Abstract
Objective
Studies suggest that obesity’s adverse impact on cardiovascular mortality may be reduced in African Americans relative to white Americans. We examined whether obesity’s association with novel cardiovascular risk factors such as C-reactive protein (CRP) also varies by race and ethnicity.
Methods and Procedures
We analyzed data from 10,492 white, African-American, and Hispanic-American participants of the 1999–2004 National Health and Nutrition Examination Survey, who were aged 20 years and older, with a BMI ≥18.5 kg/m2 and CRP ≤10 mg/l. We fit sex-specific multivariable models of the association of BMI or waist circumference with log CRP levels and tested for interactions of BMI or waist circumference with race/ethnicity.
Results
Higher BMI was significantly associated with higher CRP in all racial/ethnic groups for both men and women (P > 0.05 for BMI–race/ethnicity interaction) before and after adjustment for age, education, and health behaviors. Larger waist circumference was also associated with higher CRP levels in all racial/ethnic groups before and after adjustment; among women, the relationship was strongest for Mexican Hispanics (P < 0.01 for waist circumference–race/ethnicity interaction). Results were similar after additional adjustment for medications that might affect CRP levels.
Discussion
The association between obesity and CRP is at least as strong in African Americans and Hispanic Americans as in white Americans. Racial differences in the relationship between obesity and cardiovascular mortality are unlikely to be due to racial differences in obesity’s impact on CRP.
INTRODUCTION
Obesity is a leading cause of preventable death and a major contributor to cardiovascular risk and mortality in the United States. Despite obesity’s disproportionately high prevalence in African Americans and Hispanic American (1,2), studies suggest that its adverse impact on cardiovascular risk and mortality may be reduced in some minority populations (3–8). For example, even though African Americans have a higher prevalence of hypertension and diabetes than white Americans, evidence suggests that the associations between obesity and these cardiovascular risk factors are steeper in white Americans than in African Americans (9–11). The adverse relationship between obesity and dyslipidemia is similarly attenuated in African Americans relative to white Americans (11).
Increasingly, systemic and vascular inflammation are implicated in the pathogenesis of cardiovascular outcomes (12,13). C-reactive protein, or CRP, is a sensitive marker of inflammation and is perhaps the most well studied of these novel markers of cardiovascular disease (14–16). Higher levels of CRP are associated with higher risk of myocardial infarction, ischemic stroke, and cardiovascular mortality (14–17). CRP levels are also elevated in the presence of metabolic risk factors such as obesity (18). Adipose tissue is a major producer of proinflammatory cytokines and hormones and is thought to induce low-grade systemic inflammation (19). However, while several studies demonstrate that levels of CRP are elevated in persons with higher BMI (18), and that weight loss reduces CRP (20,21), few studies have examined whether obesity might have a differential impact on CRP levels in different racial and ethnic groups.
In this context, we examined the interplay of race, ethnicity, and obesity on CRP levels in a nationally representative sample of US adults to evaluate whether the relationship between obesity and CRP is attenuated in Africans Americans and other ethnic minorities relative to white Americans.
METHODS AND PROCEDURES
Data source and measurements
We used data from the National Health and Nutrition Examination Survey, or NHANES, a stratified multistage probability sample of the noninstitutionalized civilian population of the United States conducted by the Centers for Disease Control and Prevention and the National Center for Health Statistics (22). NHANES is designed to assess the health and nutritional status of adults and children through interviews and physical examination; methodological aspects of the study have been described in detail elsewhere (22–25). Beginning in 1999, the study was redesigned to be an ongoing continuous program. Data are released in 2-year cycles. NHANES oversamples certain populations, including African Americans, Mexican Americans, and pregnant women; however, design weights and sampling information are provided so that analyses can account for the complex sampling design and be generalized to the US population. Our study utilized the most recently available completed data from 1999 to 2004. This study was exempted from continuing review by the Institutional Review Board at Beth Israel Deaconess Medical Center.
Our study sample consisted of adults aged 20 years and older, who completed home interviews, self-administered questionnaires, and physical and laboratory examinations at mobile examination units. Information about participants’ sociodemographic characteristics, health habits, and medical history were collected via in-person interviews and through self-administered questionnaires. We categorized participants’ self-identified race/ethnicity as non-Hispanic white, non-Hispanic black or African American, Mexican Hispanic, and non-Mexican Hispanic, and other race/ethnicity. Because participants in the “other race” category are a small but heterogeneous group (n = 466), we did not include these participants in our study. We also classified participants according to other relevant demographic and behavioral factors including educational status (less than high school, completed high school, high school and beyond), smoking history (never smoked or smoked <100 cigarettes in lifetime, former smoker, and current smoker), alcohol use, and physical activity level. Quantity and frequency of alcohol use were jointly characterized as follows: nondrinker; 1–2 drinking days/week and less than two drinks per day; 1–2 drinking days/week and two or more drinks per day; 3 or more drinking days/week and two or less drinks per day; 3 or more drinking days/week and two or more drinks per day. We calculated the energy expended in metabolic equivalents (METs) based on participants’ reports of physical activity using estimates provided in NHANES (22,26) and classified physical activity level in population-based quartiles.
