagement, and retention at the organizational level.55 We now have a long history of recruitment and retention of our public schools, across 6 randomized controlled studies, and 11 supplemental studies. It is noteworthy that 106 public schools have been involved in the randomized controlled studies that we have conducted to date. Ninety percent of all schools were successfully recruited, and 98% of those schools were retained. In fact, in one study, 100% of participating schools were retained over 8 years.
Rigorous Research on Long-Term Community-Level Outcomes
Some findings from our longest running partnership-based program outcome evaluation study are illustrative. This study, referenced earlier and called the Project Family Trial, entailed the random assignment of 33 rural Iowa schools to 3 experimental conditions: the Iowa Strengthening Families Program, Preparing for the Drug Free Years Program, and a Minimal Contact Control. All rural communities had populations of 8,500 or less, with most having populations of less than 2,500. All families of 6th graders were invited to participate. For the sake of brevity, a subset of outcomes will be briefly summarized, with a specific focus on those associated with the Iowa Strengthening Families Program (ISFP).56
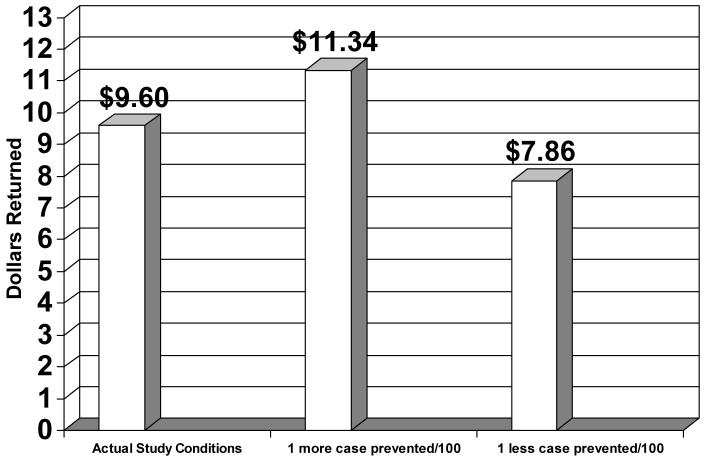
We have examined growth of substance initiation from the 6th grade pretest assessment through to the 12th grade follow-up. The pattern of growth in use of “substances of choice,” such as alcohol, follows a curvilinear growth pattern, with an initially slow rate of growth that next rapidly increases, followed by return to a slower growth rate in the later years of high school. When we were evaluating outcomes through the 12th grade, we needed to accommodate this particular growth pattern in our analyses. The estimated growth curves for the ISFP and control conditions were statistically different with respect to the growth parameters that described youth trajectories of substance use over time. These differences are illustrated for the case of lifetime drunkenness, as depicted in Figure 3. Lower intensity alcohol-related initiation measures (such as lifetime use of alcohol) exhibited similar patterns, but with steeper growth at earlier ages.57
Figure 3. Partnership-Based Iowa Strengthening Families Program: Lifetime Drunkenness Through 6 Years Past Baseline.
Note: Based on data reported in a Research Update entitled, “PROSPER project overview: Sustainability partnership model for large-scale prevention of underage drinking.” Presented to the National Institute on Alcohol Abuse and Alcoholism, Bethesda, MA (October, 2005).
