Abstract
Objective. While there has been a great deal of speculation by clinical researchers over the last three decades on effective and safe methods for the pharmacological management of aggression in children and adolescents, it is only in the last decade that there have been well-designed studies available to address this issue. Medication is commonly used to control aggression in children and adolescents in inpatient units. Also, there exists a need for evidence-based guidelines for the use of these different pharmacological agents for managing pediatric aggression on inpatient units. The aims of this article are to provide a systemic review and to provide treatment guidelines based on these limited but currently available studies.
Methods. The articles reviewed in this study were obtained through a PubMed search using the key words ‘children,’ ‘adolescents,’ ‘aggression,’ ‘inpatient,’ ‘ziprasidone,’ ‘lithium,’ and ‘risperidone.’ A total of 499 studies were generated. Only studies focusing on pharmacological management of inpatient pediatric aggression with mean duration less than six weeks and published during January 1980 to August 2009 were included. Only English articles were considered. A total of 13 studies met these criteria, which were included in the review without any further statistical analysis. Recommendations are made on this available evidenced-based literature.
Results. There is some evidence for the standing use of oral lithium, haloperidol, olanzapine, and risperidone for aggression related to specific psychiatric diagnoses. Intramuscular ziprasidone and olanzapine administered as needed were found to be effective for the rapid management of moderate to severe aggression. Oral or intramuscular diphenhydramine administered as needed was found to be useful for managing mild aggression due to a placebo effect.
Conclusions. Studies are available on managing aggression in children and adolescents in inpatient treatment settings but are limited. Further studies on the use of various psychotropic medications are needed in order to develop comprehensive guidelines for the safe and effective pharmacological management of child and adolescent inpatient aggression.
Keywords: children, adolescents, aggression, inpatient, ziprasidone, behavioral, psychiatric, antipsychotics, management
Introduction
Although there are many studies on the use of psychotropic medications to treat pathological aggression in children and adolescents,1 research is limited and often conflicting on the use of medications to treat aggression in hospitalized pediatric patients. Medications prescribed on an as-needed basis (PRN) are frequently used2,3 to manage aggression or disruptive behavior on inpatient units, but the studies supporting the use of this method with children and adolescents are mixed. In contrast, adult studies on the use of PRN medications for agitation suggest effectiveness.4 Furthermore, atypical antipsychotics administered on a regular basis have been found to reduce the use of seclusion and restraints on adult psychiatric patients.5–7 However, the effectiveness of scheduled atypical antipsychotic medications with child and adolescent inpatients is still not as clearly established.
A study investigating aggressive incidents and the use of restraints on inpatient units reported that PRN medications were used in 38 percent of incidences before restraints and in 22 percent of incidences during restraints.8 Despite their frequent use, the evidence is limited to support the effectiveness of PRN medications for inpatient aggressive pediatric patients. A study on PRN medication for 49 children on an inpatient unit found that PRN medications were effective in only one-third (32%) of the total incidences.3 The purpose of this review article is to explore the recent but limited evidence for the use of medication for inpatient pediatric aggression in order to provide practical clinical guidelines based on the available studies.
Methods
We conducted the PubMed electronic database search using words ‘children,’ ‘adolescents,’ ‘aggression,’ ‘inpatient,’ ‘ziprasidone,’ ‘lithium,’ and ‘risperidone.’ The different combinations of these words were used as follows: 1) ‘children+adolescents+inpatient+aggression;’ 2) ‘ziprasidone+children’, 3) ‘ziprasidone+adolescents;’ 4) ‘lithium+children+adolescents+aggression;’ and 5) ‘risperidone+adolescents+aggression. A total of 499 related studies were generated using these combinations. Out of these, we only included the studies focusing on the pharmacological management of aggression in hospitalized children and adolescents. Only studies in the date range January 1980 to August 2009 were included. Studies more than six weeks of mean duration were excluded. Only studies in English were considered. Studies on both PRN and standing use of medications were considered. A total of 13 studies met these criteria. As these studies were lacking consistency in their methods, all of these 13 studies were considered for review without any further statistical analysis. Recommendations were made mainly based on the data from these studies.
Results
The following studies examine the usefulness of psychotropic medications for managing inpatient child and adolescent aggression.