Participants were also asked to report all over-the-counter and prescription medications including medications that might affect CRP levels such as nonsteroidal anti-inflammatory medications, lipid-lowering statin medications, and estrogen-containing medicines (27). At the time of our study, medication use was available only for participants of the 1999–2002 NHANES.
A standardized set of physical and laboratory examinations were conducted in mobile examination centers and included measured height and weight. Our primary measure of adiposity, BMI, was calculated from measured height and weight; we classified participants as normal weight (BMI = 18.5–24.9 kg/m2), overweight (BMI = 25.0–29.9 kg/m2), class I obesity (BMI = 30.0–34.9 kg/m2), and class II–III obesity (BMI = 35.0 kg/m2 and higher), according to standard definitions (28). Waist circumference, our second marker of adiposity, was measured in centimeters and then converted to inches and was classified in sex-specific quartiles. Blood samples were collected on adults’ aged 20 years and older and centrifuged within 1 h of phlebotomy and frozen at −10 °C. CRP concentrations were measured by latex-enhanced nephelometry (N high-sensitivity CRP assay) (22). We treated high-sensitivity CRP as a continuous outcome and excluded participants with CRP levels >10 mg/l (n = 1528) (27), as such high levels likely reflect acute illness. We also excluded a small number of underweight participants with a BMI <18.5 kg/m2 (n = 183) and women who were pregnant (n = 486).
Statistical analysis
We characterized CRP levels in our overall sample, according to race, ethnicity, BMI, and waist circumference. Because CRP levels were not normally distributed, we used the logarithmic transformation of CRP levels as our outcome measure in sex-specific multivariable analyses and then “back transformed” our results and expressed our findings in terms of the geometric mean of CRP. We examined the association between BMI and log CRP, adjusting for race and ethnicity and then tested for an interaction between race/ethnicity and BMI. Our primary analyses were adjusted for age, education, and health behaviors (smoking, alcohol, and physical activity). In sensitivity analyses in the subset with complete data, we considered the confounding effect of income and medication use (nonsteroidal anti-inflammatory drugs, statins, and estrogen use in women) separately on the relationship between BMI and log CRP. To explore the robustness of our findings, we examined the association between waist circumference and log CRP using the similar approach as for our BMI-log CRP analyses.
We weighted all analyses to reflect population estimates and used SAS-callable SUDAAN statistical software (Research Triangle Park, NC) (29) to produce appropriate standard errors that account for the complex clustered sampling design.
RESULTS
Table 1 describes our study population of 10,492 men and women aged 20 years and older, who have a BMI of 18.5 kg/m2 or higher and a CRP of 10 mg/l or lower. Sex-stratified demographic and behavioral factors differed significantly across race and ethnicity in our sample. Before adjustment, BMI and waist circumference also varied significantly by race and ethnicity in both men and women. In contrast, mean CRP levels were significantly different by race and ethnicity in women but not in men; among women, CRP levels were lowest in whites and highest in Mexican Hispanics.
Table 1.
Characteristics of the study sample (n =10,492)
| Men (n = 5,517) |
Women (n = 4,975) |
|||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| White | African American | Mexican Hispanic | Non-Mexican Hispanic | P valuea | White | African American | Mexican Hispanic | Non-Mexican Hispanic | P valueb | |
| Mean age, y (s.e.) | 46.7 (0.36) | 42.1 (0.49) | 37.6 (0.66) | 41.3 (1.02) | <0.0001 | 48.9 (0.36) | 43.8 (0.54) | 39.2 (0.85) | 43.3 (1.33) | <0.0001 |