Other analyses from the Project Family prevention trial have focused on the average age of students in each condition at which the students in that condition reach a given prevalence rate on a range of lifetime use measures. Basically, these analyses allow comparisons of the point at which a certain percentage of students in the intervention or control conditions have progressed from a negative to a positive history of use for a particular substance or substance use behavior. For example, in the case of the lifetime drunkenness measures, the ISFP group did not attain a 50% prevalence rate until more than 2 years after the control group.57
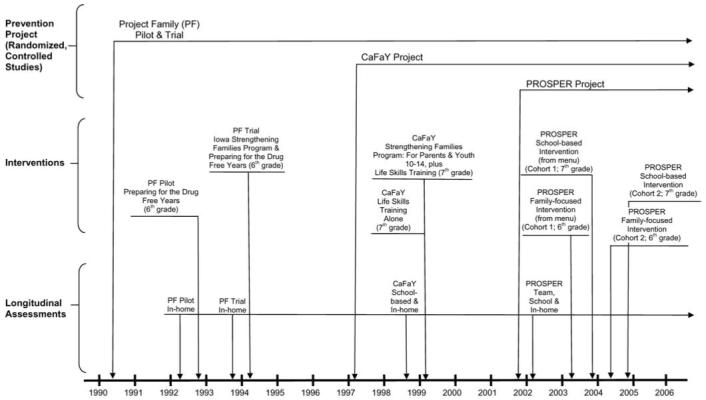
Analyses of economic benefits also were instructive. We used data on intervention effects on the delay of onset in alcohol use—along with data on (1) the relation between delayed onset of alcohol use in adolescence and alcohol use disorders in adulthood, and (2) the societal costs avoided by preventing adult alcohol use disorders—to estimate benefit-cost ratios. Figure 4 shows the estimated return for each dollar invested in the ISFP under actual study conditions. Figure 4 also shows the expected changes in the dollars returned when the number of adult alcohol use disorders prevented per 100 participants is increased and decreased by 1. The fact that the estimates remain well above zero suggests the robustness of the conclusion that the preventive intervention constituted a fiscally sound investment.58
Figure 4. Partnership-Based Iowa Strengthening Families Program: Benefit-Cost Ratios Under Different Assumptions.
Note: Based on a subset of tabular data presented in Spoth, R., Guyll, M., & Day, S. X. (2002). Universal family-focused interventions in alcohol-use disorder prevention: Cost-effectiveness and cost-benefit analyses of two interventions. Journal of Studies on Alcohol, 63(2), 219-228
The most recent outcome evaluation addresses methamphetamine use. Methamphetamine use has recently increased dramatically among adolescents, with 2003 prevalence rates almost 5 times higher than in 1992.59-61 Researchers have noted that adolescents in smaller towns and rural areas are particularly vulnerable to methamphetamine use, given potentially powerful peer influences in rural environments and the appeal of stimulants to rural youth.62 The threat to adolescents in the rural Midwest has been particularly acute.63-65 Project Family Trial and the CaFaY prevention trial are now showing that partnership-based universal interventions for families and students in schools can significantly reduce lifetime or past-year methamphetamine use up to 6.5 years past baseline.66
A number of additional findings reveal the benefits of preventive interventions, including: long-term conduct/behavior problem reduction (eg, 40% fewer aggressive and destructive behaviors by 10th grade);67 positive youth protective factor and skills-building outcomes (eg, significant improvements in relationships with parents, refusals of offers from peers to use alcohol;68,69 and long-term positive effects on school engagement and academic success (eg, increased grade point average).70
Current Findings on Partnership Processes and Outcomes
Current literature reviews suggest a dearth of studies that address the third set of research needs noted in the introduction, specifically, those concerning factors that influence community partnerships in their efforts both to overcome barriers to quality implementation of evidence-based interventions and to produce positive community-level outcomes, especially in terms of long-term reductions in problem behaviors. To address this need we have designed the PROSPER study, the primary aims of which are to evaluate the effectiveness of partnership implementation of evidence-based interventions on youth and family outcomes, in terms of long-term reductions in problem behaviors, and to learn what factors are most important in partnership effectiveness, particularly sustained, quality implementation.
The centerpiece of the project is a study that has random assignment of 28 school districts in Iowa and Pennsylvania, with 2 successive cohorts of participants, starting with a total of over 12,000 students in the 6th grade. To briefly summarize the primary activities initially undertaken by PROSPER’s local teams, they include: (1) recruiting members and building local teamcohesion; (2) considering local needs and resources for program implementation; and (3) selecting from a menu of evidence-based interventions (both family-focused and school-based programs). Early findings on the sustainability of implementation quality and the sustainability of the interventions themselves have been very encouraging. There have been: high levels of general population recruitment across states;52 high implementation quality (>90% adherence) sustained over 1 year;47 and demonstrated capacity building for local team fundraising, with 100% of community teams securing funding for continued programming. Finally, key factors in the positive functioning of community teams (eg, perceived value of prevention, team member collaborative experience) have been identified.71,72 Most importantly, positive outcomes have been observed at 1.5 years past baseline, for family functioning, youth competencies, and reduction in youth substance use.73
Capacity Building and a Partnership Research Network
The ultimate purpose of addressing the research needs described in the introduction is to move closer to larger-scale rural community benefits from preventive interventions. As described earlier, there are many obstacles to surmount. As summarized, a model for community-public school partnerships with land grant universities has guided some initial steps in expanding the relevant knowledge base and suggests some opportunities and benefits in further implementation and evaluation of the partnership model. Partnership-based research should be combined with efforts to increase capacity for dissemination of evidence-based interventions on a larger scale, in order to achieve larger-scale benefits to community health and well-being. As noted in the earlier discussion of evidence-based interventions, there has been very limited dissemination and, indeed, there exists little capacity for dissemination, particularly in rural communities.36 Thus, for dissemination purposes, capacity building to coordinate a network of community-university partnerships across a large number of rural communities is indicated; this network would constitute a fourth-generation partnership model.