Antihistaminics. Antihistamines, particularly first generation (older) antihistamines, are known to have effects on the central nervous system by causing rapid sedation and slowing down psychomotor performance and cognitive function.9,10 Antihistamines are the most frequently prescribed medication for hospitalized pediatric patients for inducing sleep11 and may be considered to be appropriate for usage in medically ill children with behavioral instability. Diphenhydramine (an antihistamine) can be administered by oral, intramuscular (IM), and intravenous (IV) route and is generally well tolerated.10 The potential for serious side effects exists. If the patient experiences airway or cardiac problems, then vigilant monitoring is required.10 Despite the common use of antihistamines for aggression and agitation, there is only one published, controlled study for an antihistamine (diphenhydramine) on managing child and adolescent aggression on psychiatric inpatient units on acute basis.2
Diphenhydramine (Benadryl). In this double-blind, placebo-controlled, pilot study of an antihistamine for 21 male patients (aged 5–13 years old), PRN diphenhydramine was not superior to placebo in reducing aggression, as there was a significant placebo effect. Interestingly, the most effective route of administration for reducing aggression was IM, regardless of whether the injection contained diphenhydramine or placebo.2
Mood stabilizers. Divalproex was found to be effective in reducing aggressive episodes in outpatient pediatric population after a random placebo-controlled clinical trial of six weeks.12 However, after doing a literature search, we conclude that lithium carbonate and carbamazepines are the only scheduled mood stabilizers studied for treating child and adolescent inpatient aggression.
Lithium carbonate (Eskalith). Malone et al13 in 2000 conducted a double-blind, placebo-controlled study of 40 hospitalized aggressive children and adolescents with conduct disorder (CD). Lithium was superior compared to placebo in terms of decreasing inpatient aggression as measured by the Overt Aggression Scale (OAS) over four weeks of inpatient treatment. However, as compared to placebo, patients on lithium did experience side effects other than weight gain, such as increase in urinary frequency and gastrointestinal side effects (e.g., vomiting and nausea).13 In an older study, 61 inpatient children (from 5.2–12.9 years) with diagnoses of conduct disorder, aggressive type and resistant to treatment were treated with haloperidol and oral lithium carbonate over a four-week period. This was also a double-blind, controlled study with the use of placebo versus haloperidol or lithium. Lithium carbonate and haloperidol were both found to be superior to placebo in reducing aggressive behavior. Regarding safety, lithium was less frequently associated with unwanted side effects. The most common unwanted side effects associated with haloperidol were drowsiness, followed by acute dystonia. The most common unwanted side effects associated with lithium were stomachache and headache.14
Another double-blind, placebo-controlled study of lithium carbonate with 33 inpatients (aged 12–17 years) with CD showed no improvement in aggression based on OAS ratings after two weeks of treatment.15 This may suggest that lithium carbonate should be continued for at least four weeks in order to observe improvement in child and adolescent inpatient aggression. This time course of efficacy may not be practical for most inpatient units with short hospital stays but may be more appropriate for child and adolescent residential units or state hospitals. Drugs having more rapid onset that can be used as PRN and that have a minimal side effect profile would be the best choice for controlling aggression on inpatient child psychiatry units. Giving lithium and monitoring the levels for weeks on inpatient units may not be a practical approach.
Carbamazepine (Tegretol). Ten hospitalized patients aged 5 to 10 years with CD showed improvement in inpatient aggression after three weeks of treatment with carbamazepine. However, this was an open pilot study.16 In a double-blind, placebo-controlled study, Cueva et al17 in 1996 studied the effect of carbamazepine in children with treatment-resistant aggression.22 Inpatient children with CD (age range 5–12 years) were randomized to receive carbamazepine or placebo for six weeks. Surprisingly, the study concluded that both carbamazepine and the placebo had similar clinical outcomes.17 Therefore, we need to evaluate a different category of medication other than mood stabilizers that would be rapidly effective for inpatient pathologic pediatric aggression.
Atypical antipsychotics. The use of atypical antipsychotics has expanded to treat a broad range of psychiatric diagnoses for children and adolescents despite the limited empirical evidence supporting their efficacy.18 For acute treatment of aggression on child and adolescent inpatient units, ziprasidone is the most extensively studied atypical antipsychotic medication. The usefulness of other antipsychotics is also discussed.