| Mean CRP levels (mg/l) (s.e.) | 2.14 (0.04) | 2.23 (0.07) | 2.03 (0.07) | 2.19 (0.13) | 0.21 | 2.77 (0.05) | 3.09 (0.07) | 3.25 (0.09) | 2.84 (0.17) | 0.0004 |
| BMI (kg/m2) | <0.0001 | <0.0001 | ||||||||
| 18.5–24.9 | 29.1 | 35.5 | 29.0 | 29.6 | 42.9 | 24.0 | 31.6 | 30.6 | ||
| 25.0–29.9 | 42.2 | 35.9 | 43.6 | 50.5 | 29.9 | 31.3 | 35.0 | 38.7 | ||
| 30.0–34.9 | 20.1 | 18.1 | 21.0 | 13.4 | 16.4 | 24.0 | 21.6 | 20.5 | ||
| 35.0 or higher | 8.5 | 10.5 | 6.4 | 6.6 | 10.8 | 20.7 | 11.8 | 10.2 | ||
| Waist circumference, median (Q1, Q3) | 39.3 (35.9, 43.0) | 36.8 (33.0, 41.3) | 37.8 (34.6, 41.0) | 37.1 (34.1, 39.9) | <0.0001 | 35.3 (31.7, 39.7) | 37.3 (33.5, 41.7) | 36.0 (32.4, 39.8) | 35.1 (32.2, 38.3) | <0.0001 |
| Physical activity | <0.0001 | <0.0001 | ||||||||
| ≥160 METs | 30.6 | 27.6 | 20.0 | 23.5 | 21.8 | 18.1 | 14.3 | 22.4 | ||
| Alcohol | <0.0001 | <0.0001 | ||||||||
| Abstainers | 15.6 | 26.0 | 10.8 | 15.2 | 33.2 | 50.0 | 50.0 | 49.7 | ||
| <1 day/week | 38.1 | 36.9 | 49.5 | 39.8 | 39.3 | 33.4 | 39.9 | 34.9 | ||
| ≥1 day/week | 46.3 | 37.1 | 39.7 | 45.0 | 27.5 | 16.6 | 10.1 | 15.4 | ||
| Smoking | <0.0001 | <0.0001 | ||||||||
| Never smoker | 42.2 | 51.0 | 44.8 | 46.4 | 53.8 | 65.1 | 72.7 | 66.8 | ||
| Former smoker | 32.0 | 16.6 | 25.1 | 27.2 | 23.7 | 13.4 | 12.9 | 14.7 | ||
| Current smoker | 25.8 | 32.4 | 30.1 | 26.4 | 22.6 | 21.4 | 14.4 | 18.6 | ||
| Education | <0.0001 | <0.0001 | ||||||||
| Less than high school | 12.8 | 32.2 | 54.8 | 38.2 | 13.4 | 31.3 | 53.1 | 29.2 | ||
| High school graduate | 27.8 | 24.9 | 21.6 | 18.7 | 28.0 | 22.1 | 20.3 | 23.0 | ||
| College graduate | 59.4 | 42.9 | 23.6 | 43.1 | 58.6 | 46.6 | 26.7 | 47.7 | ||
| Medications | ||||||||||
| Statins | 10.9 | 4.9 | 2.1 | 5.3 | <0.0001 | 8.7 | 4.0 | 3.1 | 4.1 | <0.0001 |
| Anti-inflammatory | 24.1 | 7.9 | 6.1 | 9.3 | <0.0001 | 22.6 | 12.0 | 8.8 | 14.4 | <0.0001 |
| Estrogen-containing hormones | 0.01 | 0 | 0 | 0 | 0.79 | 23.0 | 7.7 | 7.0 | 4.0 | <0.0001 |
CRP, C-reactive protein; MET, metabolic equivalent.
Significance level for racial and ethnic differences for factor of interest in men;
Significance level for racial differences in women.
Table 2 presents age-adjusted CRP levels across BMI and race/ethnicity, as well as across waist circumference and race/ethnicity. Higher BMI and higher waist circumference were associated with higher CRP levels for men and women in all racial and ethnic groups studied (P < 0.001 for all).
Table 2.
Mean unadjusted crP levels (s.e.) by BMI and waist circumference
| White | African American | Mexican Hispanic | Non-Mexican Hispanic | |
|---|---|---|---|---|
| BMI, kg/m2 | ||||
| Men | ||||
| 18.5–24.9 | 0.91 (0.04) | 0.84 (0.05) | 0.78 (0.06) | 0.81 (0.13) |
| 25.0–29.9 | 1.29 (0.04) | 1.46 (0.08) | 1.48 (0.07) | 1.55 (0.11) |
| 30.0–34.9 | 1.96 (0.08) | 2.07 (0.14) | 2.07 (0.16) | 1.99 (0.40) |
| ≥35 | 2.76 (0.09) | 3.20 (0.27) | 2.96 (0.27) | 4.81 (0.96) |
| Women | ||||
| 18.5–24.9 | 1.06 (0.06) | 0.89 (0.08) | 1.28 (0.10) | 0.95 (0.16) |
| 25.0–29.9 | 1.94 (0.07) | 1.87 (0.12) | 2.17 (0.17) | 1.96 (0.20) |
| 30.0–34.9 | 2.78 (0.12) | 3.00 (0.19) | 3.62 (0.16) | 3.08 (0.40) |
| ≥35 | 3.88 (0.17) | 3.52 (0.19) | 5.09 (0.27) | 3.90 (0.84) |
| Waist circumference | ||||
| Men | ||||
| Lowest quartile | 0.76 (0.04) | 0.81 (0.05) | 0.74 (0.06) | 0.88 (0.13) |
| 2nd quartile | 1.17 (0.06) | 1.47 (0.10) | 1.32 (0.07) | 1.43 (0.13) |
| 3rd quartile | 1.50 (0.04) | 1.93 (0.12) | 1.81 (0.10) | 1.72 (0.19) |
| 4th quartile | 2.24 (0.06) | 2.68 (0.18) | 2.43 (0.21) | 3.10 (0.39) |
| Women | ||||
| Lowest quartile | 0.86 (0.05) | 0.82 (0.09) | 1.03 (0.11) | 0.91 (0.15) |
| 2nd quartile | 1.51 (0.08) | 1.53 (0.14) | 1.81 (0.16) | 1.56 (0.24) |
| 3rd quartile | 2.19 (0.12) | 2.19 (0.13) | 2.42 (0.12) | 2.64 (0.24) |
| 4th quartile | 3.20 (0.09) | 3.35 (0.15) | 4.50 (0.14) | 3.04 (0.47) |
P < 0.001 for the association between C-reactive protein (CRP) and BMI or waist circumference (WC) across sex, race, and ethnicity.