In addition to further development of the theoretical models necessary to guide dissemination efforts, it will be important to develop a comprehensive strategic framework for capacity building. Many have called for capacity building that would help achieve sustained, quality implementation of prevention-oriented evidence-based interventions, and some general frameworks have been suggested for that purpose.74-76 Nonetheless, comprehensive strategies for large-scale evidence-based intervention implementations are quite limited. Related strategies lack comprehensiveness in a number of ways (such as in focusing on a single type of youth problem, failing to address positive youth development, failing to address necessary resources and agency coordination, and limited partnering of practitioners and scientists). A comprehensive strategy for capacity building for larger-scale preventive intervention research and implementation will require further attention to research issues (eg, culturally competent intervention research, study of sustainability under conditions of limited resources) and relevant policy change issues, as previously described.38 Central to a comprehensive strategy for capacity building is the development of a network of effective community partnerships for sustained, quality evidence-based intervention implementation, and related multisite community research. Such a network could function like interorganizational networks that foster diffusion of innovations,43 but would require extensive infrastructure development. Examples of projects working toward this end are provided by Spoth and Greenberg38 and include the Healthy People 2010 Project.77
Work directed toward capacity building for partnership-based dissemination of evidence-based interventions in land grant universities would benefit from consideration of some lessons learned from our experience with Cooperative Extension System-assisted partnerships. First, it is important to underscore how the aforementioned Cooperative Extension System science-with-practice orientation and the existing infrastructure to support the integration of science with practice have provided fertile ground for growing our partnership-based program of research funded by the NIH. Early in the history of this line of investigation, the existing research-to-practice orientation and the infrastructure supporting it contributed greatly to a state of readiness for our type of collaborative preventive intervention research. Another critically important condition for our partnership-based research has been administrative support garnered for conducting the research, eventually including contributed funding for supporting key Extension staff positions as well as administrative champions for the work. In retrospect, it appears that these conditions combined to create a helpful synergy between the land grant university Cooperative Extension System and the NIH-funded program of research—one that has given impetus to the production of the range of positive results reported earlier.
Other lessons learned through the effort to implement a partnership-based program of research concern barriers to this type of collaborative research. Examples include (1) competing demands on Cooperative Extension System staff, (2) staff incentive structures that are not optimally conducive to collaborative research, and (3) difficulties in diffusing evidence-based intervention innovations into a system conducting primarily “traditional,” education-oriented Cooperative Extension System practices. These barriers were highlighted in an Extension staff survey that was conducted for a McDowell Memorial Lecture.78 Among the key points made by Extension staff in response to this survey was that the partnership-based evidence-based intervention implementation added demands on part-time staff co-leading community teams that competed with their ongoing, day-to-day responsibilities. Various strategies have been used to successfully address this issue, including shifting available human resources in the system to cover the competing demands, such as by assigning assistants to assume some of the responsibility of those involved in the project.
Another related difficulty has been the limited rewards and incentives for the type of sustained efforts required by partnerships implementing and evaluating evidence-based interventions. To address this barrier, the author and colleagues have, among other things, developed various types of recognitions for this type of work and collaborated with administrators to include such work as part of what is addressed in annual evaluations, as well as writing letters of commendation about partnership work for those evaluations. A third, and somewhat related type of difficulty, concerns the degree to which partnership-based implementation and evaluation of evidence-based interventions can conflict with emphasis on more traditional educational and awareness-building practices. For example, a common priority in the Cooperative Extension System is to reach a large number of community residents through educational programming efforts; the use of various forms of mass communication is emphasized. Dissemination of informational sheets or booklets—or offering brief programs that do not require sustained partnerships—are common practice in the Cooperative Extension System and staff are required to report “counts” of people reached, or the frequencies of programming efforts. These counts are considered to be part of their productivity evaluation. By contrast, the type of programming and partnership work advocated in this paper is more labor intensive and can result in lower individual programming counts. The recognitions and incentives illustrated above also serve to address these issues, along with conducting training to educate staff about the value of partnership-based implementation of evidence-based interventions.