Ziprasidone (Geodon). Ziprasidone was the first atypical antipsychotic available in IM form19 and this might be the reason that it was observed as the most extensively studied antipsychotic for managing aggression in inpatient children and adolescents. Ziprasidone has been found to be beneficial in treating aggression in child and adolescent inpatients20–24 as well as adolescents in the emergency room.47 A case report of three youths treated with IM ziprasidone reported an immediate beneficial effect on controlling the aggressive episode on the inpatient child psychiatry unit.22 A retrospective study comparing the efficacy of IM ziprasidone and IM olanzapine PRN in 100 juvenile (younger than 18 years) psychiatric inpatients found that these medications were similar in terms of their ability to address inpatient aggression.20 However, patients taking IM ziprasidone received significantly more doses of IM ziprasidone, as well as other potentially calming medications, such as antihistamines or lorazepam. Somnolence was the most common side effect noted during this study for either IM ziprasidone or IM olanzapine. Neither medication had any documented significant effect on QTc interval, blood pressure, or heart rate.20 At this time, it is not possible to put together definitive conclusions for the safety of using IM ziprasidone and IM olanzapine with children, given the possibility that adverse events have been inadequately charted in this retrospective study.20
In another retrospective study, treatment with IM ziprasidone was compared to IM haloperidol with lorazepam for severe aggressive episodes in adolescents (12–17 year olds) in psychiatric emergency rooms.24 Both treatment groups had similar outcomes in regards to restraint time and use of rescue medications. Behavior Activity Rating Scale (BARS) scores were available only for 7 out of 28 adolescents that received IM ziprasidone. The BARS scores in these seven subjects started decreasing immediately after the IM ziprasidone injection and had a significant decrease after one half hour and continued to decrease up to two hours. Although no severe side effects, such as profound somnolence, were found, side effects may not have been monitored or documented carefully.24 Nonetheless, the authors conclude that IM ziprasidone should be considered since it leads to a similar clinical outcome while avoiding potential severe adverse events associated with typical antipsychotic medications such as haloperidol.24
Olanzapine (Zyprexa). A study of five inpatients (aged 6–11 years) treated with open-label, oral olanzapine for 2 to 7 weeks found improvement in aggression in three of the children, but treatment was discontinued for all five of the patients due to unfavorable side effects or being short of therapeutic response. Side effects included significant weight gain, akathisia, and sedation.25
Risperidone (Risperdal). Risperidone is considered the most effective and safe in the treatment of aggression in children as per most of the available studies.1 Risperidone was also found to be useful in reducing aggression in children with autism.26 However, risperidone was only “modestly” effective in managing the treatment-resistant aggression in a short-term outpatient study of 25 children with attention deficit hyperactivity disorder (ADHD).27 In this double-blind study, risperidone was added to the psychostimulant treatment.27
Most of the risperidone studies were conducted in outpatient settings and are targeted to treat chronic aggression rather than acute inpatient aggression. As per our search, only one study has attempted to observe the effects of risperidone in treating the aggression in an inpatient unit. In this study, 38 aggressive adolescent inpatients with CD and other oppositional problems were randomly assigned to risperidone or placebo treatment for six weeks in a double-blind, placebo-controlled, randomized clinical trial. Risperidone was superior to placebo in reducing aggression. The most common side effect was drowsiness.28
Quetiepine (seroquel). As per our search, short-term studies on assessing the effectiveness quetiepine for inpatient pediatric aggression are not available at this time. However, in one short-term (eight week), open-label, outpatient study (including 6–12 year old children with CD), quetiepine was found to be helpful and well tolerated when targeting aggression.29
Aripiprazole (Abilify). Although the inpatient studies on aripiprazole for pediatric aggression are also lacking, one open-label study of 15-day duration suggests that it is effective and safe in reducing aggression in children and adolescents with CD.30
Summary. Overall, PRN use of IM ziprasidone and IM olanzapine and standing use of risperidone may have a positive effect for inpatient aggression on child and adolescent psychiatry units. PRN use of IM ziprasidone and IM olanzapine has a rapid onset of action but safety data is limited. Considering the effectiveness of quetiepine and aripirazole after short-term use, these medications may also be considered for this purpose.
Typical antipsychotics. According to our literature review search results, the standardized studies of typical antipsychotic medications in reducing aggression in inpatient pediatric patients are limited. Since acute dystonia is notably associated with a younger age, it limits the utility of typical antipsychotics for the management of agitation in pediatric patients.31
Haloperidol (Haldol). Our search showed that the controlled trials for efficacy and safety profile for haloperidol PRN use in treating hospitalized pediatric patients are lacking. As mentioned previously, four weeks of haloperidol treatment has been found to be effective in reducing aggression in hospitalized children and adolescents with CD.14
Special safety issues with antispychotic medications. A few rare but acute serious side effects, such as acute dystonia (in the form of torticollis),32 akathisia,33 and neuroleptic malignant syndrome (NMS),34 are reported in children and adolescents. It is necessary to consider these underestimated side effects before starting antipsychotic medication in children and adolescents (Table 1).
Table 1.