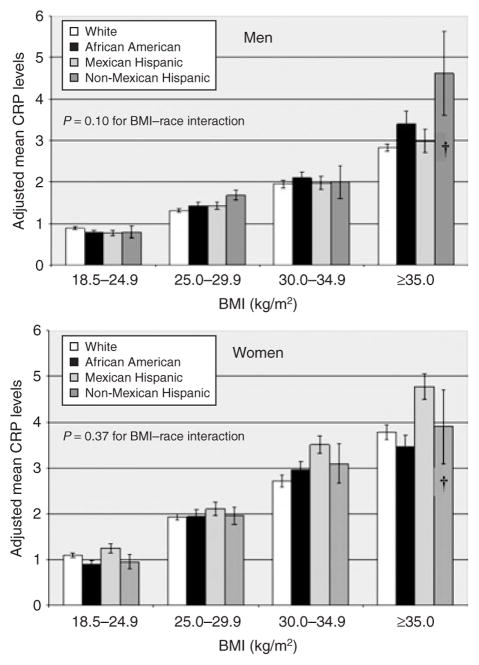
Higher BMI was associated with CRP levels after adjustment for age, race and ethnicity, education, and health behaviors, P < 0.001 for both men and women (data not shown). Figure 1 presents mean CRP levels in men and women by race and ethnicity after adjustment. The relationship between BMI and mean CRP did not vary significantly across race and ethnicity in men (P = 0.10 for race–BMI interaction) or in women (P = 0.37 for race–BMI interaction). However, while not statistically significant, the slope for the relationships between BMI and CRP appear steeper for non-Mexican Hispanic Americans than for other groups; this apparent steeper relationship was driven primarily by the disproportionately high CRP levels in non-Mexican Hispanics with a BMI ≥35 kg/m2 which comprised <30 participants. Additional adjustment for income and relevant medications in sensitivity analyses did not change our results substantially.
Figure 1.
Adjusted mean C-reactive protein (CRP) levels (s.e.) by BMI in men and women (adjusted for age, education, smoking, alcohol, and physical activity level). †Estimates unreliable, samples size <30 for subgroup.
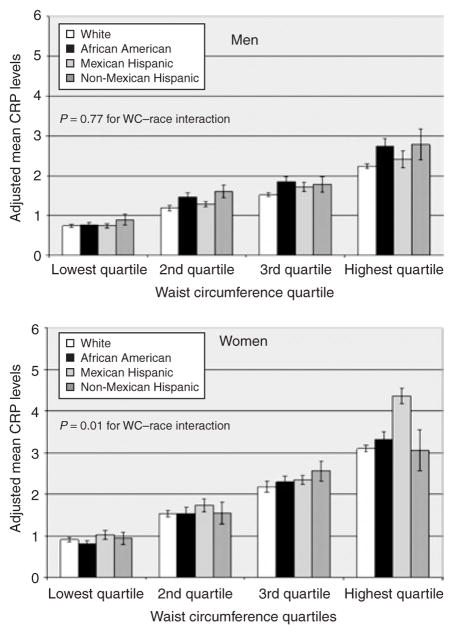
Higher waist circumference was also significantly associated with CRP levels in both men and women (P < 0.001 for both) after adjustment for age, race and ethnicity, education, and health behaviors. This association varied significantly by race and ethnicity (P = 0.01) in women but not in men (P = 0.77). Among women, the association between waist circumference and CRP was most striking for Mexican-Hispanic Americans. These results were consistent in sensitivity analyses adjusting for income and relevant medications.