In conclusion, the existing, vast, and stable infrastructures of linked Land Grant University-based Cooperative Extension Systems and public school systems offer potential for expanding networks of partnerships for sustained, quality implementation of evidence-based interventions in rural areas. Encouraged by the illustrative findings described earlier, we are taking steps toward realizing this potential—to seize the opportunities. These steps include the design of implementation studies using the PROSPER model in additional “early adopter” states, together with the development of information management and technical assistance systems necessary to support these studies across a network of multiple, partnership-linked states and community sites. In addition, specific dissemination research questions are being formulated, along with multisite research protocols. This partnership network-building is intended to contribute to a larger capacity-building effort, and is thereby expected to further the cause of enhanced rural community health on a larger scale.
Acknowledgments
Work on this paper was supported by research grants DA 070 29-01A1 and DA 013709-01A1 from the National Institute on Drug Abuse, by grant MH 49217-01A1 from the National Institute of Mental Health, and by grant AA 014702-13 from the National Institute on Alcohol Abuse and Alcoholism. A special note of appreciation is warranted to Max Guyll for editing earlier versions of the manuscript. Thanks also to co-investigators on the projects: Cleve Redmond, Chungyeol Shin, Karen Bierman, Gilbert Botvin, Mark Greenberg, David Hawkins, and Karol Kumpfer, as well as to other Institute scientists and staff for their invaluable assistance in developing effective working partnerships with Cooperative Extension System personnel.
Footnotes
Conflict of Interest Statement:
The authors declare no conflicts of interest.
References
- 1.Robertson EB, Sloboda Z, Boyd G, Beatty L, Kozel N, editors. Rural Substance Abuse: State of Knowledge and Issues. National Institute on Drug Abuse; Rockville, Md: 1997. [Google Scholar]
- 2.Muehrer P. Mental health prevention science in rural communities and contexts. Am J Community Psychol. 1997;25(4):421–424. doi: 10.1023/a:1024651420711. [DOI] [PubMed] [Google Scholar]
- 3.Biglan A, Duncan T, Irvine AB, Ary D, Smolkowski K, James L. Drug abuse prevention strategy for rural America. In: Robertson EB, Sloboda Z, Boyd G, Beatty L, Kozel N, editors. Rural Substance Abuse: State of Knowledge and Issues. U.S. Department of Health and Human Services; Rockville, Md: 1997. pp. 364–397. NIDA Prevention Monograph No. 168, NIH Publication No. 97-4177. [Google Scholar]
- 4.D’Onofrio C. The prevention of alcohol use by rural youth. In: Robertson EB, Sloboda Z, Boyd G, Beatty L, Kozel N, editors. Rural Substance Abuse: State of Knowledge and Issues. U.S. Department of Health and Human Services; Rockville, Md: 1997. pp. 250–363. NIDA Prevention Monograph No. 168, NIH Publication No. 97-4177. [Google Scholar]
- 5.Robertson EB. Introduction: Interventions and Services. U.S. Department of Health and Human Services; Rockville, Md: 1997. pp. 246–249. NIDA Prevention Monograph No. 168, NIH Publication No. 97-4177. [Google Scholar]
- 6.St. Lawrence JS, Ndiaye SM. Prevention research in rural communities: overview and concluding comments. Am J Community Psychol. 1997;25(4):545–562. doi: 10.1023/a:1024663723437. [DOI] [PubMed] [Google Scholar]
- 7.Sloboda Z, Rosenquist E, Howard J. Rural Substance Abuse: State of Knowledge and Issues. 1997. Introduction: Substance abuse in rural America; pp. 1–5. National Institute on Drug Abuse Research Monograph 168, USDHHS, NIH Publication No. 97-4177. [Google Scholar]
- 8.Bierman KL, Conduct Problems Prevention Research Group Implementing a comprehensive program for the prevention of conduct problems in rural communities: the Fast Track experience. Am J Community Psychol. 1997;25:493–514. doi: 10.1023/a:1024659622528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Spoth R. Challenges in defining and developing the field of rural mental disorder preventive intervention research. Am J Community Psychol. 1997;25(4):425–448. doi: 10.1023/a:1024603504781. [DOI] [PubMed] [Google Scholar]