Available pharmacological studies on management of inpatient pediatric aggression
| STUDY | MEDICATION | ROUTE | TYPE OF STUDY | DIAGNOSES | AGE GROUP | DOSE | FREQUENCY AND DURATION | CLINICAL OUTCOME | SIDE EFFECTS | NO. PATIENTS |
|---|---|---|---|---|---|---|---|---|---|---|
| Khan et al (2006)20 | Ziprasidone (Geodon*) | IM | Retrospective chart review | Bipolar with psychotic features; MDD with psychotic features; psychosis NOS; MDD NOS; substance use/dependence; TSD | Mean age 14.6±2.1 yrs. (included children as well as adolescents) | 20mg (15.66±4.35) for children; 20mg (19.45±2.13) for adolescents | PRN | Effective for decreasing aggression | Somnolence, no EKG changes (QTc) | 50 |
| Barzman et al (2007)21 | Ziprasidone (Geodon*) | IM | Retrospective chart review | Bipolar; MDD; MDD NOS; psychotic disorder; disruptive disorder; ADHD; impulse control disorder | 12–19 years | 20mg (81% received) | PRN | "Much to very much improved" (81%) "minimally improved" (16%) "no change" (1.3 %) "minimally worse" (1.3%) "much worse" (1.3 %) | Somnolence (60%) | 59 |
| Hazarey et al. (2004)22 | Ziprasidone (Geodon*) | IM | Case report | CD; ADHD; explosive outburst; GAD; oppositional defiant disorder; bipolar NOS | 12–13 years | 10mg | PRN | Immediate calming down effect and going to sleep | Syncope—reported only in one patient | 3 |
| Stellar et al (2004)23 | Ziprasidone (Geodon*) | IM | Retrospective chart review | Not available | 8–16 yrs | 20mg (87% received) | PRN | Effecitve in management of acute behavioral discontrol | None reported | 49 |
| Khan et al (2006)20 | Olanzapine (Zyprexa*) | IM | Retrospective chart review | Bipolar with psychotic features; MDD with psychotic features; psychosis NOS; MDD NOS; substance use/dependence; PTSD | 13.7±2.4 (included children as well as adolescents) | 5mg (5.92±2.18) for children, 10mg (9.17±1.77) for adolescents | PRN | Effective for deacreasing aggression | Drowsiness, no EKG changes ( QTc) | 50 |
| Krishnamoorthy et al (1998)25 | Olanzapine (Zyprexa*) | PO | Open label | Bipolar, psychosis NOS, schizophrenia, ADHD | 6–11 years | 7.5mg (22mg/kg) | Daily for 32 days (Range 2–7 weeks) | Better control of aggression in three out of five patients | Sedation, weight gain (upto 16 lbs), akathasia | 5 |
| Campbell et al (1984)14 | Haloperidol (Haldol*) | PO | Double blind, placebo controlled | CD aggressive type | 5.2–12.9 years | 1 to 6mg (0.04–0.21mg/kg/day) | Daily for 6 weeks | Superior than placebo to control aggression (made child more manageable) | Drowsiness most common in frequency followed by acute dystonia | 61 |
| Buitelaar JK et al (2001)28 | Risperidone (Risperdal*) | PO | Double blind, randomized (parallel group design) | Disruptive disorder | adolescents | 2.9mg (1.5–4mg) | Daily for 6 weeks | Significant improvement in Overt Aggression Scale | Transient fatigue in more than half of the patients, GI symptoms—nausea, sialorrhea. No EKG changes, no effect on BP | 38 |
| Campbell et al (1984)14 | Lithium Carbonate (Eskalith*) | PO | Double blind, placebo controlled | CD aggressive type | 5.2–12.9 years | 500–2000mg (Serum lithium level 0.32–1.51mEq/liter) | Daily for 6 weeks | Superior than placebo to control aggression (reduce explosiveness) | Weight gain more than 30kg, stomachaches, headaches, hand tremors | 61 |
| Rifkin et al (1997)15 | Lithium Carbonate (Eskalith*) | PO | Double blind, placebo controlled | CD (IQ >70) | 12–17 years | Variable dose to maintain blood lithium level of 0.6 to 1mmol/litre | Daily for 2 weeks | No significant effects on decreasing the score in Overt Agression Scale | Side effects due to autonomic system malfunctioning | 33 |
| Malone et al (2000)13 | Lithium Carbonate (Eskalith*) | PO | Double-blind placebo controlled | CD | Median age 12.7 years | 300–2100mg to maintain the level of 0.8–1Mmol/litre | Daily for 4 weeks | Rating on Overt Agression Scale decreased as compared to placebo | GI symptoms: nausea, vomiting and more than 50% patients experiencing increased frequency of urine | 40 |
| Vitiello et al (1991)2 | Diphenhydramine (Benadryl*) | PO/IM | Double-blind placebo controlled | CD, ADHD, MDD | 5–13 years | 25–50mg | PRN | IM more effective than PO | Sedation | 21 |
| Jangro et al (2009)47 | Ziprasidone (Geodon*) vs haloperidol and lorazepam | IM | Retrospective chart review | Substance use/dependence, psychotic disorders, adjustment disorders, impulse control disorder | 12–17 years | 20mg (82% received) 10mg (18% received) | PRN | There were no differences between the two treatment groups in the outcomes of restraint duration or use of rescue medications | Decreased pulse | 52 |
Abbreviations:
- Pts
patients
- IM
intramuscular
- PO
per oral
- MDD
major depressive disorder
- NOS
not otherwise specified
- yrs
years
- PRN
as needed
- QTc
QT interval on EKG
- BP
blood pressure
- H
heart rate
- ADHD
attention deficit hyperactivity disorder
- CD
conduct disorder
- GAD
generalized anxiety disorder
- PTSD
posttraumatic stress disorder
- GI
gastrointestinal
- EKG
electrocardiogram
Trade name
Benzodiazepines. It is found that the use of benzodiazepines in children and adolescents can be associated with a paradoxical reaction including agitation and other adverse side effects.35 Abuse, dependence, and withdrawal symptoms are further clinical issues with these medications in adults36 and similar risk of withdrawal exists in children.37 A case report also suggested that benzodiazepines in children could induce psychotic symptoms in a physically abused child.38 Despite these risks, benzodiazepines are still being preferred to treat pediatric agitation39, 40 even though standardized studies assessing the usefulness and adverse effects of benzodiazepine monotherapy in treating inpatient aggression in children or adolescents are lacking.