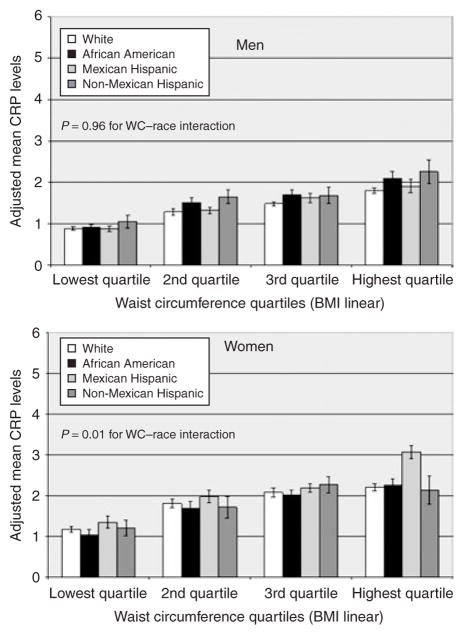
Table 3 presents the age-adjusted mean waist circumference for men and women across BMI and race and ethnicity in the overall study population. In analyses stratified by BMI category, racial and ethnic differences in mean waist circumference were highly significant (P < 0.001 at all BMI levels) in men. Among women, racial and ethnic differences reached statistical significance only for women in the middle two BMI levels (P = 0.02 for BMI = 25.0–34.9 kg/m2). To examine whether racial and ethnic differences in the adjusted relationship between waist circumference and CRP (Figure 2) might be due to racial and ethnic differences in the association between BMI and waist circumference, we conducted post-hoc multivariable analyses of waist circumference and CRP, additionally adjusting for BMI (both in categories and linearly). The relationship between waist circumference and CRP were attenuated but remained statistically significant; moreover, the interaction between waist circumference and race-ethnicity remained statistically significant in women (Figure 3).
Table 3.
Age-adjusted mean waist circumference (s.e.) according to BMI and race/ethnicity
| White | African-American | Mexican Hispanic | Non-Mexican Hispanic | P value | |
|---|---|---|---|---|---|
| BMI, kg/m2 | |||||
| Men | |||||
| 18.5–24.9 | 34.4 (0.1) | 32.4 (0.1) | 33.7 (0.2) | 33.5 (0.4) | 0.001 |
| 25.0–29.9 | 39.1 (0.1) | 37.4 (0.1) | 38.3 (0.1) | 37.9 (0.3) | 0.001 |
| 30.0–34.9 | 43.7 (0.1) | 42.4 (0.2) | 42.4 (0.3) | 41.7 (0.5) | 0.001 |
| ≥35 | 50.3 (0.3) | 49.4 (0.4) | 48.0 (0.5) | 48.4 (1.1) | 0.001 |
| Women | |||||
| 18.5–24.9 | 31.6 (0.1) | 31.3 (0.2) | 31.9 (0.2) | 31.6 (0.3) | 0.18 |
| 25.0–29.9 | 36.5 (0.1) | 36.2 (0.1) | 36.2 (0.2) | 35.3 (0.3) | 0.02 |
| 30.0–34.9 | 40.6 (0.1) | 40.1 (0.2) | 40.1 (0.2) | 39.4 (0.4) | 0.02 |
| ≥35 | 45.7 (0.3) | 45.9 (0.4) | 45.7 (0.4) | 43.9 (1.1) | 0.31 |
Results presented in inches.
Figure 2.
Adjusted mean C-reactive protein (CRP) levels (s.e.) by waist circumference (WC) in men and women (adjusted for age, education, smoking, alcohol, and physical activity level).
Figure 3.
Adjusted mean C-reactive protein (CRP) levels (s.e.) by waist circumference (WC) in men and women with additional adjustment for BMI (adjusted for age, education, smoking, alcohol, physical activity, and BMI (continuous)).
DISCUSSION
Our findings suggest that the relationship between obesity and higher CRP levels appears to be as strong in African Americans and Hispanic Americans as in white American adults. The association between BMI and CRP did not vary significantly across race and ethnicity, and the association between larger waist circumference and higher CRP levels was also at least as strong in African Americans and possibly stronger in Mexican-Hispanic–American women relative to white women.
Cardiovascular disease is the leading cause of death among Americans and the leading cause of death attributable to obesity (8). Moreover, among certain racial and ethnic minority populations such as African Americans, the rate of death from cardiovascular disease is substantially higher than the rate in whites (4,5). Paradoxically, while the prevalence of obesity and the rate of cardiovascular death is higher in African Americans, a number of studies have suggested that obesity has less of an adverse impact on all-cause and cardiovascular mortality in African Americans than in white populations in the United States (3–8). The racial difierences are most striking in women, where the relative risk of all-cause and cardiovascular mortality associated with the highest categories of BMI can be severalfold higher in white women compared to African American women (8). Much less is known about the impact of obesity on mortality differing between Hispanic and white populations.