- 10.Robertson EB. Introduction to Mental Health Service Delivery in Rural Areas. U.S. Department of Health and Human Services; Rockville, Md: 1997. pp. 413–417. NIDA Prevention Monograph No. 168, NIH Publication No. 97-4177. [Google Scholar]
- 11.Molgaard VK. The Extension Service key mechanism for research and services delivery for prevention of mental health disorders in rural areas. Am J Community Psychol. 1997;25(4):515–544. doi: 10.1023/a:1024611706598. [DOI] [PubMed] [Google Scholar]
- 12.Keller PA, Murray JD, Hargrove DS. The Current Status of Preventive Services in Rural America; Presented at the National Institute of Mental Health Workshop on Rural Mental Disorders Prevention Services Research; Bethesda, Md. 1995, September. [Google Scholar]
- 13.Small SA. Collaborative, community-based research on adolescents: using research for community change. J Res Adolesc. 1996;6(1):9–22. [Google Scholar]
- 14.Edwards RW. Community Participatory Research in Rural Communities; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: current Knowledge and Future Directions; Washington, DC. December.2004. [Google Scholar]
- 15.Roberts L. Strangers, Promises, & Stigma: Distinct Aspects of Health Research in Frontier Communities; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: Current Knowledge and Future Directions; Washington, DC. December.2004. [Google Scholar]
- 16.Smith E. Drug Abuse Prevention Programs in Rural and Urban Contexts: Translation of Approaches Across Communities; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: Current Knowledge and Future Directions; Washington, DC. December.2004. [Google Scholar]
- 17.Boyer E. Scholarship Reconsidered: Priorities of the Profesoriate. Princeton University Press; Princeton, NJ: 1990. [Google Scholar]
- 18.Learner RM, Simon LK. Directions for the American outreach university in the twenty-first century. In: Learner RM, Simon LK, editors. University-Community Collaborations for the Twenty-First Century: Outreach Scholarship for Youth and Families. Garland Publishing; New York: 1998. [Google Scholar]
- 19.Sullivan M, Kelly JG, editors. Collaborative Research: University and Community Partnership. American Public Health Association; Washington, DC: 2001. [Google Scholar]
- 20.Israel BA, Schulz AJ, Parker EA, Becker AB. Review of community-based research: assessing partnership approaches to improve public health. Annu Rev Public Health. 1998;19:173–202. doi: 10.1146/annurev.publhealth.19.1.173. [DOI] [PubMed] [Google Scholar]
- 21.Tierney WG. The Responsive University: Restructuring for High Performance. Johns Hopkins University Press; Baltimore, Md: 1998. [Google Scholar]
- 22.Hewitt M. U.S. Government Printing Office; Washington, DC: 1989. Defining “Rural” Areas: Impact on Health Care Policy and Research. Office of Technology Assessment. [Google Scholar]
- 23.Wagenfeld MO, Murray JD, Mohatt DF, DeBruyn JC. Mental Health and Rural America. Office of Rural Health Policy, U.S. Department of Health and Human Services; Washington, DC: 1994. [Google Scholar]
- 24.Clayton RR. Issues, Challenges, and Opportunities in Conducting Research in Rural and Frontier Settings; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: Current Knowledge and Future Directions; Washington, DC. December; 2004. [DOI] [PubMed] [Google Scholar]
- 25.Elifson KW. Social and Environmental Factors and Their Influence on Drug Use Vulnerability and Resiliency in Rural Populations; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: Current Knowledge and Future Directions; Washington, DC. December.2004. [Google Scholar]
- 26.Gfroerer J, Epstein J, Wright D. Estimating substance abuse treatment need by state. Addiction. 2004;99:938–939. doi: 10.1111/j.1360-0443.2004.00818.x. [DOI] [PubMed] [Google Scholar]
- 27.Ratcliffe MR. Defining Rural Communities: Demographic Change in Rural Communities; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: Current Knowledge and Future Directions; Washington, DC. December.2004. [Google Scholar]
- 28.Brody G. Meeting the Prevention Needs of Under-Served Rural Populations; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: Current Knowledge and Future Directions; Washington, DC. December.2004. [Google Scholar]