The Assessment of Aggression and Nonpharmacological Treatment Approaches
Aggression in children and adolescents can be “reactive” (impulsive and emotional in response to a trigger) and/or “proactive” (intentional and planned to fulfill a preconceived objective).41 However, any form of aggression has the potential of severe and unexpected adverse outcomes on child inpatient units. Distinguishing the root cause, type, and identifying the warning signs of aggression may be beneficial in developing the individual treatment plan. For example, the “reactive” form of aggression shows more response to medication than the “proactive” form of aggression.42
Nevertheless, even if the aggression is mostly “reactive” on a child psychiatry inpatient unit, a behavioral approach such as collaborative problem solving (CPS) can be successfully implemented to help manage the aggression, which may minimize the use of medications.43 Relaxation techniques,44 creative art therapy,44 and maintaining the inpatient milieu45 are also found to be helpful in reducing aggression in children and adolescents.
Conclusions and Recommendations
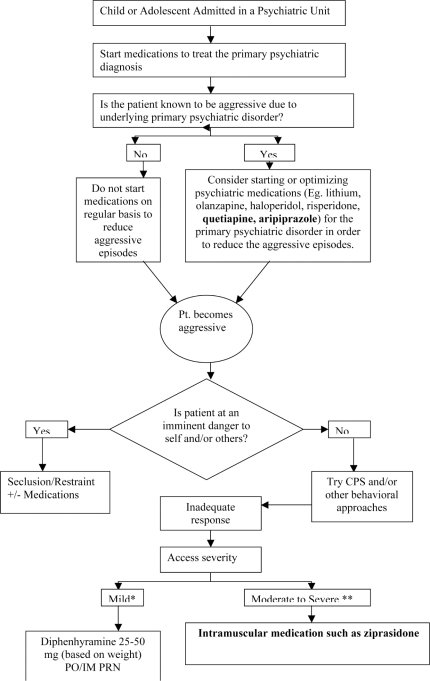
Based on the available literature, the authors have developed a flow chart to illustrate the recommended treatment approach for managing child and adolescent inpatient aggression (Figure 1). Treatment should address the primary psychiatric condition, which may decrease the pathological aggression. Standing psychotropic medications should be started or optimized for the most impairing primary psychiatric disorder. A similar protocol was developed for pediatric patients in the emergency room, which begins with nonpharmacological interventions and then progresses to oral “symptom-specific” medication followed by “general agitation” medication if agitation persists.40
Figures 1.
Pharmacological management of child and adolescent inpatient aggression
Key:
- CPS
- collaborative problem solving
PRN medication should not be used unless the patient clearly exhibits severe aggression, and psychosocial interventions and/or standing medications (when indicated) have not proven sufficient to reduce aggression to manageable levels.46 If a patient does not actually need a medication, prescribing one will put him or her at unnecessary risk of dangerous side effects, such as NMS when an antipsychotic is used. If an acute safety issue arises, the PRN medication choice should be restricted to safe, effective, and rapid-acting medication.
Medication must also be appropriate to the severity of the aggression. Mild aggression, such as no property destruction (with or without threatening behavior), can be managed with psychosocial interventions. A weight-based dose of diphenhydramine PRN can be considered for mild aggression but it should be noted that the beneficial effect may be due to a placebo effect. Moderate-to-severe aggression or threatening behavior with severe distress can be treated with either IM ziprasidone (20mg for both children and adolescents) or olanzapine (5mg for children and 10mg for adolescents). However, if the pediatric patient is imminently dangerous to self or others, it may be necessary to rapidly address the situation through the use seclusion and/or restraints with or without psychotropic medication. These recommendations are made based on the available limited evidence that was discussed in this review article. Further prospective, controlled studies are needed on oral and IM psychiatric medications for the treatment of child and adolescent inpatient aggression.
Comprehensive recommendations cannot be made until other psychotropic medications are studied for their potential to treat child and adolescent inpatient aggression. The recommendations in this article are intended to serve as helpful general guidelines, but all decisions about medicating a patient (including the choice of medication and the dose) must always be individualized by a trained clinician based on the patient’s medical history, diagnoses, and other pertinent factors.