While the factors contributing to racial differences in the impact of BMI and mortality are unclear, growing evidence suggests that obesity may have a reduced impact on some traditional cardiovascular risk factors (9–11). Using data from the National Health and Nutrition Examination Epidemiologic Follow-up Study, Resnick and colleagues found that relative to whites, the risk for developing diabetes in African American men and women was disproportionately higher in the lean BMI ranges than in the overweight and obese ranges (9). These findings are consistent with those of more recent studies (30). A few studies have also suggested that while African Americans are more likely to develop hypertension than white Americans, the association between higher BMI and the prevalence of hypertension is attenuated in African Americans (11,31). Similarly, the relationship between obesity and adverse lipid profile may also be reduced in African Americans relative to whites (11).
However, traditional cardiovascular risk factors do not fully characterize an individual’s cardiovascular risk. Increasingly, studies in primarily white-American populations suggest that inflammatory markers such as CRP levels have shown to independently predict cardiovascular disease and adverse cardiovascular outcomes (14–17). Although the magnitude of the predictive contribution of inflammation beyond that of traditional cardiovascular risk factors is being debated (32,33), one of the mechanisms by which obesity and adiposity confer cardiovascular risk is likely through heightened inflammation. Our findings suggest that the relationship between BMI and CRP levels is comparable among white, African-American, and Hispanic populations in the United States and that visceral adiposity, measured by waist circumference, may be more adversely associated with inflammation in Mexican-Hispanic women than in white women. Given our findings, observed racial differences in the relationship between obesity and cardiovascular mortality risk are unlikely to be mediated by an attenuated relationship between obesity and CRP level in certain racial and ethnic minorities.
Previous studies have suggested that CRP levels do vary by sex and race (34–37), although few have examined this variation in the context of obesity. These prior data suggest that women generally have higher CRP levels than men and that African Americans, particularly African-American women and south Asians generally have higher levels than white adults (34). In the Women’s Health Study, African-American women had the highest CRP levels, Asian women had the lowest, and white and Hispanic women had levels in the intermediate range (37). Our data also suggest that women generally have higher CRP levels than men but that much of the racial difference in CRP levels in women, in particular, is substantially diminished after accounting for age and obesity. We found no racial differences in the relationship between obesity and CRP level in both men and women, with one exception. Among women, Mexican Hispanics with the largest waist circumference had an exaggerated CRP level compared to women of other racial/ethnic groups. The significance of this finding is unclear and needs to be replicated in future studies.
Our study has several limitations. First, the cross-sectional and observational design prevents us from drawing causal inferences about the relationship between obesity and CRP levels. Second, BMI and waist circumference are surrogate markers for adiposity, and CRP is only one measure of inflammation. Finally, we were unable to adjust for residual confounding from noncardiovascular, inflammatory conditions that are not in the causal pathway between obesity and cardiovascular outcomes, although we attempted to minimize this confounding by excluding underweight and pregnant individuals and those with CRP levels above 10 mg/l from our study.
In summary, obesity appears to be as strongly associated with systemic inflammation as measured by CRP levels in African Americans and Hispanic Americans as in white Americans. Racial differences in the relationship between obesity and cardiovascular mortality are unlikely to be mediated by racial differences in obesity’s association with CRP levels. Adiposity may confer a more detrimental impact on inflammation in Mexican-Hispanic Americans, and therefore future research should clarify CRP’s role in predicting cardiovascular risk in this and other racial and ethnic minority groups.
Acknowledgments
The study was funded by a grant from the National Institutes of Health/National Institutes of Diabetes and Digestive and Kidney Diseases (R01 DK071083). We thank the Centers for Disease Control (CDC) and National Center for Health Statistics (NCHS) for providing the initial data. The analyses, interpretations, and conclusions are those of the authors, however, and do not reflect the views or opinions of the CDC, NCHS, or National Institutes of Health. The funder had no role in the analysis of data or the interpretations and conclusions of the authors.
Footnotes
DISCLOSURE
The authors declared no conflict of interest.