- 29.Hargraves M, Cornelius L. The Social, Behavioral and Environmental Contexts for Women’s Health in Rural Settings; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: Current Knowledge and Future Directions; Washington, DC. December.2004. [Google Scholar]
- 30.Embry DD, Galloway D. Moving the Needle on Drugs: Money, Logic Models, Research-Based Practices and Data in Frontier and Rural Conditions; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: Current Knowledge and Future Directions; Washington, DC. December.2004. [Google Scholar]
- 31.Weisman SA, Gottfredson DC. Maryland Blueprints Manual: A guide to Promising and Proven Prevention Programs. University of Maryland; College Park, Md: 2002. [Google Scholar]
- 32.Ennett ST, Ringwalt CL, Thorne J, et al. A comparison of current practice in school-based substance use prevention programs with meta-analysis findings. Prev Sci. 2003;4(1):1–14. doi: 10.1023/a:1021777109369. [DOI] [PubMed] [Google Scholar]
- 33.Hallfors D, Cho H, Livert D, Kadushin C. Fighting back against substance abuse: are community coalitions winning? Am J Prev Med. 2002;23(4):237–245. doi: 10.1016/s0749-3797(02)00511-1. [DOI] [PubMed] [Google Scholar]
- 34.Booth B. Utilization of Substance Abuse Services in Rural Settings; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: Current Knowledge and Future Directions; Washington, DC. December.2004. [Google Scholar]
- 35.Solano PL. The Economics of Treatment and Prevention Services in Rural Communities; Presentation for the National Institute on Drug Abuse meeting on Drug Abuse Research in Rural Communities: Current Knowledge and Future Directions; Washington, DC. December.2004. [Google Scholar]
- 36.Parsons JE, Merlin TL, Taylor JE, Wilkinson D, Hiller JE. Evidence-based practice in rural and remote clinical practice: where is the evidence? Austral J Rural Health. 2003;11:242–248. [PubMed] [Google Scholar]
- 37.Chibucos T, Lerner R, editors. Serving Children and Families Through Community-University Partnerships: Success Stories. Kluwer Academic; Boston: 1999. [Google Scholar]
- 38.Spoth RL, Greenberg MT. Toward a comprehensive strategy for effective practitioner-scientist partnerships and larger-scale community benefits. Am J Community Psychol. 2005;35(34):107–126. doi: 10.1007/s10464-005-3388-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Spoth R, Molgaard V. Project Family: A partnership integrating research with the practice of promoting family and youth competencies. In: Chibucos TR, Lerner R, editors. Serving Children and Families Through Community-University Partnerships: Success Stories. Kluwer Academic; Boston: 1999. pp. 127–137. [Google Scholar]
- 40.Coward RT, Van Horne JE, Jackson RW. The Cooperative Extension Service: an underused resource for rural primary prevention. In: Murray JD, Keller PA, editors. Innovations in Rural Community Mental Health. Rural Services Institute; Mansfield, Pa: 1986. pp. 105–120. [Google Scholar]
- 41.Bonnen JT. The land-grant idea and the evolving outreach university. In: Lerner RM, Simon LAK, editors. University-Community Collaborations for the Twenty-First Century. Garland; New York: 1998. pp. 463–480. [Google Scholar]
- 42.Spoth R. Examining Extension’s Potential for Bridging the Gap Between Prevention Research and Practice: Future Directions for Collaboration; Presented at the NIHM-Institute for Social and Behavioral Research Working Conference on the Extension System and Practitioner-researcher collaborations in the implementation, assessment, and dissemination of preventive interventions; Ames, Iowa. May.1998. [Google Scholar]
- 43.Rogers EM. Diffusion of Innovations. 4th ed. Free Press; New York: 1995. [Google Scholar]
- 44.Backer TE. Evaluating Community Collaborations. Springer; New York: 2003. [Google Scholar]
- 45.Fixsen DL, Naoom SF, Blasé KA, Friedman RM, Wallace F, University of South Florida. Louis de la Parte Florida Mental Health Institute. The National Implementation Research Network . Implementation Research: A Synthesis of the Literature. 2005. FMHI Publication #231. [Google Scholar]