Footnotes
Mild distress, no property destruction, no threatening behavior;
Moderate-to-severe distress, patient exhibiting property destruction and/or threatening behavior
Contributor Information
Parikshit Deshmukh, Dr. Deshmukh is a resident with the Division of Psychiatry, University Hospitals Case Medical Center, Cleveland, Ohio.
Guarav Kulkarni, Dr. Kulkarni is Research Assistant, Child and Adolescent Forensic Psychiatry Service, Division of Child and Adolescent Psychiatry, Cincinnati Children's Hospital Medical Center, Cincinnati, Ohio.
Drew Barzman, Dr. Barzman is Director, Child and Adolescent Forensic Psychiatry Service, Division of Child and Adolescent Psychiatry, Cincinnati Children's Hospital Medical Center, Cincinnati, Ohio.
References
- 1.Barzman DH, Findling RL. Pharmacological treatment of pathologic aggression in children. Int Rev Psychiatry. 2008;20(2):151–157. doi: 10.1080/09540260801887819. [DOI] [PubMed] [Google Scholar]
- 2.Vitiello B, Hill JL, Elia J, et al. P.R.N. medications in child psychiatric patients: a pilot placebo-controlled study. J Clin Psychiatry. 1991;52(12):499–501. [PubMed] [Google Scholar]
- 3.Vitiello B, Ricciuti AJ, Behar D. P.R.N. medications in child state hospital inpatients. J Clin Psychiatry. 1987;48(9):351–354. [PubMed] [Google Scholar]
- 4.Srivastava A. Limited evidence for the effectiveness of p.r.n. medications among psychiatric inpatients. J Psychiatr Pract. 2009;15(3):193–201. doi: 10.1097/01.pra.0000351879.52883.10. [DOI] [PubMed] [Google Scholar]
- 5.Chengappa KN, Levine J, Ulrich R, et al. Impact of risperidone on seclusion and restraint at a state psychiatric hospital. Can J Psychiatry. 2000;45(9):827–832. doi: 10.1177/070674370004500907. [DOI] [PubMed] [Google Scholar]
- 6.Chengappa KN, Ebeling T, Kang JS, et al. Clozapine reduces severe self-mutilation and aggression in psychotic patients with borderline personality disorder. J Clin Psychiatry. 1999;60(7):477–484. doi: 10.4088/jcp.v60n0710. [DOI] [PubMed] [Google Scholar]
- 7.Chengappa KN, Vasile J, Levine J, et al. Clozapine: its impact on aggressive behavior among patients in a state psychiatric hospital. Schizophr Res. 2000;53(1–2):1–6. doi: 10.1016/s0920-9964(00)00175-4. [DOI] [PubMed] [Google Scholar]
- 8.Delaney KR, Fogg L. Patient characteristics and setting variables related to use of restraint on four inpatient psychiatric units for youths. Psychiatr Serv. 2005;56(2):186–192. doi: 10.1176/appi.ps.56.2.186. [DOI] [PubMed] [Google Scholar]
- 9.Banerji A, Long AA, Camargo CA., Jr. Diphenhydramine versus nonsedating antihistamines for acute allergic reactions: a literature review. Allergy Asthma Proc. 2007;28(4):418–426. doi: 10.2500/aap.2007.28.3015. [DOI] [PubMed] [Google Scholar]
- 10.Cummings MR, Miller BD. Pharmacologic management of behavioral instability in medically ill pediatric patients. Curr Opin Pediatr. 2004;16(5):516–522. doi: 10.1097/01.mop.0000139300.13152.20. [DOI] [PubMed] [Google Scholar]
- 11.Meltzer LJ, Mindell JA, Owens JA, Byars KC. Use of sleep medications in hospitalized pediatric patients. Pediatrics. 2007;119(6):1047–1055. doi: 10.1542/peds.2006-2773. [DOI] [PubMed] [Google Scholar]
- 12.Donovan SJ, Stewart JW, Nunes EV, et al. Divalproex treatment for youth with explosive temper and mood lability: a double-blind, placebo-controlled crossover design. Am J Psychiatry. 2000;157(5):818–820. doi: 10.1176/appi.ajp.157.5.818. [DOI] [PubMed] [Google Scholar]
- 13.Malone RP, Delaney MA, Luebbert JF, et al. A double-blind placebo-controlled study of lithium in hospitalized aggressive children and adolescents with conduct disorder. Arch Gen Psychiatry. 2000;57(7):649–654. doi: 10.1001/archpsyc.57.7.649. [DOI] [PubMed] [Google Scholar]
- 14.Campbell M, Small AM, Green WH, et al. Behavioral efficacy of haloperidol and lithium carbonate: a comparison in hospitalized aggressive children with conduct disorder. Arch Gen Psychiatry. 1984;41(7):650–656. doi: 10.1001/archpsyc.1984.01790180020002. [DOI] [PubMed] [Google Scholar]