References
- 1.Mokdad AH, Marks JS, Stroup DF, Gerberding JL. Actual causes of death in the United States, 2000. JAMA. 2004;291:1238–1245. doi: 10.1001/jama.291.10.1238. [DOI] [PubMed] [Google Scholar]
- 2.Flegal KM, Carroll MD, Ogden CL, Johnson CL. Prevalence and trends in obesity among US adults, 1999–2000. JAMA. 2002;288:1723–1727. doi: 10.1001/jama.288.14.1723. [DOI] [PubMed] [Google Scholar]
- 3.Folsom AR, Stevens J, Schreiner PJ, McGovern PG. Body mass index, waist/hip ratio, and coronary heart disease incidence in African Americans and whites. Atherosclerosis Risk in Communities Study Investigators. Am J Epidemiol. 1998;148:1187–1194. doi: 10.1093/oxfordjournals.aje.a009608. [DOI] [PubMed] [Google Scholar]
- 4.Stevens J, Plankey MW, Williamson DF, et al. The body mass index-mortality relationship in white and African American women. Obes Res. 1998;6:268–277. doi: 10.1002/j.1550-8528.1998.tb00349.x. [DOI] [PubMed] [Google Scholar]
- 5.Stevens J. Obesity and mortality in Africans-Americans. Nutr Rev. 2000;58:346–353. doi: 10.1111/j.1753-4887.2000.tb01832.x. Review. [DOI] [PubMed] [Google Scholar]
- 6.Stevens J, Keil JE, Rust PF, et al. Body mass index and body girths as predictors of mortality in black and white women. Arch Intern Med. 1992;152:1257–1262. [PubMed] [Google Scholar]
- 7.Durazo-Arvizu R, Cooper RS, Luke A, et al. Relative weight and mortality in U.S. blacks and whites: findings from representative national population samples. Ann Epidemiol. 1997;7:383–395. doi: 10.1016/s1047-2797(97)00044-6. [DOI] [PubMed] [Google Scholar]
- 8.Calle EE, Thun MJ, Petrelli JM, Rodriguez C, Heath CW., Jr Body-mass index and mortality in a prospective cohort of U.S. adults. N Engl J Med. 1999;341:1097–1105. doi: 10.1056/NEJM199910073411501. [DOI] [PubMed] [Google Scholar]
- 9.Resnick HE, Valsania P, Halter JB, Lin X. Differential effects of BMI on diabetes risk among black and white Americans. Diabetes Care. 1998;21:1828–1835. doi: 10.2337/diacare.21.11.1828. [DOI] [PubMed] [Google Scholar]
- 10.Okosun IS. Racial differences in rates of type 2 diabetes in American women: how much is due to differences in overall adiposity? Ethn Health. 2001;6:27–34. doi: 10.1080/13557850120040379. [DOI] [PubMed] [Google Scholar]
- 11.Brown CD, Higgins M, Donato KA, et al. Body mass index and the prevalence of hypertension and dyslipidemia. Obes Res. 2000;8:605–619. doi: 10.1038/oby.2000.79. [DOI] [PubMed] [Google Scholar]
- 12.Tracy RP. Inflammation in cardiovascular disease. Circulation. 1998;97:2000–2002. doi: 10.1161/01.cir.97.20.2000. [DOI] [PubMed] [Google Scholar]
- 13.Ross R. Atherosclerosis: and inflammatory disease. N Engl J Med. 1999;340:115 – 126. doi: 10.1056/NEJM199901143400207. [DOI] [PubMed] [Google Scholar]
- 14.Ridker PM, Hennekens CH, Buring JE, Rifai N. C-reactive protein and other markers of inflammation in the prediction of cardiovascular disease in women. N Engl J Med. 2000;342:836–843. doi: 10.1056/NEJM200003233421202. [DOI] [PubMed] [Google Scholar]
- 15.Ridker PM, Rifai N, Rose L, Buring JE, Cook NR. Comparison of C-reactive protein and low-density lipoprotein cholesterol levels in the prediction of first cardiovascular events. N Engl J Med. 2002;347:1557–1565. doi: 10.1056/NEJMoa021993. [DOI] [PubMed] [Google Scholar]
- 16.Hackam DG, Anand SS. Emerging risk factors for atherosclerotic vascular disease: a critical review of the evidence. JAMA. 2003;290:932–940. doi: 10.1001/jama.290.7.932. Review. [DOI] [PubMed] [Google Scholar]
- 17.Ridker PM, Buring JE, Shih J, Matias M, Hennekens CH. Prospective study of C-reactive protein and the risk of future cardiovascular events among apparently healthy women. Circulation. 1998;98:731–733. doi: 10.1161/01.cir.98.8.731. [DOI] [PubMed] [Google Scholar]
- 18.Visser M, Bouter LM, McQuillan GM, Wener MH, Harris TB. Elevated C-reactive protein levels in overweight and obese adults. JAMA. 1999;282:2131–2135. doi: 10.1001/jama.282.22.2131. [DOI] [PubMed] [Google Scholar]
- 19.Greenberg AS, Obin MS. Obesity and the role of adipose tissue in inflammation and metabolism. Am J Clin Nutr. 2006;83:461S–465S. doi: 10.1093/ajcn/83.2.461S. Review. [DOI] [PubMed] [Google Scholar]
- 20.Esposito K, Pontillo A, Di Palo C, Giugliano G, Masella M, Marfella R, Giugliano D. Effect of weight loss and lifestyle changes on vascular inflammatory markers in obese women: a randomized trial. JAMA. 2003;289:1799–1804. doi: 10.1001/jama.289.14.1799. [DOI] [PubMed] [Google Scholar]
- 21.Selvin E, Paynter NP, Erlinger TP. The effect of weight loss on C-reactive protein: a systematic review. Arch Intern Med. 2007;167:31–39. doi: 10.1001/archinte.167.1.31. Review. [DOI] [PubMed] [Google Scholar]
- 22.National Center for Health Statistics. NHANES current data files. Available at < http://www.cdc.gov/nchs/about/major/nhanes/nhanes99-02.htm>.