- 46.Greenberg MT, Domitrovich CE, Graczyk PA, Zins JhE, U.S. Department of Health and Human Services . Report submitted to the Center for Mental Health Services (CMHS) and Substance Abuse and Mental Health Administration (SAMHSA) 2001. The Study of Implementation in School-Based Prevention Research: Theory, Research and Practice. [Google Scholar]
- 47.Spoth R, Guyll M, Lillehoj CJ, Redmond C, Greenberg M. PROSPER study of evidence-based intervention implementation quality by community-university partnership. J Community Psychol. doi: 10.1002/jcop.20207. In press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Spoth R, Redmond C. Research on family engagement in preventive interventions: toward improved use of scientific findings in primary prevention practice. J Prim Prev. 2000;21(2):267–284. [Google Scholar]
- 49.Spoth R, Redmond C. Project Family prevention trials based in community-university partnerships: toward scaled-up preventive interventions. Prev Sci. 2002;3:203–221. doi: 10.1023/a:1019946617140. [DOI] [PubMed] [Google Scholar]
- 50.Sandler I, Ostrom A, Bitner MJ, Ayers TS, Wolchik S, Daniels V. Developing effective prevention services for the real world: a prevention service development model. Am J Community Psychol. 2005;35:107–126. doi: 10.1007/s10464-005-3389-z. [DOI] [PubMed] [Google Scholar]
- 51.Guyll M, Spoth R, Redmond C. The effects of incentives and research requirements on participation rates for a community-based preventive intervention research study. J Prim Prev. 2003;24:25–41. [Google Scholar]
- 52.Spoth R, Clair S, Greenberg M, Redmond C, Shin C. Toward dissemination of evidence-based family interventions: maintenance of community-based partnership recruitment results and associated factors. J Fam Psychol. 2007;21:137–145. doi: 10.1037/0893-3200.21.2.137. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Spoth R, Redmond C, Shin C, Leppe H, Haggerty K, Wall M. Risk moderation of parent and child outcomes in a preventive intervention: A test and replication. Am J Orthopsychiatry. 1998;68:565–579. doi: 10.1037/h0080365. [DOI] [PubMed] [Google Scholar]
- 54.Spoth R, Goldberg C, Redmond C. Engaging families in longitudinal preventive intervention research: Discrete-time survival analysis of socioeconomic and social-emotional risk factors. J Consult Clin Psychol. 1999;67(1):157–163. doi: 10.1037//0022-006x.67.1.157. [DOI] [PubMed] [Google Scholar]
- 55.Biglan A. Changing Cultural Practices: A Contextual Framework for Intervention Research. Context Press; Reno, Nev: 1995. [Google Scholar]
- 56.Spoth R, Redmond C, Shin C. Randomized trial of brief family interventions for general populations: adolescent substance use outcomes four years following baseline. J Consult Clin Psychol. 2001;69:627–642. doi: 10.1037//0022-006x.69.4.627. [DOI] [PubMed] [Google Scholar]
- 57.Spoth R, Redmond C, Shin C, Azevedo K. Brief family intervention effects on adolescent substance initiation: school-level curvilinear growth curve analyses six years following baseline. J Consult Clin Psychol. 2004;72(3):535–542. doi: 10.1037/0022-006X.72.3.535. [DOI] [PubMed] [Google Scholar]
- 58.Spoth R, Guyll M, Day SX. Universal family-focused interventions in alcohol-use disorder prevention: cost-effectiveness and cost-benefit analyses of two interventions. J Stud Alcohol. 2002;63:219–228. doi: 10.15288/jsa.2002.63.219. [DOI] [PubMed] [Google Scholar]
- 59.Johnston LD, O’Malley PM, Bachman JG. The Monitoring the Future National Survey Results on Adolescent Drug Use: Overview of Key Findings. National Institute on Drug Abuse; Bethesda, Md: 2002. Publication NIH 02-5105; 2001. [Google Scholar]
- 60.Johnston LD, O’Malley PM, Bachman JG, Schulenberg JE. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings. National Institute on Drug Abuse; Bethesda, Md: 2004. Publication NIH 05-5726;2005. [Google Scholar]
- 61.Oetting ER, Deffenbacher JL, Taylor MJ, Luther N, Beedvais F, Edwards RW. Methamphetamine use by high school students: recent trends, gender and ethnicity differences, and use of other drugs. J Child Adoles Sub Abuse. 2000;10:33–50. [Google Scholar]
- 62.Wermuth L. Methamphetamine use: Hazards and social influences. J Drug Educ. 2000;30:423–433. doi: 10.2190/GMH7-3FWX-1AC1-RWXP. [DOI] [PubMed] [Google Scholar]