- 15.Rifkin A, Karajgi B, Dicker R, et al. Lithium treatment of conduct disorders in adolescents. Am J Psychiatry. 1997;154(4):554–555. doi: 10.1176/ajp.154.4.554. [DOI] [PubMed] [Google Scholar]
- 16.Kafantaris V, Campbell M, Padron-Gayol MV, et al. Carbamazepine in hospitalized aggressive conduct disorder children: an open pilot study. Psychopharmacol Bull. 1992;28(2):193–199. [PubMed] [Google Scholar]
- 17.Cueva JE, Overall JE, Small AM, et al. Carbamazepine in aggressive children with conduct disorder: a double-blind and placebo-controlled study. J Am Acad Child Adolesc Psychiatry. 1996;35(4):480–490. doi: 10.1097/00004583-199604000-00014. [DOI] [PubMed] [Google Scholar]
- 18.Findling RL, Steiner H, Weller EB. Use of antipsychotics in children and adolescents. J Clin Psychiatry. 2005;66(7):29–40. [PubMed] [Google Scholar]
- 19.Brook S. Intramuscular ziprasidone: moving beyond the conventional in the treatment of acute agitation in schizophrenia. J Clin Psychiatry. 2003;64(19):13–18. [PubMed] [Google Scholar]
- 20.Khan SS, Mican LM. A naturalistic evaluation of intramuscular ziprasidone versus intramuscular olanzapine for the management of acute agitation and aggression in children and adolescents. J Child Adolesc Psychopharmacol. 2006;16(6):671–677. doi: 10.1089/cap.2006.16.671. [DOI] [PubMed] [Google Scholar]
- 21.Barzman DH, DelBello MP, Forrester JJ, et al. A retrospective chart review of intramuscular ziprasidone for agitation in children and adolescents on psychiatric units: Prospective studies are needed. J Child Adolesc Psychopharmacol. 2007;17(4):503–509. doi: 10.1089/cap.2007.5124. [DOI] [PubMed] [Google Scholar]
- 22.Hazaray E, Ehret J, Posey DJ, et al. Intramuscular ziprasidone for acute agitation in adolescents. J Child Adolesc Psychopharmacol. 2004;14(3):464–470. doi: 10.1089/cap.2004.14.464. [DOI] [PubMed] [Google Scholar]
- 23.Staller JA. Intramuscular ziprasidone in youth: a retrospective chart review. J Child Adolesc Psychopharmacol. 2004;14(4):590–592. doi: 10.1089/cap.2004.14.590. [DOI] [PubMed] [Google Scholar]
- 24.Jangro WC, Preval H, Southard R, et al. Conventional intramuscular sedatives versus ziprasidone for severe agitation in adolescents: case-control study. Child Adolesc Psychiatry Ment Health. 2009;3(1):9. doi: 10.1186/1753-2000-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Krishnamoorthy J, King BH. Open-label olanzapine treatment in five preadolescent children. J Child Adolesc Psychopharmacol. 1998;8(2):107–113. doi: 10.1089/cap.1998.8.107. [DOI] [PubMed] [Google Scholar]
- 26.Parikh MS, Kolevzon A, Hollander E. Psychopharmacology of aggression in children and adolescents with autism: a critical review of efficacy and tolerability. J Child Adolesc Psychopharmacol. 2008;18(2):157–178. doi: 10.1089/cap.2007.0041. [DOI] [PubMed] [Google Scholar]
- 27.Armenteros JL, Lewis JE, Davalos M. Risperidone augmentation for treatment-resistant aggression in attention-deficit/hyperactivity disorder: a placebo-controlled pilot study. J Am Acad Child Adolesc Psychiatry. 2007;46(5):558–565. doi: 10.1097/chi.0b013e3180323354. [DOI] [PubMed] [Google Scholar]
- 28.Buitelaar JK, van der Gaag RJ, Cohen-Kettenis P, Melman CT. A randomized controlled trial of risperidone in the treatment of aggression in hospitalized adolescents with subaverage cognitive abilities. J Clin Psychiatry. 2001;62(4):239–248. doi: 10.4088/jcp.v62n0405. [DOI] [PubMed] [Google Scholar]
- 29.Findling RL, Reed MD, O’Riordan MA, et al. Effectiveness, safety, and pharmacokinetics of quetiapine in aggressive children with conduct disorder. J Am Acad Child Adolesc Psychiatry. 2006;45(7):792–800. doi: 10.1097/01.chi.0000219832.23849.31. [DOI] [PubMed] [Google Scholar]
- 30.Findling R, Blumer J, Kauffman R, et al. Pharmacokinetic effects of aripiprazole in children and adolescents with conduct disorder. Int J Neuropsychopharmacol. 2004;7:S440. [Google Scholar]