- 23.National Center for Health Statistics. Plan and operation of the Third National Health and Nutritional Examination Survey, 1988–1994. Vital Health Stat 1. 1994;32:3–7. 11, 12, 16, 18, 20–22, 45–51, 121–181, 297–338. [PubMed] [Google Scholar]
- 24.National Health and Nutritional Examination Survey III, 1988–1994. Manual for Medical Technicians and Laboratory Procedures Used in NHANES III [book on CD-ROM] US Dept of Health and Human Services; Hyattsville, MD: 1997. [Google Scholar]
- 25.Gunter EW, Lewis BG, Konchikoski SM. Laboratory Procedures used for the Third National Health and Nutritional Examination Survey (NHANES III), 1988–1994. National Center for Health Statistics; Hyattsville, MD: 1997. p. IV-1.p. VII-M-1. [Google Scholar]
- 26.Ainsworth BE, Haskell WL, Whitt MC, et al. Compendium of physical activities: an update of activity codes and MET intensities. Med Sci Sports Exerc. 2000;32(Suppl 9):S498–S504. doi: 10.1097/00005768-200009001-00009. [DOI] [PubMed] [Google Scholar]
- 27.Pearson TA, Mensah GA, Alexander RW, et al. Markers of inflammation and cardiovascular disease: application to clinical and public health practice: a statement for healthcare professionals from the Centers for Disease Control and Prevention and the American Heart Association. Circulation. 2003;107:499–511. doi: 10.1161/01.cir.0000052939.59093.45. [DOI] [PubMed] [Google Scholar]
- 28.US Department of Health and Human Service. The practical guide—identification, evaluation, and treatment of overweight and obesity in adults. National Institutes of Health; Bethesda, MD: 2000. (NIH publication no. 00-4084.) [Google Scholar]
- 29.Shah BV, Barnwell BG, Hunt PN, La Vange LM. Release 5.50 with Addendum for SUDAAN Changes from 5.50 to 6.30. Research Triangle Institute; Research Triangle Park, NC: 1992. SUDAAN User’s Manual. [Google Scholar]
- 30.Carnethon MR, Palaniappan LP, Burchfiel CM, Brancati FL, Fortmann SP. Serum insulin, obesity, and the incidence of type-2 diabetes in black and white adults: the atherosclerosis risk in communities study: 1987–1998. Diabetes Care. 2002;25:1358–1364. doi: 10.2337/diacare.25.8.1358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Colin Bell A, Adair LS, Popkin BM. Ethnic differences in the association between body mass index and hypertension. Am J Epidemiol. 2002;155:346–353. doi: 10.1093/aje/155.4.346. [DOI] [PubMed] [Google Scholar]
- 32.Folsom AR, Chambless LE, Ballantyne CM, et al. An assessment of incremental coronary risk prediction using C-reactive protein and other novel risk markers: the atherosclerosis risk in communities study. Arch Intern Med. 2006;166:1368–1373. doi: 10.1001/archinte.166.13.1368. [DOI] [PubMed] [Google Scholar]
- 33.Wang TJ, Gona P, Larson MG, et al. Multiple biomarkers for the prediction of first major cardiovascular events and death. N Engl J Med. 2006;355:2631–2639. doi: 10.1056/NEJMoa055373. [DOI] [PubMed] [Google Scholar]
- 34.Albert MA, Ridker PM. C-reactive protein as a risk predictor: do race/ethnicity and gender make a difference? Circulation. 2006;114:e67–e74. doi: 10.1161/CIRCULATIONAHA.106.613570. [DOI] [PubMed] [Google Scholar]
- 35.Lakoski SG, Cushman M, Criqui M, et al. Gender and C-reactive protein: data from the Multiethnic Study of Atherosclerosis (MESA) cohort. Am Heart J. 2006;152:593–598. doi: 10.1016/j.ahj.2006.02.015. [DOI] [PubMed] [Google Scholar]
- 36.Anand SS, Razak F, Yi Q, et al. C-reactive protein as a screening test for cardiovascular risk in a multiethnic population. Arterioscler Thromb Vasc Biol. 2004;24:1509–1515. doi: 10.1161/01.ATV.0000135845.95890.4e. [DOI] [PubMed] [Google Scholar]
- 37.Albert MA, Glynn RJ, Buring J, Ridker PM. C-reactive protein levels among women of various ethnic groups living in the United States (from the Women’s Health Study) Am J Cardiol. 2004;93:1238–1242. doi: 10.1016/j.amjcard.2004.01.067. [DOI] [PubMed] [Google Scholar]