- 63.Rawson RA, Anglin MD, Ling W. Will the methamphetamine problem go away? J Addict Disorders. 2002;21:5–19. doi: 10.1300/j069v21n01_02. [DOI] [PubMed] [Google Scholar]
- 64.Hall JN, Broderick PM, National Institute on Drug Abuse Research Monograph Series . Community networks for response to abuse outbreaks of methamphetamine and its analogs. In: Miller MA, Kozel NJ, editors. Methamphetamine Abuse: Epidemiologic Issues and Implications. National Institute on Drug Abuse; Alcohol, Drug Abuse, and Mental Health Administration; U.S. Department of Health and Human Services; Rockville, Md: 1991. pp. 109–120. Electronic version. NIDA Research Monograph No. 115, DHHS Publication No. ADM 91-1836. 1991. [PubMed] [Google Scholar]
- 65.The National Clearinghouse on Drug and Alcohol Information (NCADI) Jun 19, 1997. The methamphetamine challenge: threatening communities coast-to-coast (telecast Downlink)
- 66.Spoth R, Clair S, Shin C, Redmond C. Long-term effects of universal preventive interventions on methamphetamine use among adolescents. Arch Ped Adolesc Med. 2006;160:876–882. doi: 10.1001/archpedi.160.9.876. [DOI] [PubMed] [Google Scholar]
- 67.Spoth R, Redmond C, Shin C. Reducing adolescents’ aggressive and hostile behaviors: randomized trial effects of a brief family intervention four years past baseline. Arch Ped Adoles Med. 2000;154:1248–1257. doi: 10.1001/archpedi.154.12.1248. [DOI] [PubMed] [Google Scholar]
- 68.Redmond C, Spoth R, Shin C, Lepper H. Modeling long-term parent outcomes of two universal family-focused preventive interventions: One year follow-up results. J Consult Clin Psychol. 1999;67(6):975–984. doi: 10.1037//0022-006x.67.6.975. [DOI] [PubMed] [Google Scholar]
- 69.Spoth R, Redmond C, Shin C. Direct and indirect latent-variable parenting outcomes of two universal family-focused preventive interventions: extending a public health-oriented research base. J Consult Clin Psychol. 1998;66(2):385–399. doi: 10.1037//0022-006x.66.2.385. [DOI] [PubMed] [Google Scholar]
- 70.Spoth R, Randall GK, Shin C. Experimental support for a model of partnership-based family intervention effects on long-term academic success. Sch Psychol Q. doi: 10.1037/1045-3830.23.1.70. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Feinberg M, Meyer-Chilenski S, Greenberg M, Spoth R, Redmond C. Predictors of operations phase functioning of local teams partnership preventions. Prev Sci. in press. [Google Scholar]
- 72.Greenberg M, Feinberg M, Meyer-Chilenski S, Spoth R, Redmond C. Community and team member factors that influence the early phases of local team partnerships in prevention: the PROSPER Project. J Prim Prev. doi: 10.1007/s10935-007-0116-6. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Spoth R, Redmond C, Shin C, Greenberg M, Clair S, Feinberg M. Substance use outcomes at 1½ years past baseline from the PROSPER community-university partnership trial. Am J Prev Med. doi: 10.1016/j.amepre.2007.01.014. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.National Research Council and Institute of Medicine . In: Community Programs to Promote Youth Development. Eccles J, Gootman JA, editors. National Academy Press; Washington, DC: 2002. Retrieved November 17, 2003, (The report is available as an “open book” online) at: http://www.nap.edu/catalog/10022.html. [Google Scholar]
- 75.Minkler M, Wallerstein N. Improving health through community organization and community building. In: Minkler M, editor. Community Organizing & Community Building for Health. Rutgers University Press; New Brunswick, NJ: 2002. pp. 30–52. [Google Scholar]
- 76.Wandersman A. Community science: bridging the gap between science and practice with community-centered models. Am J Community Psychol. 2003;31(34):227–242. doi: 10.1023/a:1023954503247. [DOI] [PubMed] [Google Scholar]
- 77.U.S. Department of Health and Human Services (USDHHS) Healthy People 2010: Understanding and Improving Health. 2nd ed. U.S. Government Printing Office; Washington, DC: 2000. [Google Scholar]
- 78.Spoth R. Extension pioneers: toward new frontiers in community-university partnerships; An invited presentation for the McDowell Memorial Lecture series at The Pennsylvania State University; State College, Pa. 2004. [Google Scholar]