- 31.Aguilar EJ, Keshavan MS, Martínez-Quiles MD, et al. Predictors of acute dystonia in first-episode psychotic patients. Am J Psychiatry. 1994;151:1819–1821. doi: 10.1176/ajp.151.12.1819. [DOI] [PubMed] [Google Scholar]
- 32.Singh MK, DelBello MP, Adler CM. Acute dystonia associated with aripiprazole in a child. J Am Acad Child Adolesc Psychiatry. 2007;46(3):306–307. doi: 10.1097/chi.0b013e31802ed925. [DOI] [PubMed] [Google Scholar]
- 33.Barzman DH, DelBello MP, Kowatch RA, et al. The effectiveness and tolerability of aripiprazole for pediatric bipolar disorders: a retrospective chart review. J Child Adolesc Psychopharmacol. 2004;14(4):593–600. doi: 10.1089/cap.2004.14.593. [DOI] [PubMed] [Google Scholar]
- 34.Chungh DS, Kim BN, Cho SC. Neuroleptic malignant syndrome due to three atypical antipsychotics in a child. J Psychopharmacol. 2005;19(4):422–425. doi: 10.1177/0269881105053310. [DOI] [PubMed] [Google Scholar]
- 35.Massanari M, Novitsky J, Reinstein LJ. Paradoxical reactions in children associated with midazolam use during endoscopy. Clin Pediatr (Phila). 1997;36(12):681–684. doi: 10.1177/000992289703601202. [DOI] [PubMed] [Google Scholar]
- 36.O’Brien CP. Benzodiazepine use, abuse, and dependence. J Clin Psychiatry. 2005;66(2):28–33. [PubMed] [Google Scholar]
- 37.Birchley G. Opioid and benzodiazepine withdrawal syndromes in the pediatric intensive care unit: a review of recent literature. Nurs Crit Care. 2009;14(1):26–37. doi: 10.1111/j.1478-5153.2008.00311.x. [DOI] [PubMed] [Google Scholar]
- 38.Marcus A, Ammermann C, Bahro M, Schmidt MH. Benzodiazepine administration induces exogenic psychosis: a case of child abuse. Child Abuse Negl. 1995;19(7):833–836. doi: 10.1016/0145-2134(95)00049-e. [DOI] [PubMed] [Google Scholar]
- 39.Dorfman D, Kastner B. The use of restraint for pediatric psychiatric patients in emergency departments. Pediatr Emerg Care. 2004;20:151–156. doi: 10.1097/01.pec.0000117921.65522.fd. [DOI] [PubMed] [Google Scholar]
- 40.Hilt RJ, Woodward TA. Agitation treatment for pediatric emergency patients. J Am Acad Child Adolesc Psychiatry. 2008;47(2):132–138. doi: 10.1097/chi.0b013e31815d95fd. [DOI] [PubMed] [Google Scholar]
- 41.Connor DF, Steingard RJ, Cunningham JA, et al. Proactive and reactive aggression in referred children and adolescents. Am J Orthopsychiatry. 2004;74(2):129–136. doi: 10.1037/0002-9432.74.2.129. [DOI] [PubMed] [Google Scholar]
- 42.Steiner H, Saxena K, Chang K. Psychopharmacologic strategies for the treatment of aggression in juveniles. CNS Spectr. 2003;8(4):298–308. doi: 10.1017/s1092852900018514. [DOI] [PubMed] [Google Scholar]
- 43.Greene RW, Ablon JS. Treating Explosive Kids: The Collaborative Problem Solving Approach. New York: Guilford; 2005. [Google Scholar]
- 44.Bornman BA, Mitelman SA, Beer DA. Psychotherapeutic relaxation: How it relates to levels of aggression in a school within inpatient child psychiatry: a pilot study. The Arts in Psychotherapy. 2007;34(3):216–222. [Google Scholar]
- 45.Malone RP, Luebbert JF, Delaney MA. Nonpharmacological response in hospitalized children with conduct disorder. J Am Acad Child Adolesc Psychiatry. 1997;36(2):242–247. doi: 10.1097/00004583-199702000-00015. [DOI] [PubMed] [Google Scholar]
- 46.dosReis S, Barnett S, Love RC, Riddle MA. The Maryland Youth Practice Improvement Committee. A guide for managing acute aggressive behavior of youths in residential and inpatient treatment facilities. Psychiatric Serv. 2003;54(10):1357–1363. doi: 10.1176/appi.ps.54.10.1357. [DOI] [PubMed] [Google Scholar]
- 47.Jangro WC, Preval H, Southard R, Klotz SG, et al. Conventional intramuscular sedatives versus ziprasidone for severe agitation in adolescents: case-control study. Child Adolesc Psychiatry Ment Health. 2009;3(1):9. doi: 10.1186/1753-2000-3-9. [DOI] [PMC free article] [PubMed] [Google Scholar]